Salivary Glands
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
What is meal time syndrome and what are its 2 causes?
It is the acute intermittent swelling of the gland after food stimulus.
It is caused via blockages to the salivary gland ducts causes by sialolithiasis or strictures of the duct.
What could be causing acute generalised swelling with no obvious trigger? (2)
An infection of the Salivary Glands either bacteria (sialadenitis) or viral (mumps).
What are 2 possible causes of chronic generalised swelling of the Salivary glands?
1. sialosis - this is the fat infiltrate within the gland which has no obvious cause
2. sjorgens syndorme (either primary or secondary)
What could be the 4 possible causes of a discrete lump swelling? (think local causes of swellings)
1. neoplasm - benign or malignant
2. cyst
3. intraparotid lymph node lymphoadenopathy
4. jugular digastric lymph node lymphadenopathy (just posterior to the submandibular gland)
What are 5 possible causes of dry mouth?
1. sjogrens syndrome
2. post radiation damage
3. dehydration
4. medication related
5. anxiety
What is the ideal radiograph to take to view the submandibular gland?
90 degree true occlusal of the mandible - allows you to see the FOM and SM duct openings
LOWER STANDARD OCCLUSAL
What are the 3 radiograph techniques to view parotid gland pathology?
1. anteroposterior view of the parotid with the cheeks puffed out (to move the teeth out the way so can see other calcifications)
2. intraoral views on parotid (only shows sialoliths if the stone is anterior to masseter and buccinators)
3. OPG - calculi can be seen superimposed over the ramus and body of mandible if within parotid gland
What are the 2 advantages to taking radiographs of salivary gland pathology?
1. they are cheap/ quick/easy
2. it is good for acute inflammations when sialography is contradicted.
What are the 3 disadvantages to taking radiographs of SG pathology?
1. only 60-80% of sialoliths are radiopaque
2. often superimposed over calcified bone
3. other soft tissue calcifications may be confused for sialoliths
What is the gold standard imaging technique for Salivary Gland pathology?
Ultrasound.
What are the 3 advantages to taking ultrasounds of Salivary Gland pathology?
1. non-ionising
2. non-invasive
3. allows for differentiation between lumps nodes, cysts and neoplasms
What are the 2 disadvantages to taking ultrasounds of Salivary Glands pathology?
1. it is operator dependant
2. it is hard to assess the deep parotid gland
What is sialography?
It is the injection of a radioactive isotope into the salivary gland
This is then assessed via radiographs to assess the passage of salivary flow for any blockages etc.
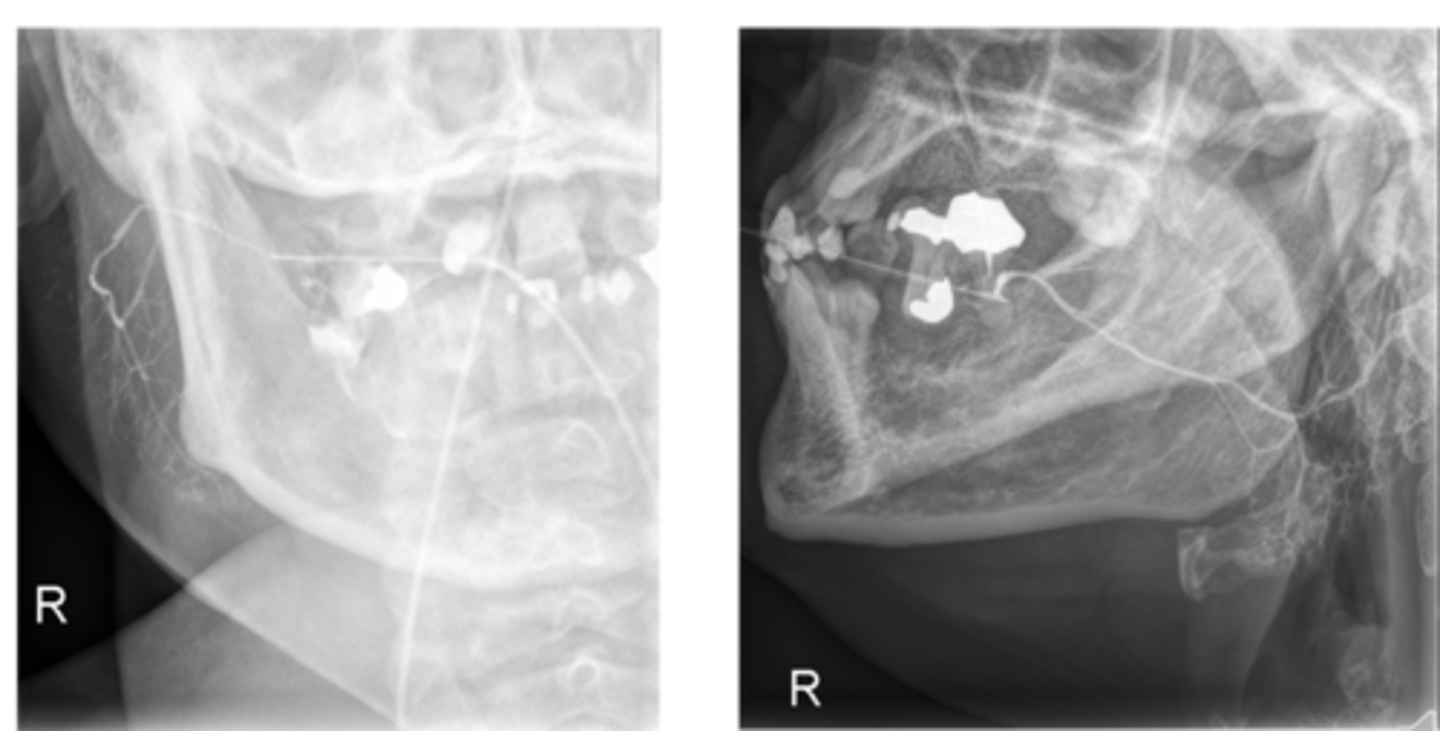
What are the 4 advantages to taking sialographs of Salivary Gland pathology?
1. good for assessing ductal abnormalities/blockages
2. can be used with digital subtraction radiology (takes out irrelevant continuous background features)
