Mixed Density Lesions
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
What are the 4 steps in forming a differential diagnosis for a radiological lesion?
1) describe the mixed density/opaque lesion
2) decide whether it is normal or not
3) decide whether it is an artefact eg superimposed spine etc
4) decide whether it is pathological or a variation of normal anatomy
What are the 8 rough groups of mixed density lesions?
1. osteoma
2. exostoses/enostosis
3. osseous dysplasia
4. fibrous dysplasia
5. odontomes
6. adenomatoid odtonogenic tumour
7. cementoblastoma
8. dystrophic calcification
What are exostosis?
They are bony outgrowths in an irregular shape made from normal bone- TORI.
They are usually bilateral.
What are exostosis known as in the mandible and where are they found?
Torus Mandibularis- found in the lingual mandible.
What are exostosis known as in the maxillary and where are they found?
Torus Palatinus- found at the vault of the palate.
How are exostosis managed?
No treatment is needed, but they can be shaved away if they interfere with the denture.
What is an enostosis?
It is an area of dense bone within the alveolar bone commonly known as a dense bone island.
Who does an enostosis commonly tend to present in and where?
Young people.
Most commonly seen in the molar region of the mandible.
How do enostosis tend to present?
It presents as a dense area of cortical bone within the cancellous bone and may connect with the cortex or not.
How does enostosis affect the surrounding teeth?
The PDL and vitality of the adjacent teeth are normal.
What is an osteoma?
This is a benign tumour made up or cortical or cancellous bone.
What demographic are osteomas seen in?
Commonly seen in patients older than 40 years.
How do osteomas present clinically and where?
They present as a bony hard painless swelling in the Lingual mandible, Condyle and coronoid.
How do osteomas present radiographically?
They can often be seen as a well defined mushroom shape with internal trabeculation.
