Immune System I: Innate Immunity & Antigen Recognition
1/167
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
168 Terms
What are the three lines of defense against pathogens in mammals?
Physical barriers, innate immune system, adaptive immune system.
What role do tight junctions between epithelial cells play?
They keep most pathogens and toxins from entering the body.
What is the function of the mucus layer secreted by many epithelial cells?
It protects against pathogens, toxins, and other chemicals.
What is the role of ciliated cells in the respiratory tract?
They sweep away mucus, trapped bacteria, and other foreign matter.
What do some mucus layers produce that are hostile to pathogens?
They produce chemicals (e.g., acids, digestive enzymes, lysozyme) that are hostile to pathogens.
Are physical barriers part of the immune system?
No.
What type of response does innate immunity provide?
An immediate, nonspecific response to cellular pathogens such as bacteria and viruses.
Does innate immunity have memory of prior pathogen exposure?
No, it has no memory of prior exposure to the pathogen.
What is a defining feature of adaptive (acquired) immunity?
It is specific — it recognizes individual pathogens and mounts an attack that directly neutralizes or eliminates them.
How does adaptive immunity respond to a second exposure to the same pathogen?
It retains a cellular memory of the pathogen and reacts quickly upon second exposure.
What mechanisms are associated with adaptive immunity?
Inherited mechanisms leading to the synthesis of molecules that target pathogens in a specific way.
What is the role of the innate immune system during an infection?
It provides some protection against invading pathogens while the more powerful, specific response system is mobilized, which can take several days.
What makes up the immune response?
The collective defensive reactions of innate immunity and adaptive immunity.
How do innate and adaptive immunity interact?
They interconnect and communicate at chemical and cellular levels.
What characterizes innate immunity?
Recognition of traits shared by broad ranges of pathogens using a small set of receptors and a rapid response.
What are the barrier defenses of innate immunity?
Skin, mucous membranes, and secretions.
What are the internal defenses of innate immunity?
Phagocytic cells, natural killer cells, antimicrobial proteins, and inflammatory response.
What characterizes adaptive immunity?
Recognition of traits specific to particular pathogens using a vast array of receptors and a slower response.
Who has adaptive immunity?
Vertebrates only.
What is the humoral response?
Antibodies defend against infection in body fluids.
What is the cell-mediated response?
Cytotoxic cells defend against infection in body cells.
What types of components does the innate immune system have?
Both cell-mediated and secreted components.
What types of components does the adaptive immune system have?
Both cell-mediated and secreted components.
How specific is the innate immune response?
Broadly specific against types of pathogens
How specific is the adaptive immune response?
Specific response against pathogen strains.
How does the adaptive immune response change when infections recur?
The response is more rapid and efficient when infections recur.
How does innate immunity protect the body from pathogens?
Through inherited mechanisms that protect the body from pathogens in a nonspecific way.
What are neutrophils and lymphocytes?
They are types of white blood cells (leukocytes) involved in immune responses.
