NEUROLOGIC UPPER EXTREMITY: Function and Management
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
TRUNK-LIMB CONNECTION
Anticipatory Postural Control
Interaction of UE’s with the Environment (Beyond Postural Support)
Dynamic trunk control for reach beyond arm’s length
Biomechanical Considerations
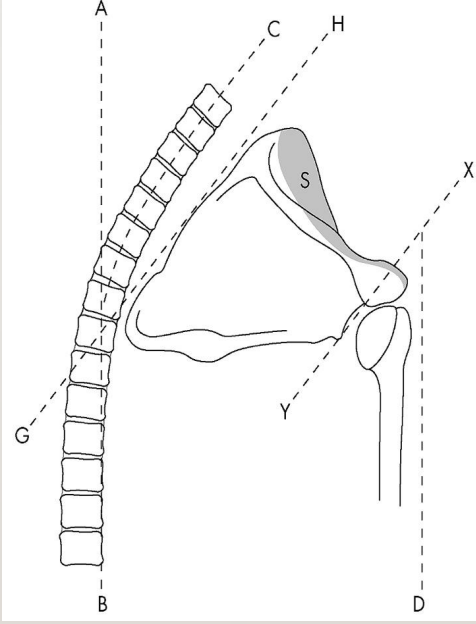
Skeletal: Clavicle serves as a bridge between the trunk and UE complex (e.g., sternoclavicular joint)
Origins and insertions of muscles that stabilize and move the UE are dependent on trunk stability and alignment
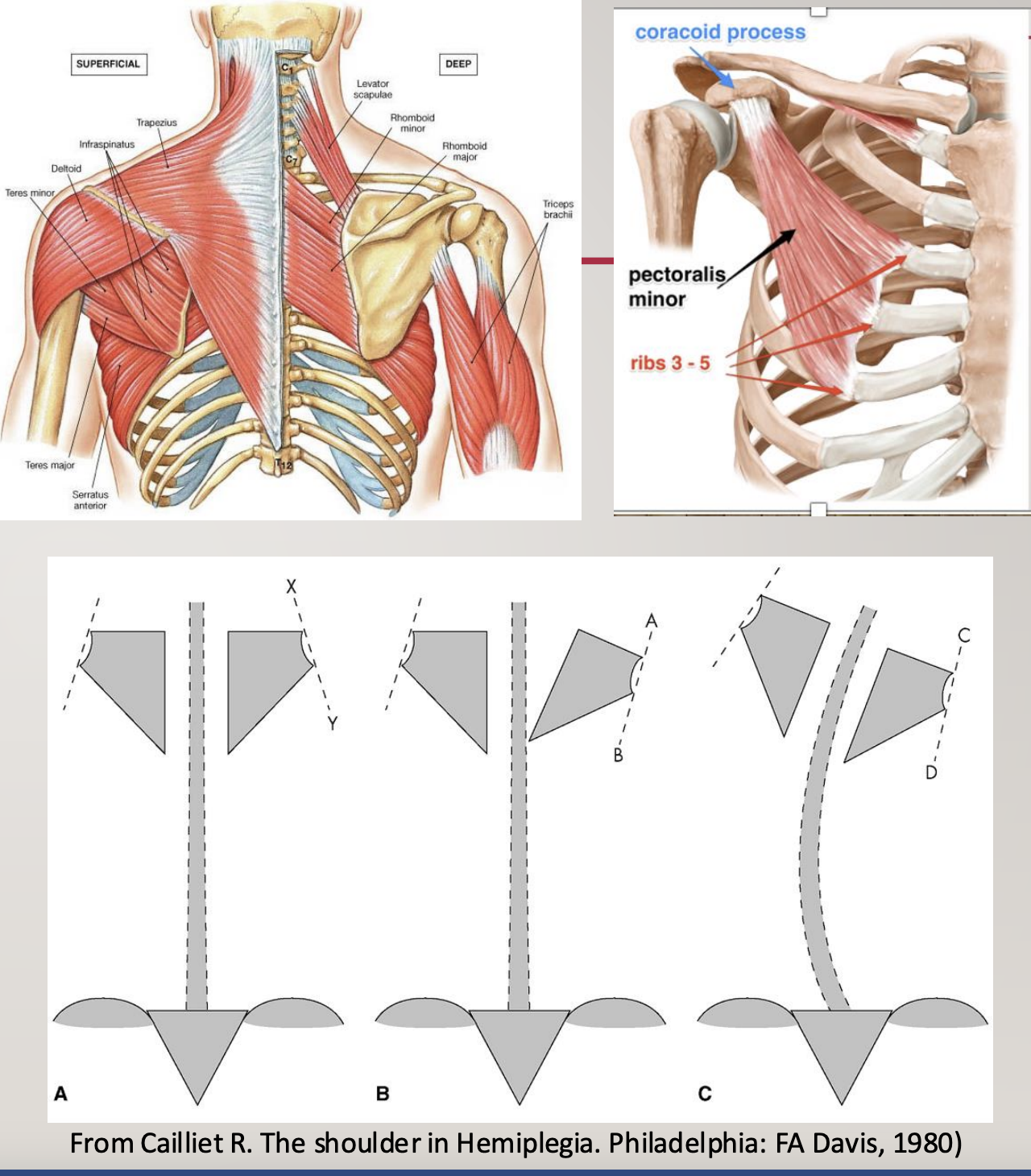
LOSS OF SCAPULAR ALIGNMENT AND CONTROL
Resting position of scapula (i.e., appropriate alignment)
Function of the scapula:
stability,
support overhead motions,
glides to prevent impingement
Why does scapula fall out of alignment?
Weakness in scapula
of upper traps, of lower traps, etc.
Muscle imbalance around the scapula
Trunk mal-alignment (B in photo)
Usually, downward rotation, “tipping”, and winging
due to a problem with the serratus anterior
What to look for?
scapula
vertebrae
pelvis
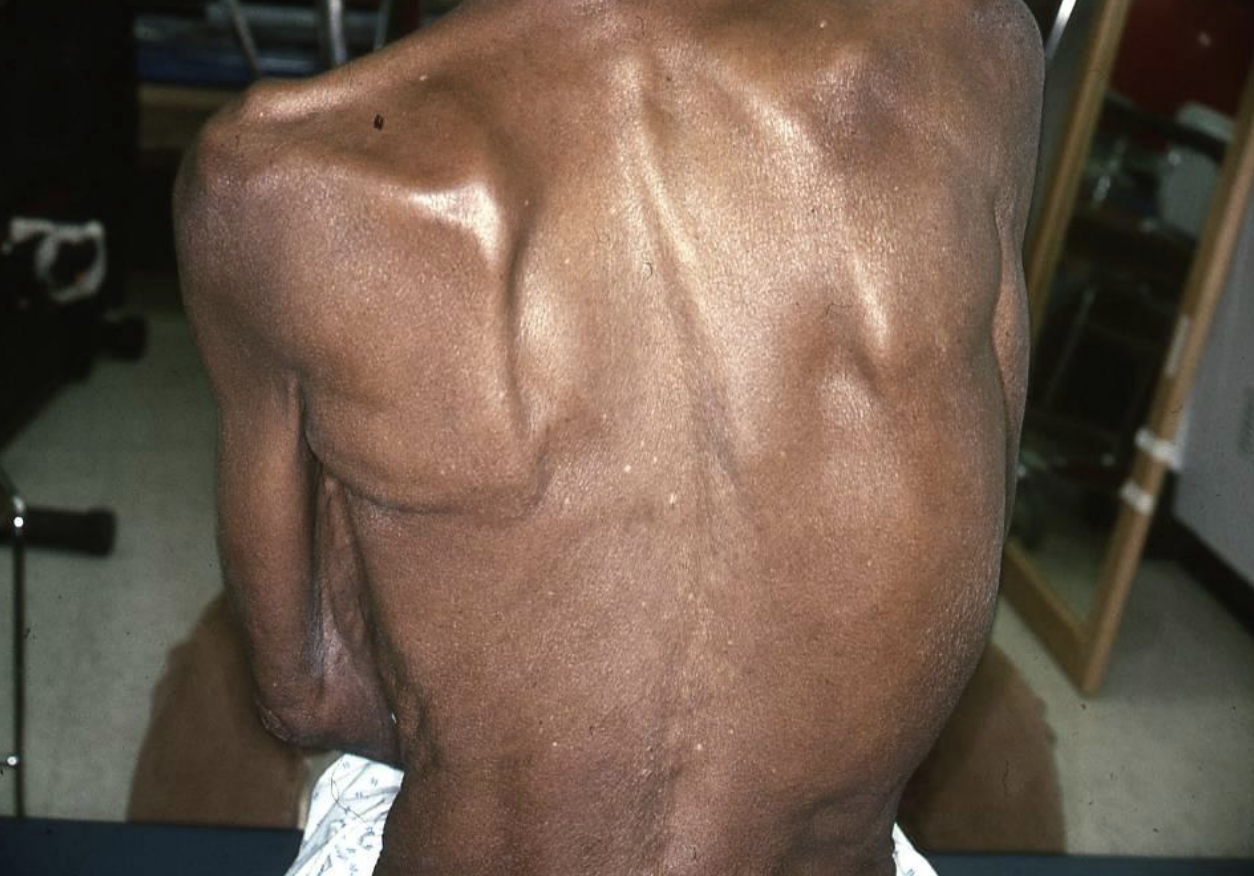
observations
curvature of the spine
lateral flexion of the trunk
shortened left, elongated right side of the trunk
(potentially) downward winging scapula (as seen by too much clarity)
shoulder/arm/elbow is internally rotated
weight shifting more onto 1 side than the other
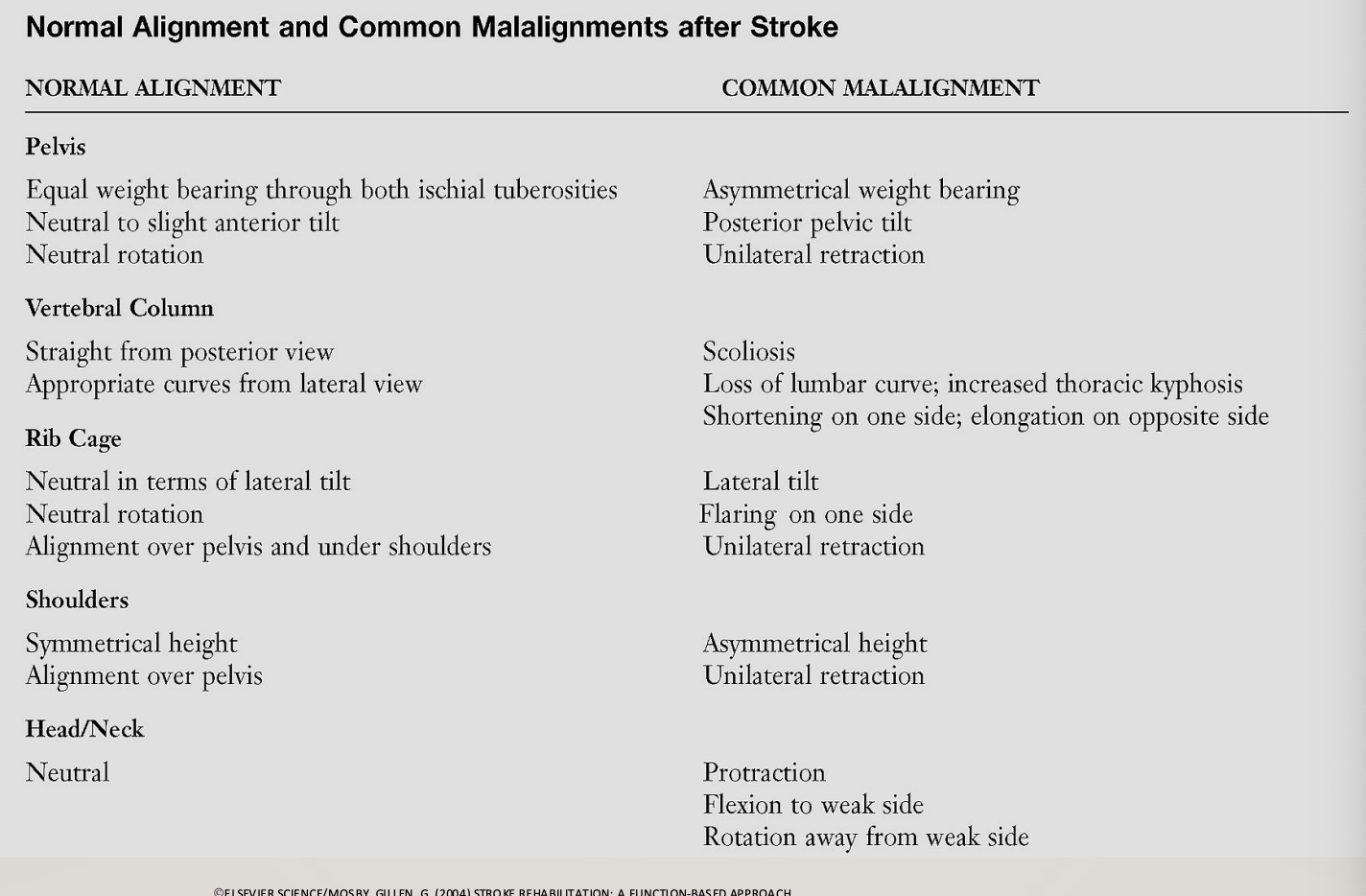
normal alignment vs common malalignment of
pelvis
vertebral column
rib cage
shoulders
head/neck
SCAPULA MAL-ALIGNMENT (results in)
Subluxation
shoulder muscles are initially weak
—> followed by gravity continuing to actively pull it down
Abnormal Scapulohumeral Rhythm
Pain and Impingement
scapula can’t get out of the way when the shoulder goes into flexion
—> followed by pain and impingement
Ineffective & Inefficient Movement Patterns
Possible SHS (shoulder hand syndrome)/CRPS
Decreased Function
image
A-B: neutral
C-B: lateral flexion
SUBLUXATION PATTERNS + ***how you would treat a sublux
patterns
Inferior
Anterior
Superior
treating
Positioning & Support
goal: prevent the humeral head from pulling downward due to gravity
supportive positioning:
when sitting: keep the arm supported on a pillow or lap tray
when in bed: position the arm slightly abducted and externally rotated, with a pillow under the shoulder/arm
