JARVIS Workbook | Chapter 13 - Skin, Hair, and Nail
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
You are conducting a class for new graduates on skin assessment. Which statement is true regarding the epidermis?
A. The epidermis consists mostly of connective tissue or collagen.
B. The epidermis contains the blood vessels.
C. The epidermal cells are continually lost and replaced with new cells.
D. A "paper cut" stimulates nerve cells in the epidermis.
C
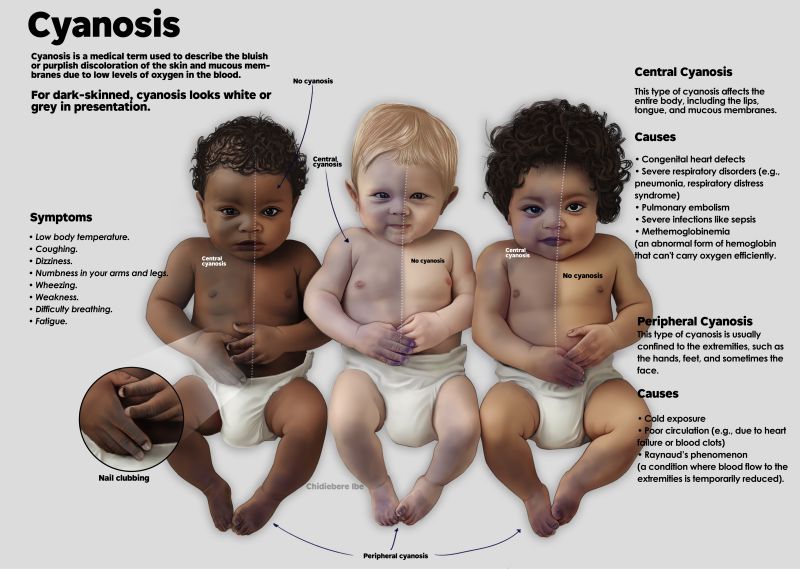
You are preparing to care for a 63-year old Black man with a history of heart attack who now presents with a heart failure. What is the best technique to assess for cyanosis?
A. Palpate the skin for increased heat
B. Inspect the hard palate of the mouth
C. Inspect the feet for an ashen gray look
D. Inspect the nail beds for a dusky pale color
D
You are taking a history for a 25-year-old woman with a rash on her upper chest and neck. Which questions would give you further information on the woman's rash?
A. How much alcohol would you say you drink each week?
B. Have you tried a new food or medicine?
C. Have you recently started oral contraceptives?
D. With which racial-ethnic group do you identify?
B
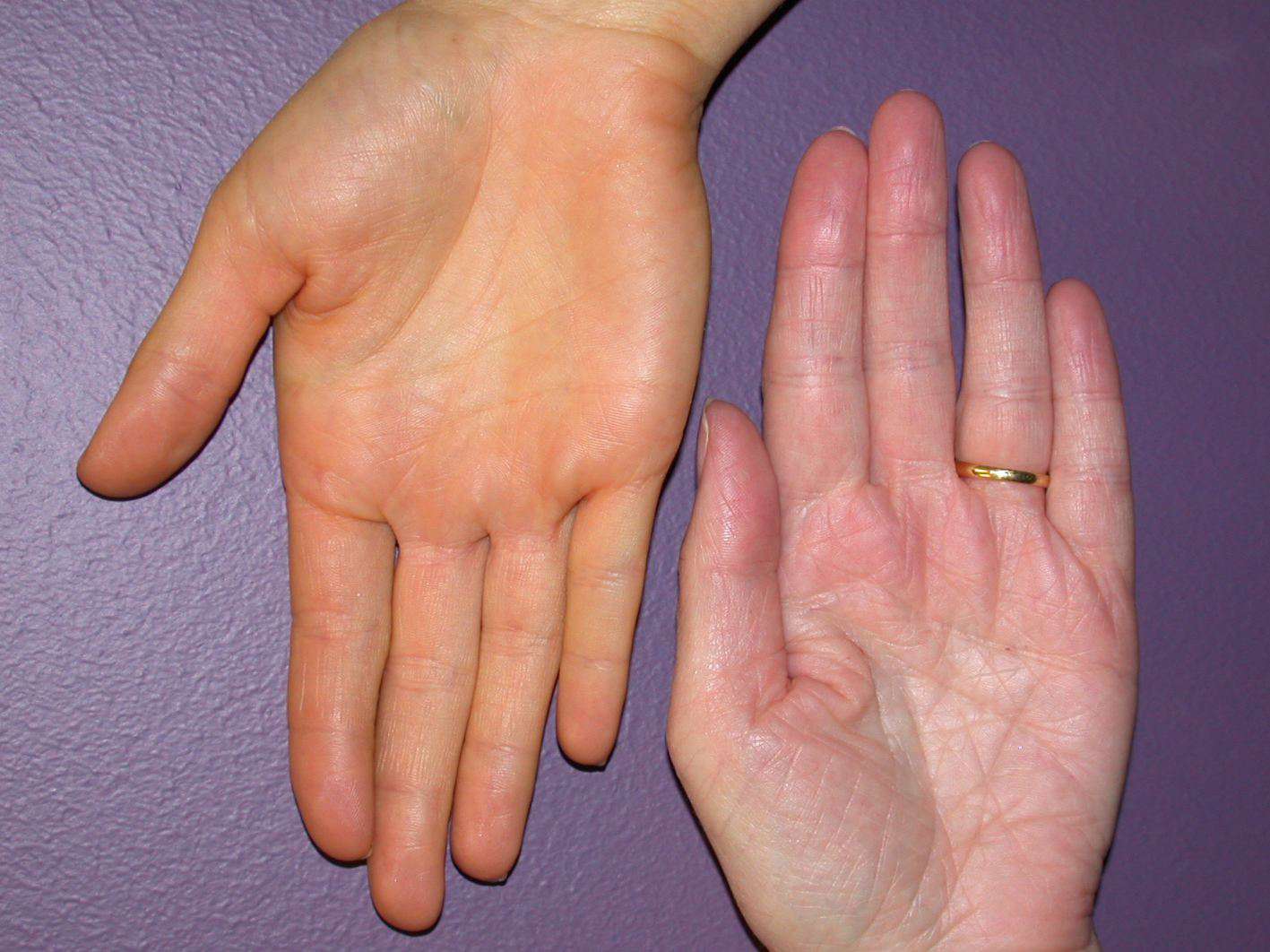
You are caring for a 48-year old with a history of chronic alcohol abuse and liver disease. Which site is the best technique to assess for early jaundice?
A. Sclera and hard palate
B. Nail beds
C. Lips
D. Visible skin surfaces
A
You are assessing the skin of a 57-year old during a clinic appointment. Which technique is the best to assess for increased skin temperature?
A. A grasping with your fingertips of both the hands.
B. Laying the palmar surface of your hands on the abdomen.
C. Placing the ventral surface of your hands on the person's shins and feet.
D. Laying the dorsal surface of your hands on the persons neck.
