2. Foodborne Illnesses - Gram Positive Pathogens
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
What is a spore?
Produced by bacteria, moulds and yeasts
Endospore, endo = inside
moulds also use it to reproduce
Resistant structures
Role in spoilage and disease
Dormant structure: no metabolic activity
DNA is present in the core
Different protective layers
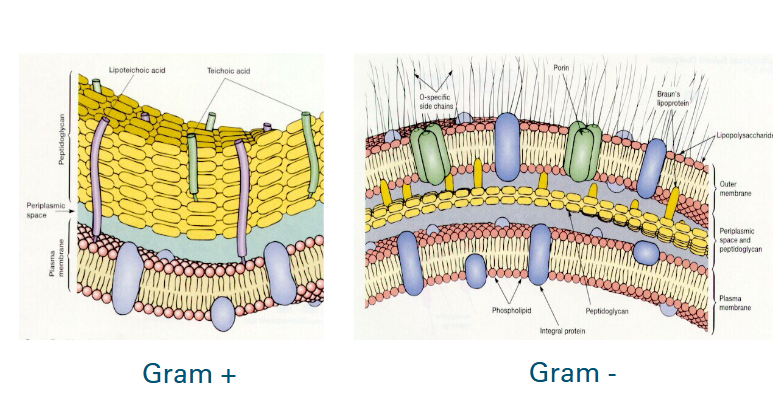
Gram positive vs Gram negative
What are spores resistant to?
Wet heat
Dry heat
UV and gamma radiation
Extreme dessication
Oxidative chemicals
Listeria monocytogenes
Gram +
Motile rod
Facultative anaerobe
Ubiquitous pathogen (an organism that causes disease and is widespread and abundant in its environment)
Salt tolerant (Awmin = 0.92)
Grows in chilled foods (Tmin = 0 C)
Different Listeria species
There are 6 listeria species: only L. monocytogenes is pathogenic for humans
The invasive listeriosis has had 4 confirmed cases per million people
Of all confirmed cases 16-30% die.
What can Listeriosis do to you?
Mild intestinal illness:
Gastro-enteritis, mild flu-like illness
Incubation time: <1 day - 48h, lasts 1-3 days
Severe illness
Stillbirth (fetus), septicemia, meningitis
Incubation time: <1 day - 3 months
YOPI
Consumers considered most vulnerable to foodborne illness include the young (0-5 years), older (65+ years), pregnant, and immunocompromised -
L. monocytogenes in foods
Deli meats
Soft cheese
Raw milk
Pate
Smoked and lightly processed fish
Ready to eat foods
Does MAP & vacuum packaging prevent growth of L. monocytogenes?
No
Prevention of growth of L. monocytes
Restrict outgrowth during storage:
pHmin = 4.3
Awmin = 0.92
Heat the product
D-value in milk = 1-2 s at 71.7 C
Pasteurization (15s at 71.7 C) sufficient to inactivate L. monocytogenes
Staphylococcus aureus characteristics
Gram +
Coccus
Growth range: 7-48C
Facultative anaerobic bacterium
Remarkably salt tolerant (Awmin = 0.83)
Bad competitor
Toxin in Staphylococcus
Produced by 50-70% of the strains
Produced in the food
Heat stable
Symptoms in Staphylococcus
Mild symptoms, vomiting
Incubation time: 0.5-6h
duration 1-2 days
Staphylococcus aureus on food
Low level of initial contamination
additional growth needed for toxin production
Temperature abuse
Protein-rich food, limited microbial competition
Heated foods, which are recontaminated
Meats that are salted (awmin = 0.83), salmon
Which pathogen has a higher disease burden per case?
L. monocytogenes
How are spores formed?
Due to stress response induced by nutrient limitation
vegetative cell
sporulating cell
spores (released when cell lyses)
Waking up of spores
Known as germination: spore → vegetative cells
Nutrients trigger germination because environment becomes favourable
Outgrowth occurs: reproduction of vegetative cells
Spore formers
Food spoilage
Bacillus subtillis
Food pathogens
Bacillus cereus
Clostridium botulinum
Clostridum perfringens
Non-food related pathogens
Bacillus anthracis
Bacillus thuringiensis
Where is Bacillus cereus found? (Resevoir) and what does it contaminate?
