Ch16 Pulmonary Ventilation
1/75
Earn XP
Description and Tags
APK2105C @ UF w/ Dr. Nguyen | Module 4 | Ch16 Pulmonary Ventilation
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
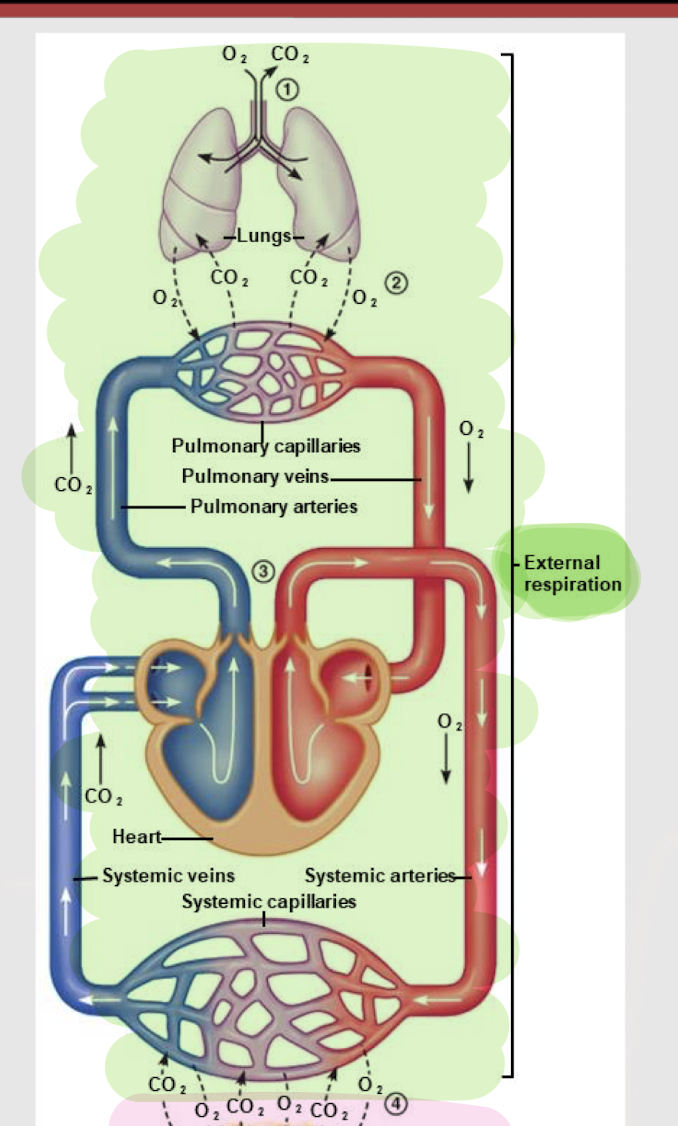
external respiration
Exchange of gases b/t the atmosphere and body tissues
internal respiration
Use of O2 at the mitochondria to generate ATP via oxidative phosphorylation and the resulting production of CO2
ventilation; lung air; blood; lungs; tissues; blood; tissues
4 processes of external respiration:
Pulmonary ________ (i.e. breathing)
Exchange of gases b/t _____ ____ and ______ via diffusion
Transportation of gases b/t _______ and _______
Exchange of gases b/t _______ and ______ via diffusion
nasal/oral cavity, pharynx, larynx
What are the 3 main structures of the upper respiratory tract?
less; defense against pathogens
As you move down the conducting zone, do you find more or less cilia and goblet cells? What is their function?
more; bronchoconstriction/dilation
As you move down the conducting zone, do you find more or less smooth muscle? Why?
no; could impede gas exchange
Will you find other structures/tissues in the respiratory zone (i.e. respiratory bronchioles + alveolar sacs)? Why or why not?
conducting zone
The airways that transport air to the lungs w/o participating in gas exchange, including the trachea, bronchi, and bronchioles.
respiratory bronchioles; alveoli
The respiratory zone (i.e. where gas exchange occurs) is made up of _______ ______, alveolar ducts, alveolar sacs and _______.
