Immunology-Antigen Capture and Presentation
1/31
Earn XP
Description and Tags
9/5/2025-9/8/2025-
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Antigens recognized by T lymphocytes:
The major histocompatibility complex are cell surface proteins that present self or non self-antigens to T cells. T cells can only recognize specific antigens. Helper T Cells (CD4) and Killer T Cells (CD8) recognize MHC-bound peptides. When found the specific receptor, MHC will show their anchor residue of peptide into its “pocket” to connect with T cell.
Antigen-presenting cells (APCs) capture microbial antigens and present them to T lymphocytes via…
MHC
Binding to antigens presented by dendritic cells is critical for naïve T
lymphocytes to undergo…
clonal expansion and differentiate into their
effector and memory cells
How does the antigen presenting cells (APCs) get to the T cells?
Dendritic cells capture antigens directly and take them to the T cells. The antigens travel to secondary lyphoid organs via blood or lymph, or dendritic cells. Dedritic cells occupy epithelia and subepithelial cells.
2 populations of dendritic cells
1) conventional/classis: in skin (Langerhans cells) and tissues and lymphoid organs
2) Plasmacytoid: blood and tissues m produce Type 1 IFNs.
DCs have varied receptors, PRRs binding to PAMPs result in release of TNF and IL-1 that further activates DCs to change phenotype, migration, and function
DC is activated:
Express chemokine receptor CCR7, which a receptor that will follow a chemokine gradient from one area to the next. What areas? T cell zones. Naive T cells lymphocytes and DC cells connect, starts clonal expansion of T cells.
DC is migrating:
Shifts from antigen capture to stimulating T lymphocytes, increase or upregulation of MHC expression indicates this shift.
How long can it take for T cell response?
Takes 12-18 hours from antigen entering body to T cell response.
Dendritic cells are…
the main APCs to induce T cells. They can move specifically to lymph nodes and secondary lymphoid organs.
Other APCs?
Macrophages are important for inducing helper T cells (CD4+ effector T cells in the effector phase of cell-mediated immune response), along with B lymphocytes, as they endocytose protein antigens for helper T cells in lymphoid tissues (important for development of humoral immunity). Also, any nucleated cell can present antigens via MHC class I to CD8+ T cells (killer T cells).
The Major Histocompatibility Complex (MHC)
Is the Cornerstone of the adaptive immune system. Originally discovered in experimenting with tissue grafts (self vs nonself) Referred to as HLA (human leukocyte antigen) in humans. Women were making more antibodies against paternal leukocytes in pregnancies and leukocytes in blood transfusions. (Making antibodies against leukocytes).
Two main classes of MHC:
I and II
Using MHC what can we do genetically?
We can predict compatibility of alleles and Locuses as they have different patterns and levels of being condensed.
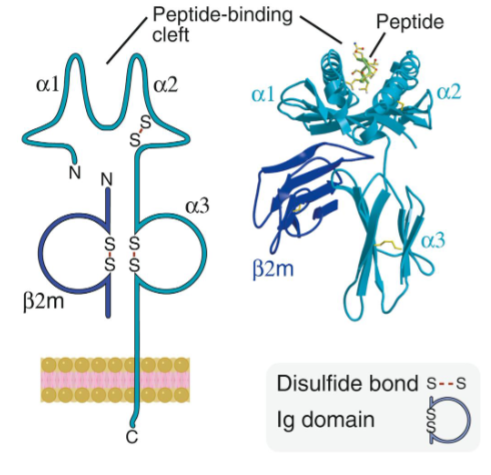
What class is this?
Class I MHC
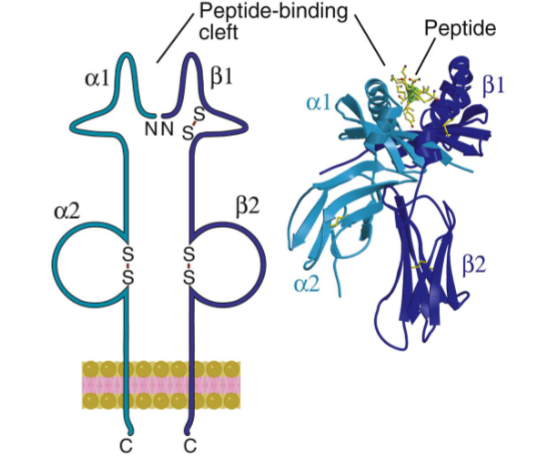
What class is this?
Class II MHC, note the set of alphas and betas. Inheritance plays much more of a role in this.
MHC genes and proteins are
Highly polymorphic within an individual and within populations. Also have genetic compatibility. Class I are found on all nucleated cells. Class II are mainly found on APCs (except thymic epithelial cells).
HLA is estimated
to have about 10,500 Class I and 3500 Class II alleles within the entire population of humans
Inheritance patterns (in humans)
There are three MHC class I genes (HLA-A, B, C). One cell can express up to six different class I molecules (if each one has a different allele). MHC class II involves being inherited from each parent, (depends on parents, will not always be the same alpha and beta chains). The aplha and beta chains can interact across chromosomes and express different combinations.
A set of genes is called
MHC haplotype. Important for bone marrow or tissue donor, it is important to know your alleles, there must be matches.
Peptide binding to MHC molecules
Peptide/antigen binding clefts (ABCs, PBC, PBR) only certain amino acids within a cleft bind to residues on the peptide (anchor residues) Peptides also have residues that are recognized by TCRs—Highly specific! One MHC does not present only one antigen but can present many if they have similar anchor residues.
Greater diversity of MHC=
wider range of peptide recognition
MCH has broad specificity, true or false?
True, it can bind many different peptides on the same MHC molecule.
MHC I class will be more in the…
cytosol
External, extracellular bacterium would interact with?
Class II MHC
Viruses would interact with?
Class I MHC (intracellular)
Does MHC have a slow off rate?
Yes, to ensure that the bound peptide is displayed long enough to be recognized by T helper cell.
Heterozygosity (Aa) is
good for a population, has more fitness.
More alleles generally equals
less infection risk. (Not always the case though!)
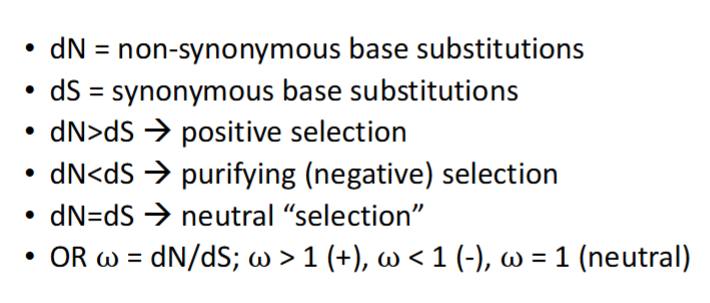
What is this detailing?
MHC diversity and patterns of molecular evolution on codons.
As we evolve (to be ahead of pathogens as they evolve) we get small changes to amino acid sequences. What amino acids might get dN>dS or positive selection?
The ones that can bind to the selective MHCs.
Selection is…
hard to measure between one generation. Easier to measure over evolutionary and population history. If we have the history of pathogens and their shifts it is easier to measure, along with seeing the closeness of alleles between related species for fighting off pathogens.