* **History taking and physical examination** embodies the time-honored skills of healing and patient care and is the bedrock of clinical medicine * **Challenges of integrating the essential elements of clinical care** are emphatic listening, ability to interview patients of all ages, moods and backgrounds, techniques for examining different body systems, levels of illness, process of clinical reasoning and diagnostic plan * ==Health history== is a structured framework for organizing patient information in a written or verbal form. * ==Health history== also focuses the clinician’s attention on a specific pieces of information that must be obtained from the patient. * The ==interviewing process== generated the pieces of information in a fluid manner. * ==History taking== is a ==planned professional conversation== between the doctor and the patient. * History taking enables the patient to communicate to the doctor of the symptoms, feelings, fears * History taking obtains an insight into the nature of patient’s illness and his attitude towards them * The ultimate goal of history taking is to facilitate the basis for diagnosis and therefore appropriate diagnostic work-ups and therapeutic options. * Interviewing skills: the doctor should practice effective listening, he/she should be aware of nonverbal clues and body language, should have a broad knowledge base and should summarize to form a general picture. * **Patient-centered approach-** encourage and facilitate patients to participate and always use an open ended questions * Successful interviewing is dependent upon excellent communication skills * How to establish patient-physician relationship? * Demonstrate genuineness and honesty, * explain and tell the patient what you will do, * empathize and demonstrate a real concern, * accept the patient’s views and feelings * accept your own limitation, * demonstrate and maintain respect * value the patient as an individual * be non judgmental * honor the patient’s rights * maintain privacy * address the patient appropriately * ensure patient’s comfort at all times * no ridicule/arrogance/derogatory or demeaning remarks * be clean, neat and conservative * wear the complete inform and nameplate * no sexual innuendos or advancements * maintain professionalism and decorum at all times * don’t use authority to coerce the patient * turn your phones on silent mode * avoid texting or answering your phone * capacity to identify with the patient * maintain eye contact with your patient * listen intently to the patient * observe silence and let the patient talk * Fundamentals of Skilled Interviewing: * active listening * empathic responses * guided questioning * nonverbal communication * validation * reassurance * partnering * summarization * transitions * empowering the patients * Preparation before the interview * reviewing the clinical record * setting goals for the interview * reviewing your clinical behavior and appearance * Sequence of the interview * greeting the patient and establishing rapport * taking notes * establishing the agenda for the interview * inviting the patient’s story * identifying and responding to emotional cues * expanding and clarifying the patient’s story * generating and testing diagnostic hypotheses * sharing the treatment plan closing the interview and the visit * taking time for self-reflection * Cultural context of the interview * demonstrating cultural humility- a changing paradigm * Components of History Taking * Opening portion * greetings * shake hands if appropriate * introduction of yourself * ensure privacy, keep the doors/curtains closed * get informed consent * speak with respect * put the patient at peace, avoid distractions * express the duration of the history and PE * sit down next to the patient * remove any physical barriers (bedside rails) * complete focus on your patient * maintain a positive atmosphere * explain the need to take notes and its confidentiality * take notes as sparingly as possible * Information gathering power * encourage to the patient to tell his/her story * begin with an open ended questions and use concise, easy to understand, avoid jargons for example “tell me about your problem or how can I help” * establish a narrative thread: no interruption, establish dates, logical sequence of events, follow significant leads * expound on the problem/s, ask and verify problem appropriately for example, “Let me see if I got you correctly…” * be alert and responsive to verbal and nonverbal cues * look for facial expression and speech, etc. * encourage patient to be relevant for example, “let us go back to what you said about your abdominal pain” * after sufficient data, ask close-ended question like, “did you fall when you felt dizzy?” * progress for one section to another using transitional statements like, “let us now move to past medical history” * Closing or concluding power * summarize * ask if they would like to add anything * encourage patients to ask questions * thank the patient and state appreciation for the patient’s efforts and cooperation * Dealing with your own discomfort (during the interview) * uncomfortable scenario * the process is very intrusive * asking intimate questions of a person * violating patient’s space- overstepping boundaries * peering in the life (privacy/ dignity) of a completely stranger * Primary history * personal/ general data * NASEOMADR * reliability (of the source of information) * reflects the quality of the information provided by the patient, family member, relatives and etc. * made at the beginning/ end of the interview * usually in (%) * chief complaint * a.k.a chief concern, present complaint, reason for admission/ consultation/ presenting, problem on admission, presenting problem * provides the reason or concern for which the patient sought consultation * it is a Sign or a Symptom * or may be due to an abnormal lab results, continuation of treatment, executive check-up * example: “Tell me what brings you here today” * record the answer verbatim in quotation marks * may use medical terms after clarifications * guide to a focused medical history and hopefully a logical initial diagnosis and diff. diagnosis * manner of asking: USE OPEN ENDED QUESTIONS * history of present illness (HPI) * main part of the medical history * primary history that recounts the events of patient’s main problem * identifies the organ involved or multiple organ systems * complete, clear, chronologic description of the patient’s problem * main goal is to develop a working diagnosis of the patient’s chief complaint * it is a series of follow-up questions designed to help the doctor for example: * when the patients was the last time * mode and cause of onsent * time of onset * when was the first s/s noticed * progression- was it continuous or intermittent * was it aggravating or relieving * what were the treatments taken * Manner of writing HPI * state a chronological order of event from previously well or worsening, for example, 1 year PTA, 2 months PTA, 1 month PTA, 1 week PTA, 2 days PTA * characterize symptoms using mnemonics: * OLD CARTS- * onset, * location, * duration, * character, * aggravating/alleviating factors, * region/radiation, * time, * severity scale (1-10) * OPQRTS- * onset, * precipitating/palliative factors for example “What makes the pain better/worse?” * quality for example, “Describe the pain” * radiation/region for example, “Where is the pain?” * severity of symptoms for example, “How does the pain compare with other pain you experienced?” * temporal/timing for example, “Does the intensity of the pain change with time” * include associated active medical, surgical/psychiatric problems which may have an impact on the CC for example, “diabetic and hypertensive” * include past experience with symptoms for example, prior treatment, medication given, data from past charts * use universal pain assessment tool * 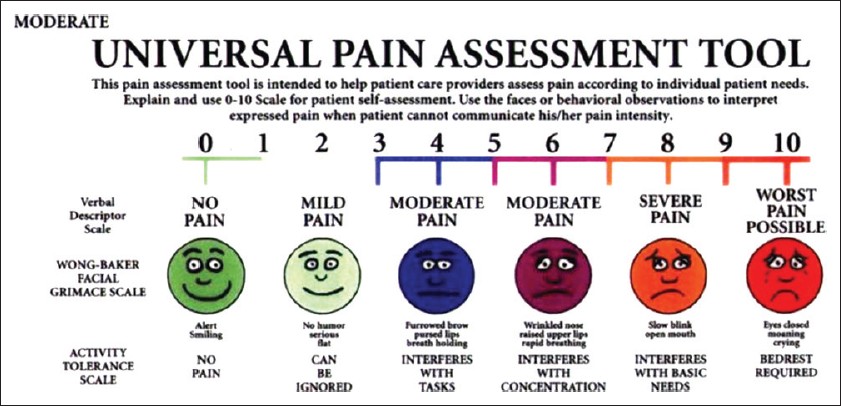
Updated 1158d ago