anatomical dead space
Volume of air in the conducting zone that doesn’t make it to the respiratory zone for gas exchange.
150mL
What is the typical volume of the anatomical dead space?
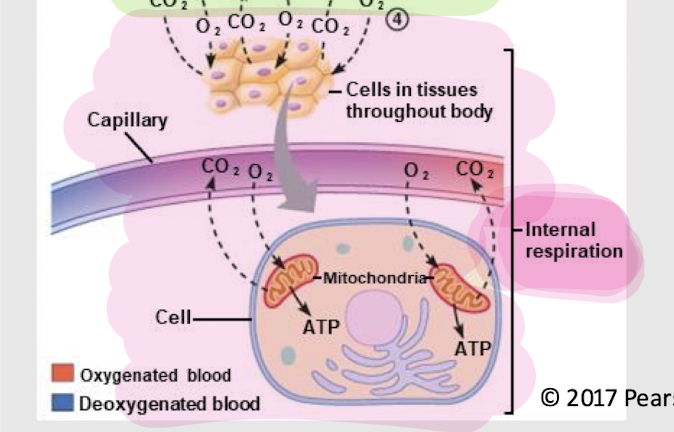
capillary network, alveolar pores, elastic fibers
What are the 3 physical characteristics of alveoli?
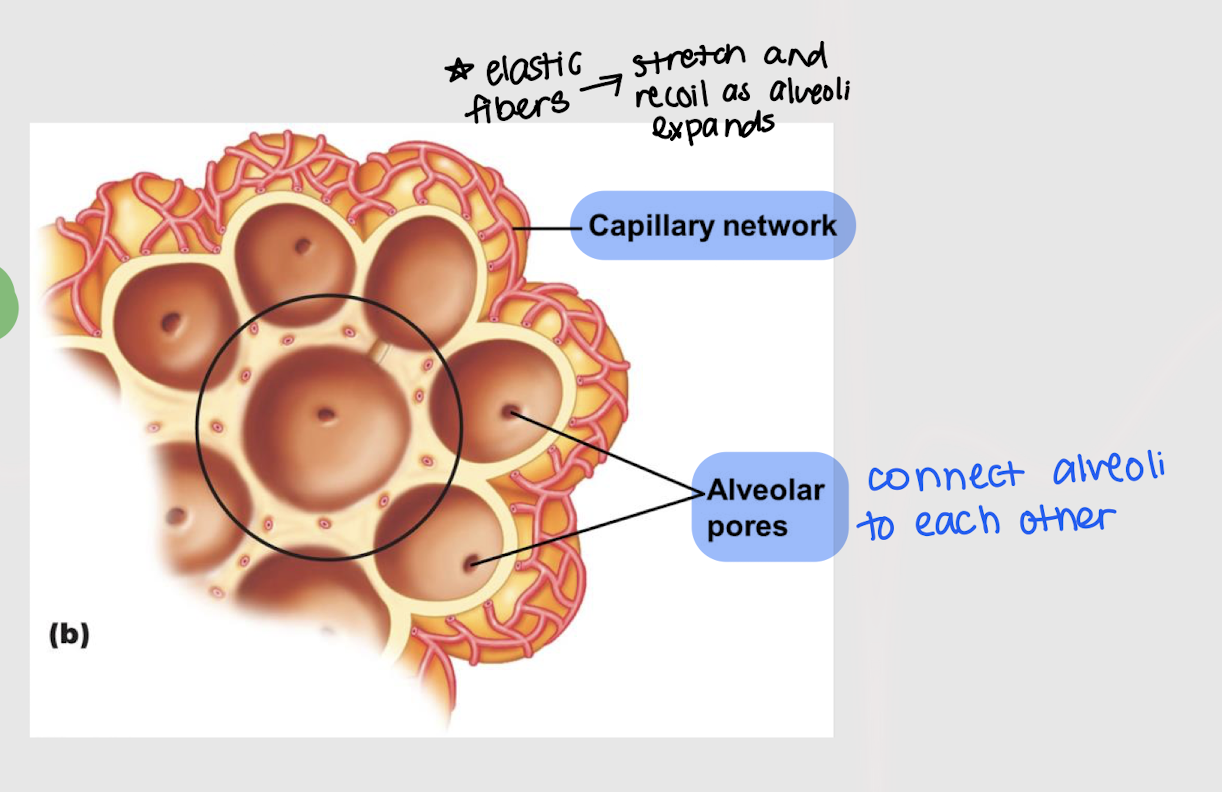
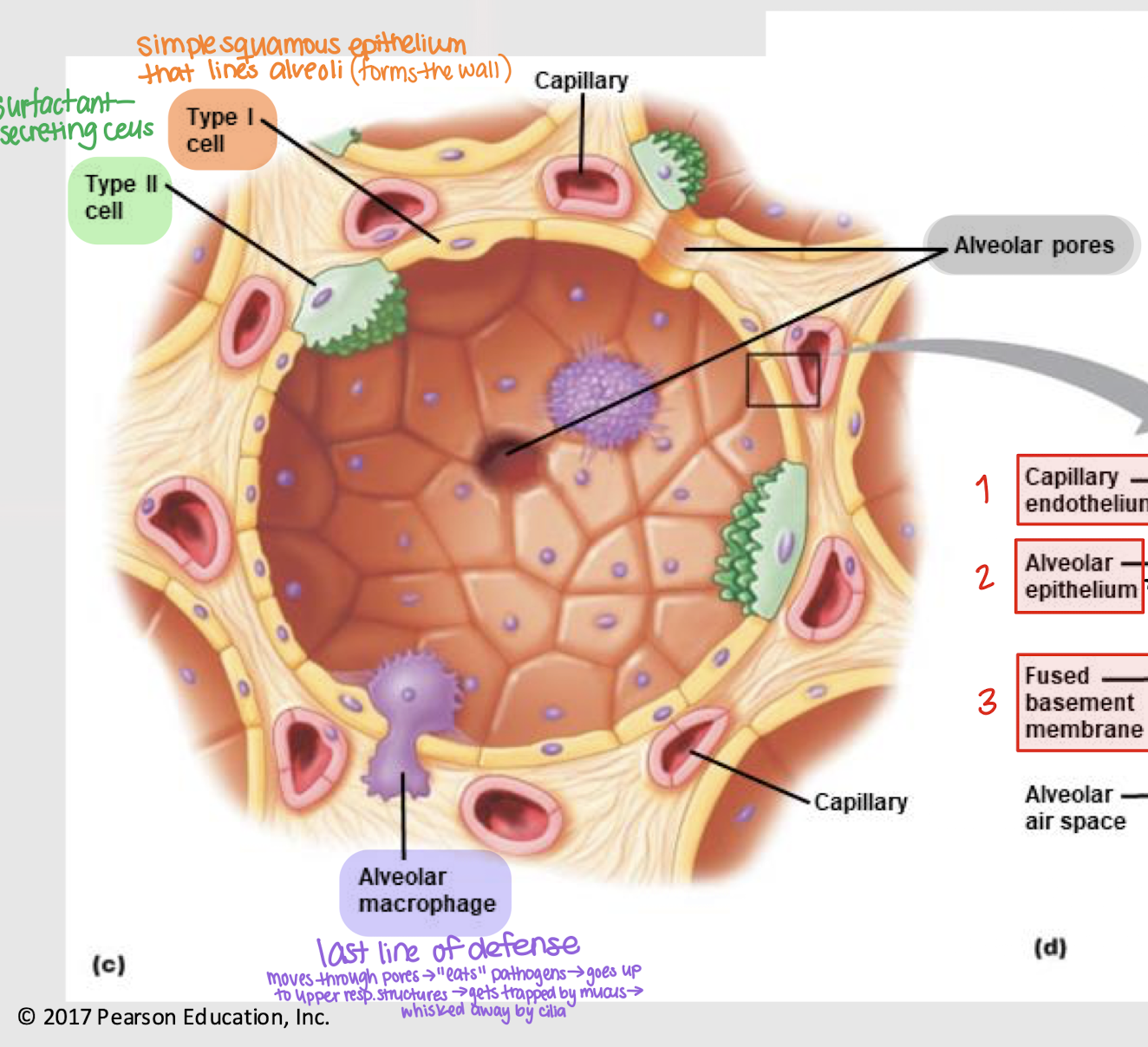
respiratory membrane
The thin respiratory membrane that separates air from blood
Type I cell
Simple squamous epithelium that line the alveoli, forming the wall
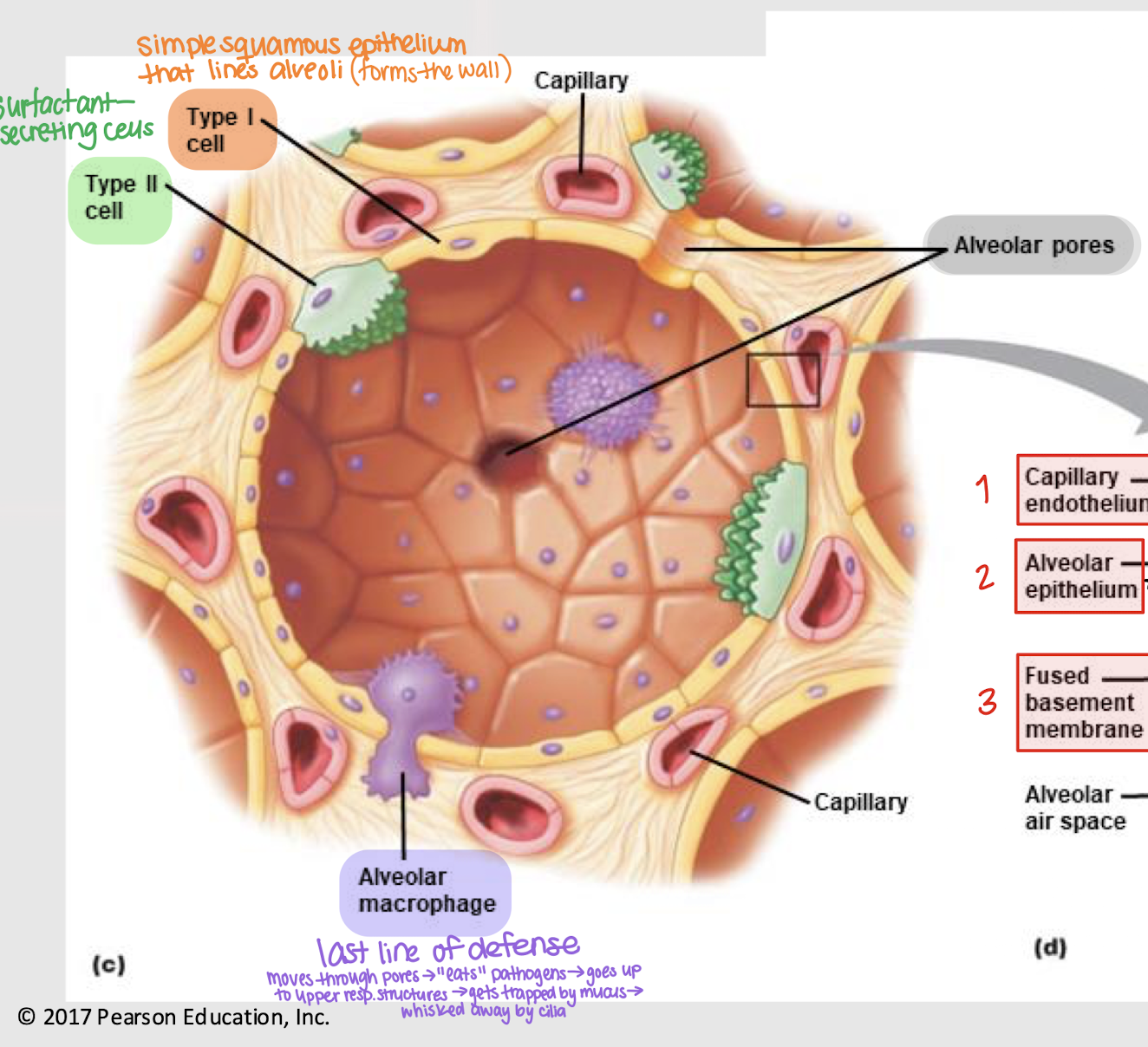
Type II cell
Surfactant-secreting cell that helps in relieving surface tension
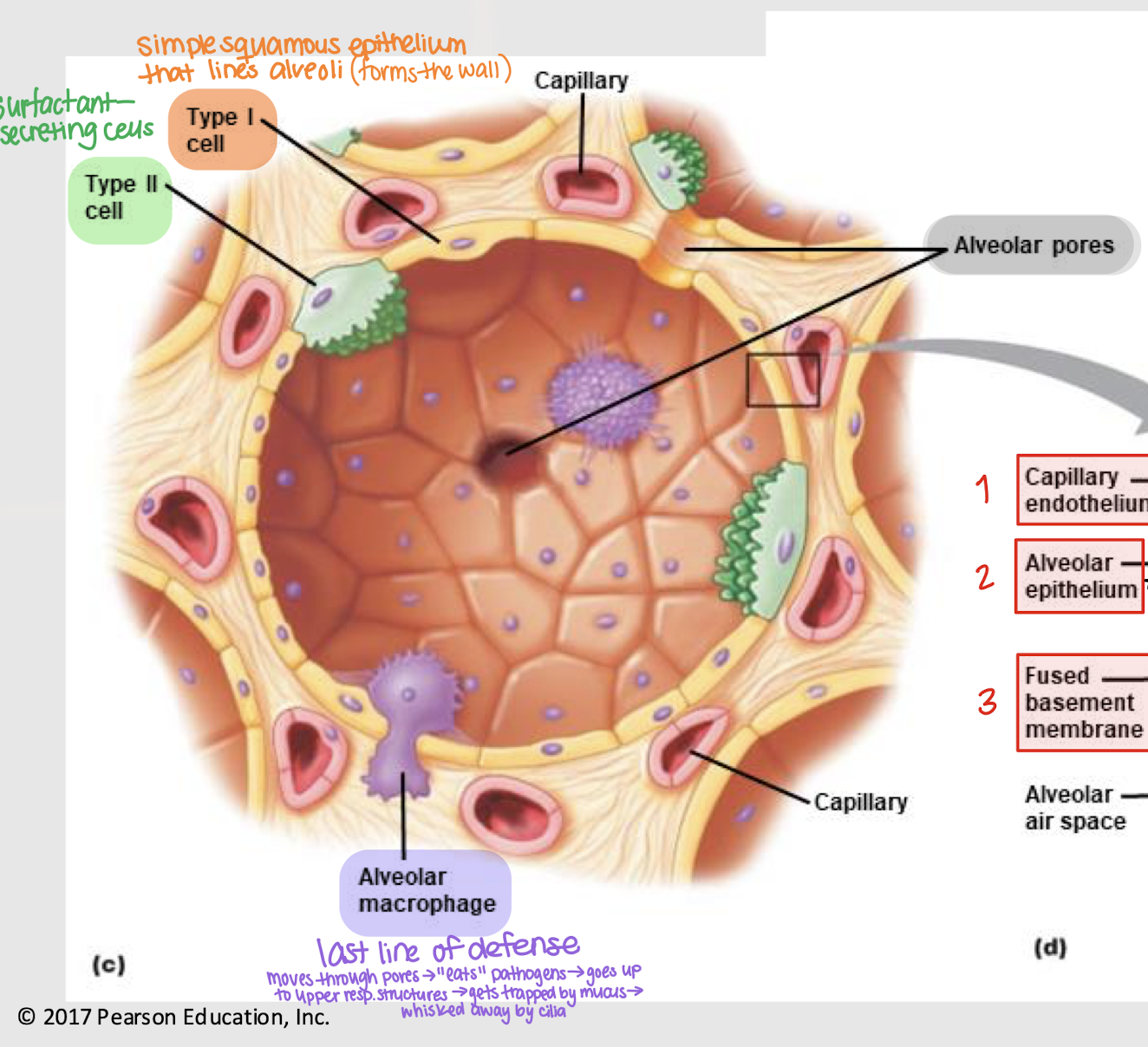
alveolar macrophages
Cells in the alveoli that act as a last line of defense
Move through pores → “eat” pathogens → go up resp. structures → get trapped by mucus → whisked away by cilia
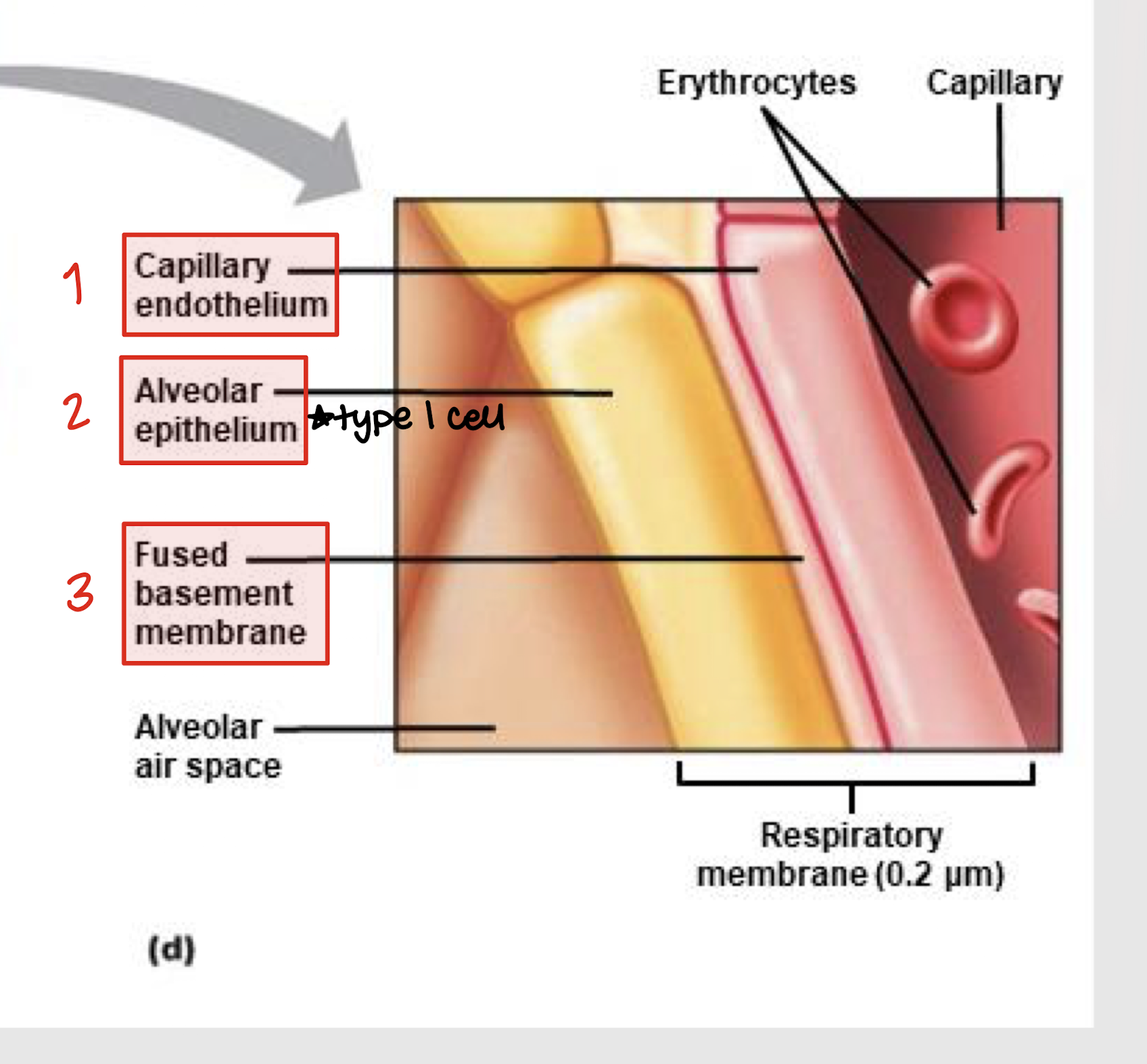
capillary endothelium, alveolar epithelium, basement membrane
What are the 3 structures that make up the respiratory membrane?
diffusion
How does gas exchange occur in the pulmonary system?
thin; surface area
2 factors that make gas exchange (diffusion) a fast process:
_____ respiratory membrane (minimal barrier)
Huge ________ _____ (huge blood supply to alveoli)
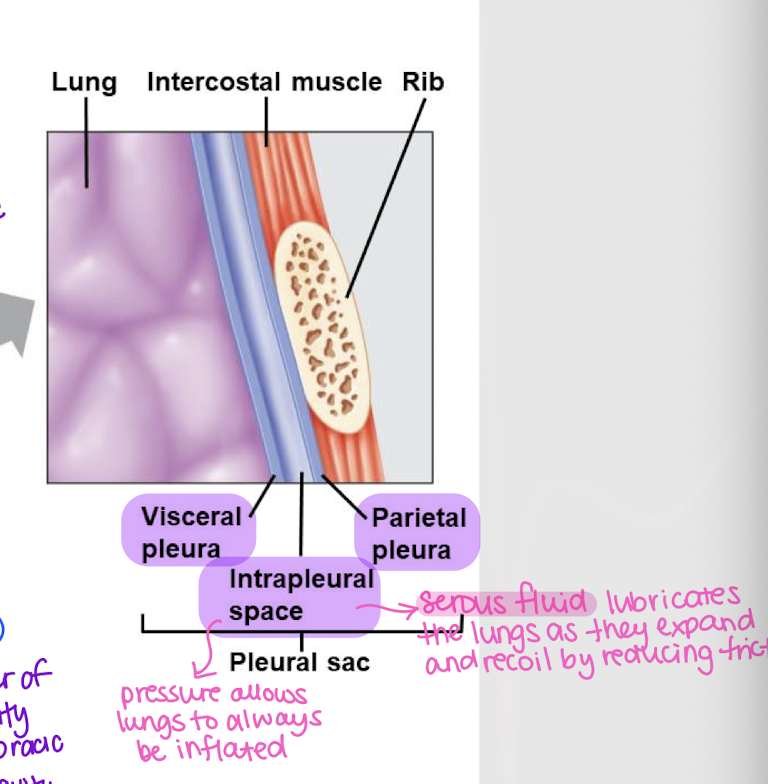
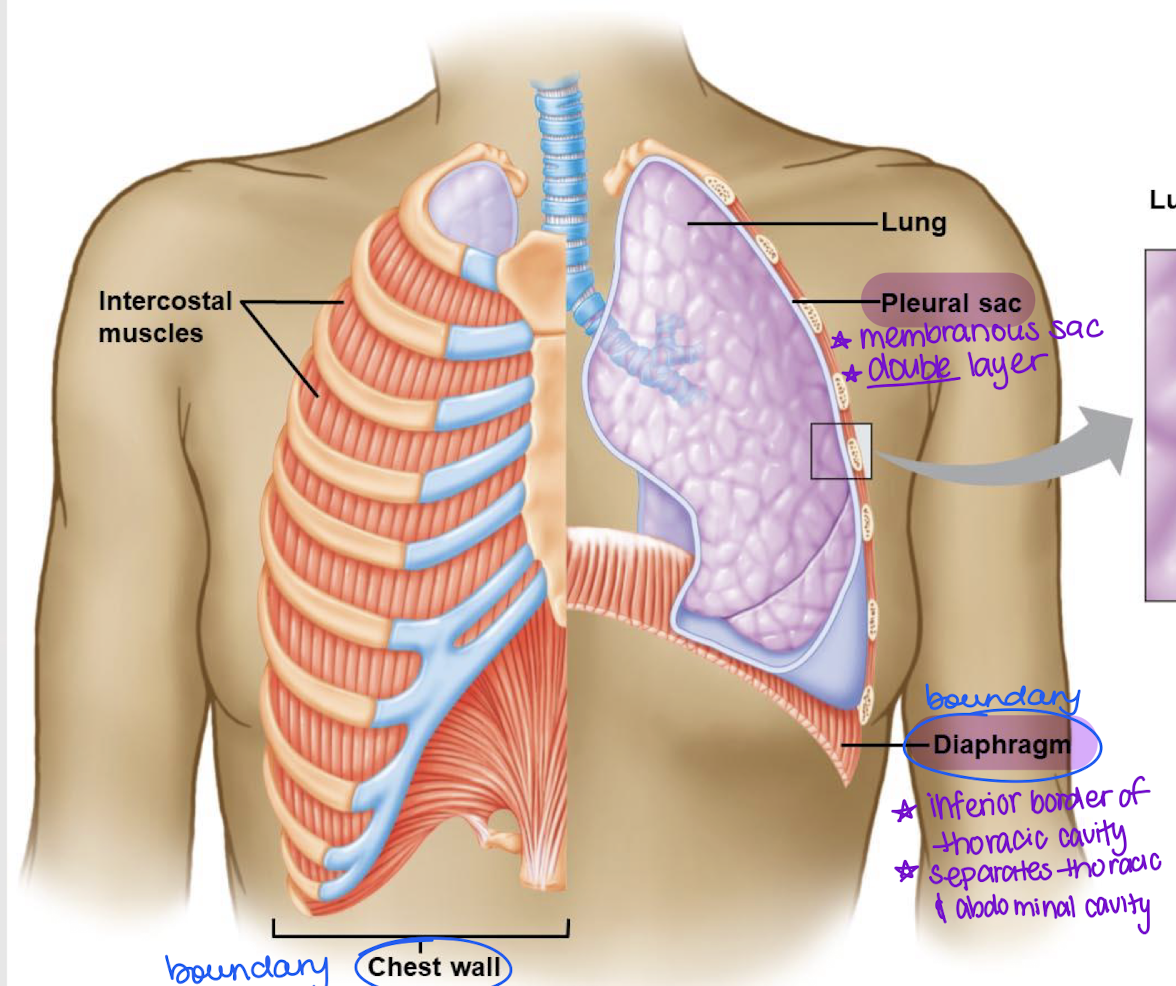
visceral and parietal pleura; simple squamous epithelium
What are the 2 layers of the pleural sac? What tissue is the pleura made up of?