What condition are osetomas associated with?
Gardners syndrome.
What is gardners syndrome and what are 4 features of it?
A genetic disorder associated with multiple osteoma.
features:
- multiple dense bone islands (5+ is pathogenic)
- epidermoid cysts
- polyps of the intestine (cancer risk so need screening)
- multiple unerupted supernumerarys (hyperdontia)
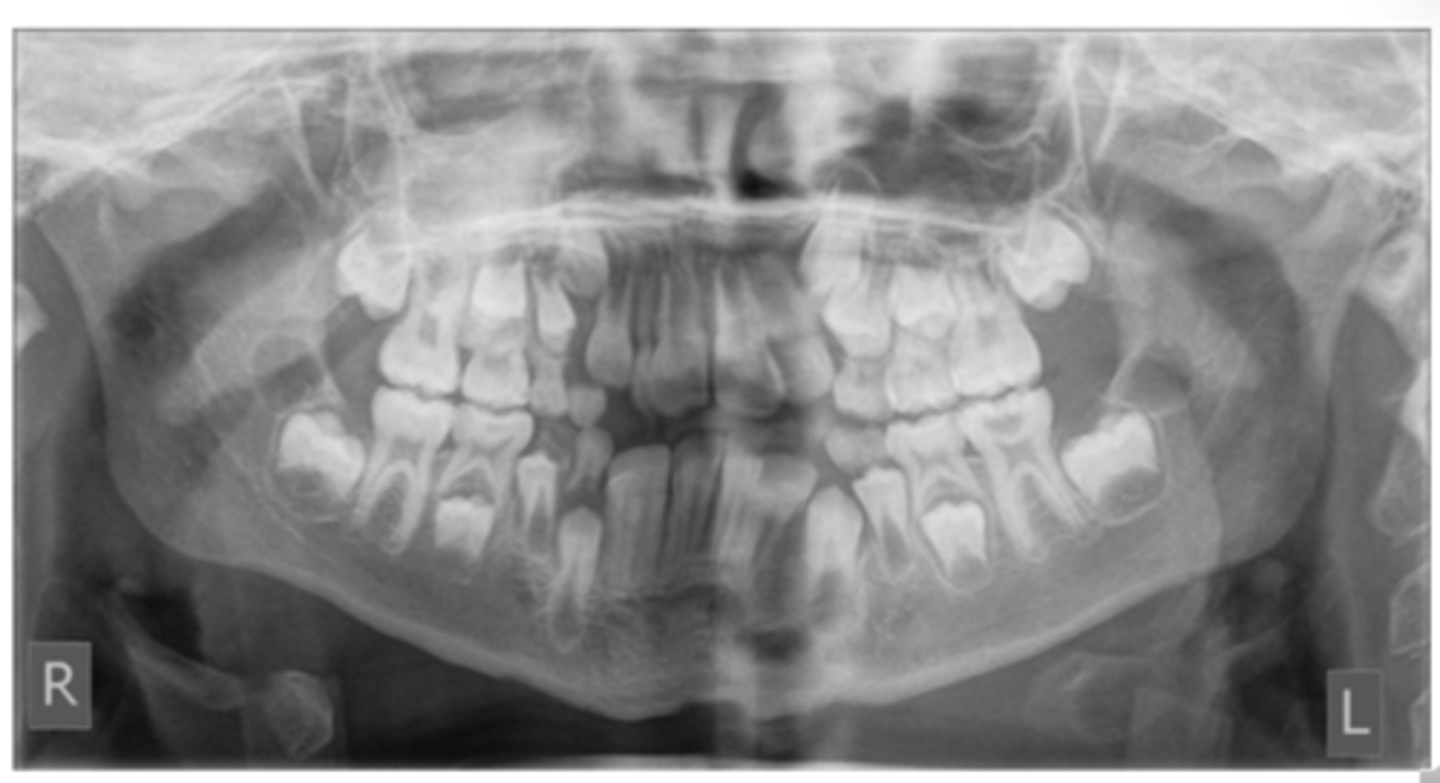
What are the 3 different forms of odontomes?
Complex - an amorphous mess containing enamel, dentine and cementum
Compound - has denticles (small teeth) with obvious enamel dentine features
Dilated odontome - it is like a v large supernumerary tooth with an external ring of enamel and pulp with a donut like appearance
Odontomas= benign odontogenic tumours.
What are the generic radiographic features of odontomes? (5)
1. well defined border either smooth or irregular
2. radiolucent internal soft tissue capsule
3. radiopaque centre with a density similar to tooth tissue
4. more radiolucent when first formed and as mature become more dense
5. do not expand
What are the specific radiographic features of compound/complex odontomes and where do they present?
Compound= there are lots of little teeth/ denticles. It is present in the anterior maxilla and associated with unerupted canines.
Complex - amorphous tooth like density with spiky lobulated margins. It tends to occur In mandibular molar region
What effect do odontomes have on adjacent teeth? (3)
1. cause impaction
2. cause a diastema - especially compound odontomes
3. cause the malformation of teeth
What is an ameloblastic fibrous odontoma?
The middle ground between an ameloblastic fibroma and odontoma.
At what age does an ameloblastic fibrous odontoma present?
Between the ages of 5-20 years.
What are ameloblastic fibrous odontomas associated with?
Unerupted or missing tooth.
How do ameloblastic fibrous odontomas present radiographically?
It appears identical to an ameloblastic fibroma but as it matures it develops internal calcification (of a similar density of enamel/dentine).

