PANCE Blueprint Reproductive - All Smarty PANCE reproductive flashcard lesson sets combined (Smarty PANCE)
1/699
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
700 Terms
What is a breast abscess?
A breast abscess is a pus-filled lump that grows under the skin as a result of an infection. Most common in non-lactating women, symptoms same as mastitis but less severe.
Causes of breast abscess?
Breast abscesses develop most commonly as a progression of non lactational mastitis or cellulitis that does not respond to antibiotic treatment, but an abscess can also be the first presentation of breast infection.
The most common bacteria of breast abscess?
The most common bacteria are Staphylococcus aureus and Streptococcus. Sometimes anaerobic bacteria can cause breast abscesses.
Symptoms of breast abscess?
Patients with primary breast abscess present with localized, painful inflammation of the breast associated with fever and malaise, along with a fluctuant, tender, palpable mass
What is the treatment of breast abscess?
Management of primary breast abscess consists of drainage and antibiotic therapy. In the setting of lactational infection, milk drainage (either by breastfeeding or pumping) is important for resolution of infection and relief of discomfort
What must be ruled out with a breast abscess in a nonlactating woman?
Inflammatory breast cancer should be considered if a breast infection does not resolve with appropriate treatment
What is lactational mastitis?
Infection of the breast during breastfeeding (no abscess) —most commonly caused by S. aureus; treat with antibiotics and follow for abscess formation
What is a fibroadenoma?
Fibroadenoma is a benign, slow-growing breast tumor w/ epithelial and stromal components. Most common benign breast lesion in women <30yo.
What is the clinical presentation of a fibroadenoma?
Solid, mobile, well-circumscribed round breast mass, usually < 40 years of age
What is the recommended work-up for suspected fibroadenoma?
Diagnostic mammogram with ultrasound. If indeterminant, fine-needle aspiration of the mass with pathology. In women younger than 25 years, fibroadenomatous mass should be biopsied.
What is the treatment?
Surgical resection for large or growing lesions; small fibroadenomas can be observed closely
How is a well-defined solid mass with imaging features consistent with fibroadenoma managed?
A well-defined solid mass with imaging features consistent with fibroadenoma can be managed with core biopsy or short-term (three to six months) follow-up with a repeat ultrasound and breast examination. Definitive diagnosis can only be confirmed with a core biopsy or excision.
Are women with simple fibroadenomas at increased risk of developing breast cancer?
For the majority of women with simple fibroadenomas, there is no increased risk of developing breast cancer. The risk of subsequent breast cancer is slightly elevated only if there is associated proliferative disease or if there is a significant family history of breast cancer.
What is fibrocystic breast disease?
Fibrocystic breast disease, commonly called fibrocystic breasts or fibrocystic change, is a benign (noncancerous) condition in which the breasts feel lumpy. Fibrocystic breasts aren't harmful or dangerous, but may be bothersome or uncomfortable for some women.
Symptoms is fibrocystic breast disease?
Symptoms include a change in breast texture, pain or tenderness, and lumpiness. These may be more bothersome before menses and usually resolves with the start of the menstrual cycle
Peak incidence of fibrocystic breast disease?
Peak incidence of fibrocystic breast disease is 30 to 40 year old's
What distinguishes fibrocystic breast changes from carcinoma?
Pain, size fluctuation, and multiple lesions distinguish fibrocystic changes from carcinoma. A huge clue that this is fibrocystic disease is that the pain is commonly worse and mass size increases during the premenstrual part of the cycle
After the establishment of fibrocystic breast disease, what is the recommended treatment?
Avoiding trauma and by wearing a bra with adequate support. Combined oral contraceptive agents limit the severity of the cyclical changes in the breast tissue. Many patients report relief of symptoms after abstinence from coffee, tea, and chocolate.
Women should be encouraged to perform monthly self-breast exams when?
Women should be encouraged to perform monthly self-breast exams one week after a period when cysts are at their smallest
Are fibrocystic changes harmful?