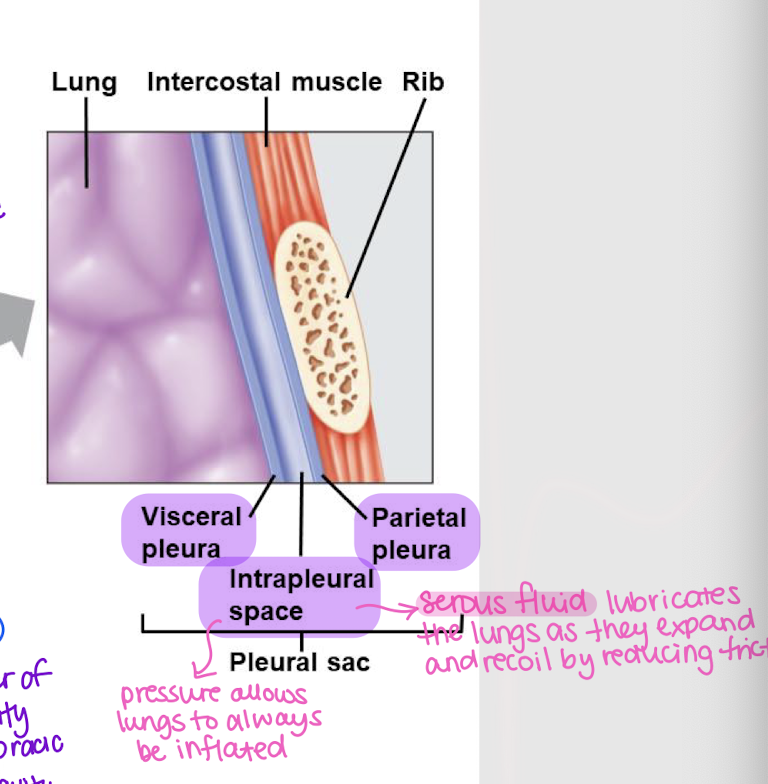
intrapleural space
Space that allows the lungs to expand w/o collapsing by creating a pressure gradient
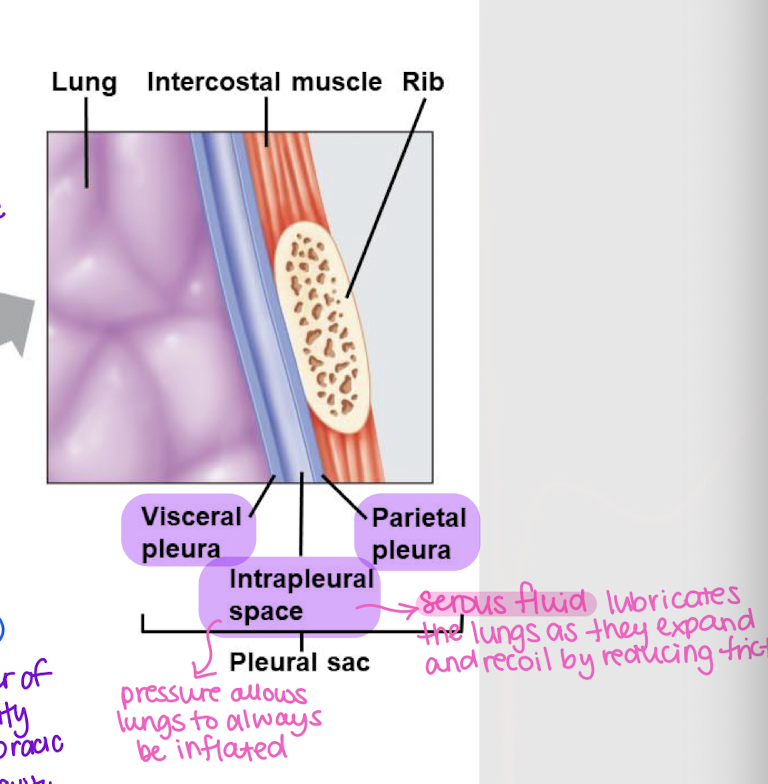
serous fluid
What is found in the intrapleural space that lubricates the lungs as they expand and recoil, reducing friction?
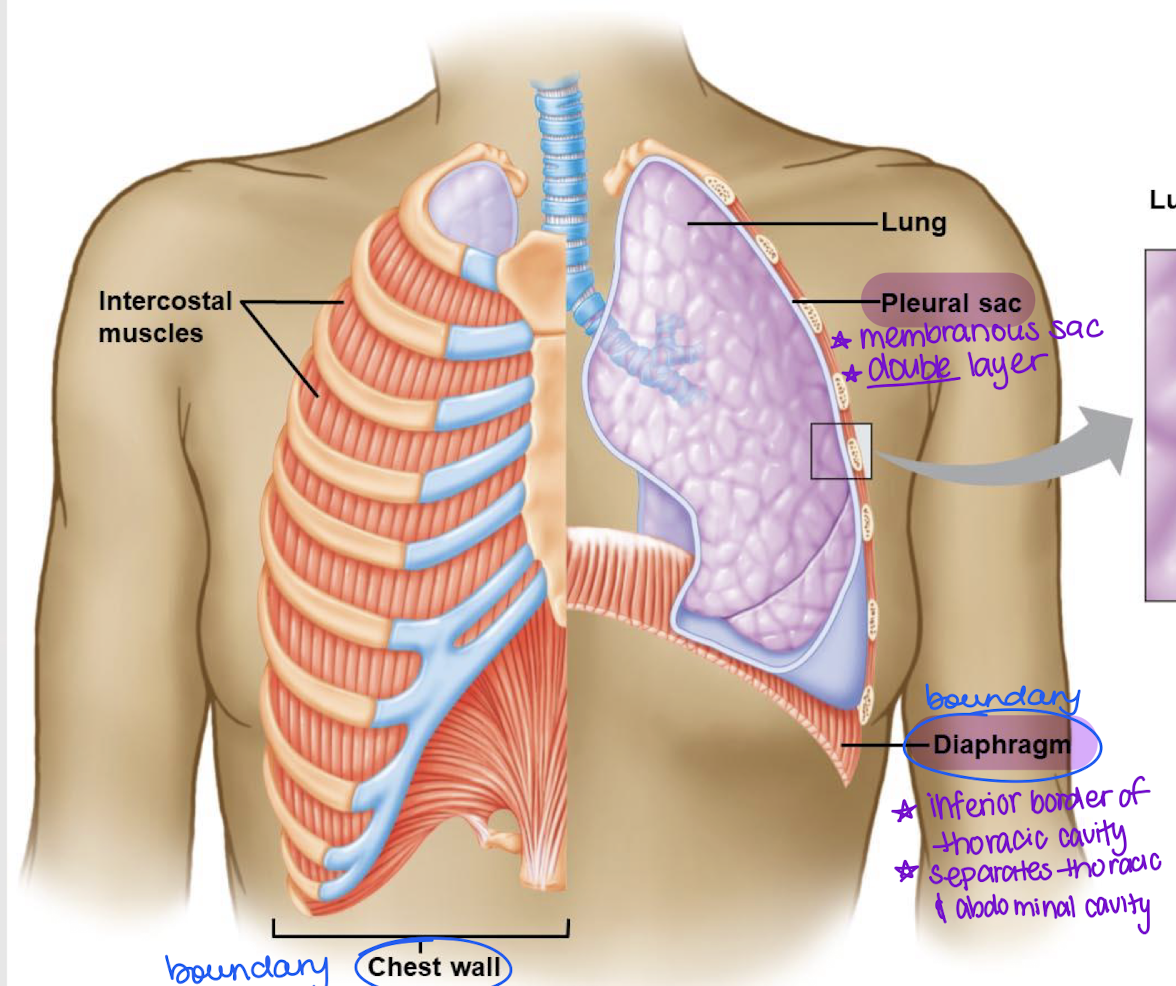
diaphragm
Inferior border of the thoracic cavity
Separates the thoracic cavity from the abdominal cavity
lubrication; compartmentalization; pressure
Pleural functions:
________ b/t moving organs
___________ of the thoracic cavity
Intrapleural ________ keeps the lungs partially expanded at all times
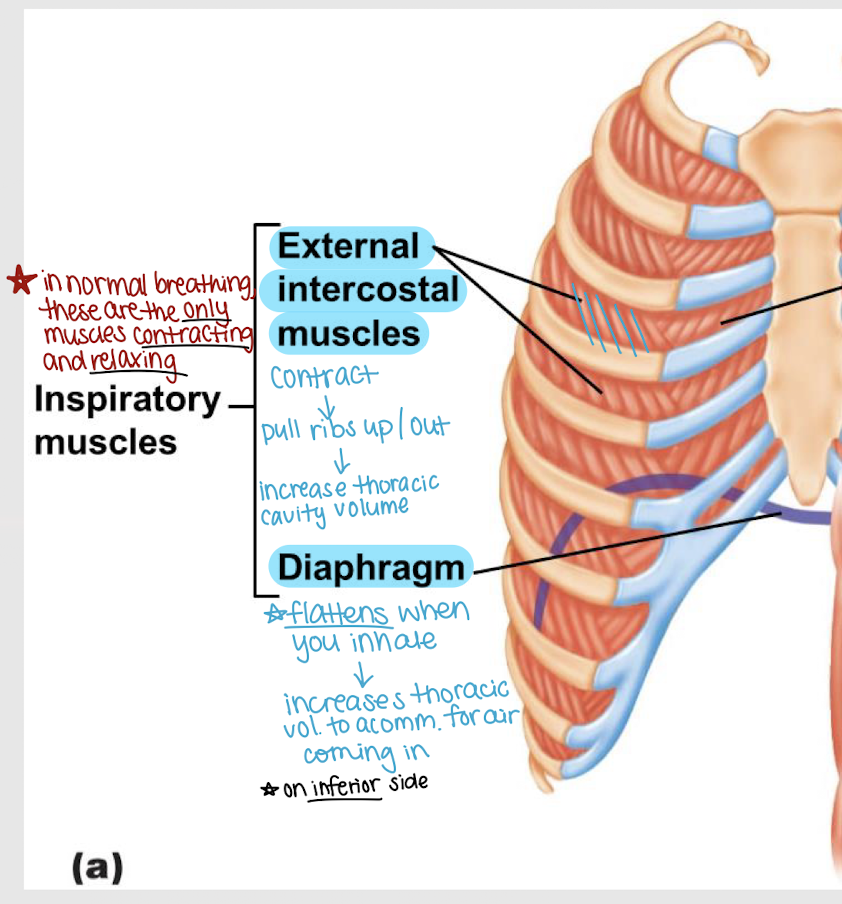
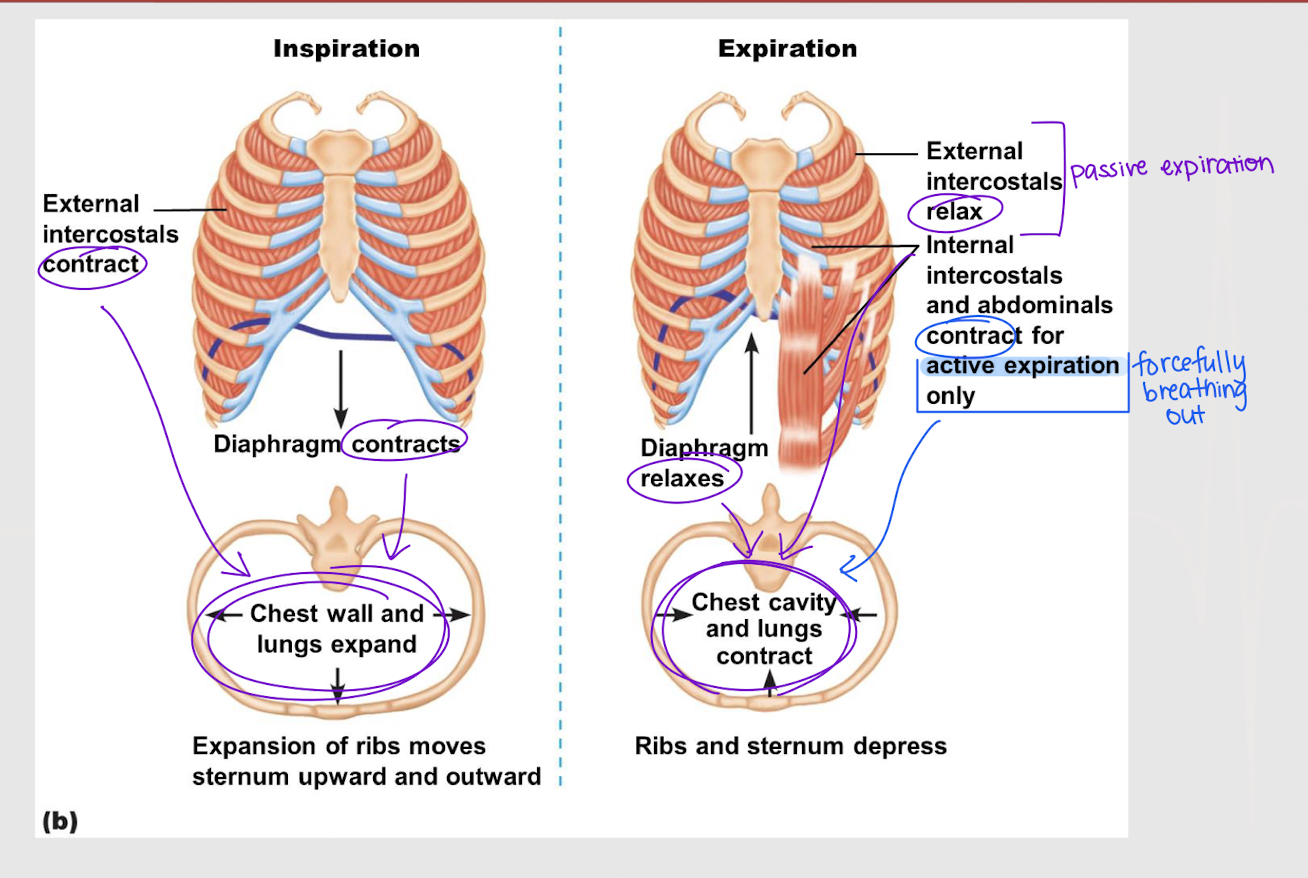
external intercostal muscles
Inspiratory muscles:
contract → pull ribs up/out → increase thoracic cavity volume
diaphragm
Inspiratory muscles:
inhalation → muscle flattens → increases thoracic volume (to accommodate for air coming in)
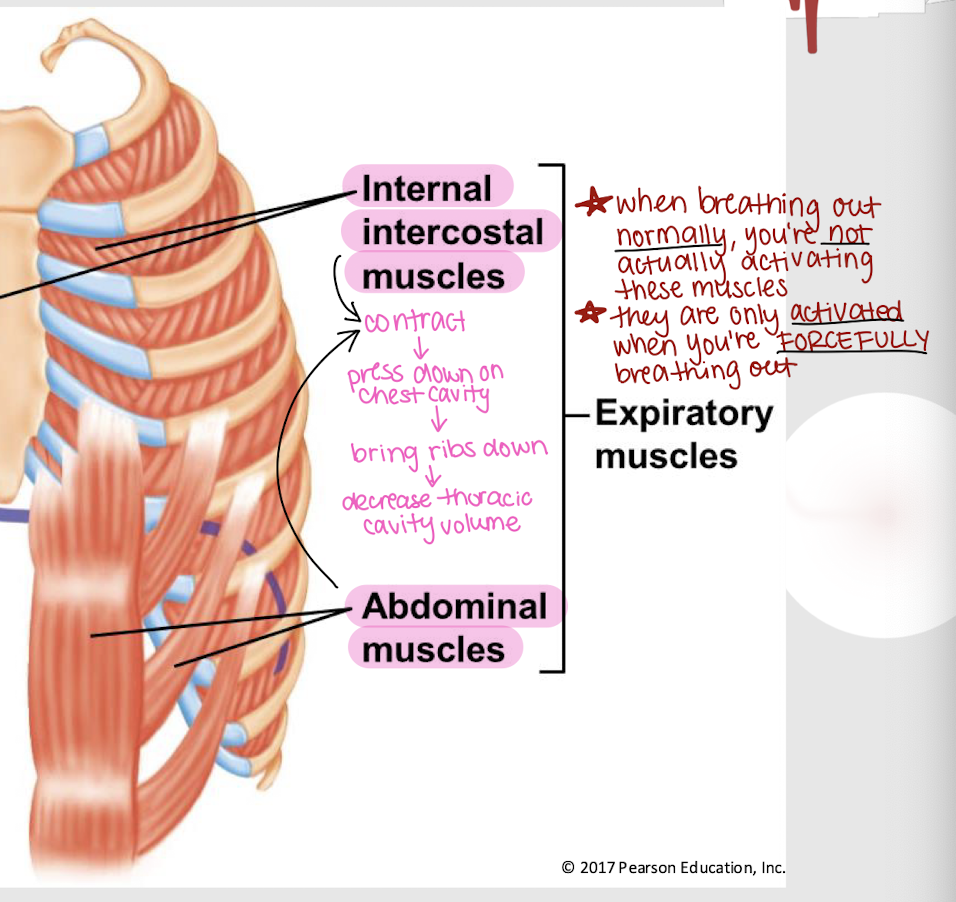
internal intercostal muscles and abdominal muscles
Expiratory muscles (2):
contract → press down on chest cavity → bring ribs down → decrease thoracic cavity volume
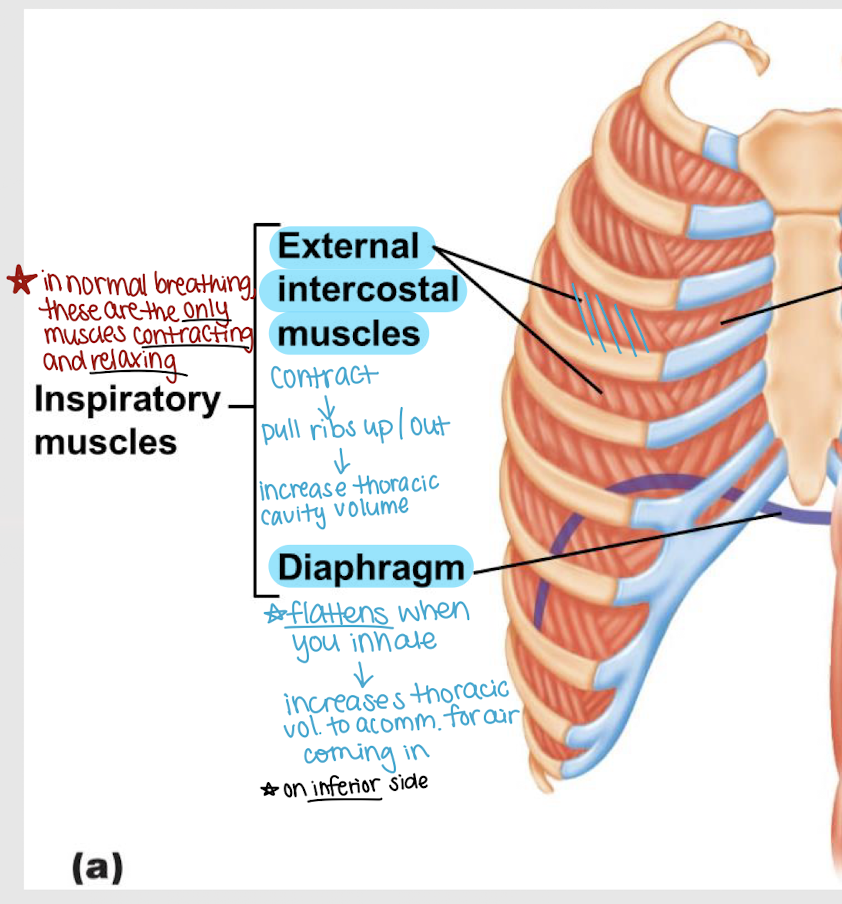
external intercostal muscles
In normal breathing, which muscles are the only ones being used?