D
You are assessing the general skin color of a darkly pigmented person. You would expect which finding?
A. Lighter pigmentation on the palms of the hands
B. A reddened color on the lips
C. Patchy pigmentation on the dorsal surface of the hands
D. Small flat macules of browner pigment melanin on the chest
A
You are in the ED when a 70-year-old woman is brought by ambulance after falling in her assisted living space and then not being found for 14 hours. Vital signs are stable, imaging shows no broken bones. She is alert and oriented. One of your assessment findings is the skin on her upper chest "tents" after you lift it. This finding is consistent with:
A. Edema
B. Dehydration
C. Dry skin (xerosis) of aging
D. A normal finding for her age and upper chest
B
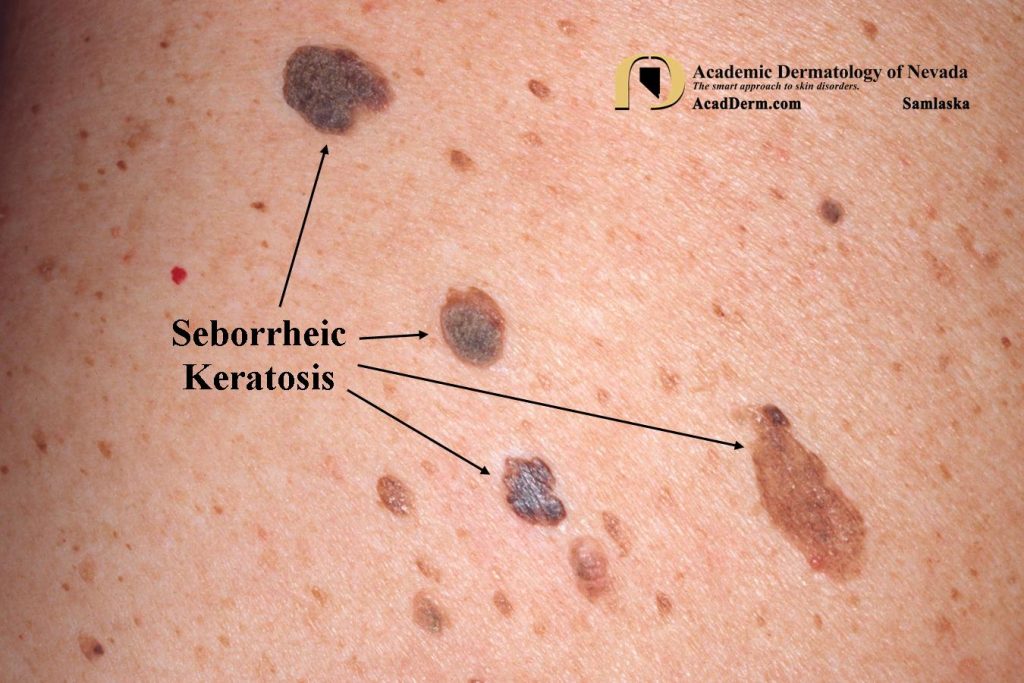
During your skin assessment of a 65-year-old white landscape worker, you notice a raised, thickened area of increased pigmentation of 1.5cm that looks dark brown and greasy. What is your next most appropriate action?
A. Interpret their as seborrheic keratosis and move on with the examination
B. Notify the physician
C. Inquire about recent exposure to toxic outdoor plants
D. Inquire about recent exposure to deer ticks
A
A 78-year-old retired physical examination teacher comes to your clinic for a routine assessment. The teacher asks about small, round, flat, evenly brown macules on the backs of the hands. After assessing the area, what is your best response?
A. "These are the result of sun exposure and do not require treatment."
B. "These are related to sun exposure and may become cancerous."
C. "These are skin tags that occur with older age and do not require treatment."
D. "I'm glad you brought this to my attention. I will refer you for a biopsy."
A