Fibrocystic breast changes aren't harmful. And the chances of getting cancer don't increase if patient's have them. But it can make it tricky to feel for new lumps or changes in the breasts during self-exams
What is galactorrhea?
Galactorrhea is a milky nipple discharge unrelated to the normal milk production of breast-feeding. Galactorrhea itself isn't a disease, but it could be a sign of an underlying problem
What is the most common cause of galactorrhea?
Galactorrhea is generally due to a prolactin-secreting pituitary adenoma (prolactinoma).
● May be caused by ingestion of certain drugs
● Primary hypothyroidism can cause hyperprolactinemia and galactorrhea
● Prolactin levels may rise in circulation as a consequence of renal insufficiency
● Nipple stimulation and pregnancy are physiologic causes of increased prolactin secretion
Signs and symptoms associated with galactorrhea?
Signs and symptoms associated with galactorrhea include persistent or intermittent milky nipple discharge may be spontaneous or expressed, one or both breasts, absent or irregular menstrual periods, headaches, or vision problems
What pattern of nipple discharge would one expect with benign galactorrhea?
Bilateral, induced, clear/white/yellow color
Diagnosis of galactorrhea?
Diagnosis of galactorrhea due to a prolactin-secreting pituitary adenoma is based on elevated prolactin levels (typically > 5 times normal, sometimes much higher)
● MRI is the method of choice in identifying microadenomas. High-resolution CT may be used when MRI is contraindicated or unavailable.
● Serum gonadotropin and estradiol levels are either low or in the normal range in women with hyperprolactinemia, and testosterone levels may be low in men. Primary hypothyroidism is easily ruled out by absence of elevated TSH.
Treatment of galactorrhea?
The initial treatment for both sexes is usually a dopamine agonist such as bromocriptine or cabergoline which lower prolactin levels. Surgery is second-line therapy in patients whose tumor is resistant to dopamine agonists or patients who are intolerant of medical therapy
Radiation therapy should be used only in patients with progressive disease who do not respond to other forms of therapy.
What is gynecomastia?
Gynecomastia is a common condition which results in enlarged male breast tissue. It can be seen in males of all ages, but usually occurs during the newborn period, puberty and older adulthood
What is pseudogynecomastia?
Pseudogynecomastia is increased breast fat, but no enlargement of breast glandular tissue
Symptoms of physiologic gynecomastia?
Enlargement is usually transient, bilateral, smooth, firm, and symmetrically distributed under the areola; breasts may be tender.
What is the cause of physiologic gynecomastia that develops during puberty?
Physiologic gynecomastia that develops during puberty is due to fluctuating hormones, including drops in testosterone and surges in estrogen that cause breast tissue to grow and usually resolves within about 6 months to 2 years
In adult men, what are the most common causes of gynecomastia?
In adult men, the most common causes are persistent pubertal gynecomastia, idiopathic gynecomastia, and drugs (particularly spironolactone, anabolic steroids, and antiandrogens)
Diagnosisis of gynecomastia?
Extensive testing is often unnecessary, especially for patients in whom the gynecomastia is chronic and detected only during a physical examination. Patients with physiologic or idiopathic gynecomastia are evaluated again in 6 months. If breast cancer is suspected, mammography should be done. If another disorder is suspected, appropriate testing should be done
Treatment of gynecomastia?
In most cases, no specific treatment is needed because gynecomastia usually remits spontaneously or disappears after any causative drug (except anabolic steroids) is stopped or an underlying disorder is treated
What is mastitis?
Superficial infection of the breast (cellulitis)
In what circumstance does it most often occur?
Breast-feeding - Mastitis usually occurs within the first few weeks of breastfeeding but may occur later on
Mastitis symptoms?
Mastitis symptoms may include high fever and breast symptoms: erythema, induration, tenderness, pain, swelling, and warmth to the touch. Mastitis is different from the pain and cracking of nipples that frequently accompanies the start of breastfeeding.