forceful exhalation
Internal intercostal muscles get activated during _______ _______.
functional residual capacity (FRC)
Lung capacities:
Volume of air in the lungs after normal exhalation (ERV + RV)
All forces acting on the lung and chest wall are balanced (i.e. no pressure gradient)
inspiration; expiration
Intra-alveolar pressure (Patm)
At rest, Palv = Patm
During _______, Palv < Patm
During _______, Palv > Patm
intrapleural pressure (Pip)
Lung pressures:
Changes w/ phases of ventilation, but
Is always less than Patm (i.e. negative relative to Patm)
transpulmonary pressure
Lung pressures:
Pressure difference across the entire lung, calculated by Palv - Pip
inflated; pneumothorax
A negative Pip (relative to Patm) allows the lungs to remain ________. What would happen if Pip = Patm?
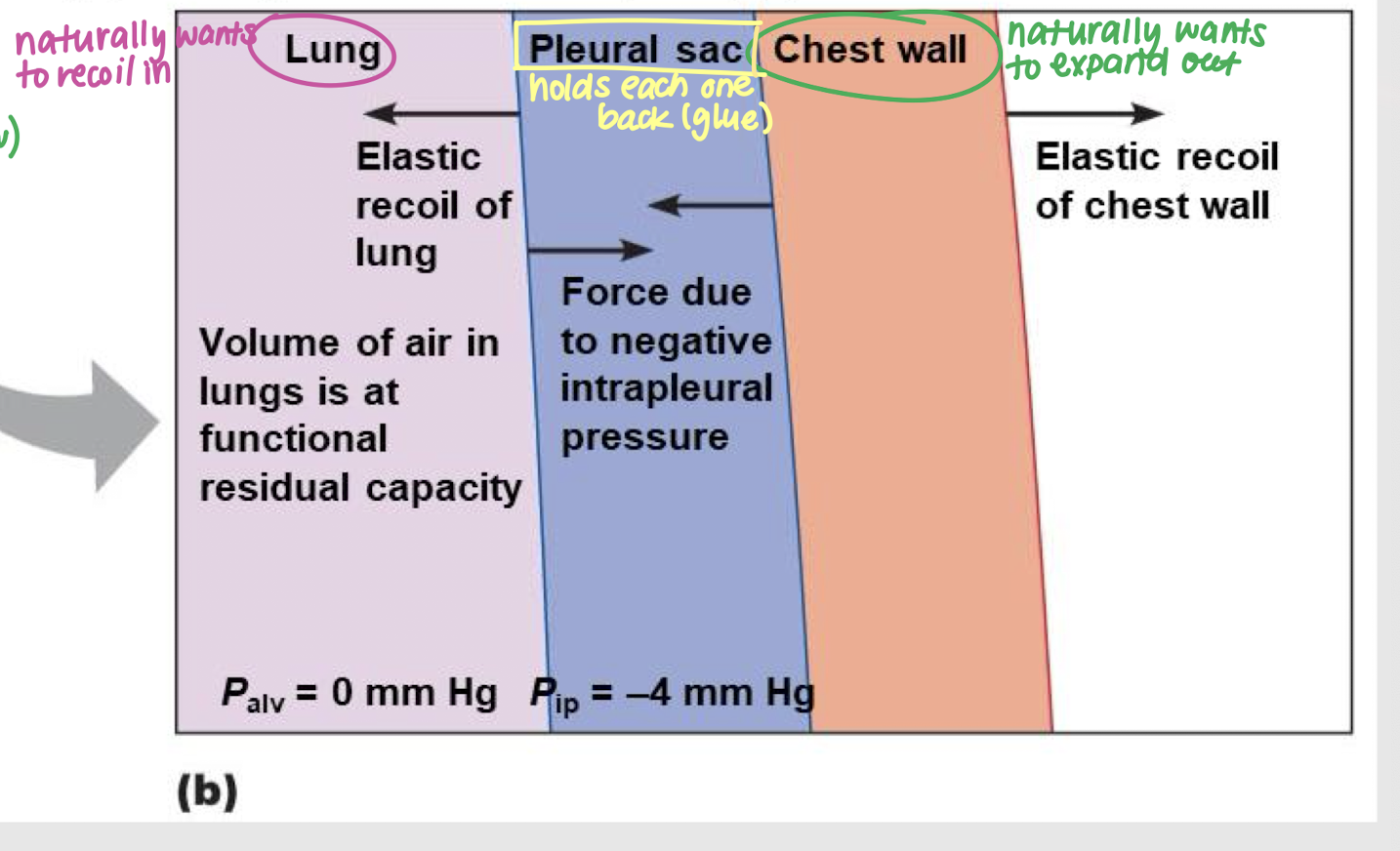
in; 0; -4; bulk flow
Due to elasticity, the lungs naturally want to recoil ____. However, Palv = ___ (FRC) and Pip = ___, so _____ _____ grants the pleural sac enough force to prevent the lung from collapsing.
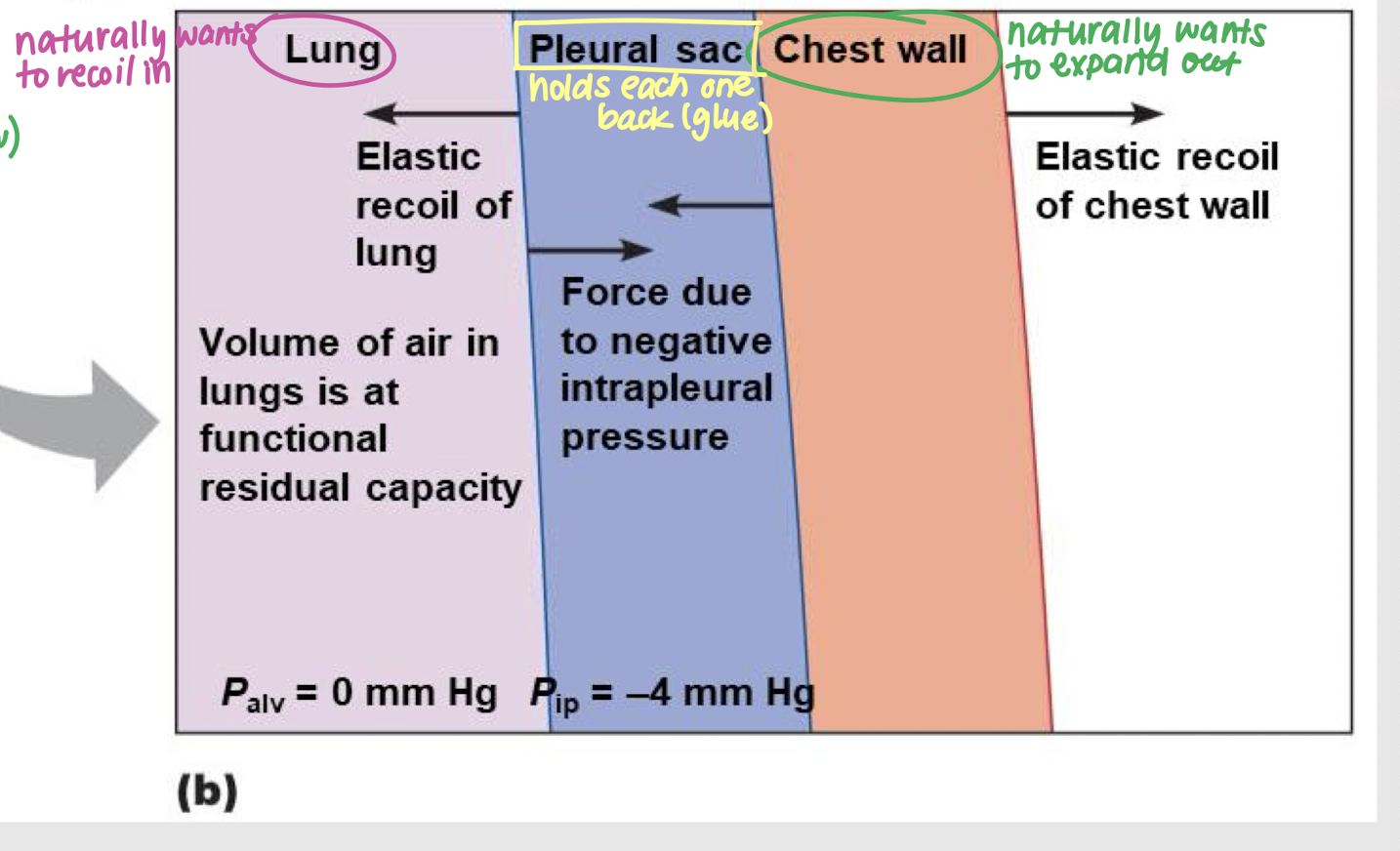
out; -4; bulk flow
Due to elasticity, the chest wall naturally wants to recoil ____. However, since Pip = ____, _____ _____ grants the pleural sac enough force to keep the chest wall from expanding.
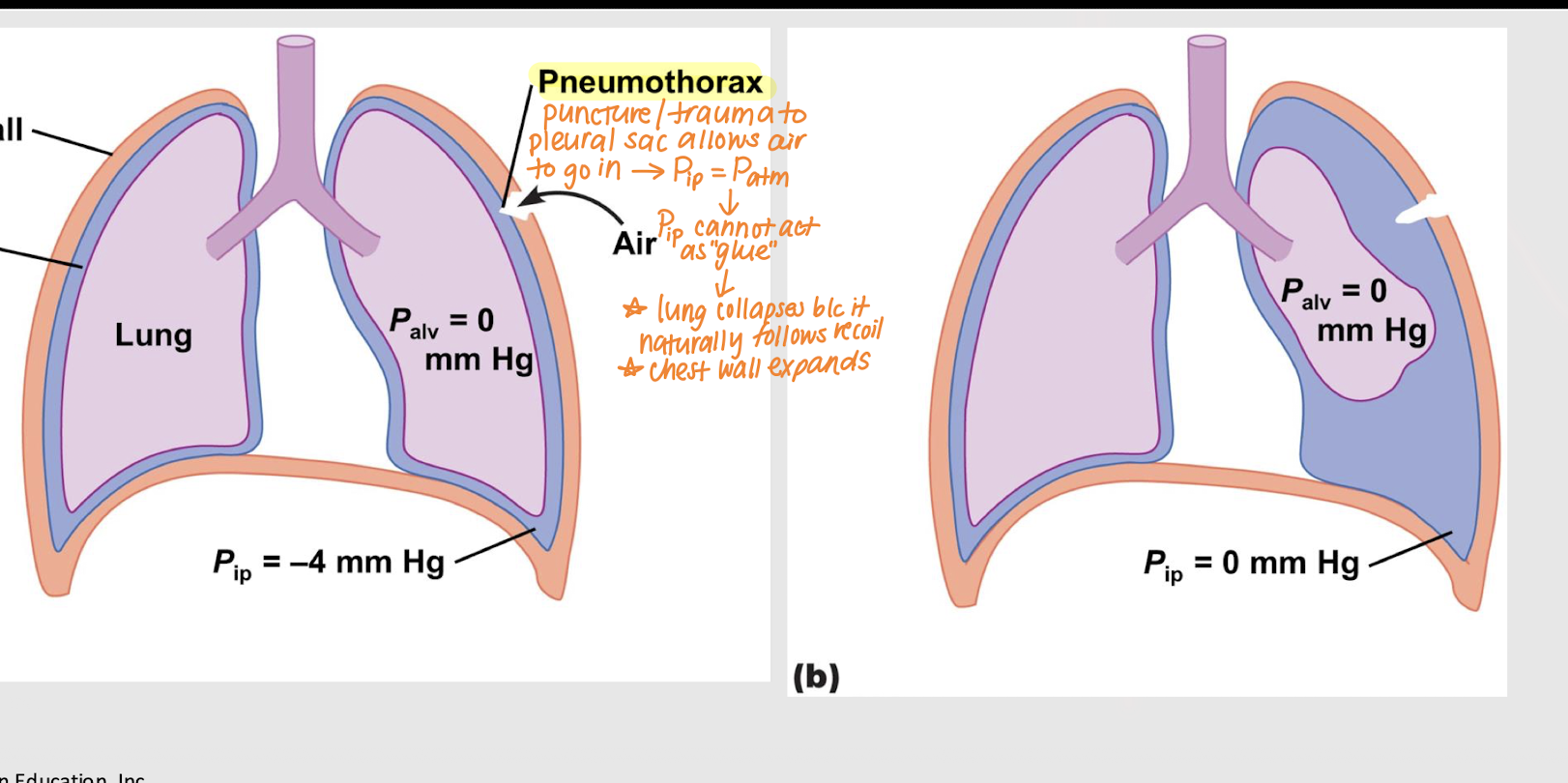
=; Pip; collapses; expands
Pneumothorax (collapsed lung):
Trauma/puncture to pleural sac → air comes in → Pip ___ Patm → ___ unable to hold lungs and chest wall → lung ____ and chest wall _____
air flow; Palv
What does this equation represent? Patm - Palv / R
Which of these terms determine the direction of air movement?
volume; thoracic; quantity
2 determinants of Palv:
Alveolar _______ (i.e. size)
Changes are produced by changes in the ________ cavity due to respiratory muscles expanding or compressing it.