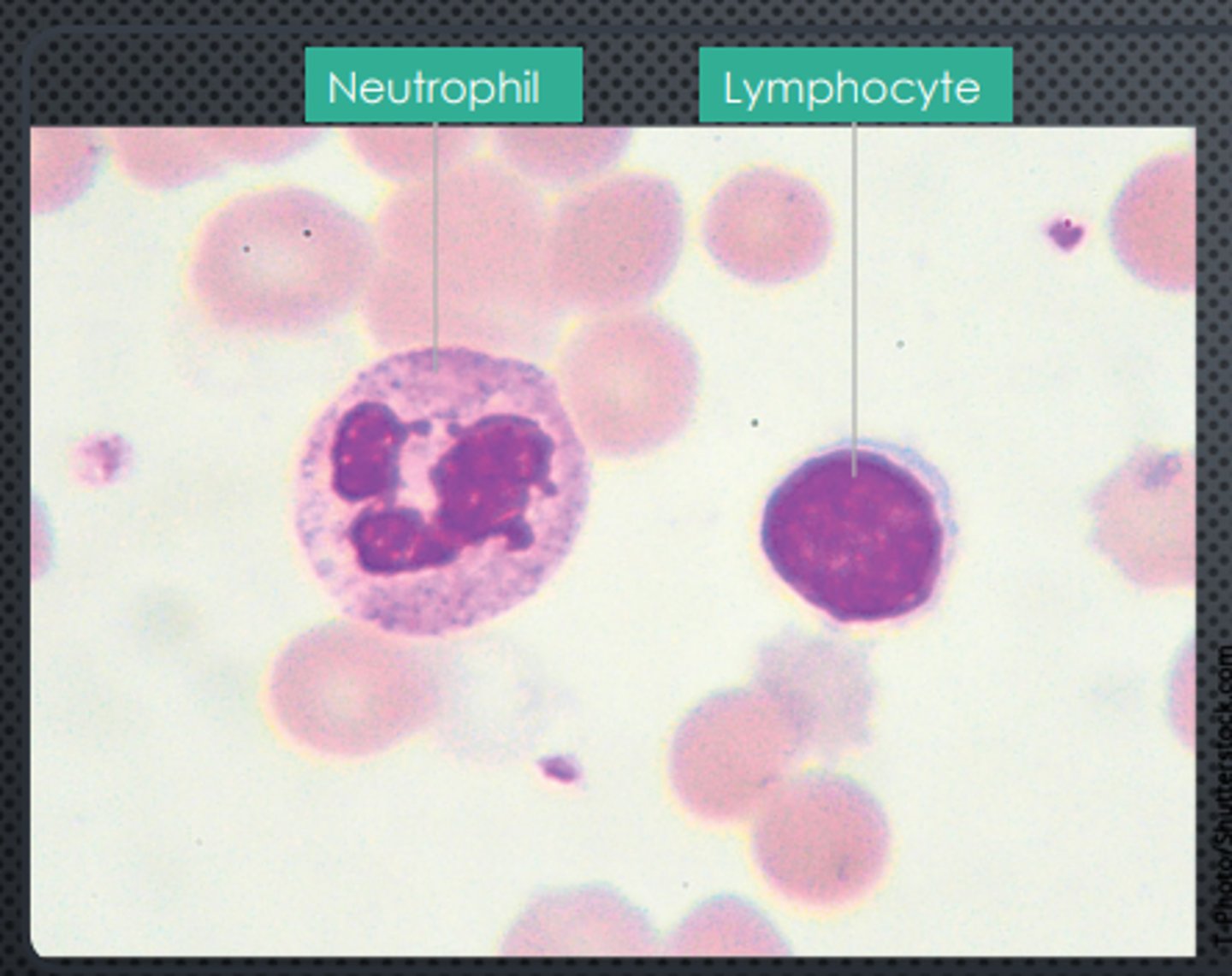
What is responsible for the activities of the two immune systems?
White blood cells (leukocytes) and their derivatives, along with several types of plasma proteins.
What is the function of some white blood cells as phagocytes?
They engulf foreign particles (phagocytosis).
Where do most leukocytes originate?
From stem cells in bone marrow.
Where are lymphocytes formed and where do they migrate?
They form in the bone marrow and then migrate to the thymus.