Avoid pulling on the arm
Supportive devices
e.g., humeral cuff sling, lap trays ← preferred over standard slings to reduce traction while allowing some movement
Facilitation & Strengthening
goal: re-activate and strengthen shoulder stabilizers
Facilitate scapular alignment (retraction + upward rotation) through guided movement or neuromuscular re-education
Strengthen key muscles:
Supraspinatus
Deltoid
Rotator cuff and scapular stabilizers
Therapeutic activities/exercises:
Weight-bearing through the affected arm on a stable surface
Gentle, supported reaching in different planes
Mirror therapy or bilateral task training for awareness and symmetry
Neuromuscular Electrical Stimulation (NMES)
goal: activate weak shoulder muscles and realign the humeral head
Commonly applied to supraspinatus and posterior deltoid
Shown to reduce inferior subluxation and improve shoulder control when used early post-stroke
Taping or Strapping
goal: provide proprioceptive input and mechanical support
Kinesio taping or therapeutic taping can help reposition the humeral head and cue muscle activation
Often used along with NMES or exercise—not as a standalone intervention
Tone Management (for spastic stages)
goal: reduce abnormal muscle pull contributing to anterior/superior subluxation
Stretch tight muscles
Use weight-bearing and slow, rhythmic movements to inhibit spasticity
Botulinum toxin injections may be prescribed by physicians for severe tone
Education
goal: prevent injury and promote independence
train patient and caregivers in safe handling, proper positioning, and use of support devices during mobility or transfers

INFERIOR SUBLUXATION
evaluate by letting the arm hang (to see whether the arm is out of its socket)
downward humeral head displacement
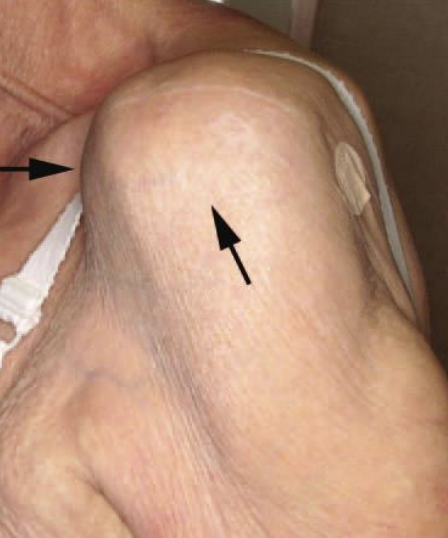
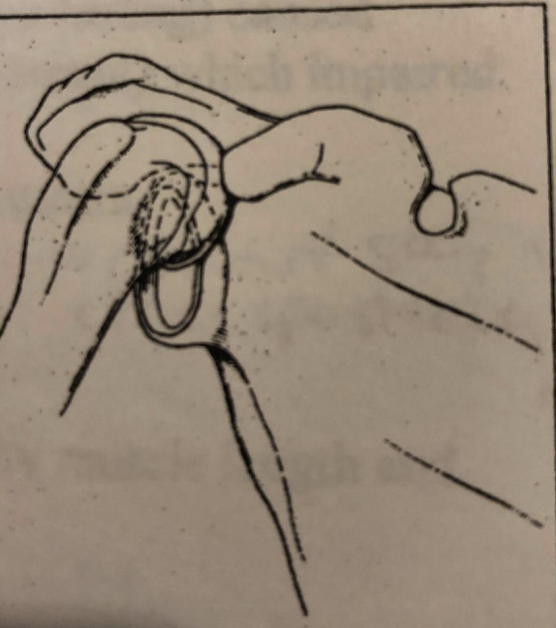
ANTERIOR SUBLUXATION
forward and downward humeral head displacement
humerus in extension
elbow is flexed
biceps tendon is getting overstretched by shoulder overextension
SUPERIOR SUBLUXATION
upward humeral head displacement
occurs w/ movement
humerus goes up while in flexion, instead of dropping (what it’s supposed to do), resulting in impingement
FACTORS ASSOCIATED WITH HEMIPLEGIC SHOULDER PAIN (HSP):
what might be correlated to HSP?
