MMD I: Week 3 - General Principles for MSK Imaging
1/37
Earn XP
Description and Tags
Exam 1 Content
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
What is the #1 terminal course learning objective regarding imaging?
Identify normal radiographic anatomy
T/F: Advanced Imaging Modalities include X-rays, MRI, US, CT, and bone scan.
FALSE. X-rays are not considered an advanced imaging modality.
What is the process of attenuation?
The patient’s tissues absorb part of the X-rays, then the “remnant radiation” hits the receptor to produce an image
X-Rays: Pros and Cons
Indicated for bone and chest imaging
Pros: Inexpensive, readily available, no preparation required, non-invasive
Cons: Radiation exposure (significant), caution in pregnancy - cannot do on fetus
MRI: Pros and indications
Indicated for ligament, cartilage, intraosseous abnormalities, and bone tumors
Pros: Multi-plane images, no known health hazards, good contrast in water-density tissue
Good for LE ST injuries, peripheral, spinal, and nerve root compression and injury,
Better than CT at soft tissue differentiation
MRI: Cons and contraindications
Contraindicated with claustrophobia, metal clips/devices, and pacemakers
Cons: More expensive than intro studies, LONG time scans (+motion artifacts), limited availability, bone trauma poorly shown
CT: Pros and indications
Indicated to visualize complex fracture patterns, better than MRI for cortical bone
Pros: Improved ability to identify subtle and complex pathology, less expensive
What are the “shades of gray” on a CT scan?
Air = black
Fat = Gray/black
Water (ST)= Gray
Bone = Gray/White
CT: Cons and contraindications
Condraindication for radiation exposure
Cons: HIGH doses of radiation, hard to differentiate soft tissue
US: Pros and indications
Indicated for superficial structures - thinner areas
Pros: Real-time observation, fast, cheap, functional, NO CONTRAINDICATIONS
US: Cons and contraindications
NO CONTRAINDICATIONS - but do consider that risks are not well understood
Cons: Poor modality for metallic objects or bone, cannot go beyond the cortex
Radiologist training/experience is KEY in diagnostic utility for US
Scintigraphy: Pros and indications
Indicated to identify bone changes due to fracture, tumor, or infection (indicates ↑ metabolism)