A 50-year-old is admitted to your medical surgical unit with chronic obstructive lung disease (emphysema). Signs are: alert and oriented, on low-flow oxygen, with BP 156/78 mmHg, HR 88 bpm and regular, respirations 20 per minute and unlabored. During initial assessment, you observe a rounded appearance of the nail beds to their base in all 10 fingers. Your next appropriate action is to:
A. Notify the physician
B. Increase the oxygen flow
C. Note this is an expected finding for this person and move on
D. Take his vital signs again
C
During a routine assessment of a 35-year-old, you notice the makings in the nail beds of the photo below (white lines, horizontal, across nail bed), these linear streaks are appropriately recorded as:
A. Increased linear pigmentation
B. Leukonychia stiata
C. Melanoma of the nail matrix
D. Splinter hemorrhages
B
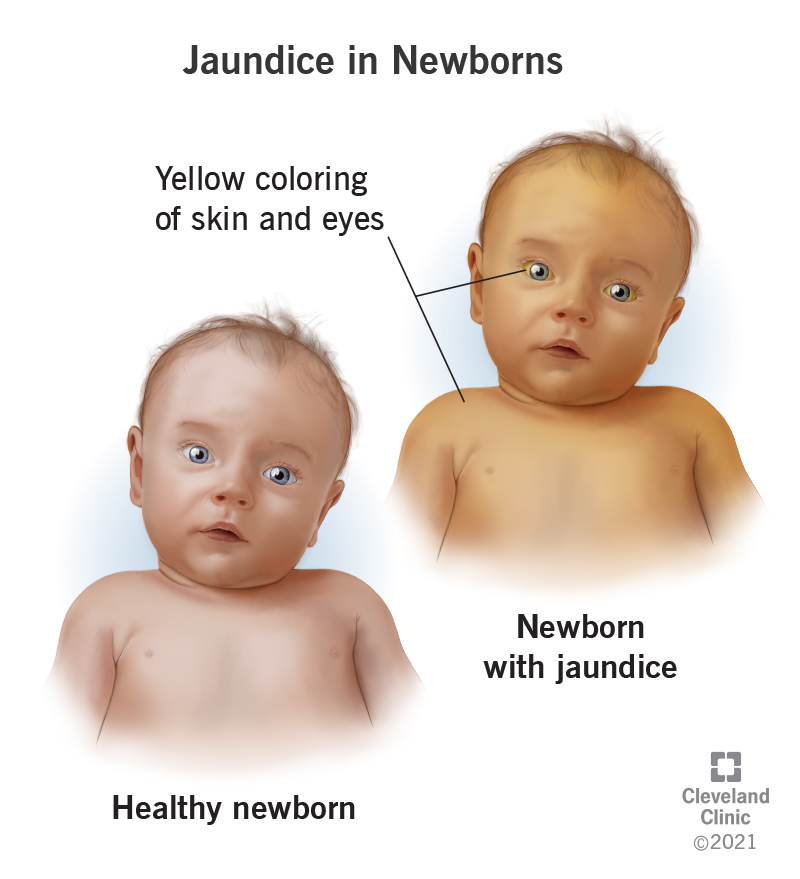
A 3-day-old infant has had healthy assessments since birth. On this 3rd day, you notice a yellowing of the skin, sclera, and mucous membranes. Your next most appropriate action is:
A. Ask the breast-feeding mom to avoid carotene-rich foods
B. Notify the physician that this many be hemolytic disease of the newborn
C. Record this as physiological jaundice and proceed with the assessment
D. Perform deep palpation on the abdomen to elicit possible pain associated with biliary tract obstruction
C
During a sports physical for a 14-year-old adolescent, you observe many papules, pustules, nodules, and "blackheads" covering the cheeks and jaw of his face. Which of these statements would be your most appropriate one?
A. "Have you heard any other kids say anything about your acne?"
B. "You have severe acne; it is at its peak and will eat better in a year."
C. "How do you feel about the acne on your face?"
D. "Would you say your acne has made you feel depressed?"
C