Infectious vs. congestive mastitis
Infectious (unilateral) - Unilateral, fever, chills and color change
Congestive (bilateral) - Bilateral breast engorgement that usually occurs in primigravidas (first pregnancy)
What is the most common causative organism in mastitis, breast infection, or breast abscess?
Staphylococcus aureus
What is the treatment for acute mastitis?
Warm compresses to breast, analgesics, dicloxacillin, or a cephalosporin
How is mastitis diagnosed?
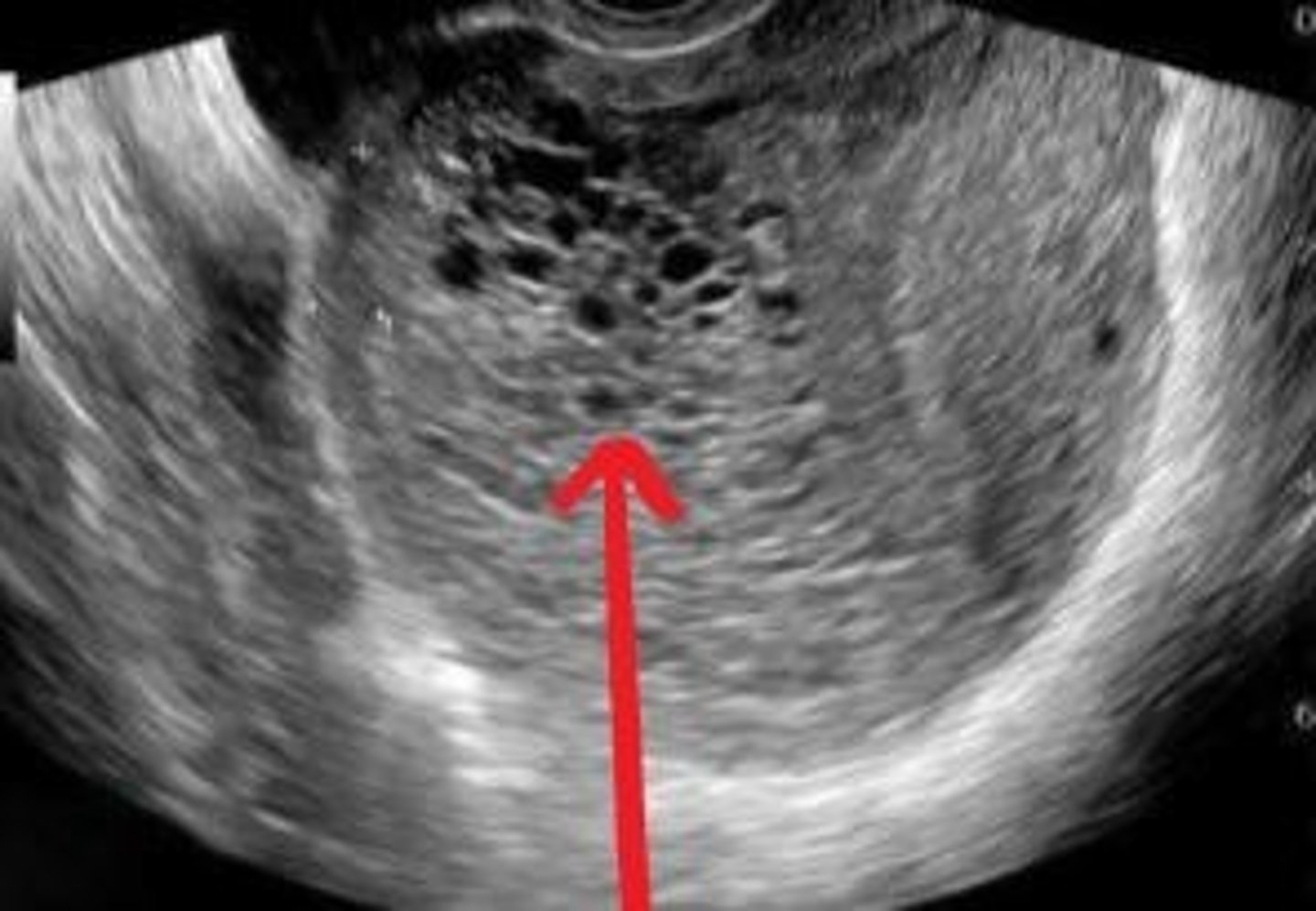
Diagnosis is clinical - if an abscess is suspected and ultrasound may be warranted
Can a nursing mother with mastitis continue to nurse?