Diagram 1
Innate and adaptive immune cell interaction timeline
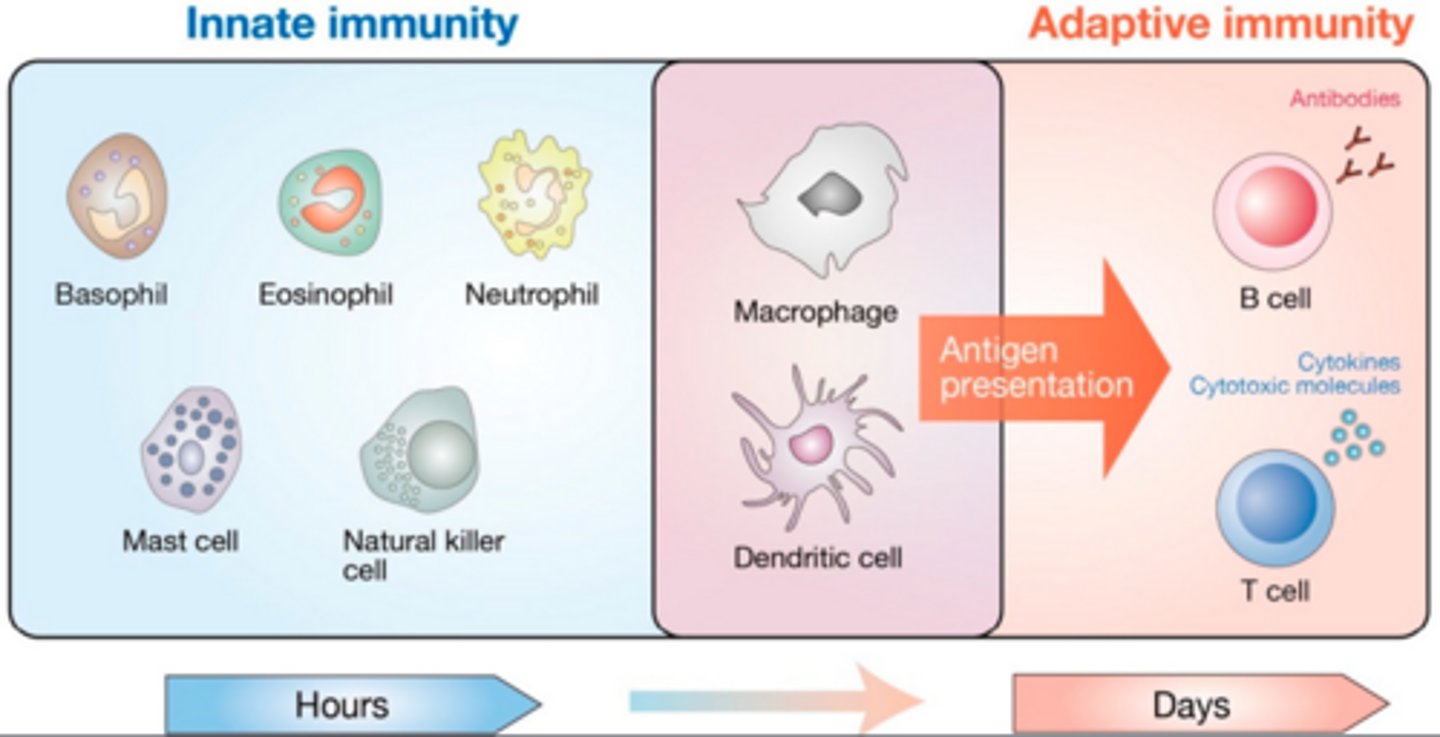
How long does it take the body to develop an effective specific response when a pathogen is first encountered?
About 7 to 10 days.
What types of components does innate immunity have?
Both molecular and cellular components.
Do cellular and viral pathogens elicit the same innate immune responses?
No, cellular pathogens (such as bacteria) and viral pathogens elicit different innate responses.
How do cellular pathogens usually enter the body?
When injuries break the skin or epithelial surfaces.
How are cellular pathogens recognized by the host?
Specific cell-surface receptors in the host recognize various types of molecules on microbial pathogens.
What determines the type of innate response to a cellular pathogen?
The specific receptor involved.
What innate response may occur that directly kills the microbe?
Secretion of antimicrobial peptides that kill the microbe.
What innate response involves engulfing the pathogen?
The host cell engulfs and destroys the pathogen, initiating inflammation.
The host cell engulfs and destroys the pathogen, initiating inflammation.
Activation of the complement system.