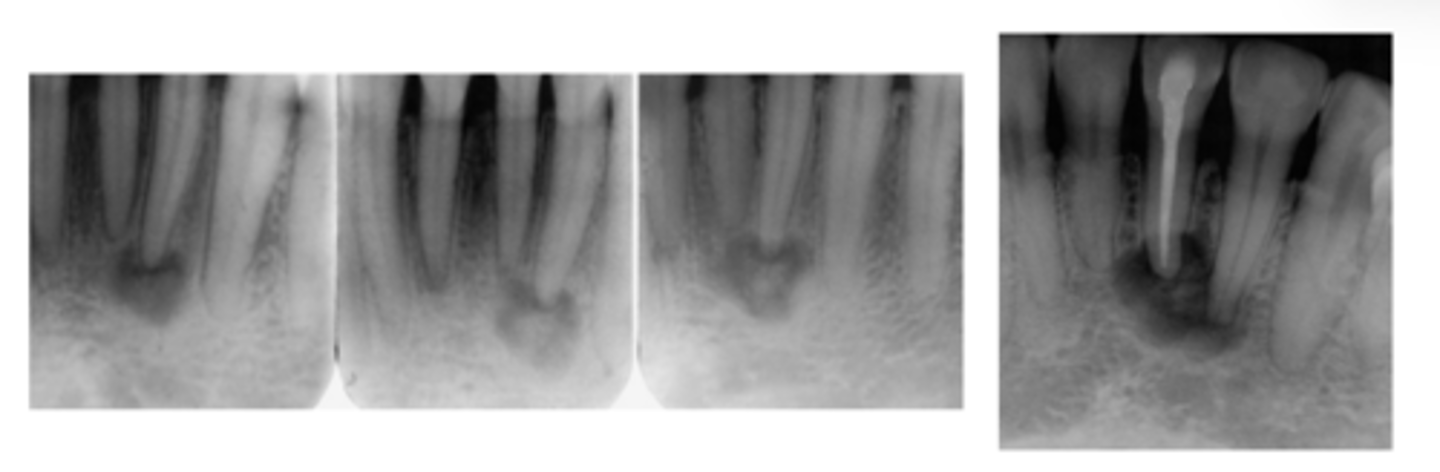
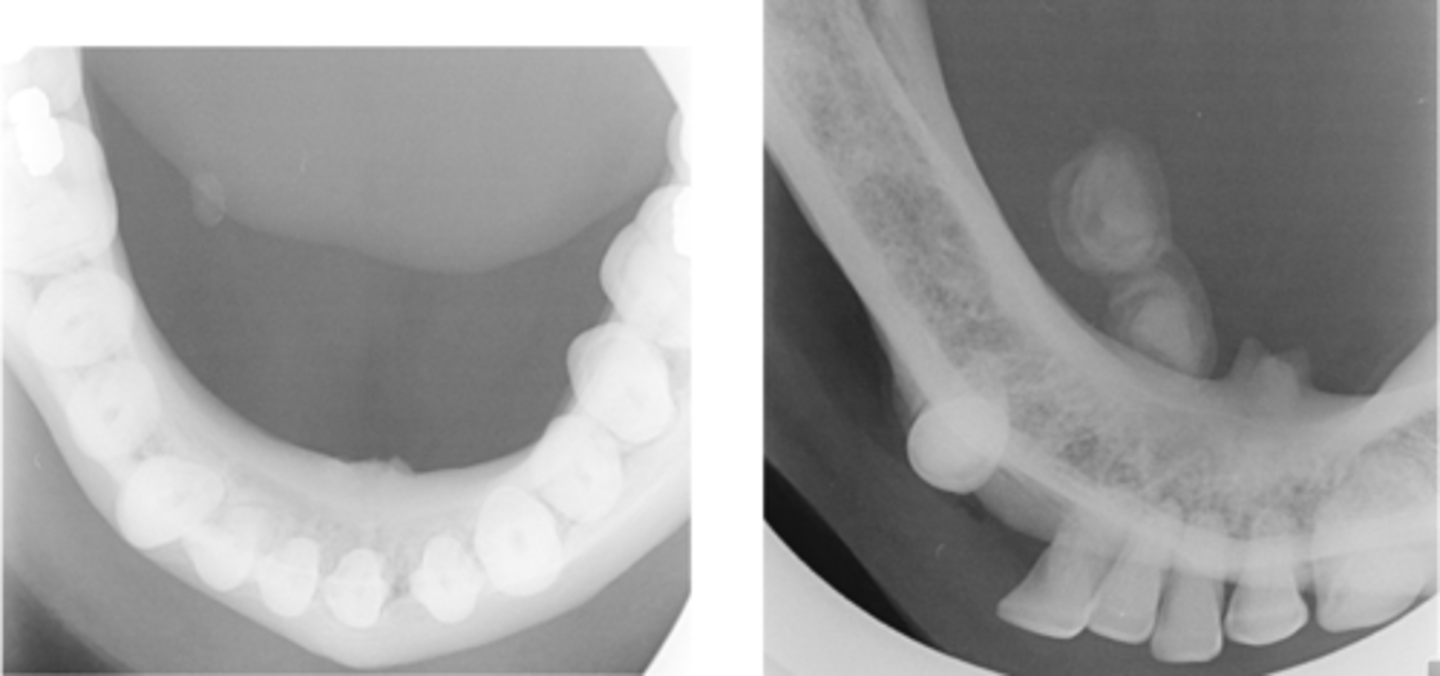
What is a cementoblastoma?
A rare odontogenic tumour which is a mass of cementum or cementum like tissue attached to roots.
How do cementoblastomas present radiographically? (3)
1. Well defined radio opacity at the root apex with cortical border and radiolucent soft tissue capsule just inside cortical border
2. Internal pattern amorphous mixed density often with a central lucent nidus.
3. If the root can be seen external root resorption is seen

Where are cementoblastomas commonly found and how do they present clinically?
In the molar/ permolar region of the mandible.
The vital tooth may be painful.
What affect do cementoblastomas have on adjacent teeth? (2)