Yes! Nursing facilitates the drainage of the infection and the infant will not be harmed because he/she is already colonized
Why must the patient with mastitis have close follow-up?
To make sure that she does not have inflammatory breast cancer! Inflammatory breast cancer presents with breast tenderness and color change, but fever and chills are not usually present
What is cervicitis?
Cervicitis is inflammation or infection of the cervix. This usually occurs due to sexually-transmitted diseases, such as chlamydia or gonorrhea. Chemical irritation from lubricants, spermicides, or douching may also cause cervicitis. Bacterial vaginosis may also cause a bacterial infection of the cervix.
Cervicitis symptoms?
Cervicitis may not cause symptoms. The most common symptoms are vaginal discharge and vaginal bleeding between menstrual periods or after coitus. Some women have dyspareunia, vulvar and/or vaginal irritation, and/or dysuria.
Diagnosis of cervicitis?
Pap smear with gonorrhea and chlamydia cultures should be done for a definitive diagnosis. Wet prep + KOH + nucleic acid amplification testing (NAAT) from a swab of the cervix, screen for other STIs (RPR, HIV, HSV)
Is cervicitis always cause by an STI?
Though sexually transmitted infections are the most common cause of the cervicitis, it can also be caused by allergies, injury and vaginal bacteria imbalance (bacterial vaginosis), among other things.
Cervical motion tenderness should make you think of what?
PID
Vesicles, vulvar or vaginal pain, and/or ulceration should make you think of what?should make you think of what?should make you think of what?
HSV infection
Punctate hemorrhages (strawberry spots), green and frothy should make you think of what?
Trichomoniasis
Clear/scant vaginal discharge should make you think of what?
Chlamydia
Mucopurulent vaginal discharge should make you think of what?
Gonorrhea
Fever should make you think of what?
Pelvic inflammatory disease (PID) or HSV infection
Grayish and frothy with an amine ("fishy") odor and clue cells should make you think of what?
Bacterial vaginosis (Gardnerella vaginalis)
Examination findings of cervicitis?
Examination findings can include purulent or mucopurulent discharge, cervical friability (eg, bleeding after touching the cervix with a swab), and cervical erythema and edema
Treatment of cervicitis?
Treat most women for chlamydial infection and gonorrhea at the first visit. Once the cause or causes are identified based on the results of microbiologic testing, subsequent treatment is adjusted accordingly.
Treatment of trichomonas and BV?
Metronidazole (Flagyl)
Treatment of gonorrhoeae?
Ceftriaxone (Rocephin)
Treatment of chlamydia?
Doxycycline or azithromycin
Treatment of HSV?
Acyclovir (Zovirax)
What is cervical dysplasia?
The abnormal growth of cells on the surface of the cervix. Cervical dysplasia is usually caused by certain types of human papillomavirus (HPV) and is found when a Pap test or cervical biopsy is done. It can be mild, moderate, or severe, depending on how abnormal the cells look under a microscope and how much of the cervical tissue is affected. Cervical dysplasia is not cancer, but may become cancer and spread to nearby normal tissue.
RFs for cervical dysplasia and cervical cancer?
RFs for cervical dysplasia and cancer include:
- Early intercourse
- Multiple sex partners
- HPV
- Smoker
- HIV/IC'd
- EtOH
- OCPs
Mgmt of ASC-US or LSIL in women 21-24 year old?