Lack of G-H Joint External Rotation
Correlation: HSP and decreased UE motor function
Correlation: HSP and shoulder weakness
Correlation: Orthopedic involvement
HSP and tendinitis of the long head of the biceps and supraspinatus
Shoulder hand syndrome (SHS) in hemiplegia is initiated by peripheral lesions
HSP and adhesive capsulitis, rotator cuff tear, and SHS
But NOT subluxation
Correlation: poor handling of the UE and pain
Choosing Wisely: Don’t use pulleys for people with a hemiplegic shoulder
you will yank the shoulder overhead without looking at the scapula and its scapulohumeral rhythm
different situation for an orthopedic situation, but you should NOT do this for hemiplegic cases
SHS (shoulder hand syndrome)/CRPS
***how would you prevent it
Suggests that SHS in Hemiplegia is initiated by a Peripheral Lesion (tissue or nerve injury)
Risk factors:
visual neglect (perceptual negligence when someone doesn’t attend to their arm and subsequently drags it along everywhere),
subluxation,
shoulder weakness,
moderate spasticity
Implemented Prevention Protocol:
Education to Family, Patient, and Staff at Admission to Prevent Peripheral Injury
Modified Bed and W/C Positioning to prevent pain in the arm
No PROM Before Scapula Mobilization
No Pain During Exercise/Activity/Positioning
No Infusions into Affected Hands
Incidence of SHS decreased from 27% to 8%
symptoms
shoulder gets tight and painful
arm starts to look shiny (mid stages of the syndrome)
edema
UPPER EXTREMITY EVALUATION
Clinical evaluation
AROM (flexor synergy versus isolated movements),
flexor synergy= abnormal all encompassing movement pattern in which muscles that normally work independently begin to contract together in a fixed, stereotypical way; it’s a sign of spasticity and loss of motor control following damage to the corticospinal tract
instead of being able to reach out smoothly, the arm tends to bend and pull toward the body (e.g., elbow, wrist, finger flexion, forearm supination, etc.)
Flexor synergy usually appears in the recovery phase after flaccidity, often as muscle tone starts returning
we want to aim to isolate these movements, so that the UE can be functional; plan interventions to reduce abnormal tone and promote isolated movement, such as through task-oriented training, neuromuscular re-education, or constraint-induced movement therapy
PROM
MMT (?)
hard to do unless a patient is a little further along and can do isolated movements without compensation from other muscles
Sensation
Spasticity
Pain
Posture (pelvis, trunk, scapula, shoulder, etc.)
Hand function
Fine motor coordination, grasp and release, and strength
ADL
use of arm with ADL
how are they using that arm, especially in tasks?
UE STANDARDIZED ASSESSMENTS
***objective vs subjective?
Fugl-Meyer Assessment-Upper extremity (FMA-UE)
objective
Stroke Upper Limb Capacity Scale (SULCS)
objective
Wolf Motor Function Test (WMFT)
objective
Action Research Arm Test (ARAT)
objective
Motor Activity Log (MAL)
subjective (self-report by patient)
ABILHAND
subjective (self-report by patient)
Functional Upper Extremity Levels (FUEL)
objective
Jebsen-Taylor Hand Function Test (JTHFT)
objective
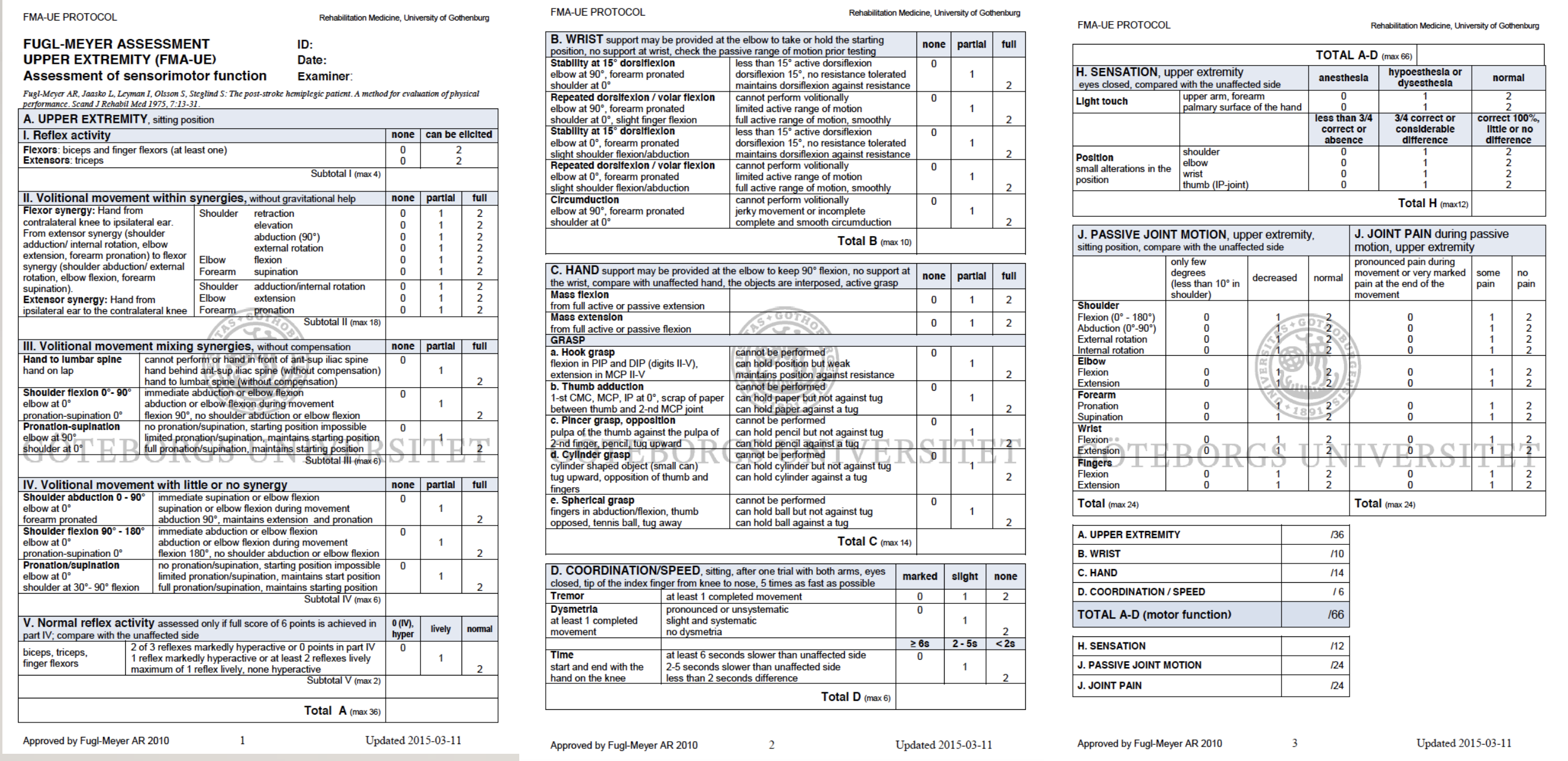
FMA-UE (Fugl-Meyer Assessment-Upper Extremity)
objective measure
FMA measures recovery in stroke survivors (UE and LE)
hint: Fugl-Meyer is a gold standard example of a recovered stroke survivor
Used in both clinical and research setting
The Gold Standard for assessing recovery post-stroke (but could be better, since it’s not very function-based)
Length of test: 30 minutes, but quicker once you have more experience
Age range: 13-65+
FMA-UE
Motor: Upper extremity, wrist, hand, coordination
Sensation
PROM
Pain
Likert scale 0-2, with a max score of 66, with higher scores indicating greater recovery
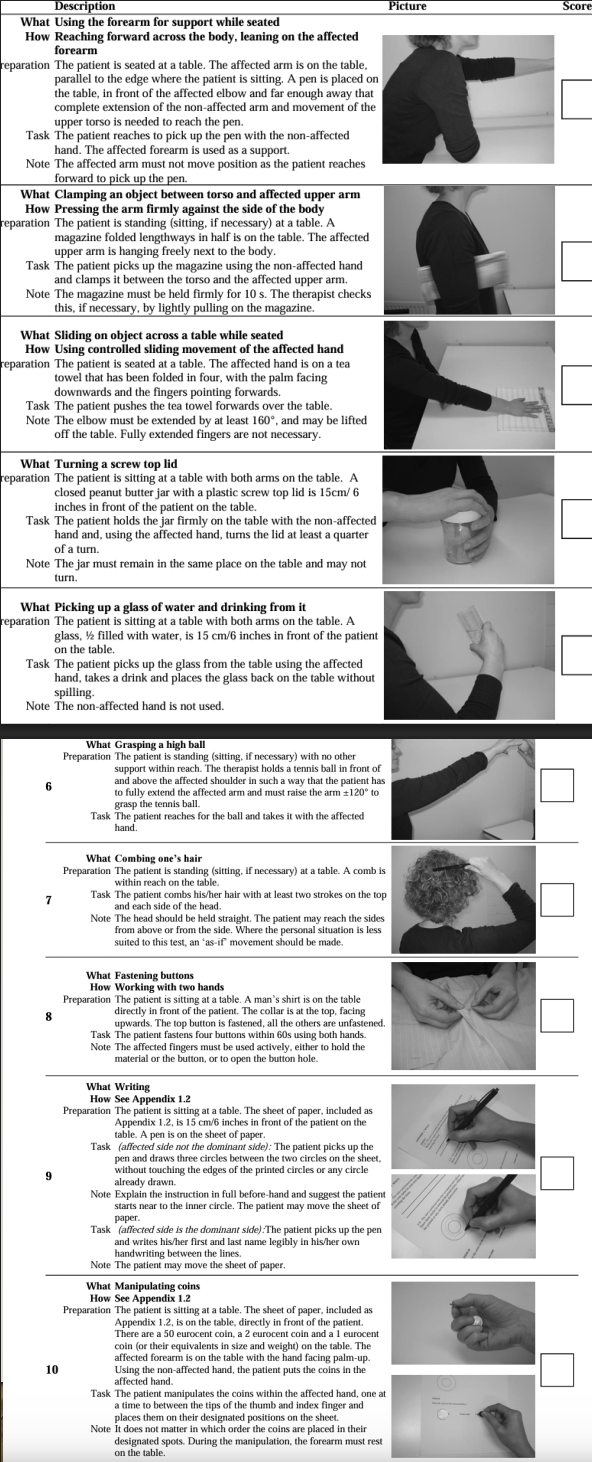
STROKE UPPER LIMB CAPACITY SCALE (SULCS)
objective measure
10 tasks: simple to complex
Performed standing or sitting
hint: SulcS; Standing or Sitting
All tasks unaided
Examines performance of task, not the quality (very functions-based!)