Pros: VERY sensitive, can show stress fx 6-72 hrs from onset (better than radiograph), defines the EXTENT of multifocal lesions
Normal ↑ in WB surfaces, bladder, bone marrow
Scintigraphy: Cons and contraindications
Uses radioactive dye
Cons: Does not define the anatomy/mets of lesions, LOW SPECIFICITY
It will also reveal healed fractures, DJD, or growth plates
Abnormal ↑ in shafts and non-loading surfaces
Define radiodensity
Property of the tissue regarding ray absorption/attenuation
Composition and thickness of tissue
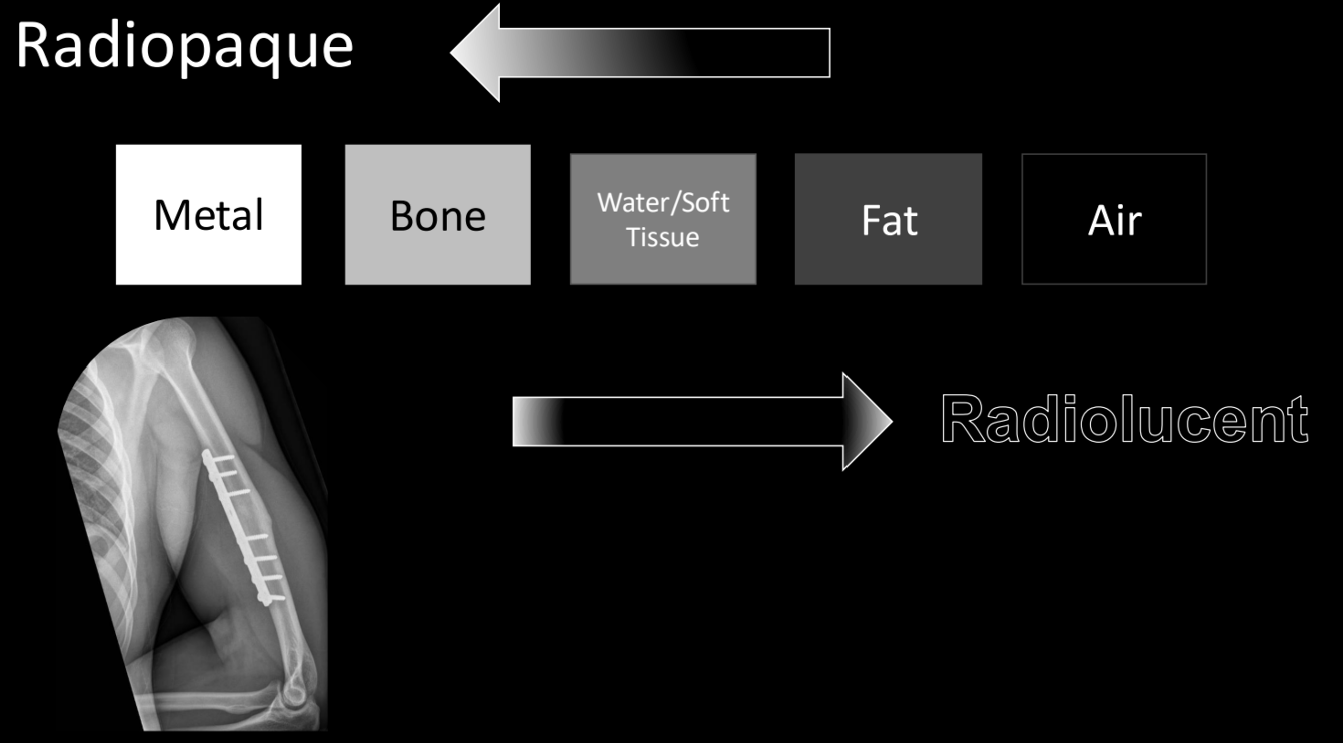
Define the radiopaque components and how they show on a radiograph:
Radiopaque structures are NOT easily penetrated by x-rays (eg. metals)
They will show lighter/whiter in the radiograph

Define the radiolucent components and how they show on radiograph:
Radiolucent structures are easily penetrated by x-rays (eg. air)
They will show lighter/whiter in the radiograph
*think about the fact that there is nothing that would absorb the X-ray, so it shows up black/intact)
Label the following from most radiopaque to most radiolucent:
Water/ST
Fat
Bone
Metal
Air
See image
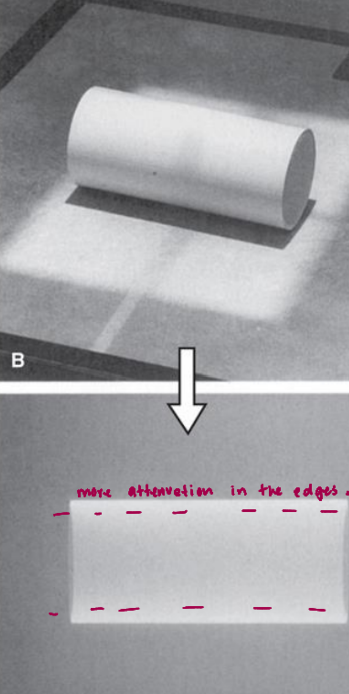
T/F: Depending on the angle of projection in the curved plane, the portion parallel to the image receptor is the thickest
FALSE. The section parallell to the receptor is the thinnest, the perpendicular section is the thickest
T/F: For curved objects, there will be more attenuation observed in the edges
True
T/F: Fractures usually appear as black lines on x-rays
True

For x-rays one view is the same as no view, therefore we need a minimum of 2 views offset by ____
90°
What are the two main pitfalls of image interpretation?
Errors of observation
Errors of interpretation (failure to link clinical data, over reliance on imaging, 20-40% of reports have errors!)
According to Shelbourne JBJS 2010, what % of ortho specialists touched the involved knee AND had a comparison of the uninvolved site?
ONLY 37% of the 89% ortho specialists that touched the knee had ALSO touched the uninvolved side for comparison
According to Shelbourne JBJS 2010, out of the 89% of ortho specialists that performed a physical exam, how many performed an exam through clothes?