Repeat in 1 year
Mgmt of ACS-H, HSIL, or AGC in women 21-24 y?
Colposcopy with cervical biopsy
Mgmt of ASC-US (HPV not done) in women > 25 y?
Repeat cytology in 1 year (acceptable) OR HPV testing (preferred)
Mgmt of ASC-US + high-risk HPV negative in women > 25 y?
Repeat in 3 YEARS
Mgmt of ASC-US + high-risk HPV positive in women > 25 y?
Colposcopy and cervical biopsies
Mgm of LSIL in women > 25 y/o if HPV negative
vs. LSIL in women > 25 y/o if HPV positive?
HPV negative: repeat co-testing in 1 year
HPV positive: colposcopy and bx
Mgmt of HSIL in women > 25?
Colposcopy with endocervical assessment + cervical biopsies if indicated OR immediate LEEP/loop
Mgmt of AGC in women > 25?
Colposcopy, HPV screen, cervical biopsies, endocervical sampling AND endometrial biopsy in women aged 35 or older (or with RFs)
Mgmt of ASC-H in women > 25?
Colposcopy
Women with CIN II and CIN III biopsies require what?
Treatment with surgical excision, typically with LEEP
Patients w/ a Pap test reading of atypical glandular cells (AGC) should what?
Undergo colposcopy with endocervical sampling
Patients who receive an ASC-H or high-grade squamous intraepithelial lesion (HSIL) seed what?
Colposcopy
T or F: HPV testing should not be performed for women aged 21 to 24.
True
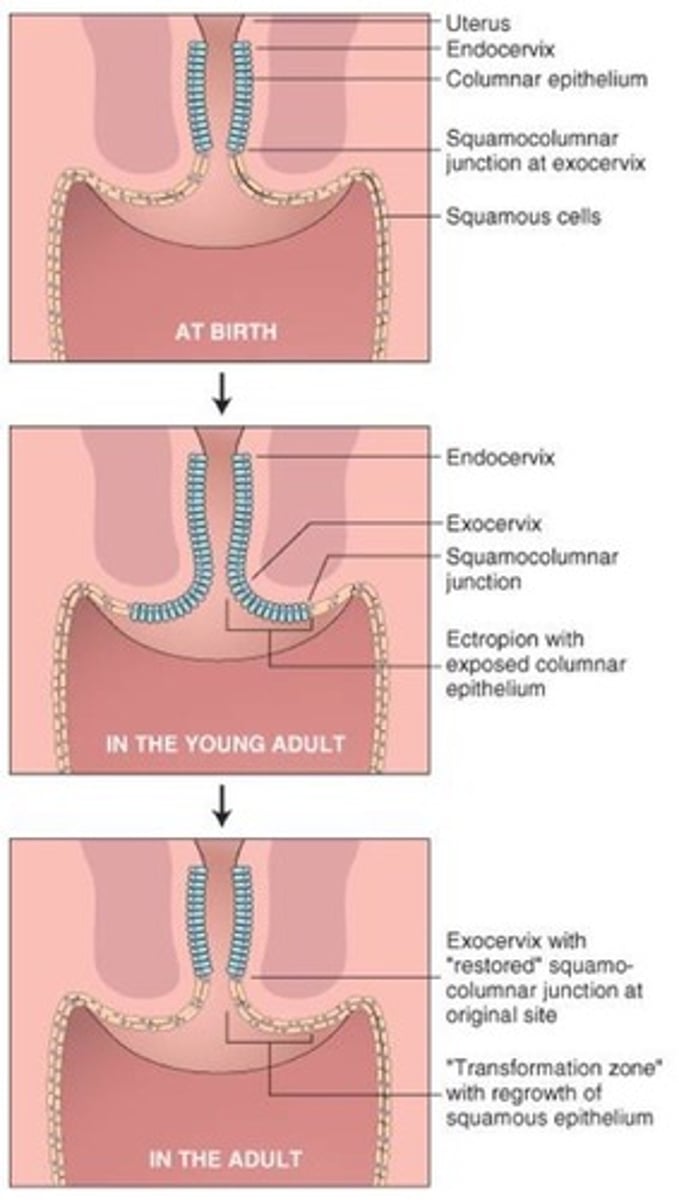
What is the transformation zone?