________ of air molecules in the alveoli.
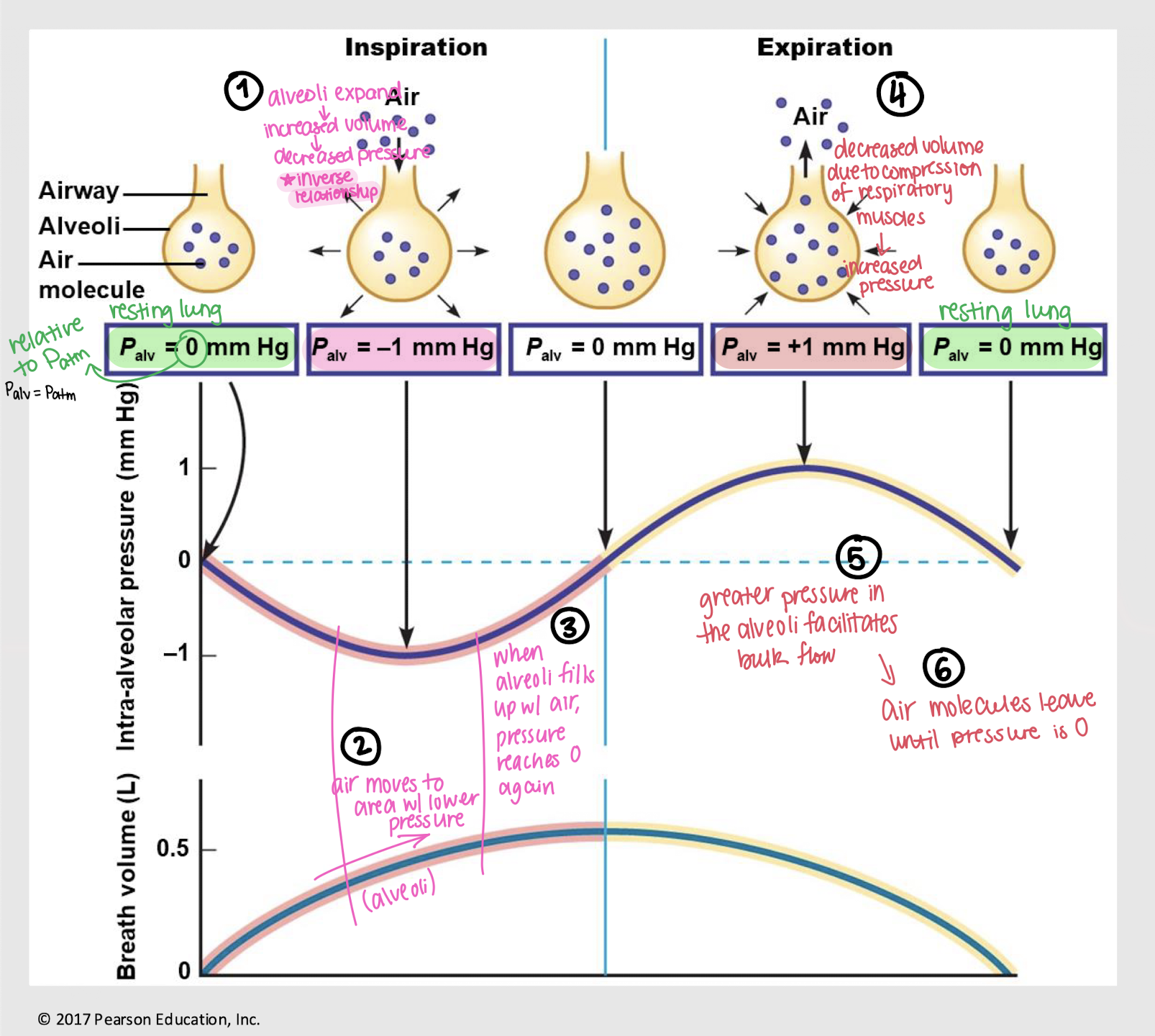
increased; decreased; into; decreased; increased; leaves
Thoracic volume impacts alveolar volume:
Inspiration: Alveoli expand → _______ volume → _______ pressure
Bulk flow: Air moves ____ alveoli, until pressure reaches 0
Expiration: Compression of respiratory muscles → _______ volume → _______ pressure
Bulk flow: Air ______ alveoli, until pressure reaches 0
lung compliance; airway resistance
2 factors impacting pulmonary ventilation:
______ ______: ease of alveolar distention
______ ______: resistance of entire system of airways
smaller; larger; inspiratory
Larger compliance means that a ______ change in transpulmonary pressure results in a ______ volume of air brought in. (This requires less muscular work and thus less energy.)
Such a change in transpulmonary pressure means ________ muscles contracted but they didn’t have to put in a lot of effort to pull on pleura.
elasticity; surface tension
Lung compliance depends on:
_______ of lungs
_______ _______ of water lining the alveoli
high; more
______ surface tension requires _____ muscular work to decrease Pip
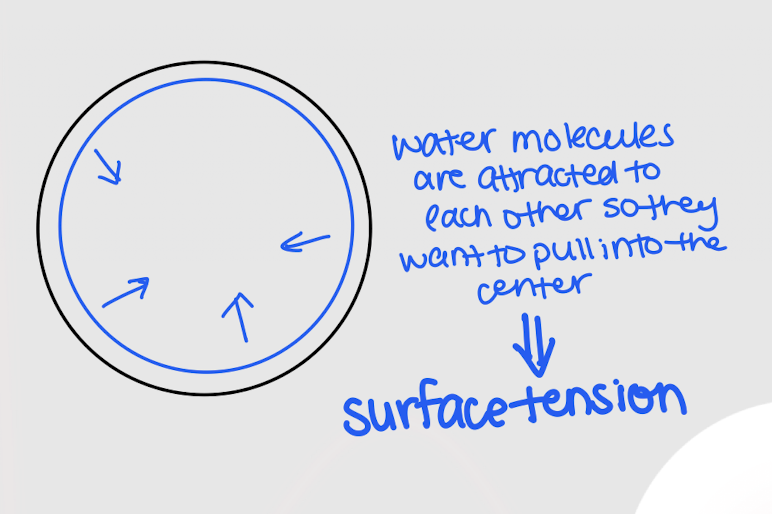
directly; inversely
The pressure necessary to prevent alveolar collapse (P) is _______ proportional to surface tension (T) and _______ proportional to alveolar radius (r)
P = 2T / r
pulmonary surfactant; decreases; increases; decreases
Detergent-like substance secreted by Type II cells that helps counter the effects of the water in the alveoli
Decreases/increases surface tension
Decreases/increases compliance
Decreases/increases muscular work
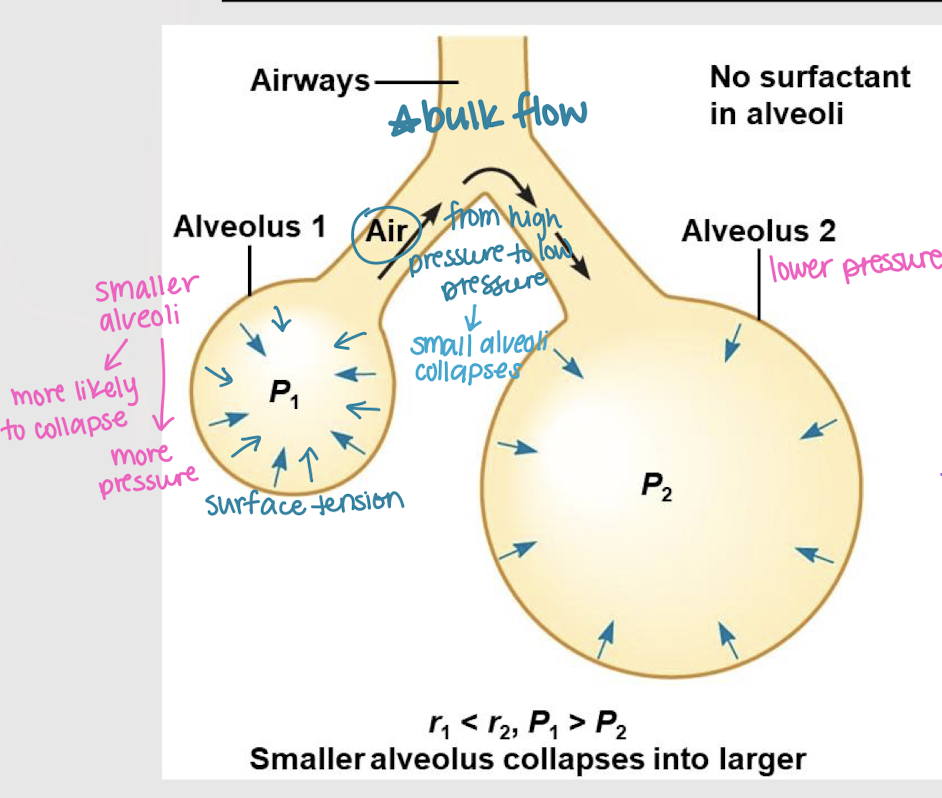
high; more; bulk flow
In a small alveolus, there is _____ surface tension, which generates _____ pressure (Palv). Due to _____ _____, air wants to leave the alveolus into a larger one → alveolar collapse
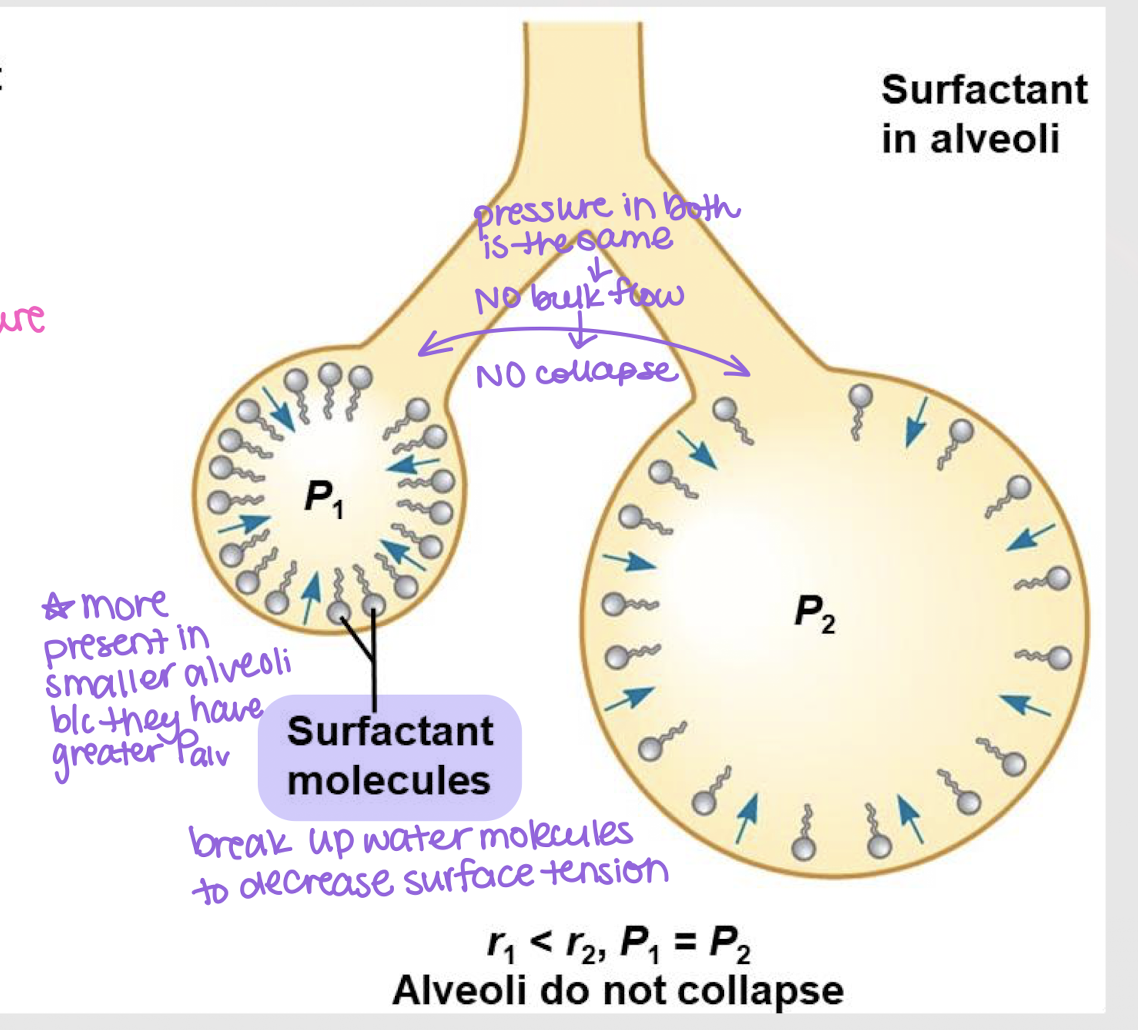
small; greater
Surfactant molecules are more present in ______ alveoli b/c they have _______ Palv.
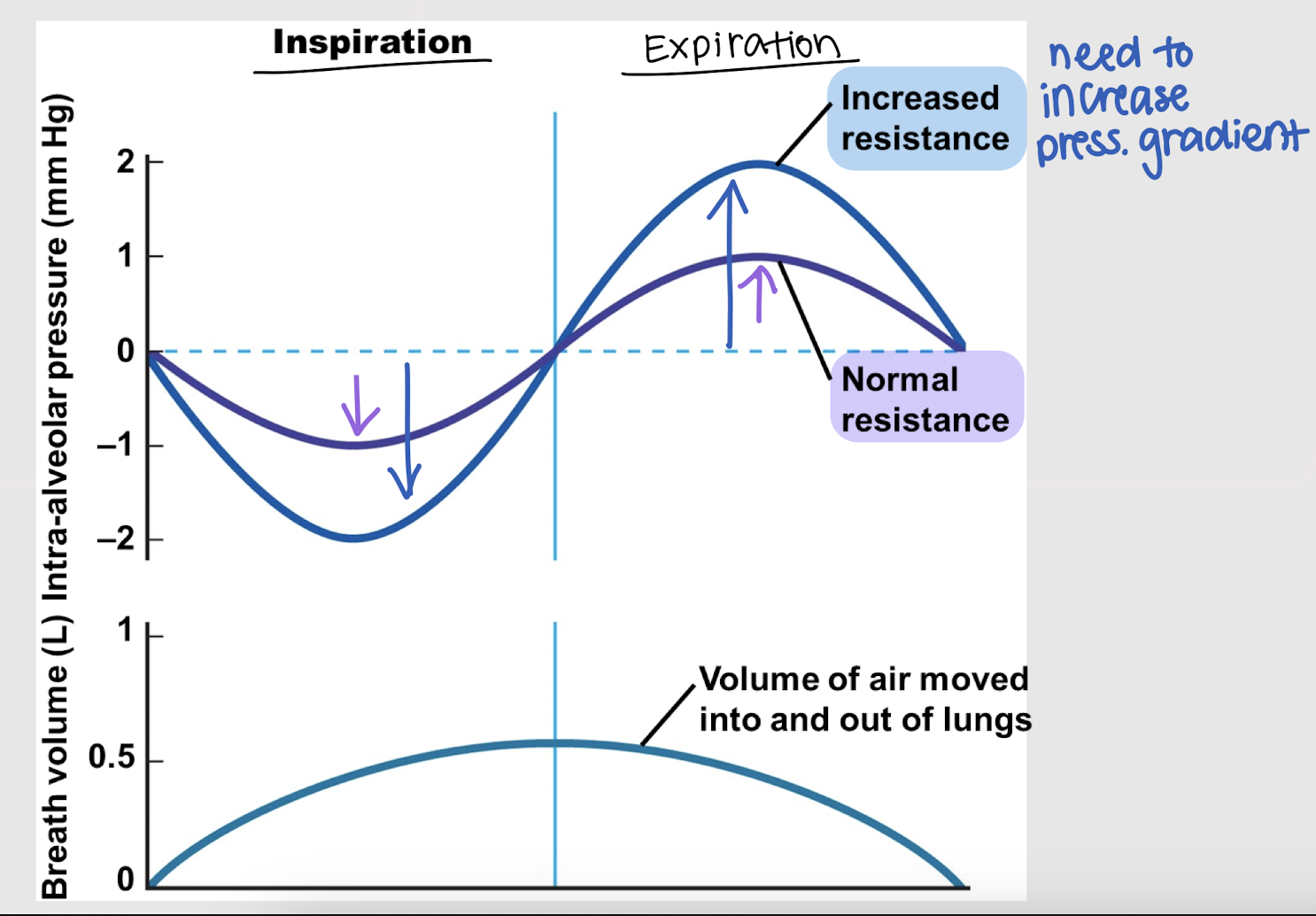
increases
As resistance ________, a larger ΔP (i.e. Patm - Palv) is necessary to produce a given flow gradient.