e.g., reaching, opening lids, grasping a high ball, combing hair
hint: CAPACITY scale ==> PERFORMANCE, NOT QUALITY of a skill
Score:
0= Patient unable to perform the task in the manner described
1= Patient is able to perform the task in the manner described
hint: CAPACITY ==> COMPUTER; scoring is like binary coding (0- no, 1- yes)
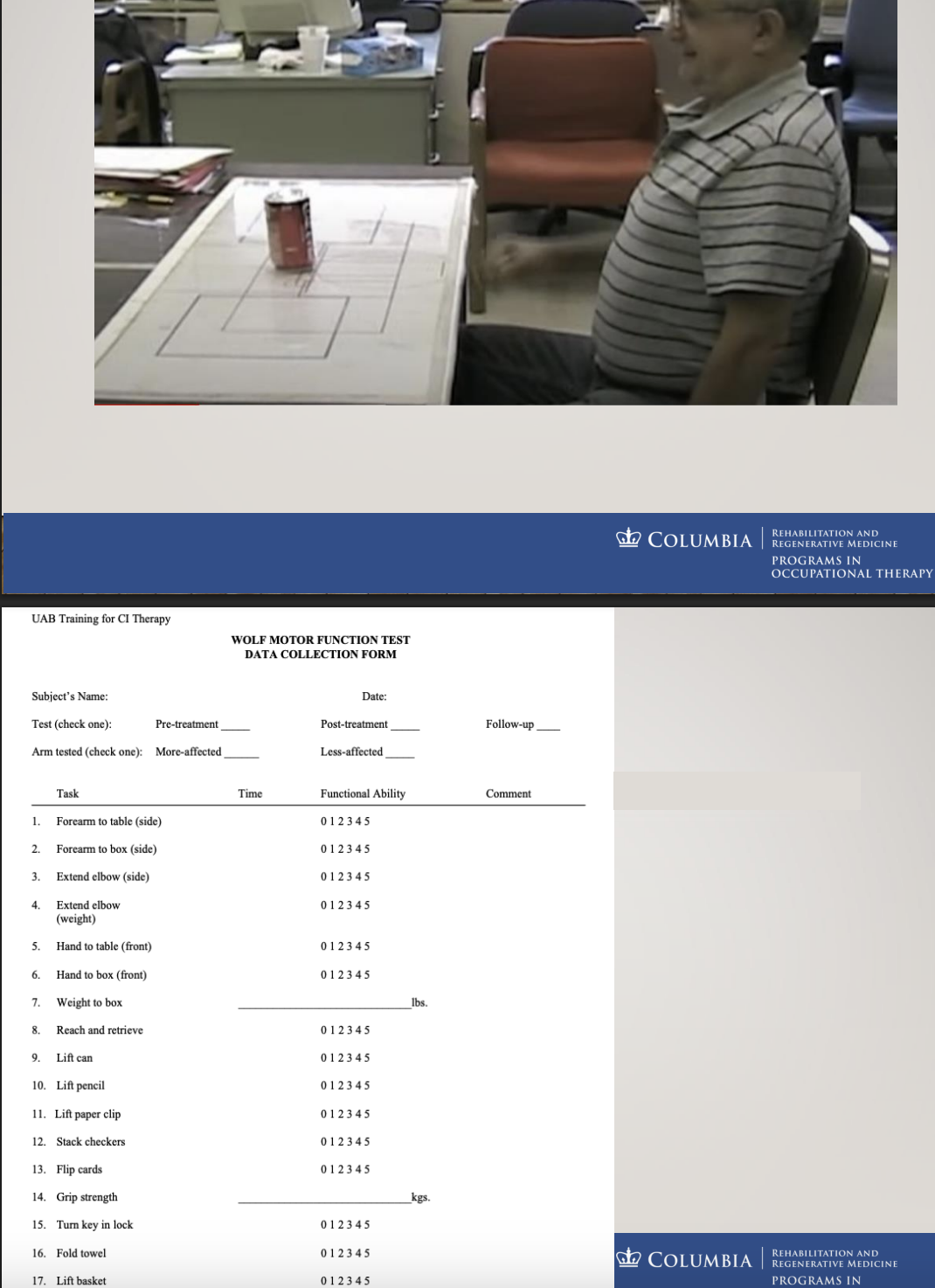
WOLF MOTOR FUNCTION TEST (WMFT)
objective measure
Standardized assessment to quantify upper extremity motor ability through timed and functional tasks for stroke patients
hint: WOLVES can (1) execute, and (2) be fast
Brain injury and stroke
measured in
Functional ability (WMFT-FA): 17 items on a 6-point scale (0-5) with higher scores indicating higher functioning levels, and
Performance time (WMFT-PT): 120 seconds max for each item
Standardized template so items can be placed in specific areas
and then doing tasks in these specific set-ups
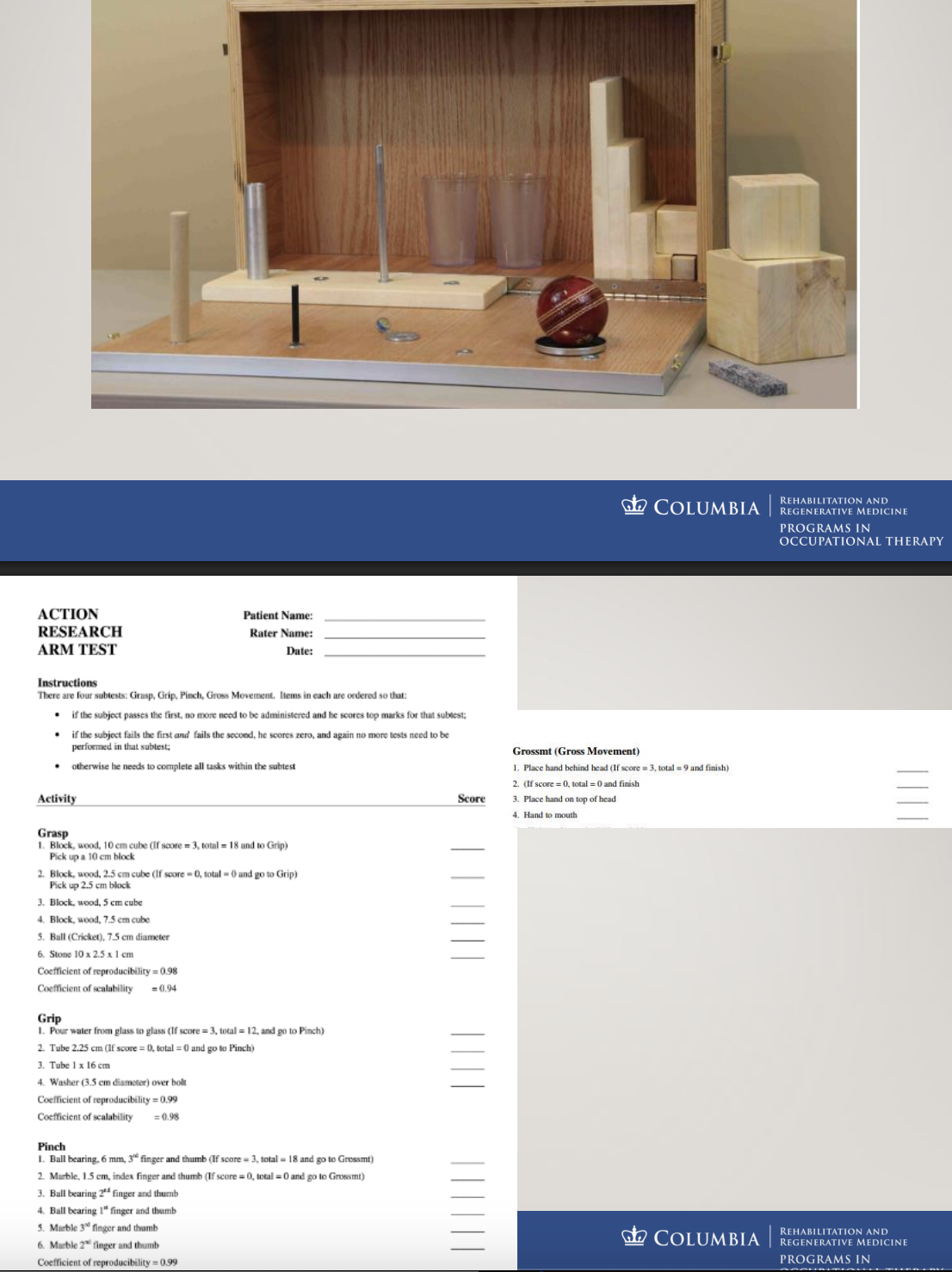
Action Research Arm Test (ARAT)
standardized objective assessment to measure arm and hand functional performance
Mostly used in research
Brain injury, stroke, MS
19 items divided into 4 subsets; hint: ARM TEST ==> what can you do with your UEs?