Diagram 2
Pathogen recognition
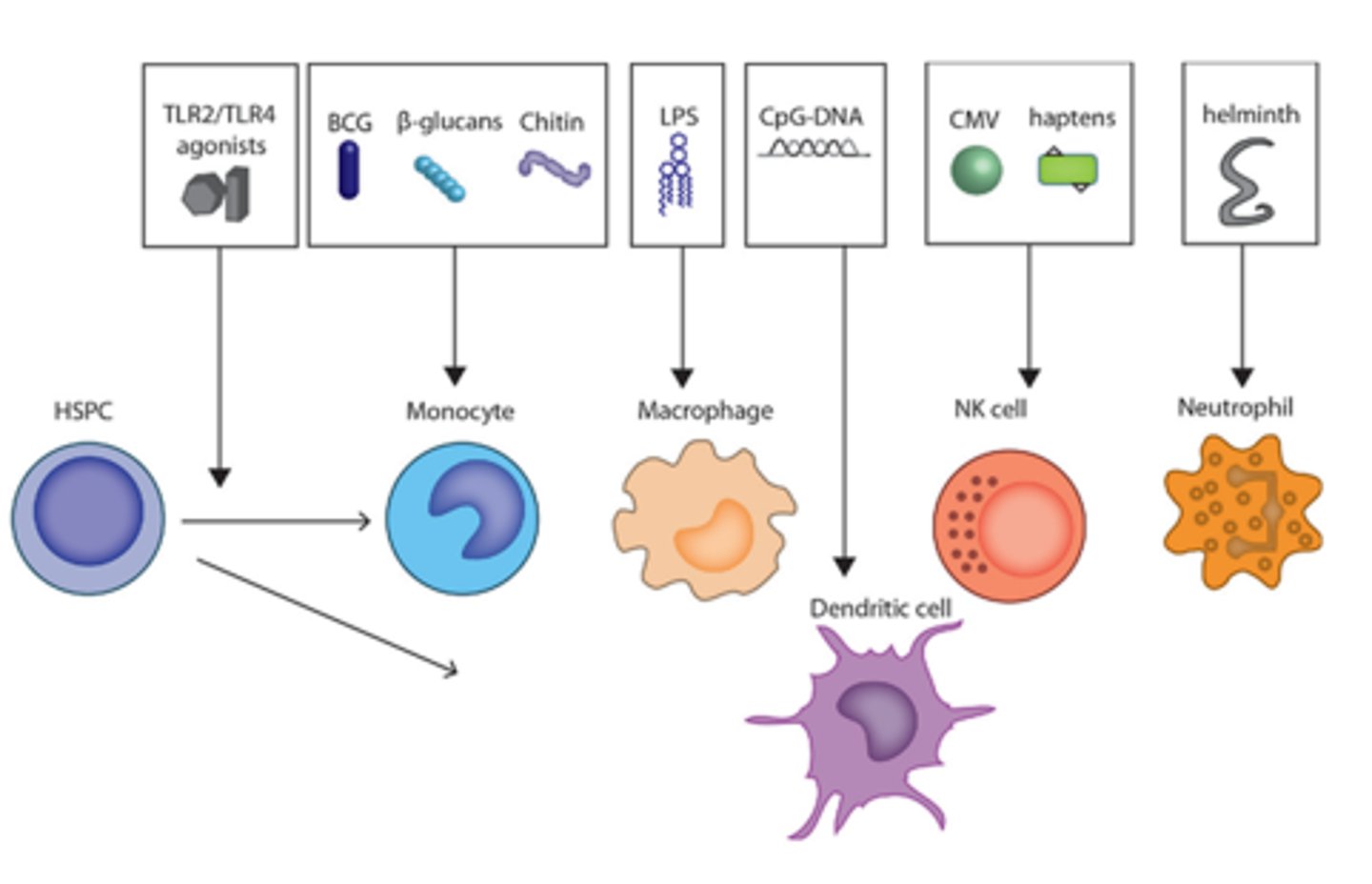
What does the innate immune system recognize to identify pathogens?
Pathogen-associated molecular patterns that are associated with pathogenic organisms but are absent in the host.
What recognizes pathogen-associated molecular patterns?
Pattern recognition receptors of phagocytic cells.
What type of receptors do mammals have for pathogen recognition?
Several classes of pattern recognition receptors, including toll-like receptors.
Where are toll-like receptors found?
On the cell surface and within the cell on various membrane-bound compartments.