You are collecting a health history on a 52-year-old woman. Vital signs and weight are within normal range. At one point, she reports "the last few weeks I have had sudden drenching sweating through my shirt." How would you proceed with data collection?
A. "Can you tell me the date of your last menstrual period?"
B. "Do you have chest pain at this time?"
C. "Would you say you are depressed?"
D. "What was your activity level at these times?"
A - consistent with hot flashes which is a menopause symptoms
A 74-year-old woman presents with a history of intense itching and a raised red linear rash on one side of her upper back. You know these findings are consistent with: (SATA)
A. A bacterial skin infection
B. Herpes zoster infection (shingles)
C. Poison ivy contact
D. History of childhood chicken pox infection
B, D
B - often follow a dermatomal pattern and is unilateral
D - shingles can only occur in individual who have had chickenpox
A father brings his 18-month old infant to your clinic because of a red blotchy rash on the face and neck. Father reports cough, runny nose, and "doesn't want to eat or drink much." Vital signs are 39 degrees C (102.4 F), HR 120 bpm, respirations 24/min, infant looks sick and miserable. What are the best techniques to continue with the assessment: (SATA)
A. Check for immunization history for the infant
B. Ask if any other children at home or daycare have the same rash
C. Inspect infant's inner cheeks for blue-white "pearls" on the mucosa
D. Check nailbeds for capillary refill
A, B, C
erythema
intense redness of the skin due to excess blood in the dilated superficial capillaries
cyanosis
bluish mottled color that signifies decreased perfusion
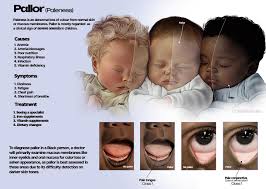
pallor
absence of red-pink tones from the oxygenated hemoglobin in blood
jaundice
increase in bilirubin in the blood causing a yellow color in the skin
___________: tiny, punctate red macules and papules on the cheeks, trunk, chest, back) and buttocks
erythema toxicum