grasp (mostly this!),
grip,
pinch and
gross movements
typically asks the patient to move their arm to move certain items
hint: ACTION ==> asking patients to make their arm ACTIVE
Max score of 57, with higher scores indicating better performance
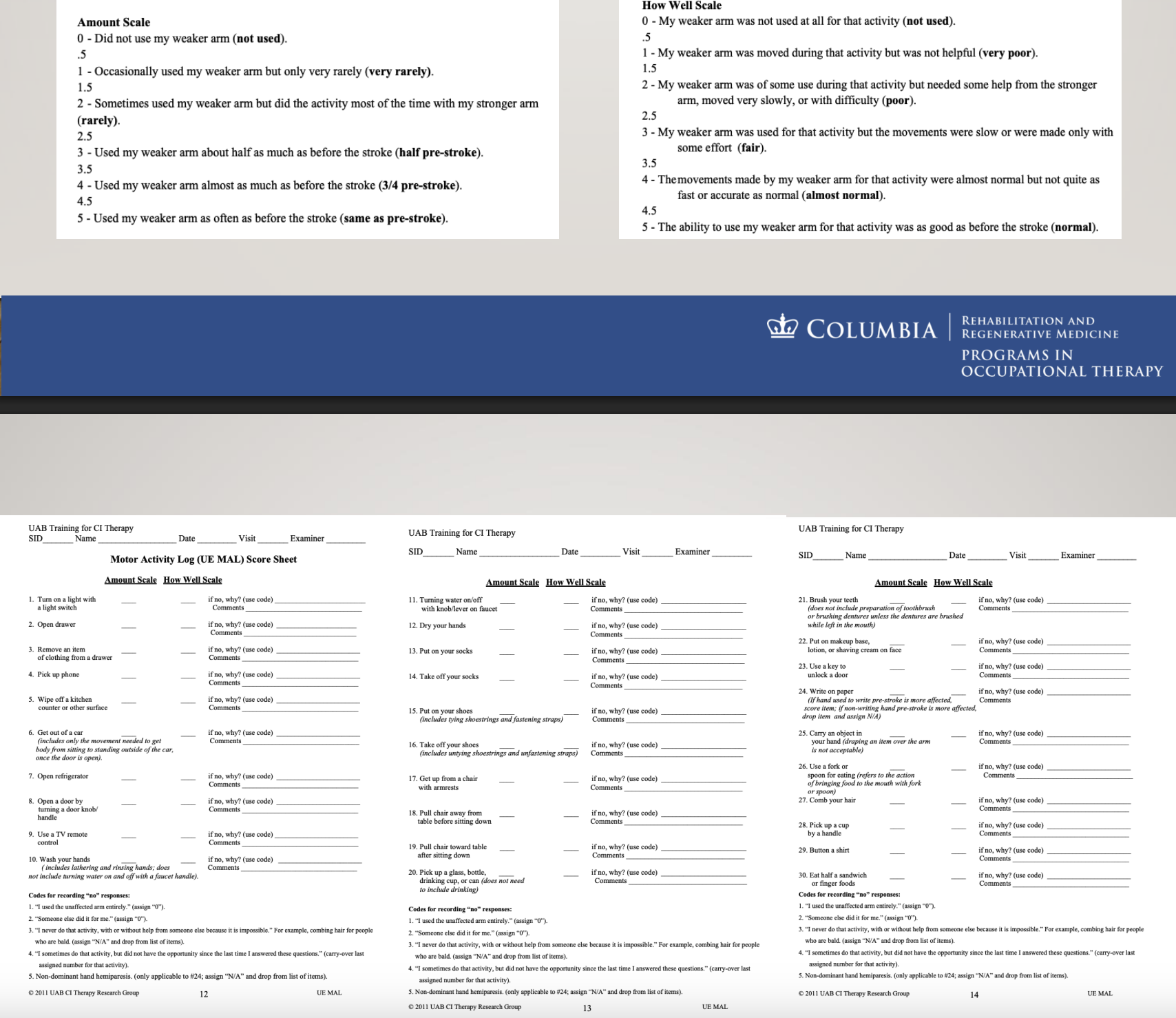
Motor Activity Log (MAL)
subjective measure; hint: LOG ==> subjective LOGGING of results by the interviewee
Structured interview to examine *how much and ***how well the stroke survivor uses their affected arm
Standardized questions (questionnaire/interview-type assessment, so it’s more subjective):
*Amount of use of their affected arm (Amount Scale or AS)
***Quality of their movement (How Well Scale or HW)
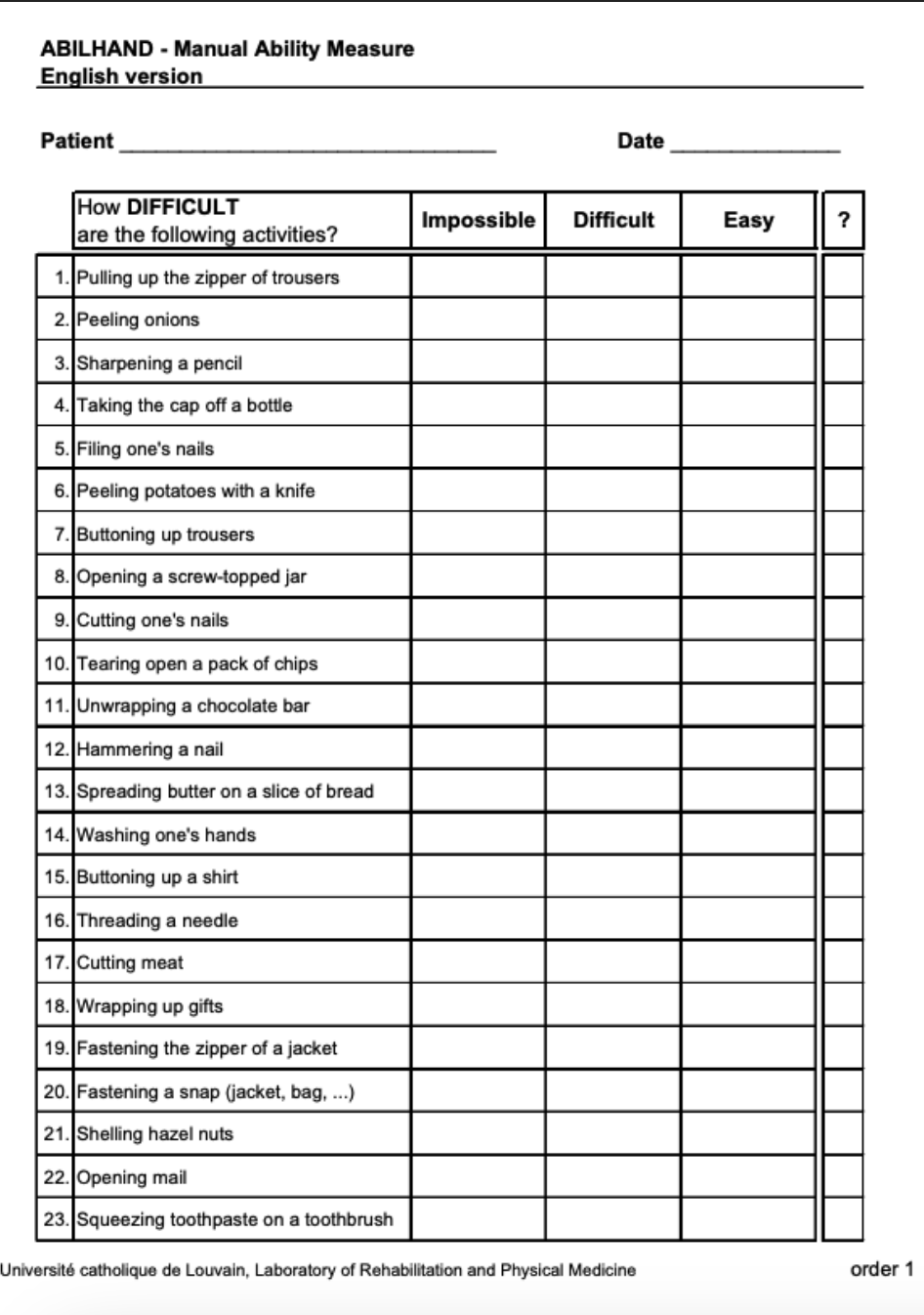
ABILHAND
subjective measure
Valid and reliable interview-based tool that measures participants’ perceived difficulty with the ***use of their arm and hands in 23 ***bimanual tasks
hint: BIL, HAND ==> use of BILateral HAND tasks; ABIL ==> see participant's subjective perception of what they’re ABLE to do
e.g., wrapping a gift, tying a shoelace
Arthritis, CP, MS, stroke, limb loss
Score: Impossible=0, difficult=1, easy=2, N/A=missing data
subjective information
Enter data into the website for results by diagnosis
***FUNCTIONAL UPPER EXTREMITY LEVELS (FUEL)
objective measure
FUEL is a semi-structured performance-based upper extremity classification system post-stroke
Mostly used in the clinic and can be used with any ADL, IADL, in any setting
7 levels: w/ more movement, a patient will move up these scales
(1) ***Non-functional
No voluntary movement or only reflexive activity; not used in daily activities
Presentation: flaccid or severely spastic limb
(2) ***dependent stabilizer
Arm can assist passively as a stabilizer, but cannot actively move
does not have enough motion to move their own arm + put it down on a surface to actively maintain a certain position
Presentation: limb positioned by the unaffected hand to help stabilize objects (e.g., unaffected arm places affected arm to hold paper while writing)
weak arm is dependent on the strong arm to help it, as it cannot stabilize itself for a task
(3) ***independent stabilizer
Arm can maintain a position independently, but without active manipulation
Presentation: can hold an object in place without help from the other hand (i.e., don’t need the stronger arm to help with stabilization), though not move it purposefully
e.g., holding paper while writing, supporting a bowl
(4) ***gross assist
some active movement; able to assist the unaffected arm in simple tasks
Presentation: can hold or stabilize items but has limited fine motor control, and no individuation (e.g., hold a cup while the other hand pours)
able to grasp things, but has no functional release (i.e., needs help of the stronger hand to release)
e.g., holding a cup while the other hand pours, stabilizing clothing
(5) ***proximal dependent semi-functional assist
Performs portions of tasks and begins fine motor movement
Presentation: reaches and grasps weakly, may manipulate light objects slowly and awkwardly (e.g., help fasten/button clothing, assist in washing face)
some fine motor, some gross grasp, some functional release
(6) semi-functional assist
Arm and hand perform more complex tasks, but are still slower or less coordinated than the unaffected side
Presentation: can use affected arm for most daily tasks (e.g., eating, grooming, folding laundry) though not fully efficient
(7) functional assist
Arm and hand function normally in daily life
Presentation: smooth, coordinated movement; strength and speed comparable to the unaffected side