It can cause root resorption and can cause the tooth to be painful.
What is an adenomatoid odontogenic tumour associated with?
It is associated with an unerupted tooth in the premolar/canine maxilla region.
Who do adenomatoid odontogenic tumours tend to affect?
Young females.
How do adenomatoid odontogenic tumours tend to appear radiographically? (3)
1. Surrounds whole tooth with corticated border
2. internal fibrous capsule
3. internal faint radiopacities to dense foci. (small pebble clusters.)

How do adenomatoid odontogenic tumours affect associated teeth?
It displaces the associated tooth but it rarely resorbs.
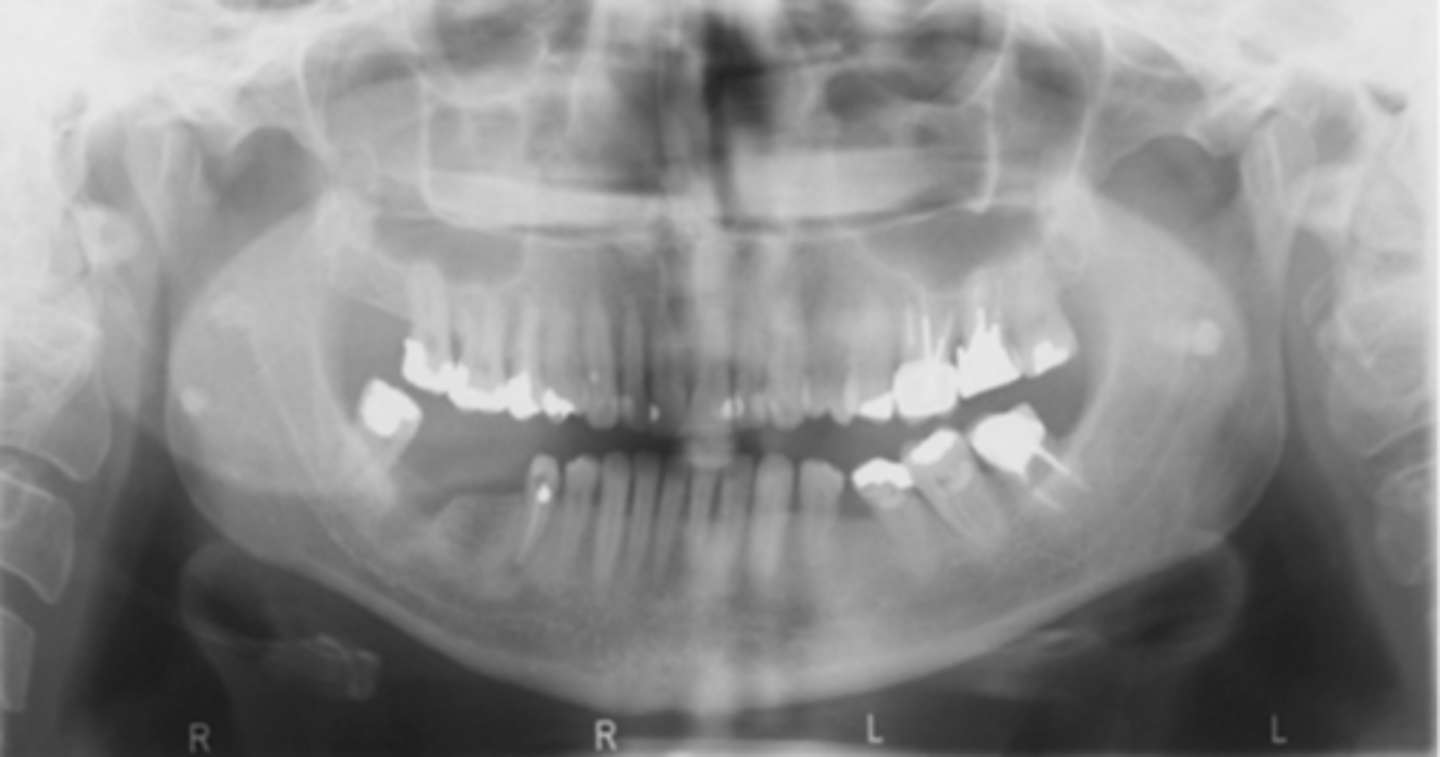
What are the 4 main types of osseous dysplasia?