Diagram 3
Cell membrane receptor pathways
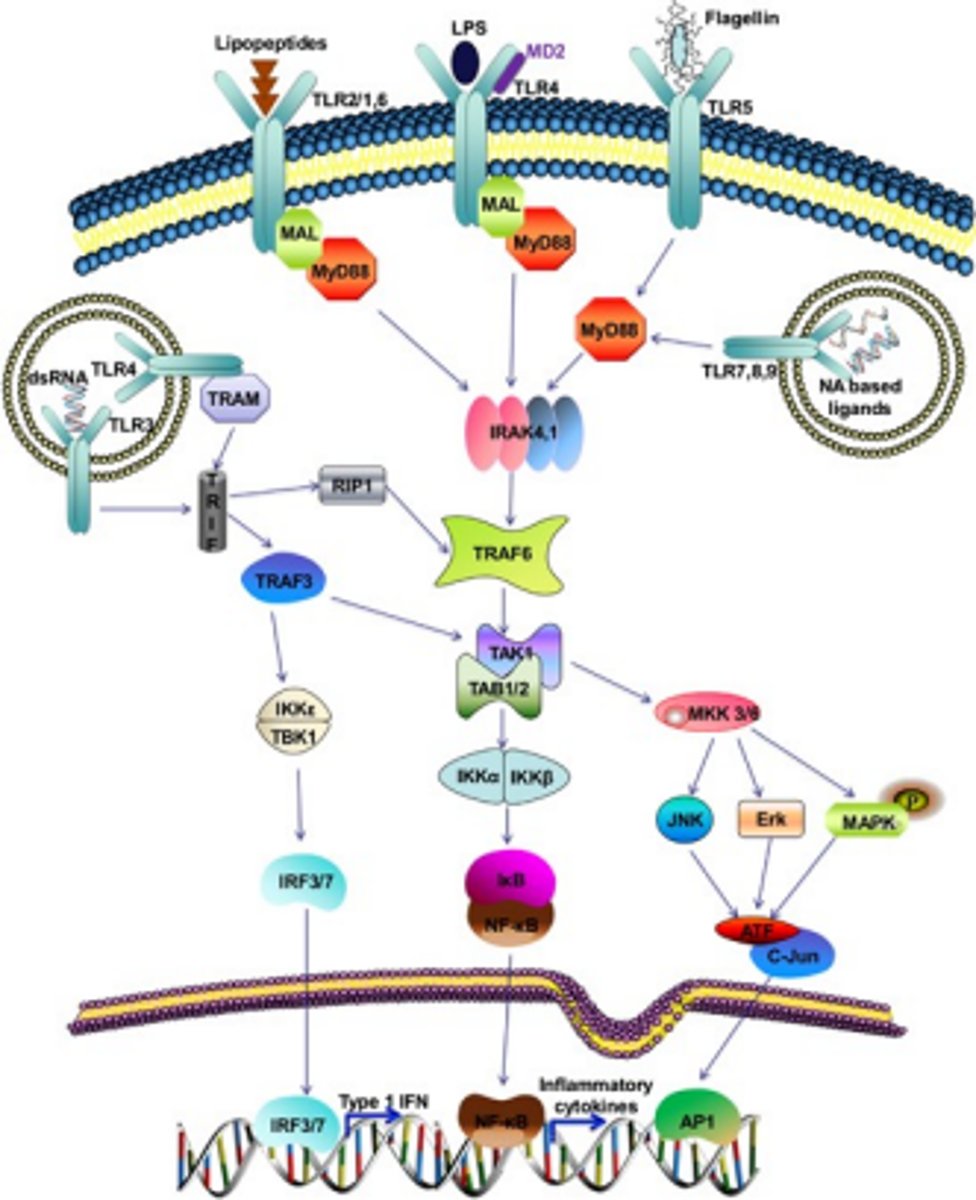
Diagram 4
What protects all epithelial surfaces, inside and out?
Antimicrobial peptides called defensins.
When do epithelial cells secrete defensins?
When attacked by a microbial pathogen.
How do defensins kill pathogens?
They attack the plasma membranes of pathogens, eventually disrupting them and killing the cells.
Where do defensins play a particularly significant role in innate immunity?
In the mammalian intestinal tract.