e.g., writing, cooking, all ADLs/IADLs
Can be used for goal writing, treatment planning, and to track UE motoric and functional improvement
JEBSEN-TAYLOR HAND FUNCTION TEST (JTHFT)
objective measure
The Jebsen Taylor Hand Function Test (JTHFT) is a standardized and objective measure of fine and gross motor ***hand functions that uses simulated activities of daily living (ADLs)
hint: “HAND FUNCTION TEST” ==> HAND FUNCTIONS TESTED through ADL execution
Stroke, arthritis, Brain injury, SCI
7 subtests performed with both UE; hint: JEBSON-T has 7 letters ==> 7 subtests
writing,
tuning cards,
picking up small objects,
stacking checkers,
simulated feeding,
moving light and
heavy cans
Score: time to complete each task, with lower scores indicating greater function
INTERVENTIONS…
FUNCTION!
use arm as much as they can!
Push
Pull
Prop (up)
Reach
Slide (sliding objects)
Engage Hand via Placement
Grasp/manipulate
Carry….Etc….Etc
SUPPORT DAILY LIVING TASKS
PREPARATION: SOFT TISSUE ELONGATION (PROM)
Soft tissue elongation & mobilization
To maintain joint play/lubrication
Prevent secondary orthopedic complications
Deformity control
Deliberate/Frequent/Full Movement of Limbs with Terminal Stretch (Active vs. Passive)
LLPS (PROM) vs. HLBS (splinting)
24 Hour Positioning Protocol (while in bed, wheelchair)
Areas of concern
Mobility of the Scapula on the Thoracic Wall: retraction/downward rotation
Shoulder internal rotation
Elbow and wrist flexion
Composite flexion
Interossei and lumbrical tightness
PREPERATION: TREATMENT TO DECREASE EXCESSIVE SPASTICITY
Guide Appropriate Use of Available Motor Control (AAROM)
guide the movement that they do have to keep the arm moving
Maintain Soft Tissue Length (PROM)
Encourage Slow/Controlled Movement
Avoid Excessive Effort during movement
Relaxation and modalities
something warm could help
Weight Bearing
weight-bearing positions can help decrease tone
e.g., quadriped positions
Refer when appropriate for pharmacological interventions
e.g., botox could help- especially for getting rid of spasticity
Unfortunately, it does paralyze the muscle (keeps it from firing), so this may also affect people’s abilities to complete tasks
SHOULDER SUPPORT GOALS
Protect Joint Capsule
Prevent Overstretch of Supraspinatus
Support Weight of Arm
Prevent Distraction
i.e., prevent subluxation
SLING USE
MINIMIZED!!!!!!; it’s not bad, but we don’t want to be excessive with it (left picture is discouraged; middle and right pictures encouraged)
Initial Upright Function Training
Specific Activities
Immediate Removal
Avoid slings that position the shoulder in…
internal rotation and
elbow flexion
Investigate Alternate Means of Support

TAPING THE SHOULDER
KinesioTape- more flexible (left photo), providing more facilitation to strengthen muscles
Facilitates (weak) muscles or inhibits (tight) muscles
Removes swelling
Activates Analgesic System
Commonly used with little evidence
Athletic Tape/Strapping- more rigid (right photo), providing more structural support to put muscles back in place
1. Stabilizes
Re-aligns
Some evidence to decrease pain

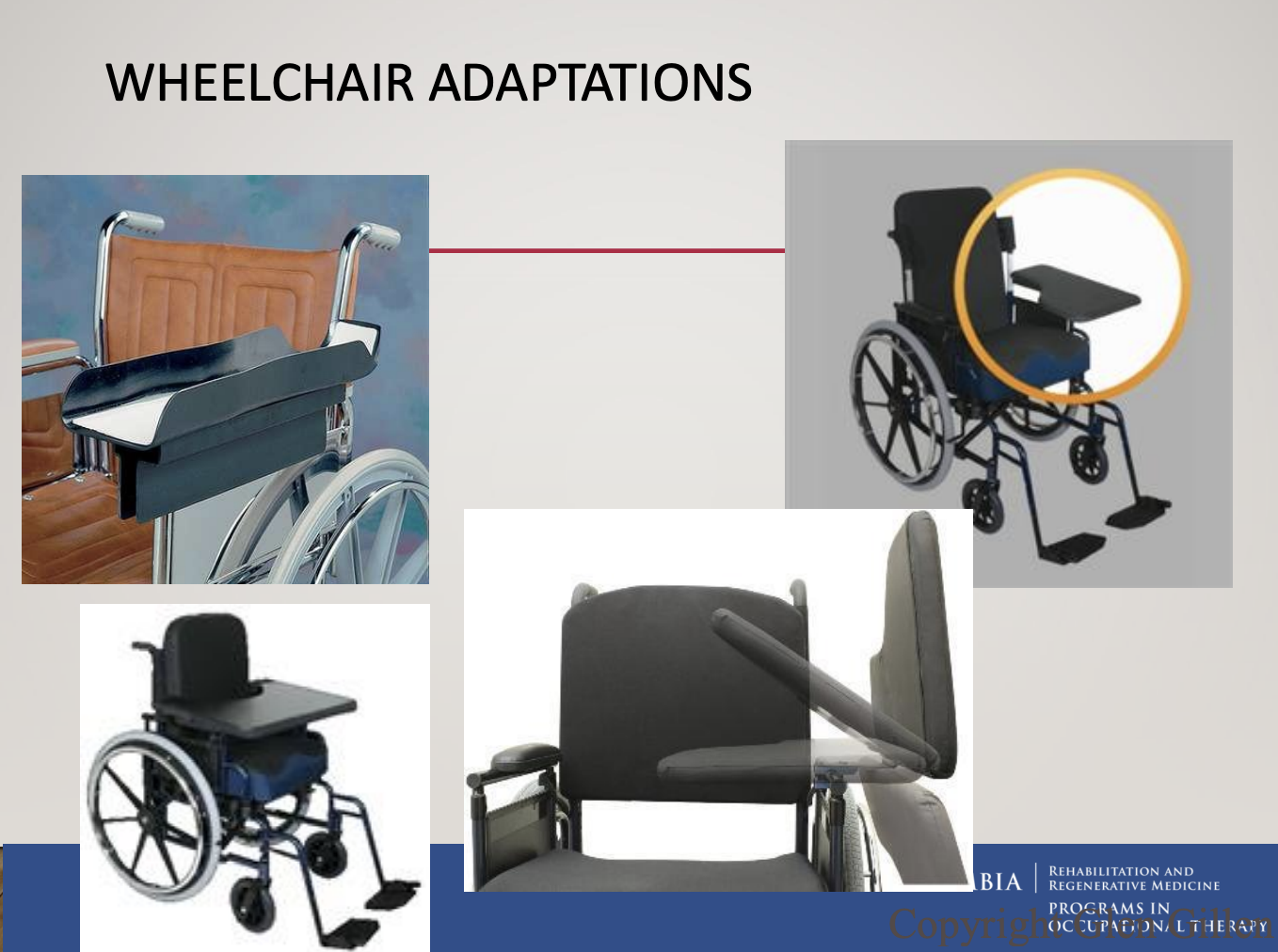
WHEELCHAIR ADAPTATIONS
to support the arm and shoulder when sitting in a wheelchair
to prevent subluxation
e.g.,
full-trays (left photo)
half-trays (right photo)
ELECTRICAL STIMULATION (ES)
ES reduces the severity of glenohumeral subluxation, but there was no significant effect on upper limb motor recovery or upper limb spasticity
potentially good for prepping before a session

TASK CHOICE TO REGAIN UPPER EXTREMITY CONTROL
function!