transpulmonary; bronchoconstriction; bronchodilation; mucous
3 factors affecting airway resistance:
Changes in _________ pressure
Inspiration → pressure increases
Expiration → pressure decreases
_________ and _________
Can be extrinsically or intrinsically mediated
_________ secretion
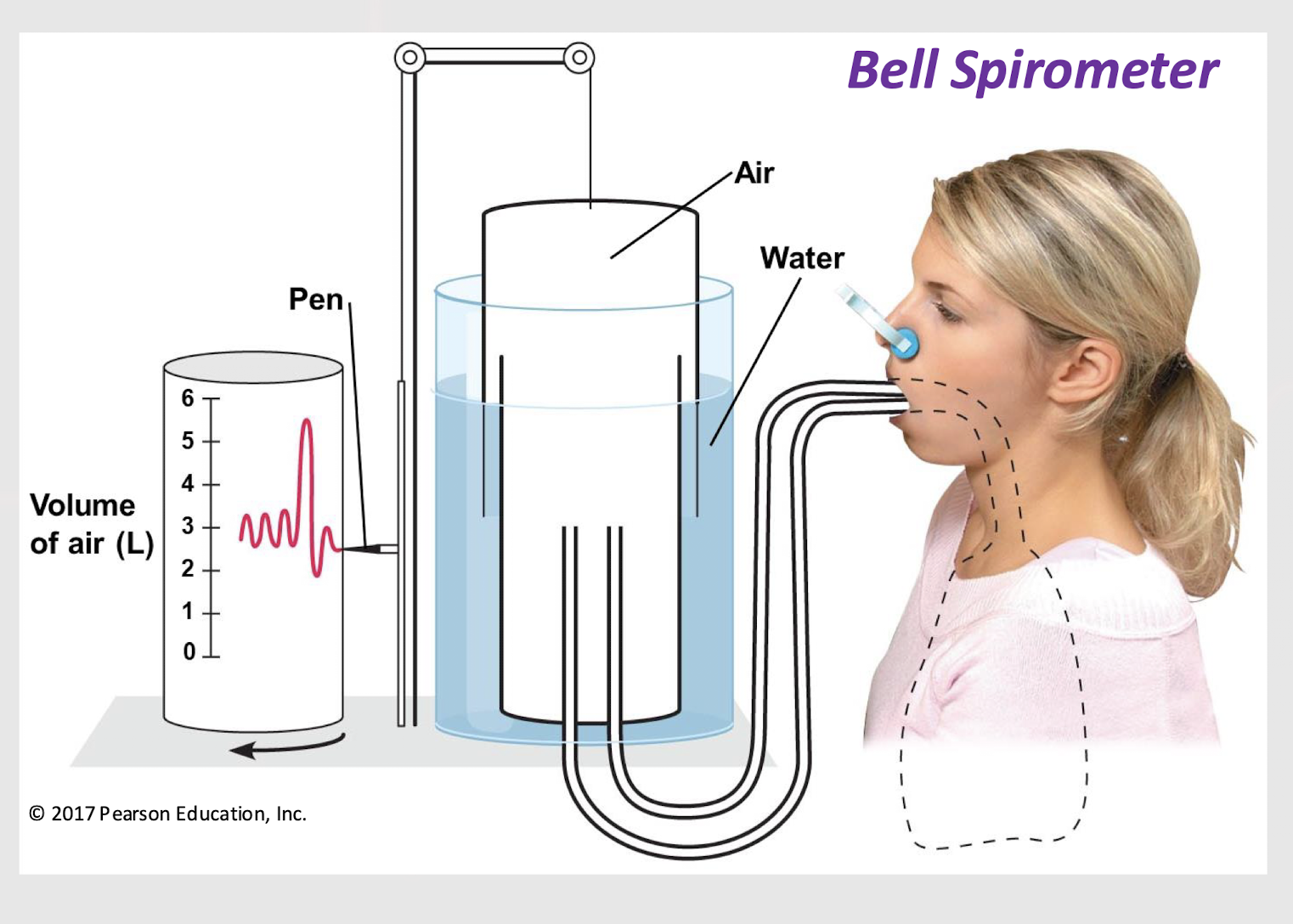
spirometry
Technique for measuring the volumes of inspired and expired air
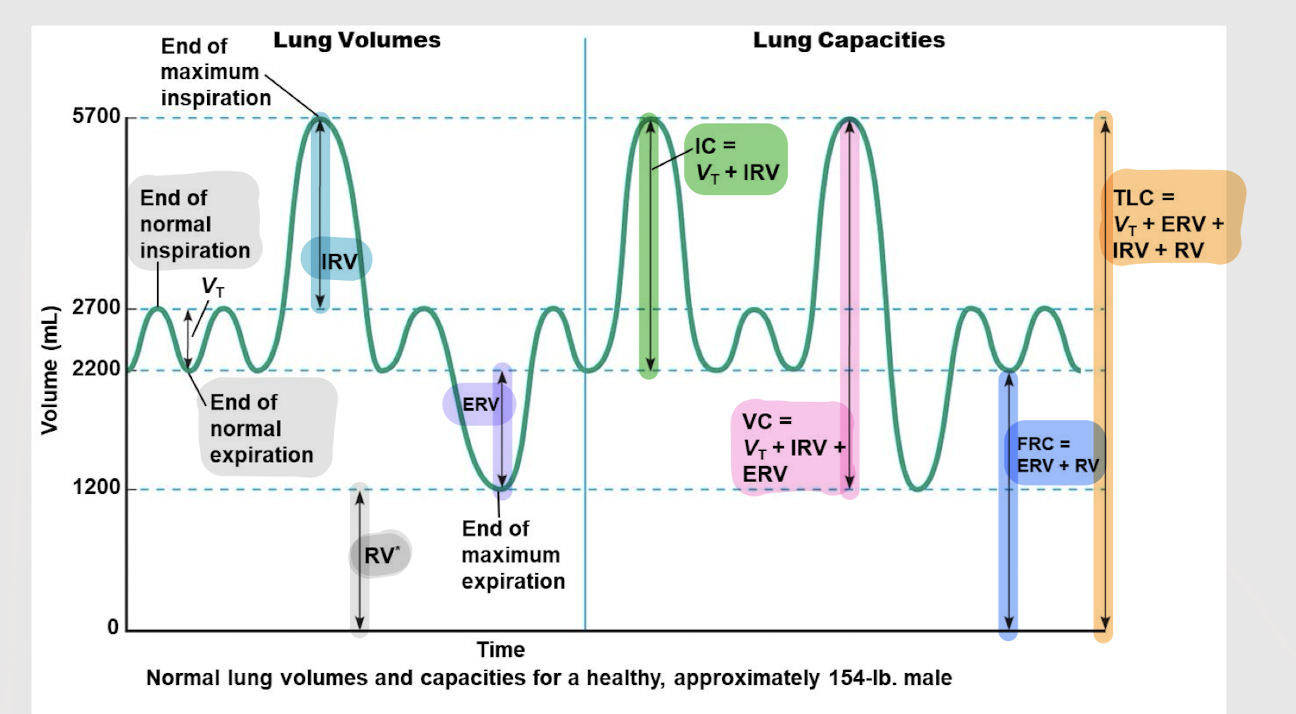
tidal volume (VT); 500mL
The amount of air inhaled or exhaled during a normal breath.
What is the typical volume?
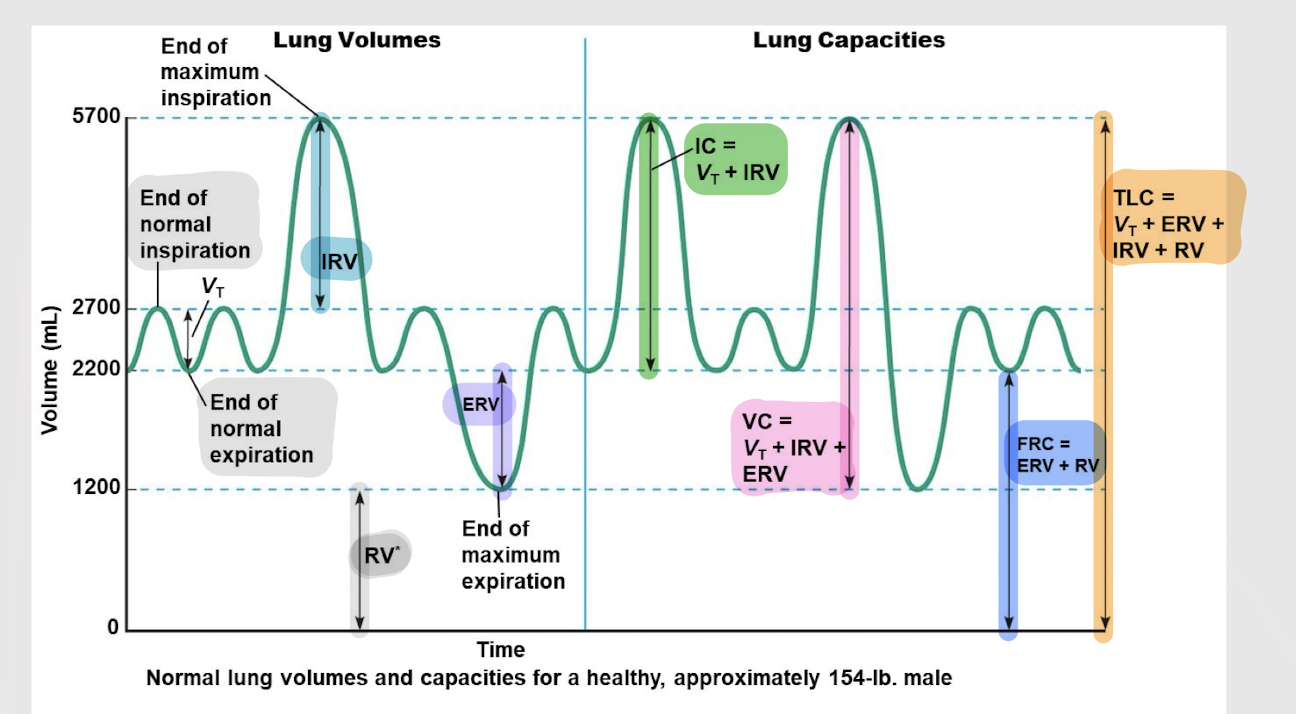
inspiratory reserve volume (IRV)
The amount of air you can forcefully inhale after a normal breath
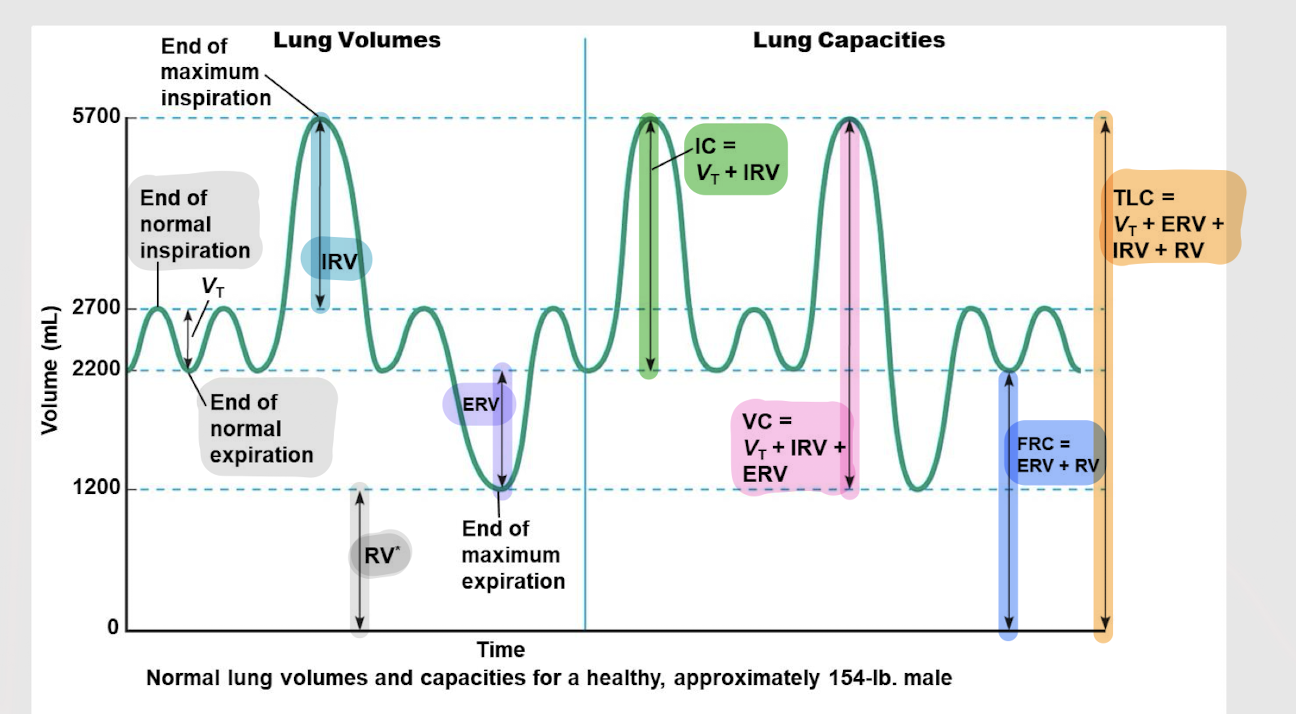
expiratory reserve volume (ERV)
The amount of air you can forcefully exhale after a normal breath
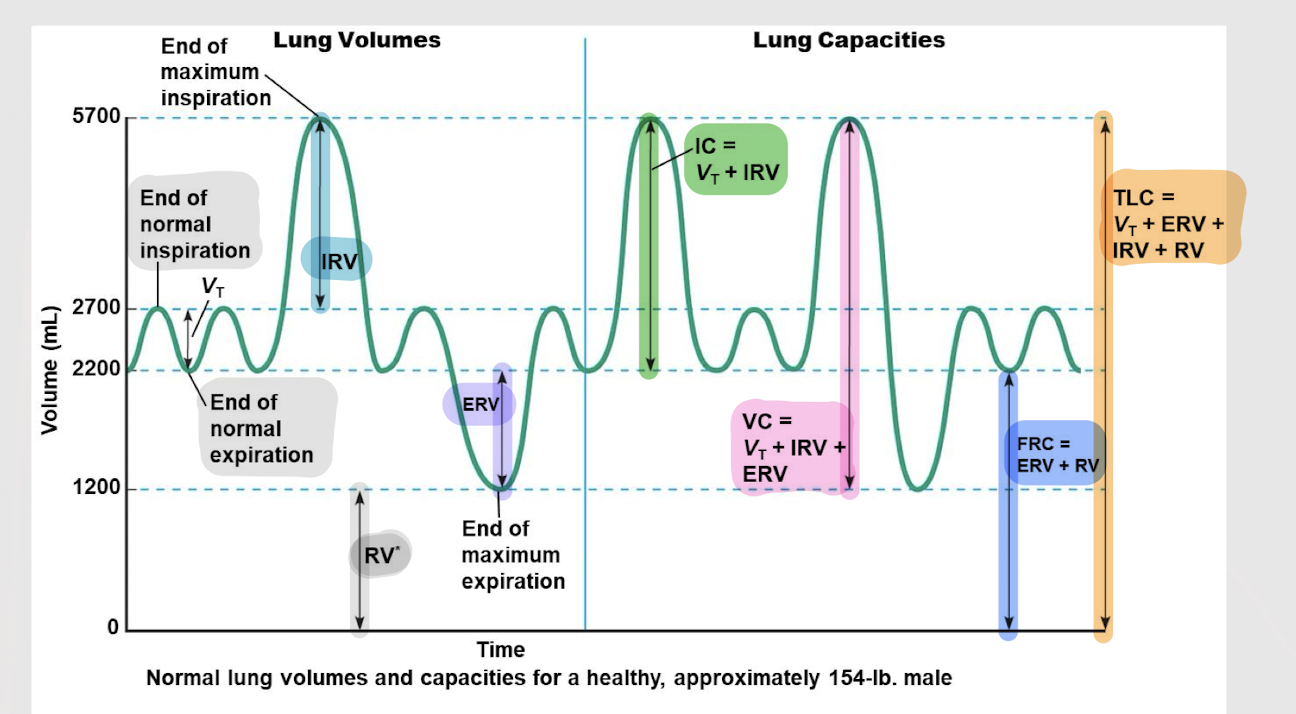
residual volume (RV)
the amount of air remaining in the lungs after a forceful exhalation
lung capacities
Two or more lung volumes together make up ______ ________
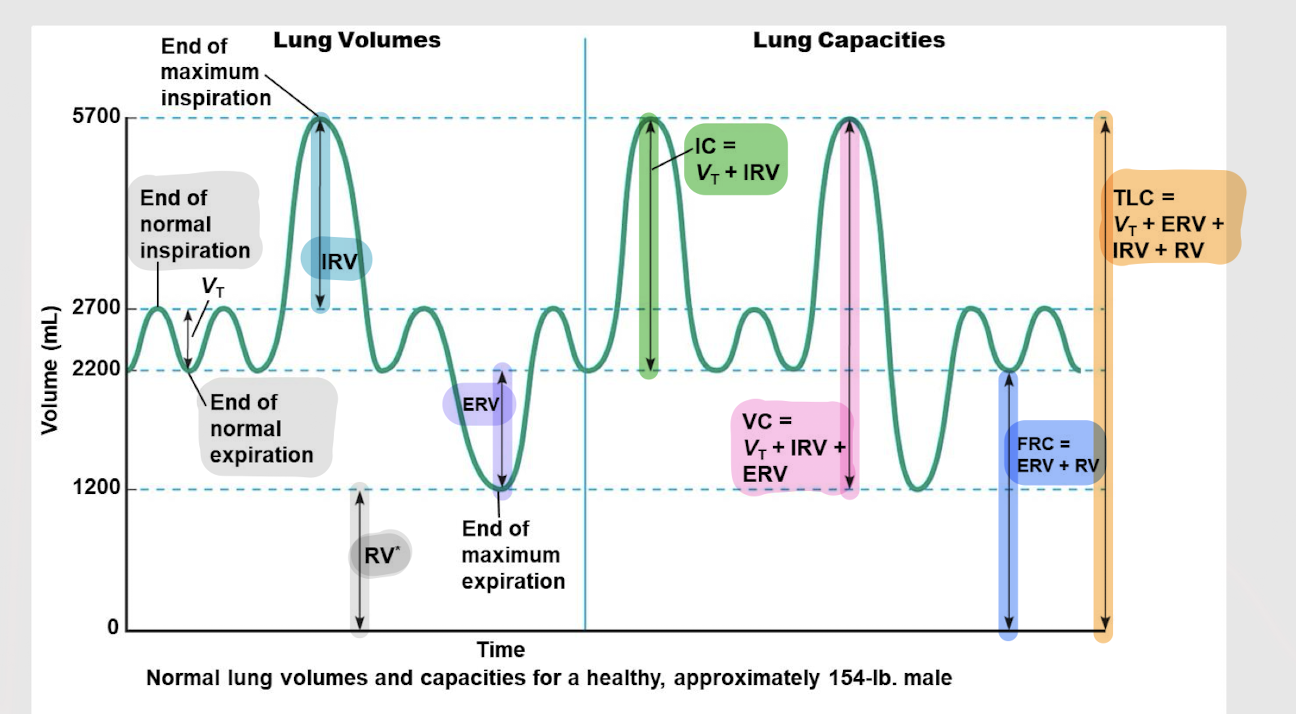
inspiratory capacity
All the volumes of air (VT + IRV) as they relate to inspiration make up the ________ ________. Shows the overall ability to bring air into the lungs.