79%
According to Shelbourne JBJS 2010, out of the 11% ortho specialists that DID NOT do a physical exam, what % ordered an MRI anyway?
73%
T/F: The ACR Appropriateness Criteria was designed in the 90s to inform clinicians of which imaging modality is appropriate, and when imaging is indicated
FALSE. The ACR does NOT provide information on WHEN imaging is appropriate
What are the ABCS of radiographic evaluation?
Alignment
Bone density
Cartilage spaces
Soft tissues
Alignment: What are the components you are examining?
General skeletal architecture
# of bones, size & shape, congenital
Countours (smooth and continuous)
Look for fracture lines, spurs, irregularities, and cortex disruption.
Relative position (good articulation)
Fractures, sublaxation, dislocation [need multiple views!]
T/F: If an edge is round and smooth, it indicates that bone has been there for a long time
True (eg. Os naviculare)

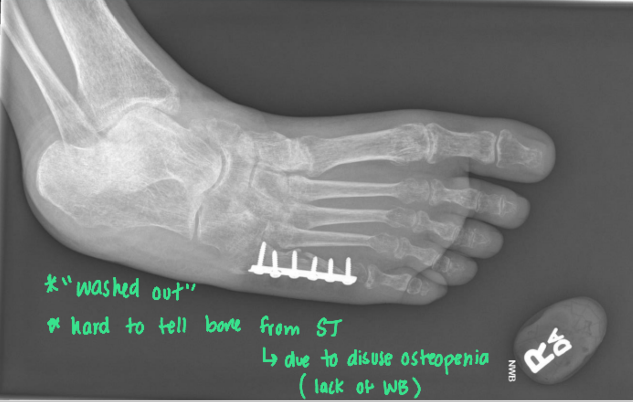
Bone Density: What are the components you are examining?
General and focal BD (contrast between ST and bone + cortical shell and cancellous center)
Loss of contrast means we are losing density
Localized contrast changes
Look for sclerosis (excessive/reactive) or spurs
This can happen due to fx, osteomyelitis, OA, or tumors \
Texture (normal trabecular architecture)
Thin, delicate, coarse, lacy, fluffy
What does “sclerosis” mean in radiology terms?
Areas of increased density(↑radiopaque)
Cartilage Space: What are the components you are examining?