_____________: lower half of body turns red, upper half blanches
harlequin

_______________: transient mottling on trunk and extremities
cutis marmorata

______________: bluish color around the lips, hands, fingernails, feet, and toenails
acrocyanosis

______________: large round or oval patch of light brown usually present at birth
cafe au lait spot

_________________: yellowing of skin, sclera, and mucous membrane due to increased numbers of red-blood cells hemolyzed after birth
physiologic jaundice
______________: yellow-orange color in light-skinned persons from large amount of foods containing carotene
carotenemia
review all of the skin color changes that could occur in infant…
harlequin
erythema toxicum
acrocyanosis
physiologic jaundice
carotenemia
cafe au lait spot
cutis marmorata
list the 3 layers associated with the skin, and describe the contents of each layer
epidermis - first layer, thinnest, keratinized stratified squamous epithelium
dermis - thickest layer, middle, loose, dense irregular, and areolar connective tissues
subcutaneous - third layer, adipose connective tissue
differentiate between the sebaceous, eccrine, and apocrine glands…
sebaceous - glands that produces sebum (oily substance) (hair, lips, eyelids, and nipples)
eccrine - glands that produces sweat outward onto the skin (throughout the body)
apocrine - glands that produces sweat into hair follicles (e.g., breastmilk, earwax, etc)
pallor on light-pigmented vs. dark-pigmented skin…
light skin - paleness of the skin, nail bed and mucous membrane
dark skin - gray or ashen appearance on dark brown to black skin and yellow-ish on brown skin
erythema on light-pigmented vs. dark-pigmented skin…
light skin: redness
dark skin: reddish brown, gray, or purplish like a bruise

cyanosis on light-pigmented vs. dark-pigmented skin…
light skin: bluish-purplish skin tone (most look like cyan)
dark skinL grayish or whiteish (some blueish hue)
jaundice on light-pigmented vs. dark pigmented skin…
light skin: yellowish
dark skin: darker yellowish

what are the possible causes of skin temperature changes (hypothermia/hyperthermia)?
hypothermia: immobilized extremities or exposed to the cold
hyperthermia: increased metabolic rates (e,g., fever, exercise, trauma, infection, and sunburn
what are the possible causes of skin moisture (increase/decrease)?
increased - increased activity, warm environmental, anxiety, thyrotoxicity, heart attack, pain
decreased - dehydration
what are the possible causes of texture (normal/hyperthyroidism/hypothyroidism)?
normal - skin feel smooth and even surface
hyperthyroidism - skin feel smooth like velvet - grave’s diseases (autoimmune disorder)
hypothyroidism - dry rough flaky - increased carotene, reduce eccrine gland, thickened skin, reduced thyroid hormone
white linear marking that are normally visible through the naul and on the pink nail bed are _____________
lunula
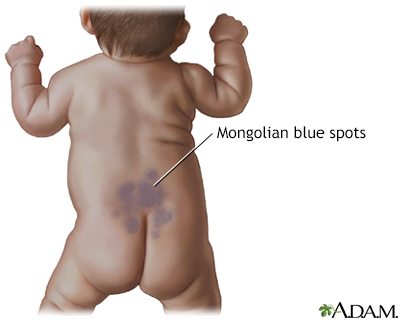
mongolian spot
flat, blue gray, birthmark that may appear on a baby (usually at the sacrum/buttock) at birth or shortly after
milia
tiny white papule on cheek and forehead and across nose and skin (caused by sebum that occludes the follicles)

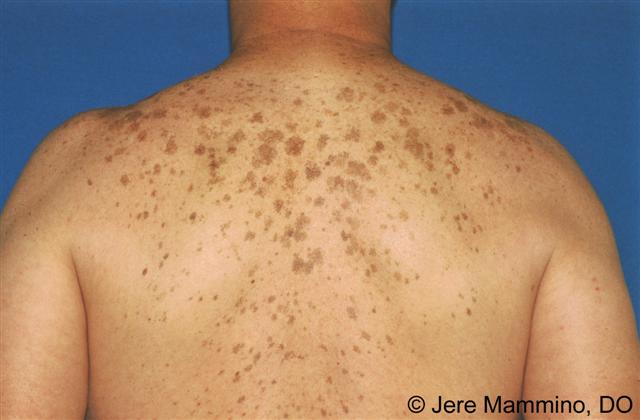
lentigines
“liver spot” - usually benign, flat, brown macules (flat discoloration) from sun exposure
seborrheic keratosis
normally benign, brown, black, light tan growth - while the exact cause of SK is unknown, some factors that may contribute to it manifestation is genetics, sun exposure, aging, hormonal factors, and mutations of specific genes
actinic keratosis
rough, scaly skin patch from sun exposure