What is the role of defensins in innate immunity?
Defensins are antimicrobial peptides that disrupt the membranes of pathogens.
Diagram 5
Calor, Rubor, Tumor, Dolor
What is inflammation?
The heat, pain, redness, and swelling that initially or exclusively occur at the site of an infection.
Infection by most pathogens involves what response?
Inflammation.
Diagram 6
Local Inflammation
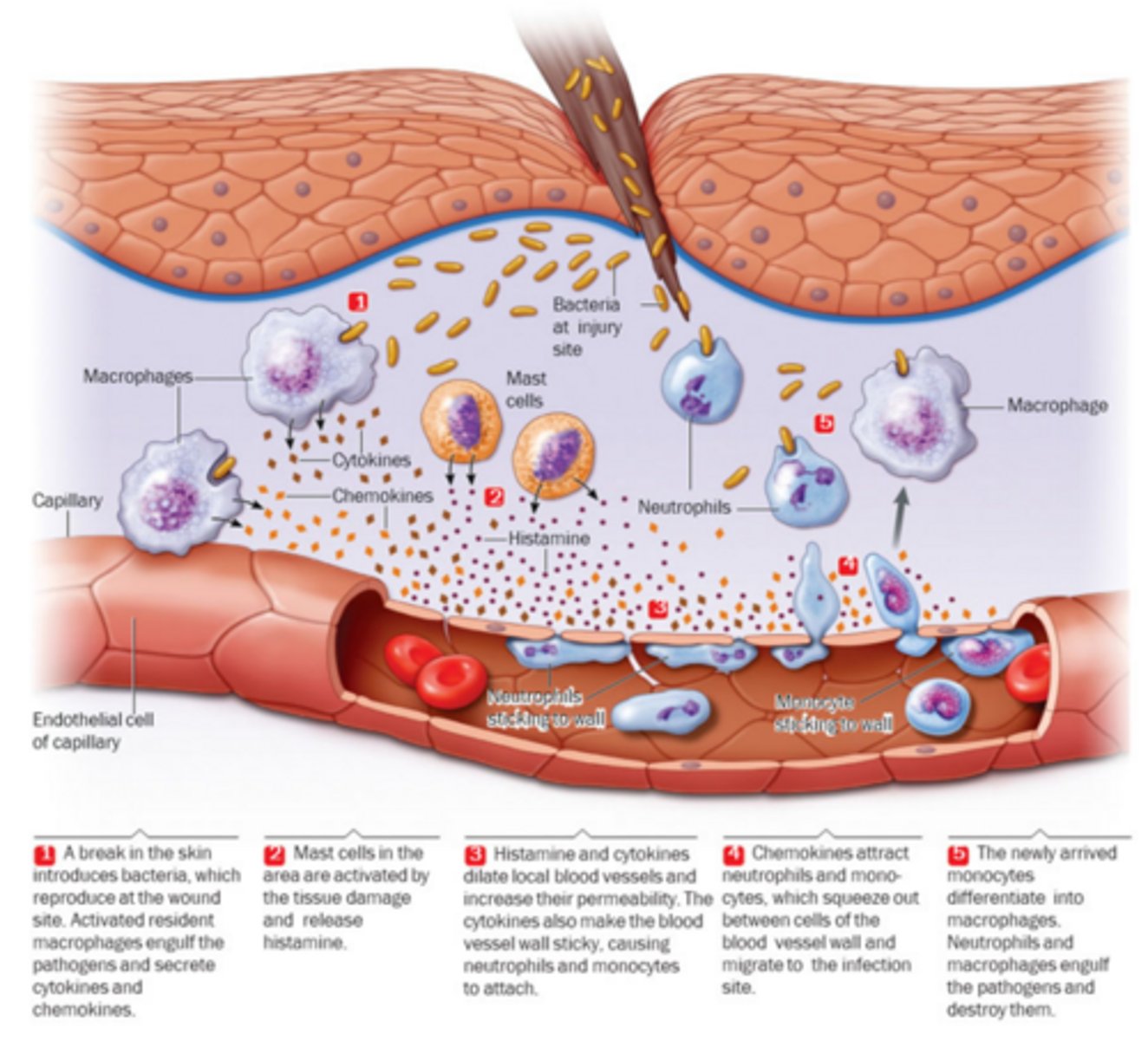
What happens when cell-surface receptors on macrophages bind to a pathogen?