Fixed Distal Point Weight-Bearing (Forearm or Hand)
weight bearing through the extended arm
weight bearing through/on the forearm
Supported Reach (Closed chain activity)
for clients w/ less hand functions (b/c they can only work on proximal movements)
e.g., sliding a hand across a table, sliding a hand up a wall
Reach into Space (Opened chain activity)
just reaching up above
Grade Level of Antigravity/Gravity Motion and Amount of Support
Not a Developmental Process; you don’t need to go sequentially through these steps
e.g., can do reaching into space for 90% of the exercise, and then do the last 10% of reaching in a supported position
Muscle contractions are task-specific
Different Contractions (isometrics, concentric, eccentric)
But can train at different arm positions
e.g., Open chain to reach for lower-level items, then closed chain for high-level
WEIGHTBEARING ACTIVITIES
Impairment Level
Elongate Shortened Muscles
Postural Stability
Strengthening Proximal Groups
Sensory Input
Activity Level
Upright function
Improve the reach span of the opposite arm
Fall prevention
Assist transitional movements
Improve activity tolerance
PROVIDE OPPORTUNITY TO USE AND MOVE ALL DAY
give activities the patient can do outside of their therapy sessions; educate them on how to incorporate their arm into everyday tasks (repetition promotes neural learning)
Overhead suspension slings or mobile arm supports
Activity-based bedside and home program
Self PROM or Self AAROM
Set the patient up to perform self-care during off times (e.g., lunch, dinner, doffing clothing, before bed, grooming, etc.)
Mirror therapy, action observation, mental practice
Provide choices of activities for any and all available movement

EFFECTIVENESS OF VARIOUS TRADITIONAL APPROACHES (ADULT NEUROLOGY)
gist: do your prep work before your session —> and then get into task-related interventions (best way to go about sessions)
Rood: no research support
PNF: no research support
Movement Therapy (Brunnstrom): no research support
EFFECTIVENESS OF TASK ORIENTED INTERVENTIONS
gist: do your prep work before your session —> and then get into task-related interventions (best way to go about sessions)
Task-related training of UE and LE vs. control (immobilization): favored task-oriented
Task-specific reaching and balance vs. sham: favored task-oriented
Usual care vs. task practice vs. strengthening: favored task practice
Occupationally embedded exercise vs. rote exercise: favored occupationally embedded tx
NDT vs. Task-Oriented/MRP: favored task-oriented
NDT vs. Task-Oriented: favored task-oriented on functional measures
ADJUNCTIVE INTERVENTIONS (IN ADDITION TO USUAL OT CARE)
Mirror Therapy (MT)
Mental Practice (MP)
Action Observation (AO)
Robotics
NMES & Bioness
Virtual Reality
Saeboflex
Constraint Induced Movement Therapy (CIMT) and Modified Constraint Induced Movement Therapy (mCIMT)
MIRROR THERAPY (MT): WHAT IS IT?
Mirror therapy is designed to improve limb and ADL function poststroke through visual feedback
The visual feedback "tricks our brains" into thinking that the involved arm is moving (by looking at the mirror image of the unaffected hand)
Why does it work?
Not sure 100% but 3 theories
Increase attention to the affected side
Motor Neuron System
Motor system
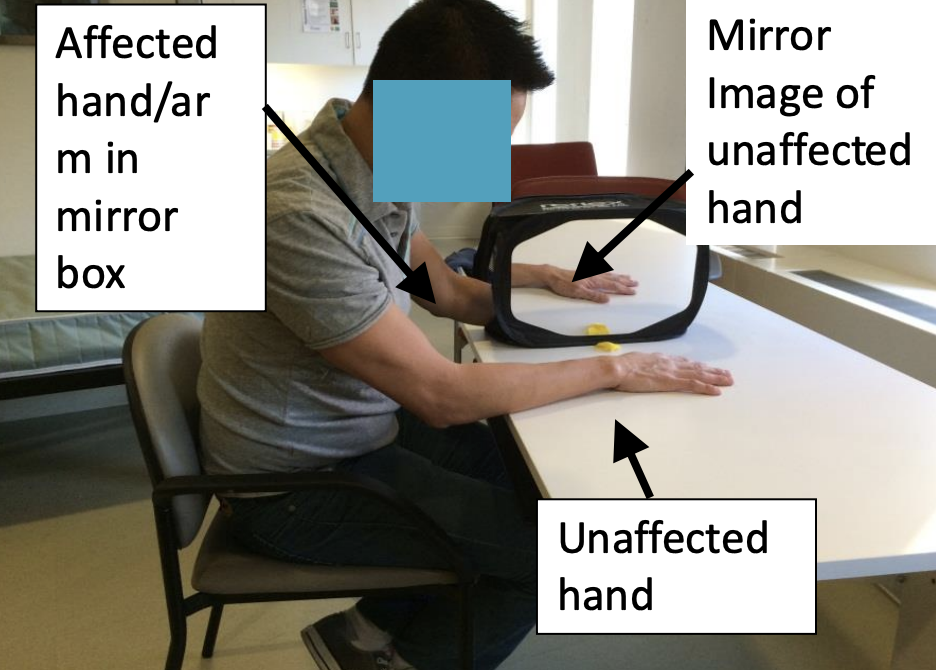
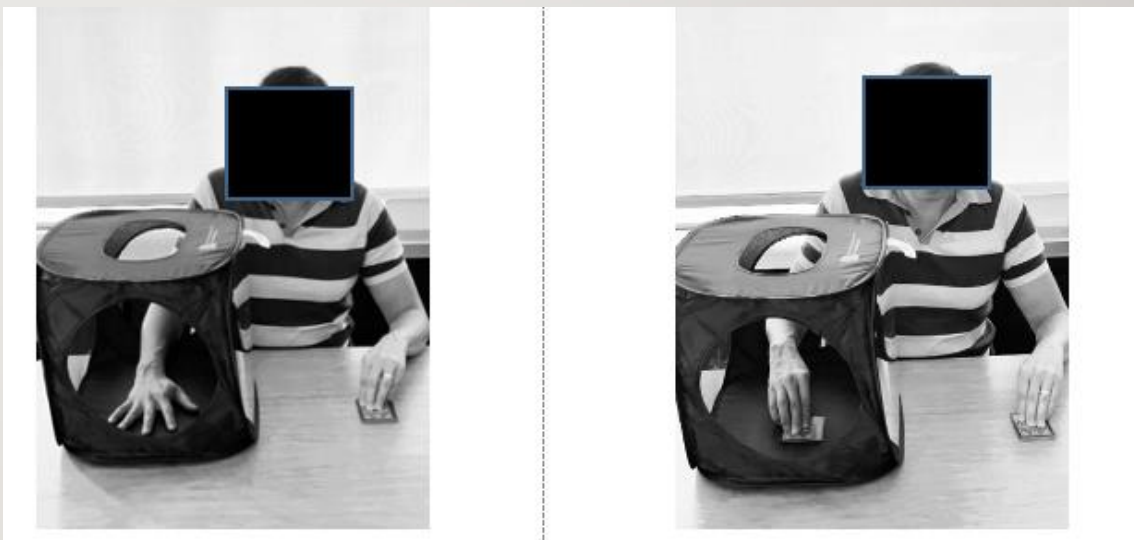
TWO APPROACHES (of mirror therapy) USED IN ADDITION TO USUAL OT
WHAT IS IT?