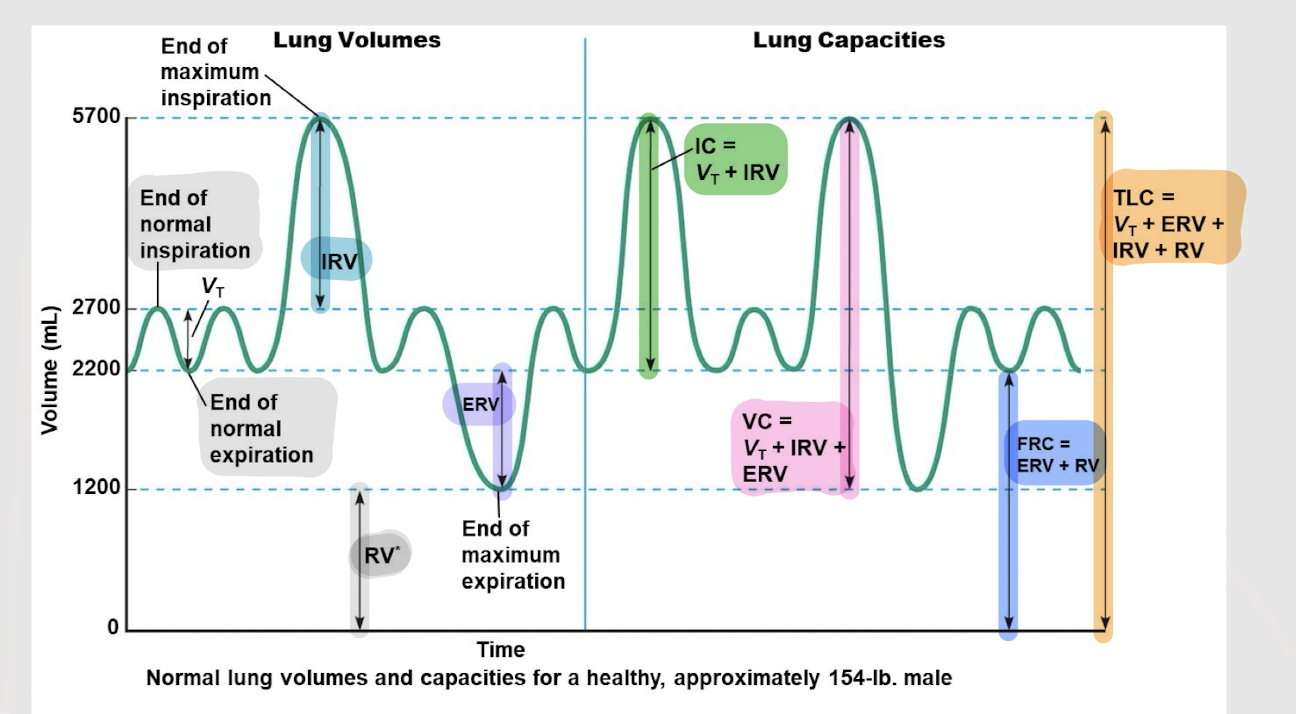
vital capacity (VC)
The max. volume of air that can be exhaled after a full, maximal inhalation
VT + IRV + ERV
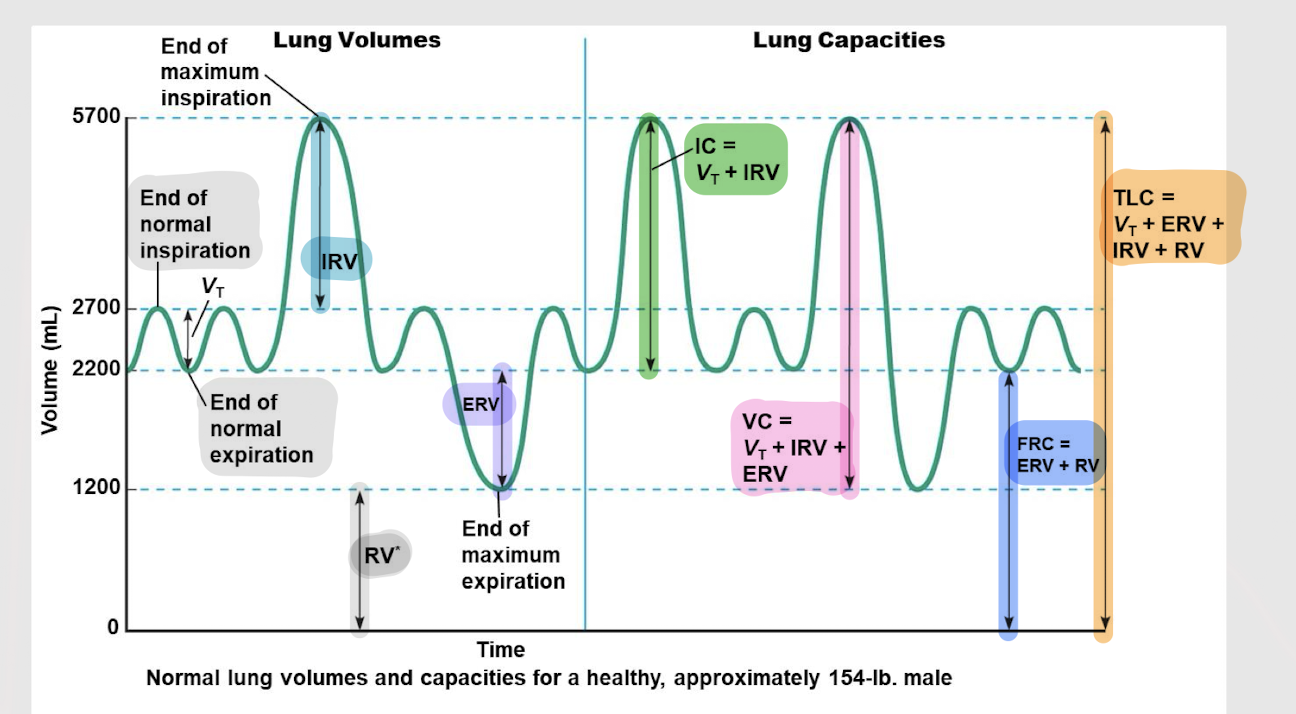
total lung capacity (TLC)
Total volume of air in the lungs after max. inhalation
VC + RV
minute ventilation (VE)
Total amount of air that flows into or out of the respiratory system in one minute
VE = VT x RR
6000 mL/min (or 6L)
What is the normal minute ventilation (VT x RR) in a healthy adult?
alveolar ventilation (VA)
The volume fresh air that reaches the alveoli each minute
VA = (VT - DSV) x RR
dead space ventilation (DSV)
The volume of inhaled air that does not participate in gas exchange.
Usually about 150mL remains in the conducting zone.
obstructive pulmonary disease
Pulmonary disease characterized by increased airway resistance
restrictive pulmonary disease
Pulmonary disease characterized by decreased lung compliance
acute obstructive pulmonary disease
What type of pulmonary disease is asthma?
asthma
Pulmonary disease:
inflammation of airway lining
increased mucous production
bronchospasm (smooth muscle wall of bronchi/oles contract)
asthma
Corticosteroids (anti-inflammatory) and bronchodilators (i.e. B2-adrenergic receptor agonists; e.g. inhalers) are used to treat what pulmonary disease?
chronic obstructive pulmonary disease (COPD)
Pulmonary disease:
Inflammation → airways narrow → decreased air flow
Inflammation → excessive mucous production
Increased RV due to decreased ability to expire
FRC and TLC
In COPD, the decreased ability to expire leads an increase in which two lung capacities?