Joint space (normal width/symmetry)
↓ joint spaces, osteophytes + sclerosis, loss of smooth joint surface (contour)
Subchondral bone (Smooth surface - no irregularity)
↑ sclerosis and erosion
Epiphyseal plates (normal thickness/position relative to secondary epiphysis)
Abnormal thickness, irregular margin

What is wrong with this patient?
Nothing, this is a pediatric radiograph. The lines show epiphyseal plates
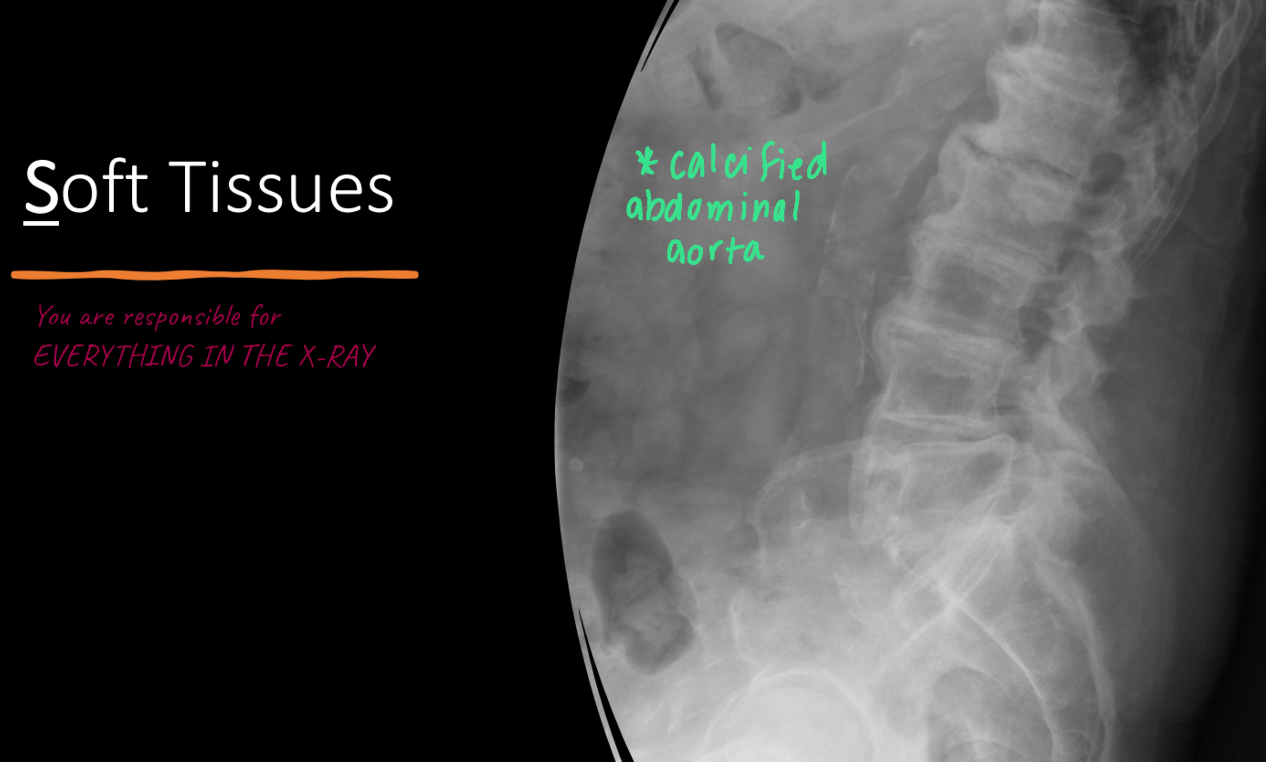
Soft tissue: What are the components you are examining?
Gross musculature contour
Wasting, swelling, and calcification
Joint capsule (normally you CAN’T see it)
distended by effusion/hemorrhage, or calcified
Fat pad sign (not visible OR very thin)
Enlarged, displaced, elevated, blurry → indicates trauma nearby
Periosteal reaction (not visible)
Fuzzy, indistinct margin → physiological healing response (like stress injury)
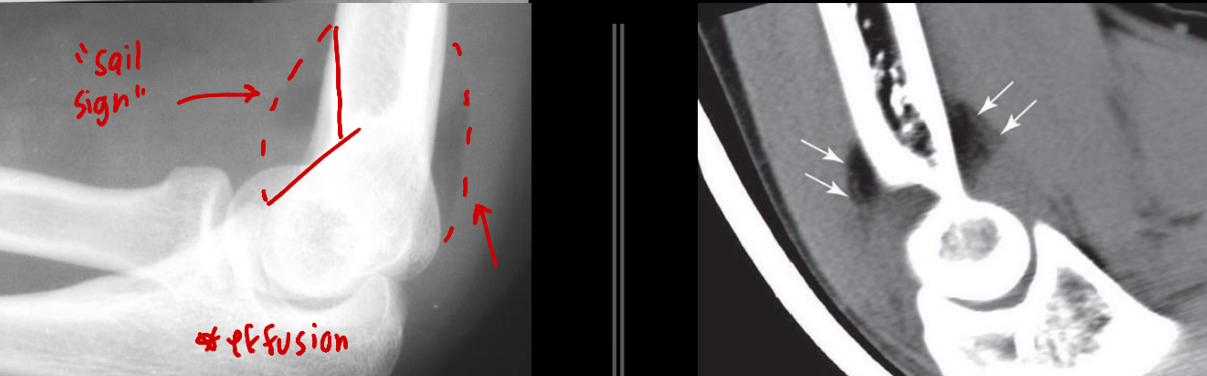
Where can you observe a “sail sing” and what does it indicate?
Disruption in the ANTERIOR fat pad, correlates to:
Kids: Epicondyle/humeral fracture
Adults: Radial head fracture
Does an abnormal finding on imaging imply a significant pathological process?
NO, an abnormality on imaging DOES NOT mean it’s significant or symptomatic
What is the most important requirement for the appropriate utilization of imaging?
Quality patient examination
What are the three ways in which harm can be caused with the inappropriate use of imaging?
Misinterpretation by providers
Misinterpretation by patients
Radiation exposure