Area near the ectocervix where columnar cells undergo metaplasia / become squamous
Can pregnant women still get colposcopy?
YES! This is safe to have during pregnancy
Screening of cervical cancer?
21-29: Q3Y
30-65: Q5Y with co-testing/Acceptable—Pap test alone every 3 years
What are the two MC high-risk HPV types that are associated with high-grade lesions of the cervix and cervical cancer?
16 and 18
Pregnant women with cervical cytology showing ASC-H should be evaluated with what?
Colposcopy during pregnancy
What increases the risk for cervical cancer?
Multiple sex partners
3 multiple choice options
Most early cervical cancers are asymptomatic, but when symptoms occur, the most common are?
Heavy or irregular vaginal bleeding and postcoital bleeding
MC cervical cytology abnormality?
Atypical squamous cells of undetermined significance (ASC-US)
For young women (25-29 year olds) with ASC-US cytology, the next step is _____.
HPV testing. If this comes back positive, patient needs colposcopy
The pathologic cellular changes w/ cervical dysplasia most commonly occur at the cervical ______ , an anatomic landmark where the ______ epithelium of the endocervix transitions to the ______ epithelium of the ectocervix.
Transformation zone
Columnar
Squamous
White, sharply demarcated lesion of the cervix after acetic acid is applied during colposcopy?
Think cervical dysplasia
45 year old female with post coital bleeding and painful intercourse
Cervical Cancer
The mother of a 12 year old female patient is inquiring about HPV vaccine? Is her daughter eligible for the vaccine?
Yes. Ages 9-45 are eligible for vaccine
● May be initiated at 9 years old recommended for all children 11-12 y/o
● Catch up for all persons 13-26 years who were not previously vaccinated regardless of risk factors
● Shared clinical decision making for some adults aged 27-45 who are not adequately vaccinated
HPV vaccine dosing schedule?
● < 15 years old: administer a two- rather than a three-dose vaccine series. In such patients, the two doses are administered at least six months apart
● ≥ 15 years old: the HPV vaccine is administered in three doses at 0, at 1 to 2 months, and at 6 months
What is the most likely disorder in a bleeding pregnant patient with an extremely elevated beta HCG?
Gestational Trophoblastic Disease
Premature separation of the placenta from the uterine wall?
Abruptio placentae
Surgical incision of the abdominal wall and uterus to deliver a fetus
Cesarean section (C-section)
Failure of cervical dilation and fetal descent (difficult labor)
Dystocia
Rh incompatibility
If a mother is Rh- and the baby is Rh+, then the mother may develop antibodies against the infant's blood
What does a snow storm pattern on US likely represent?
Gestational Trophoblastic Disease
What is the most likely disorder in a bleeding pregnant patient with a suboptimal rise in beta HCG?
Abortion
What do a lecithin to sphingomyelin ratio > 2:1 and the presence of the pulmonary surfactant phosphatidylglycerol represent?
Fetal lung maturity
List 4 antihypertensive drugs used in pregnancy
Alpha-methyldopa - Hydralazine - beta blockers - Calcium channel blockers
Risk factors for shoulder dystocia?
Fetal Macrosomia - Diabetic mother - Maternal obesity - Postdate pregnancy
What is McRobert's Maneuver?
Used to manage shoulder dystocia during delivery of the infant. Maternal legs are removed from stirrups and sharply flexed upon the abdomen.
When is APGAR score assessed?
At 1 min and 5 min after birth (Normal score is 7-10 - Score of < 7 needs to be evaluated further)