lung expansion; TLC; VC
Restrictive pulmonary disease:
Structural damage to the pleura, chest wall, interstitium (e.g. scar tissue increases barrier) or parenchyma restrict _____ ________ → decreased compliance
Need more muscular work for air flow
Decreased _____ and _____
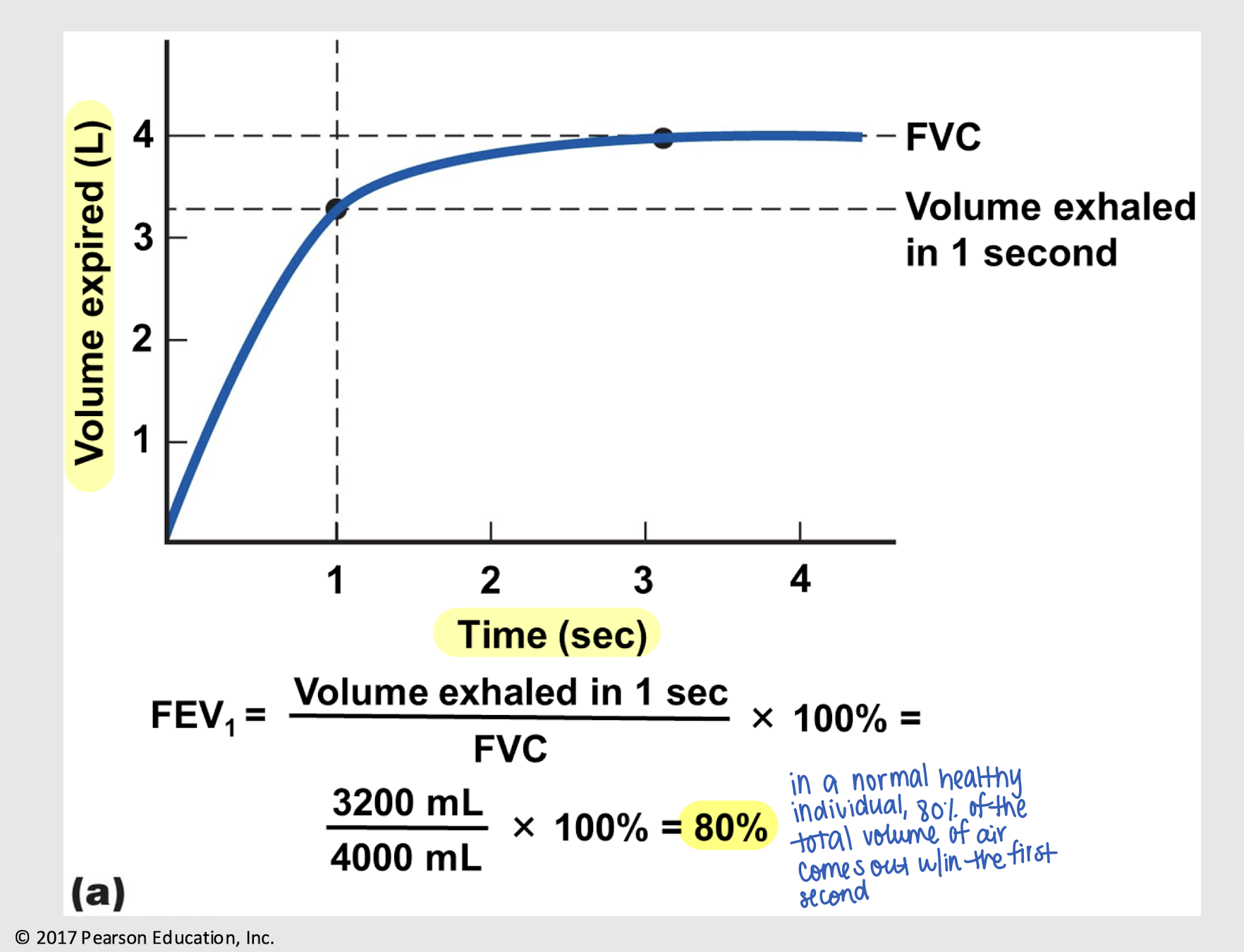
forced vital capacity (FVC)
Max. amount of air that can be exhaled after taking a deep breath in
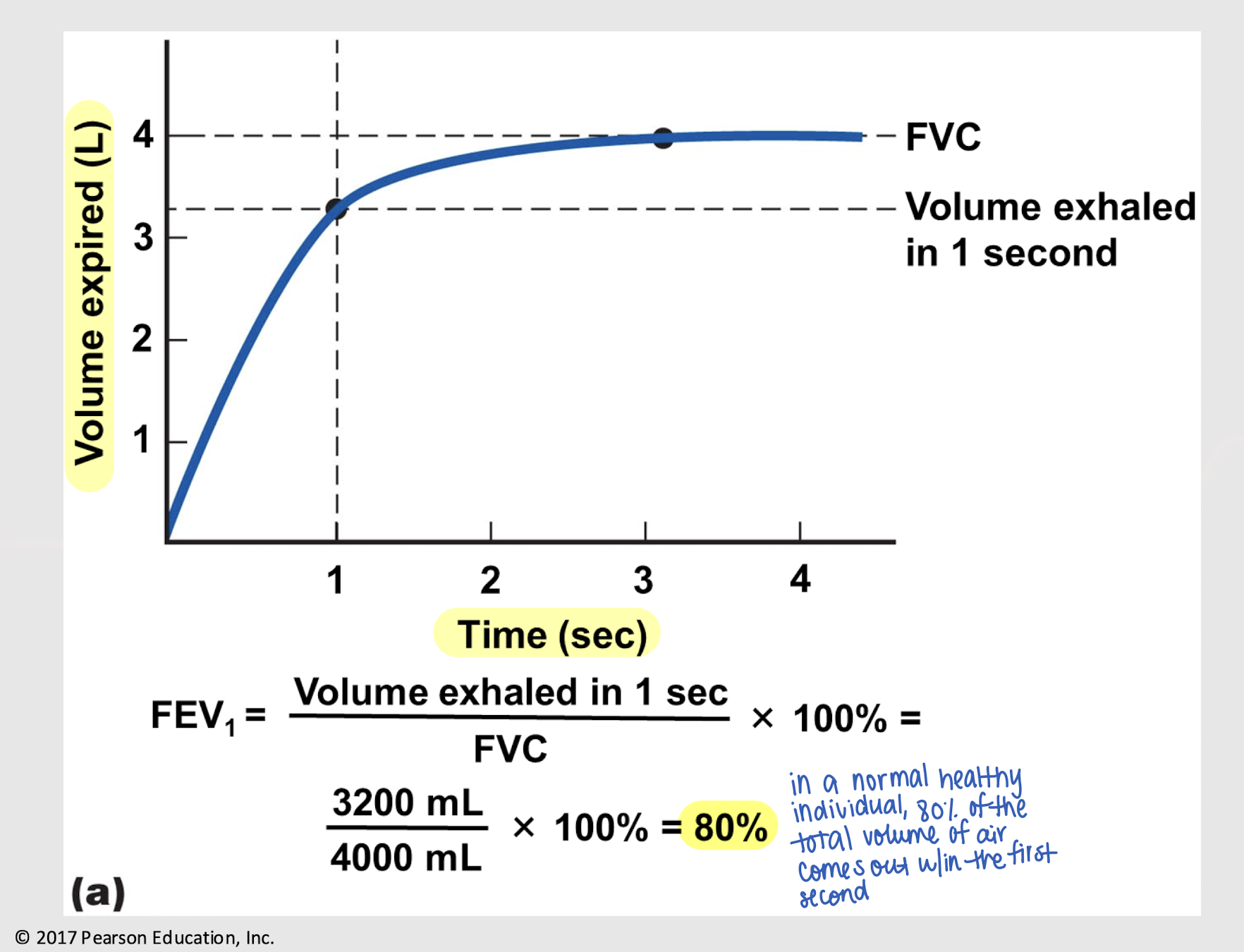
forced expiratory volume in 1 sec (FEV1)
Max. amount of air that can be exhaled after taking a deep breath in in 1 sec
(volume exhaled in 1 sec / FVC) x 100%
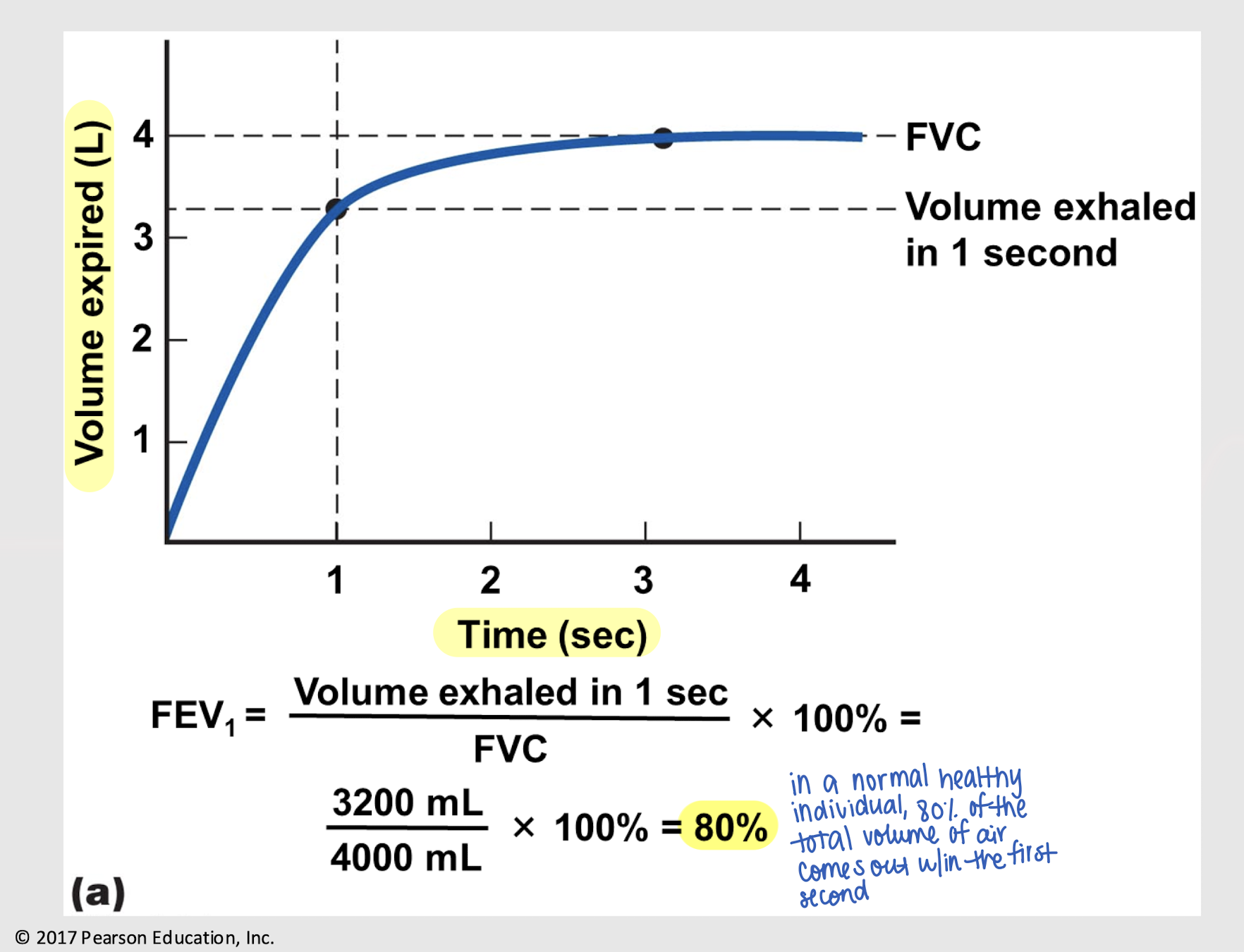
80%
What is the normal FEV1 in a healthy individual?
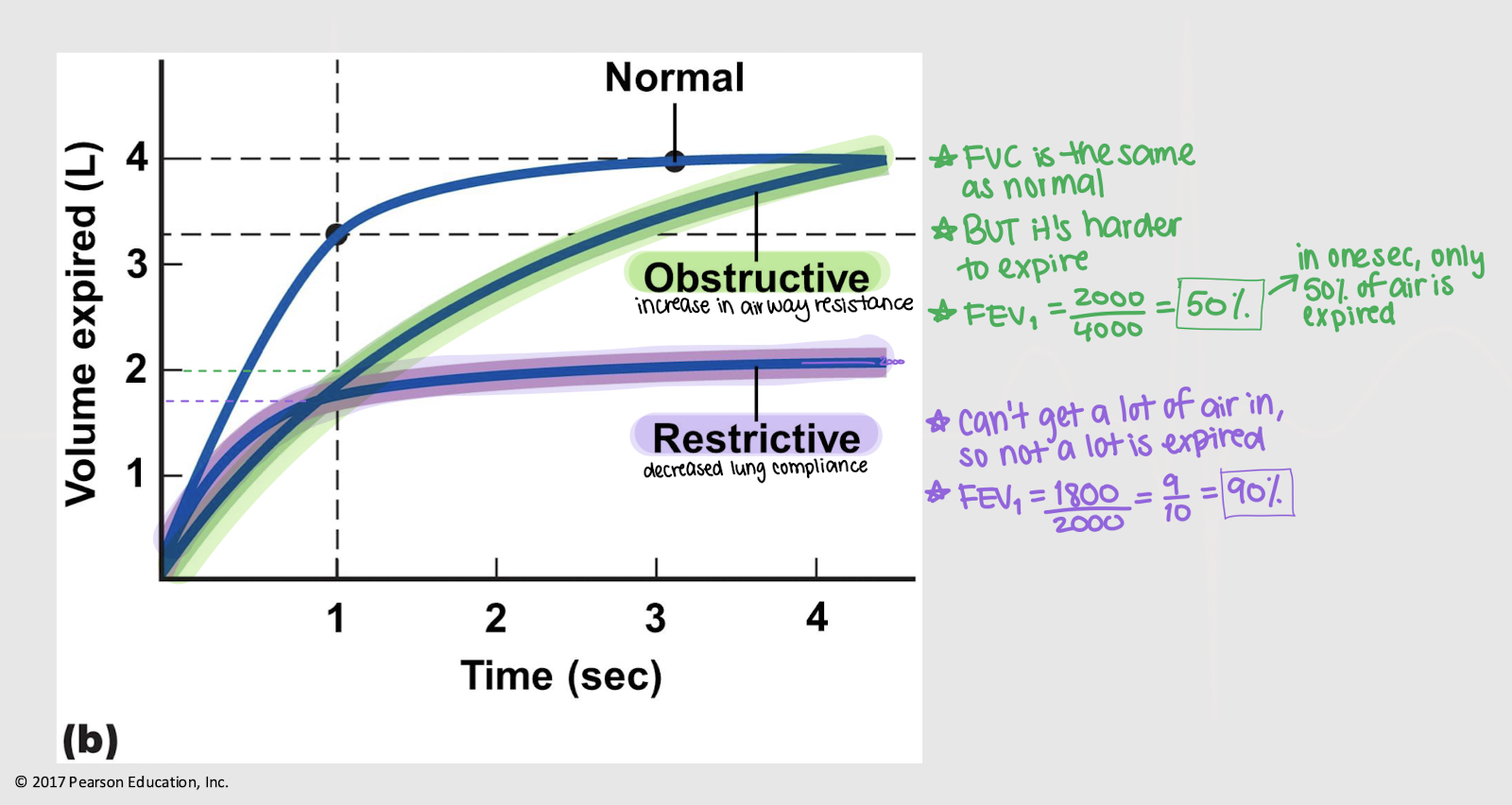
normal; low; low
In a pt w/ obstructive pulmonary disease…
FVC may be _______,
FEV1 is ____, so
FEV1 ratio is very ____
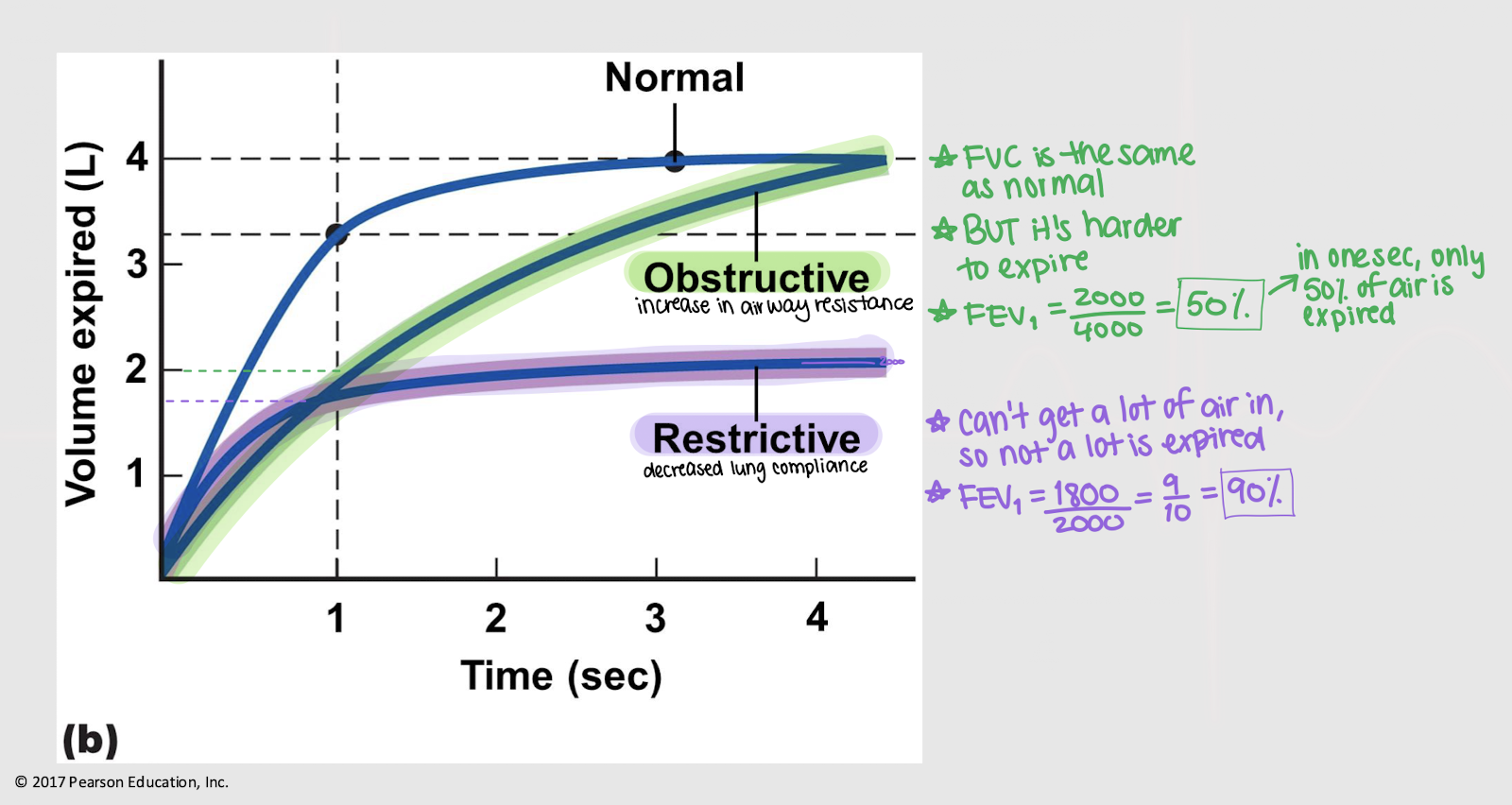
low; low; normal
In a pt w/ restrictive pulmonary disease
FVC is ____
FEV1 is ____, so
FEV1 ratio may appear _______