The macrophage is activated.
What do activated macrophages secrete during local inflammation?
Cytokines.
What is the role of cytokines in local inflammation?
They bind host cells and trigger a response.
What activates mast cells during local inflammation?
Tissue damage.
What do mast cells release during local inflammation?
Histamine, an inflammatory signaling molecule.
What is the effect of histamine and cytokines on local blood vessels?
They dilate local blood vessels and increase their permeability.
What effect do cytokines have on local blood vessel walls during inflammation?
They make the blood vessel wall stickier.
Which circulating cells attach to sticky blood vessel walls during local inflammation?
Neutrophils and monocytes.
What attracts neutrophils and monocytes to the infection site?
Chemokines secreted by activated macrophages.
What happens to monocytes once they reach the infection site?
They differentiate into macrophages.
How do macrophages and neutrophils work together at the infection site?
They engulf the pathogens.
What happens to pathogens after they are engulfed?
They are destroyed.
What happens when pathogens are too large to be engulfed?
Macrophages, neutrophils, and eosinophils cluster around the pathogen and kill it by secreting large amounts of lysosomal enzymes and defensins.
Which types of pathogens are often too large to be engulfed?
Parasitic worms.
What type of inflammation may occur if tissue damage is extensive or infection spreads to the blood?
Chemical signaling molecules stimulate the release of neutrophils from bone marrow.
What is the result of neutrophil release from the bone marrow during systemic inflammation?
An increased number of circulating white blood cells.
What systemic inflammatory response may involve the onset of fever?
Systemic inflammation.
What do macrophages release that stimulates the hypothalamus during fever?
Pyrogens.
What do pyrogens stimulate the hypothalamus to release?
Locally-acting prostaglandins.
What is the role of prostaglandins in fever?
They signal the hypothalamic thermostat that regulates body temperature to produce the fever.
How may fever fight infection?
By enhancing phagocytosis or by interfering with bacterial propagation.
What is the complement system made of?
More than 30 interacting plasma proteins that circulate in blood and interstitial fluid.
What is the complement system?
A group of plasma proteins that enhance the immune response and can lyse pathogens.
What activates the complement system?
Molecules on the surfaces of pathogens.
What structures do some complement proteins assemble into?
Membrane attack complexes.
What do membrane attack complexes do to bacterial cells?
They insert into the plasma membrane and create pores that allow ions and small molecules to pass through.
Why do bacteria swell and lyse after complement activation?
They can no longer maintain osmotic balance.
Diagram 10
Complement system

Why is the innate immune system unable to directly detect viral pathogens?
Because the virus is contained inside host cells.
What two main strategies does the innate immune system use against viral pathogens?
Interferon and natural killer cells.
What innate immune strategy is used against viral pathogens that does not involve direct pathogen detection?
Interferon.
How does interferon help fight viral infections?
It triggers changes in infected and neighboring cells to inhibit viral replication.
What innate immune cells are used to defend against viral pathogens?
Natural killer cells.
What are natural killer cells?
A type of lymphocyte that kills virus-infected or cancerous cells.
What does a virus-infected cell synthesize in response to infection?
Cytokines called interferon.
Which cells do interferons act on?
The infected cell that produces them and neighboring uninfected cells.
How do interferons affect target cells?
They bind to cell-surface receptors and trigger a signal transduction pathway that changes gene expression patterns.
What genes are activated by interferon?
Genes for an RNase
What effect does interferon have on protein synthesis in the cell?
It inhibits protein synthesis.
How do interferon effects limit viral replication?
They act on RNA and protein synthesis to inhibit replication of the viral genome.
What is the overall effect of interferon on the infected cell?
The cell is put in a weakened state from which it may or may not recover.
What types of cells do natural killer (NK) cells kill?
Host cells that are infected with a virus or have become cancerous.