1. periapical cemento dysplasia
2. focal osseous dysplasia
3. florid osseous dysplasia
4. fibrous dysplasia
What impact do osseous dysplasia have on the teeth?
In osseous dysplasia all the teeth are vital.
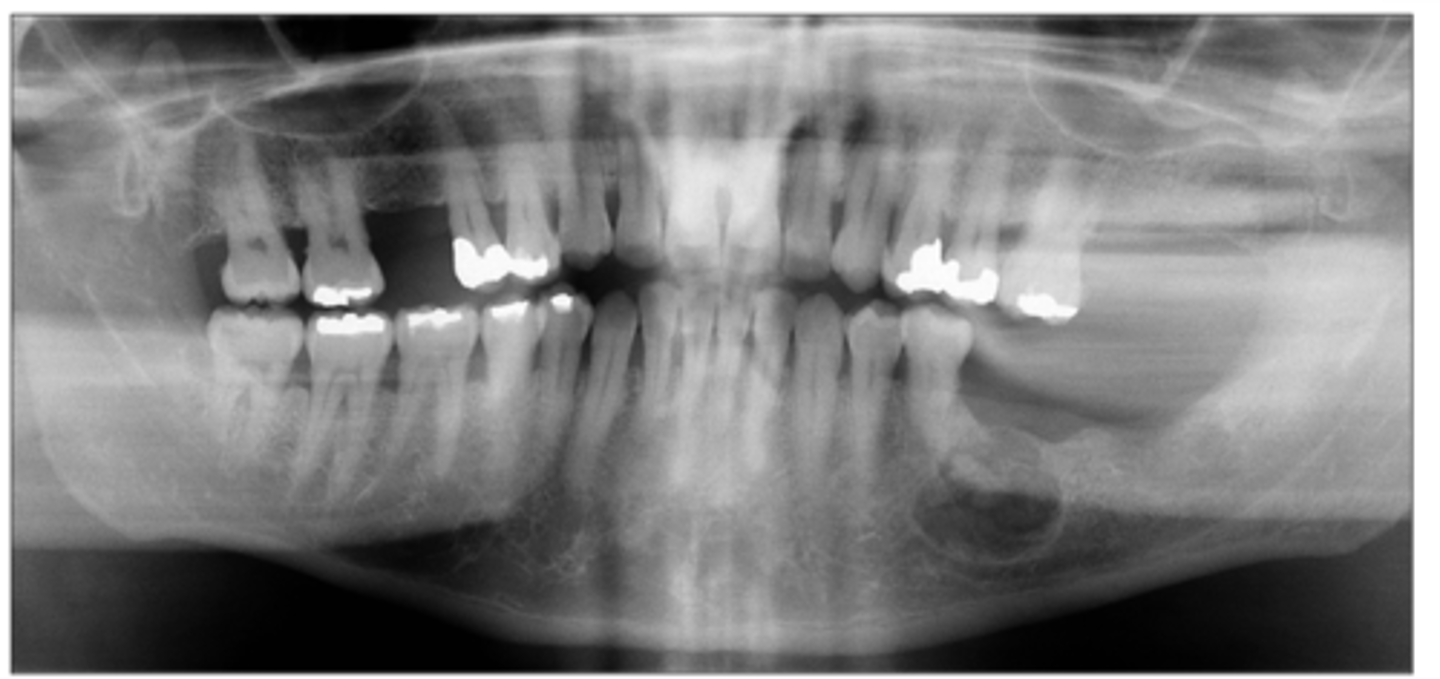
What is periapical osseous dysplasia? (2)
It is the progressive replacement of normal bone with fibrous tissues and then amorphous sclerotic bone with abnormal trabeculae.
In the anterior mandible is the most common area.
Who does periapical osseous dysplasia tend to affect?
Middle aged women.
How does periapical osseous dysplais appear radiographically? (3)
1. a well defined mixed density lesion surrounding the apex of a tooth
2. has a radiolucent fibrous capsule border surrounded by sclerotic bone
3. starts lucent and becomes opaque as it matures
How does peri apical osseous dysplasia affect the associated teeth? (4)
1. LD/PDL is lost
2. can have hypercementosis
3. can resorb but not usually the case
4. tooth remains vital
What is the difference between periapical osseous dysplasia and focal osseous dysplasia?
They have the same disease mechanism but focal osseous dysplasia is seen in isolated molar teeth opposed to anterior teeth.
What is the difference between florid osseous dysplasia and periapical osseous dysplasia?
They have the same pathology but in florid there IS 3 OR MORE QUADRANTS AFFECTED
whereas in periapical osseous dysplasia it is just in anterior teeth.