Soil
Contaminates:
Raw food, like cereals and vegetables
Found in dust in food processing environments
Bacillus Cereus characteristics
Can form spores, hence is found even in cooked foods
Spores can even germinate when not stored properly.
Forms toxins.
Gram positive
Facultative anaerobe
Spore forming rods
Food poisoning by Bacillus cereus
Diarrhoeal Syndrome
Similar to Clostridium perfringens food poisoning
Caused by enterotoxins produced by the bacteria growing in the small intestine of the host.
Appears 8-16 hours after consumption and last 12–24 hours.
Abdominal pain, watery diarrhoea, nausea
Emetic syndrome:
Similar to Staphylococcus aureus
caused by a toxin which is acid and heat resistant
Known as cereulide, a cyclic peptide toxin
Is preformed in food (toxins are there before consumption)
incubates for 0.5-5 hours
is dominated by nausea and vomiting, lasting 6-24 hours
Bacillus cereus in foods
Ubiquitous
Associated with boiled and fried rice that has been held at warm temperatures.
Meat products, vegetables, soups, puddings, sauces, dried herbs and pasta.
When are B. cereus toxins produced?
Late exponential/early stationary phase
Clostridium perfringens illness
Onset of illness 8-16 hours after food consumption, lasting between 12 and 24 hours
Symptoms include abdominal pain, profuse watery diarrhoea
Caused by an enterotoxin released by vegetative cells sporulating in the host small intestine
Can also cause wound infections
Clostridium p. in foods
Usually Linked to meat products such as stews, meat gravies, roast joints, and pies
Vegetables, spices and herbs
Cooking kills vegetative cells but not heat-resistant spores
Clostridium perfringens characteristics
Rod shaped
Gram positive
Oval spores
non-motile
Catalase negative
largely anaerobic (can survive in oxygen)
Clostridium botulinum in foods
Found in aquatic muds, soil
Frequently linked to home produced foods rather than commercial. (or underprocessed foods)
Involving: vegetables and fish
Clostridium botulinum characteristics
Gram positive
Rod shaped
Motile
Spore forming
Obligately anaerobic
Neurotoxin producer
It can be activated in the gut of humans
Clostridium botulinum illness
Causes botulism
Due to neurotoxin
Toxin types that cause botulism: A, B, E & F (F in rare cases)
pH and Clostridium botulinum
The consensus is that a pH around 4.7 represents an absolute minimum for C. botulinum to grow
Infant botulism
Infant botulism differs from the classical foodborne syndrome in that it results from the colonization of the infant's gut with Clostridium botulinum and the production of toxin in situ (within the body). This requires the ingestion of viable spores, not pre-formed toxin
Often caused by honey, thefore kids under a year should not consume honey
Characteristics of viruses
Small (25-300 nm = 0025-0.3 micrometer))
Genome: DNA or RNA (never both)
Proteins coating or surrounding the genome
Capsid (protein shell)
needs external host to multiply
No growth in foods
Host specific
Do viruses or bacteria cause more outbreaks?
Viruses, which are mostly caused by the norovirus or hepatitis A
Norovirus (NV)
Calicivirus family
Gastroenteritis: vomiting, diarrhoea
Incubation time: 15-50h
Duration:24-48h
No vaccination possible
Low dose pathogen: 1-10 particles sufficient to cause disease
Contamination cycle of Norovirus
Human: will multiply the norovirus in intestine and virus leaves body through faeces.
Faeces go into the sewage and virus can get in water
Water might be used for irrigation of fruits & vegetables.
Water might be used to grow shellfish
Virus might also spread from hand to food
Hepatitis A
Picornavirus family
Invasive virus:
Anorexia, fever, malaise, nausea, vomiting
Liver damage: dark urine, jaundice
Incubation time: 2-6 weeks
Duration: 8 weeks
Vaccination possible
Same routes as norovirus
Determination of presence of viruses
Tissue culture (not for human NV, therefore often surrogate/model viruses used in infectivity assays)
Electron-microscopy (high Detection limit)
Immunologic methods (high DL)
DNA techniques such as RT-PCR
High detection limit = many virus particles need to be present
Preventative measures to prevent viruses from spreading
use of uncontaminated water
hygiene
strict rules food workers
heating if possible
Problems with spore formers
They are ubiquitous: raw material, environment, equipment
They survive during mild processing (not sterilization)
Which bacteria will NOT grow under vacuum?
Campylobacter, pseudomonas and bacillus