acrochordons (skin tags)
stalk-like growth

sebaceous hyperplasia
raised yellow papules

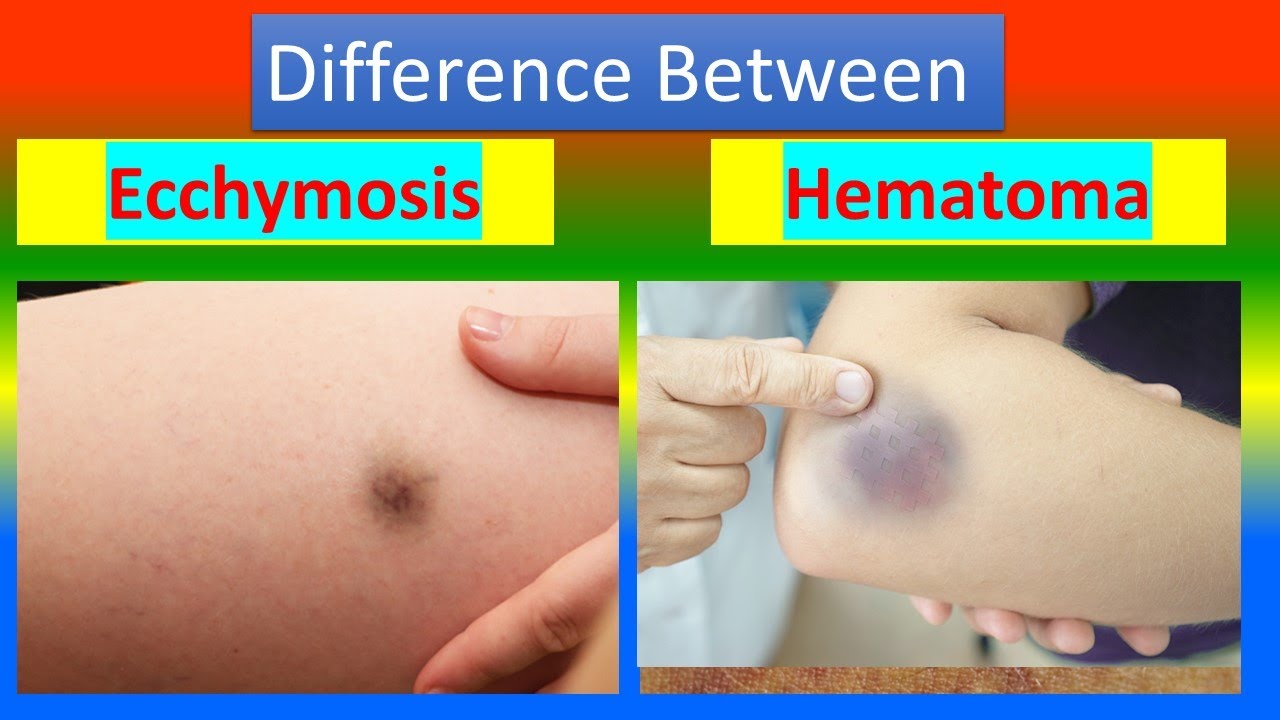
differentiate between petechiae, bruise, and hematoma…
petechiae - small red or purple spot caused by bleeding into the skin
bruise - on injury appear as an area of discolor on the body from ruptured blood vessels
hematoma - solid swelling of clotted blood
petechiae
small red or purple spot caused by bleeding into the skin (brighter than bruise)

bruise
on injury appear as an area of discolor on the body from ruptured blood vessels (usually flat while hematoma is bulbous and is generally smaller than a hematoma)

hematoma
solid swelling of clotted blood (usually bulbous while a bruise is usually flat and is generally larger than a bruise))
measles (rubeola) on light-pigmented vs. dark-pigmented skin…
light skin - red, flat, and slightly raised
dark skin - also flat and slightly raised but purple or darker than surrounding skin

german measles (rubella) on light-pigmented vs. dark-pigmented skin…
light skin - rash appears pink or red-spotted, rough, and bumpy
dark skin - rash may appear hyperpigmented and rough/bumpy

chickenpox on light-pigmented vs. dark-pigmented skin…
light skin: hot, painful, and red
dark skin: hot, painful skin with red hue, brown or violet

stage 1 of pressure injury development
nonblanchable
painful and different in firmness/temperature
skin intact and no exposed skin layer
stage 2 of pressure injury development
partial skin-thickness loss with exposed dermis
shallow open sore but skin either still intact or ruptured from blister
stage 3 of pressure injury development
full thickness loss with exposed subcutaneous
undermining
tunneling
stage 4 of pressure injury development
full thickness skin and issue loss exposing underlying muscle, tendon, bone
can cause osteomyelitis
macule
papule
nodule
wheal
vesicle
pustule
crust
sclae
fissure
erosion
ulcer
nail matrix
nail bed
posterior nail fold
cuticle
lunula
lateral nail fold
nail plate