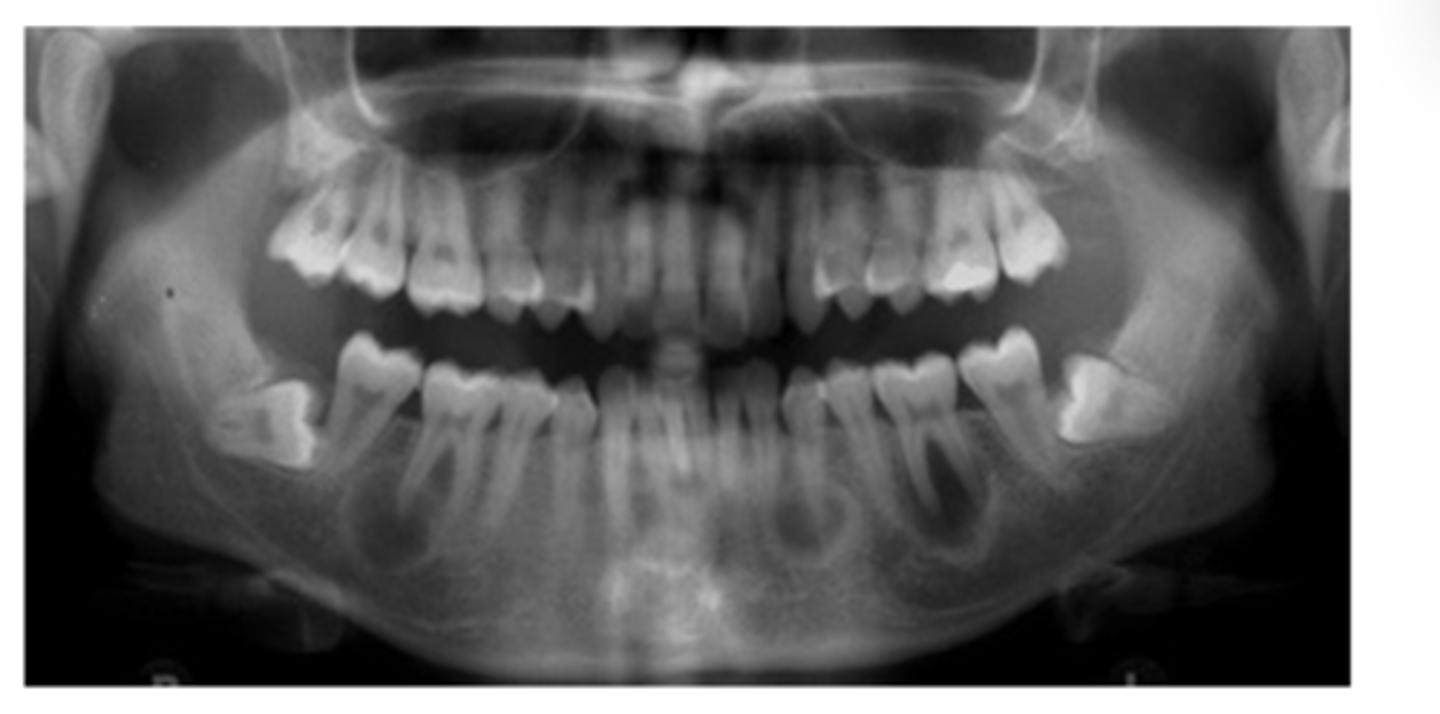
Where are florid osseous dysplasia lesions found?
They are seen throughout the jaw and are not limited to the molars/ incisors.
What affect does florid osseous dysplais have on associated teeth? (2)
They can expand and displace teeth and pose a risk of secondary infection and osteomyelitis due to poor BS.