HOW IS IT DONE?
WHO IS A CANDIDATE?
Bimanual Mirror Therapy
trying to move (the hand inside the box) as much as possible; trying to duplicate the strong arm
Unimanual Mirror Therapy
hand (inside of the box) sits in there and does nothing; the patient solely observes the strong arm without attempting to duplicate it
research actually shows better improvements w/ this version, as the different feedback/conflict in bimanual mirror therapy (when the impaired side is unable to replicate the same movements as the strong arm) makes results worse
Who is a candidate?
Acute, subacute, chronic stroke
Cognitively able to follow directions and attend to tasks
No severe visual or perceptual deficits
No motor requirements (However, for research, they may need some movement)
MENTAL PRACTICE (MP)
WHAT IS IT?
HOW IS IT DONE?
WHO IS A CANDIDATE?
Mental Practice: a training method of mental rehearsal with the goal of improved performance in the absence of physical practice
MP can be conducted before or after traditional OT
Usually administered through a CD recording of the therapist’s voice; they are approximately 10-15 minutes in length:
10 minutes in length (utilized 2x daily)
Starts with a focusing exercise
Mental Imagery for specific tasks (ADL, reaching, etc.)
Repetition is built into the scripts
Ends with refocusing
Candidate:
cognitively intact (must be able to attend/have general cognitive functioning)
no motor requirements
==> can be used for upper limb recovery (e.g., for someone who is more flaccid)

ACTION OBSERVATION (AO)
WHAT IS IT?
HOW IS IT DONE?
WHO IS A CANDIDATE?
Action observation is an intervention in which a person observes a ”typical” person perform a functional task either by video or though live performance in the stroke population
Usually, the person is asked to practice the task after AO
Candidate:
cognitively intact,
no motor requirements,
however, some movement to perform task after AO
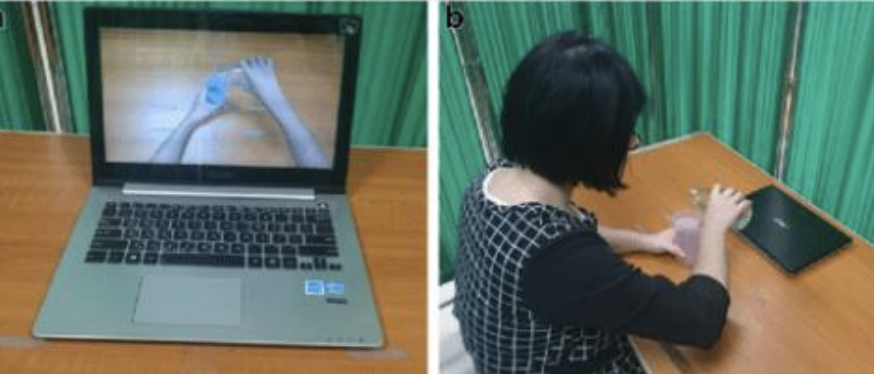
image e.g.,
patient watches a video and tries to replicate it
ROBOTICS
WHAT IS IT?
HOW IS IT DONE?
WHO IS A CANDIDATE?
Robots are defined as programmable, multifunctional manipulators that can move limbs to accomplish tasks
Place the arm in the robot, and the robot assists the hand in movement
Increase dosage, consistent practice, and reduce the burden on OT
Candidate:
No severe tone (will not fit into the robot if tone is too strong),
minimal hand and arm requirements

DO ROBOTICS WORK?
Many studies have been shown to improve motor function (i.e., proximal arm function); however, they do not appear to improve hand function, ADL, or muscle tone
NEUROMUSCULAR ELECTRICAL STIMULATION (NMES) & BIONESS
WHAT IS IT?
HOW IS IT DONE?
WHO IS A CANDIDATE?
NMES is a method to facilitate limb movements by using electrical current to paretic limbs; good to use during session functional tasks, and exercises (as long as it’s timed correctly)
usually for elbow and wrist extension
Functional electrical stimulation (FES) is a subcategory of NMES and is defined as the use of e-stimulation during voluntary movement
Candidate:
No contraindication (e.g., pacemaker),
Requires MMT 1/5,
Able to tolerate

Bioness: H200, L300
WHAT IS IT?
HOW IS IT DONE?
helps with tasks such as grasp (UE), release (UE), extending (UE or for someone w/ foot drop (right photo))

VIRTUAL REALITY
WHAT IS IT?
HOW IS IT DONE?
WHO IS A CANDIDATE?
Virtual reality (VR): use of interactive simulations for patients to engage in environments that feel similar to the real environment and increase practice through games
In VR, patients can interact with virtual environments and objects either through head-mounted devices or flat screens
Candidate:
Require some movement,
Can cause virtual sickness,
No severe tone

SAEBOFLEX & SAEBO REACH
WHAT IS IT?
HOW IS IT DONE?
WHO IS A CANDIDATE?
Dynamic orthosis developed for stroke survivors who have difficulty with hand function
springs open your hands for you (for someone who needs to practice grasp and release exercises)
Used during repetitive task practice to improve UE motor function
candidate
Recovering from stroke, TBI, SCI, radial nerve palsy
Hand and arm weakness, wrist drop, or unable to open the hand
Minimum 15 degrees of shoulder AROM in any direction
Minimum 15 degrees of elbow flexion AROM
Passively position the wrist in 15 degrees of extension with the finger straight
Some ability to pick up items
Minimal to moderate spasticity in hand/wrist (possibly severe)

CONSTRAINT INDUCED MOVEMENT THERAPY (CIMT) & MODIFIED CONSTRAINT INDUCED MOVEMENT THERAPY (MCIMT)
WHAT IS IT?
MOTOR CRITERIA
COMPONENTS OF THE INTERVENTION
Constraint Induced Movement Therapy (CIMT) is an intervention developed to reverse the effects of learned non-use
Hypothesized causes of learned non-use:
Negative reinforcement experienced by the patients as they unsuccessfully attempt to use the affected limb
Positive reinforcement experienced by using the less involved hand and/or use of successful adaptations
Motor Criteria
20 degrees of extension of the wrist and 10 degrees of extension of each finger or
10 degrees extension of the wrist, 10 degrees abduction of the thumb, and 10 degrees extension of any two other digits or
Able to lift a wash rag off a table using any type of prehension and then release it
Components of the Intervention
Repetitive, ***mass practice!, task-oriented training (this is the key to the intervention)
***Shaping/Grading
Shaping= have them do little bits at a time and reward small progress towards a more complex skill
Grading= making the activity easier or harder to meet them where they are
Task Practice
Adherence-enhancing behavioral strategies — ***Transfer Package
Behavioral contract (i.e., contract to sign saying you will do everything you need to do, even at home (e.g., at-home exercises))
Home diary
Home skill assignment
Home practice
Motor Activity Log
***Constraining the use of the non-affected UE
Mitt restraint or cast for kids
Any method to continually remind the participant to use the more affected UE
! = involves performing a skill or task with very few or no breaks, aiming to maximize repetitions in a short period (different from rote exercise, which is a type of learning that uses repetition without deep engagement, for memorizing procedures)
mass practice is better for physical skills and motivated learners
remote exercise focuses more on memorization and lacks deeper understanding or critical thinking
PROTOCOLS: TRADITIONAL CIMT
Wear a protective safety mitt on the unaffected hand for 90% of their waking hours over a 2-week period, including 2 weekends, for a total of 14 days
On each weekday, participants received ***shaping (adaptive task practice) and standard task training of the paretic limb for up to 6 hours per day
***= process of training the affected arm through a series of tasks that are progressively more difficult, with rewards given for improvements
PROTOCOLS: MODIFIED CIMT
Over a 10-week period, subjects' less affected arms were restrained every weekday for 5 hours
Half-hour, one-on-one sessions of more affected arm therapy occur 3 days per week during the 10-week period; this component included ***shaping (adaptive task practice)
***= process of training the affected arm through a series of tasks that are progressively more difficult, with rewards given for improvements
functional vs nonfunctional arm
Functional Arm
An arm that can be actively and purposefully used during daily activities (ADLs/IADLs)
Key Features:
Has voluntary movement, strength, and coordination
Can reach, grasp, release, and manipulate objects effectively
Contributes meaningfully to bilateral or independent tasks
Examples of use:
Brushing teeth or feeding self oneself
Reaching for and lifting a cup
Typing, writing, or buttoning clothing
Nonfunctional Arm
An arm that cannot be used actively or effectively for functional tasks.
Key Features:
Little to no voluntary movement
May show flaccidity, spasticity, or poor motor control
Cannot assist or only provides passive support/stabilization
Often dependent on positioning or the unaffected hand for placement
Examples of use (if any):
Used passively for support (e.g., resting on a table)
May be positioned to prevent injury or assist with balance