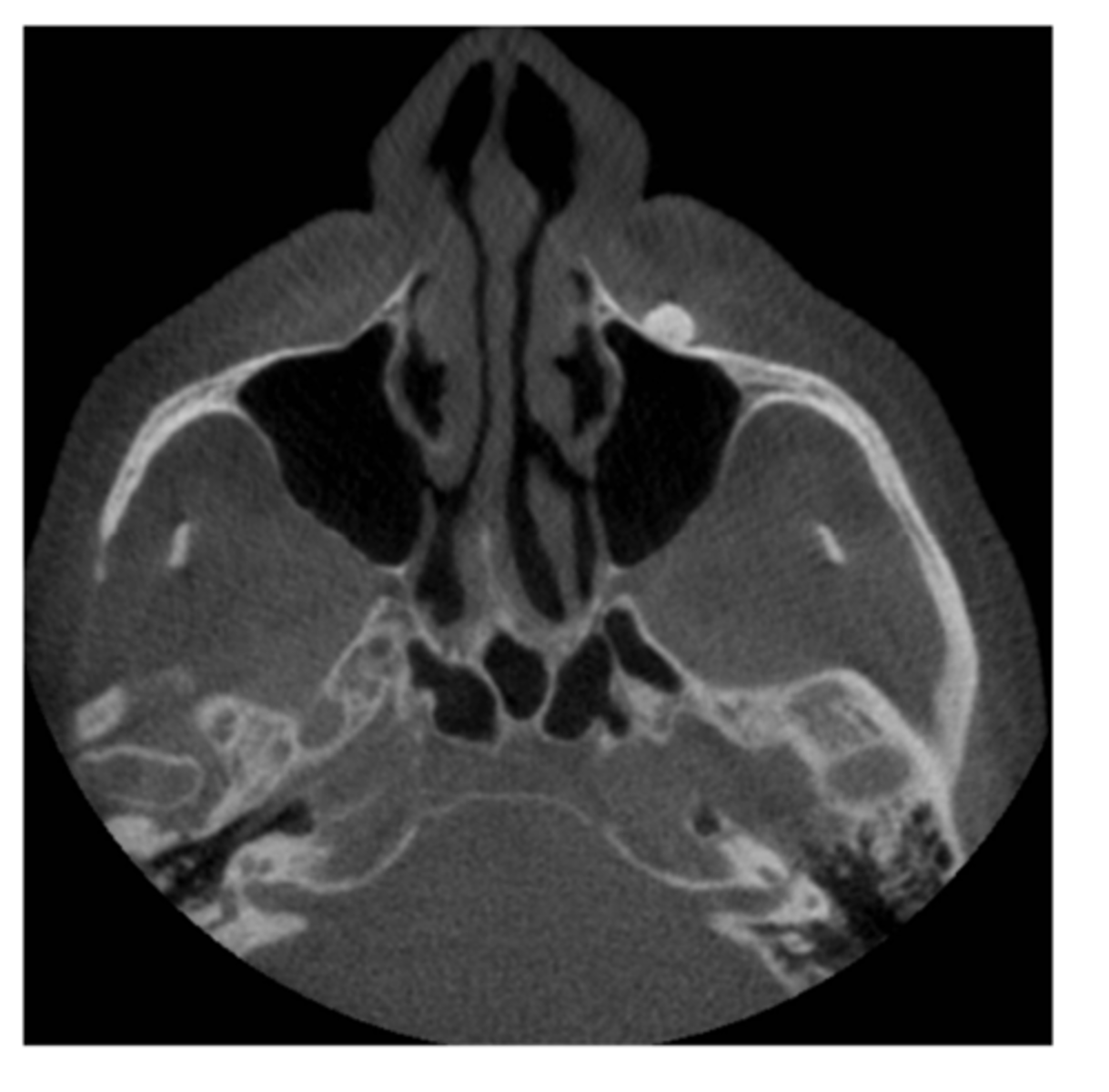
What is fibrous dysplasia?
The replacement of normal bone with fibrous tissue containing immature woven bone.
What tissues are affected by fibrous dysplasia? (4)
1. skull
2. facial bones
3. pelvis
4. spine
What are the radiographic features of fibrous dysplasia? (3)
1. appears as a radiolucency in early stages
2. has a ground glass fine trabeculation with gross expansion of bone
3. can have the superior displacement of mandibular canal which is classic for fibrous dysplasia (non-odontogenic as below ID canal)
What affect does fibrous dysplasia have on associated teeth?
It can cause teeth to become impacted or displaced.
What are the 5 categories of dystrophic calcification?
1. salivary calculi (sialoliths)
2. tonsilloliths
3. lymph nodes
4. phleboliths - calcification within vessels
5. acne
What are the radiographic features of salivary calculi (dystrophic calcification)? (3)
1. lesion of varying density
2. have a 'bullseye' appearance
3. size is v variable
What is tonsilloliths?
It is dystrophic calcification within the tonsillar crypts.