3. assesses ductal function
4. assess calculi or stone mobility - as the pressure of the dye used may move the stone so can assess if it can be flushed out etc
What are the 5 disadvantages to taking sialographs of Salivary Gland pathology?
1. contraindicated in acute infection and those with iodine allergy
2. there Is a radiation exposure to both the isotope and radiograph
3. operator dependant
4. if pressure too great can displace the stone posteriorly cause iatrogenic damage
5. can exacerbate pre existing infection
Aside from the main 3 imaging techniques used on SG (Ultra sound, radiographs, sialography) what other 4 imaging techniques can be used?
1. scintigraphy
2. MRI sialography
3. CT scanning - useful for acute spreading infection
4. sialoendoscopy
What are the 4 possible treatments for Sialoliths?
1. symptom management - chronic SS sufferers or sialosis need tom are sure they aren't dehydrated and having saliva sprays to counteract xerostomia
2. basket collection of calculi/stones
3. balloon dilation of strictures
4. lithotripsy of the calculi
What are 3 features of calculi formation (sialoliths)?
1. can be mobile within the duct or tethered. (if over 5mm likely to be tethered)
2. can be palpate in the floor of the mouth
3. patients at greater risk of bacterial infection
What is meant by primary vs secondary sjogrens?
Primary- is when the patient suffers only with sjorgens syndorme
Secondary- is when the patient suffers with sjogrens but also another autoimmune conditions eg lupus or RA
What malignancy does Sjogrens Syndrome have an association with?
MALT- mucosa associated lymphoid tissue lymphoma
What antibodies do you test for when diagnosing SS?
What test can you do to check lacrimal gland function?
Check for SSA or SSB antibodies.
Can conduct the schirmer test to test lacrimal function
What imaging technique is used for Sjogrens syndrome?
Ultrasound is the gold standard.- it can be used to visualise glandular enlargement as well as areas of fibrosis and atrophy it can also be used to screen for MALT lymphoma.
What is a mucocele?
It is a cyst resulting from damage to a minor salivary gland resulting in saliva pooling.
What are the 3 different types of mucoceles?
1. extravasation
2. retention
3. ranula
What is an extravasation mucocele?
A mucocele which forms when there is trauma which causes the entire duct to rupture resulting in a collection of saliva in connective tissue.
What is a retention mucocele?
Often seen in older patients, it is when the gland is blocked causing a swelling of saliva in the tissues but no break in epithelium.
What is a ranula mucocele?
It is a mucocele arriving from the lingual gland. It can either be oral or plunging.
What is the difference between oral and plunging ranula mucocele?
If it is plunging it will penetrate through the deep extrinsic muscles and if oral will maintain in the Floor of the mouth.
What are 4 features of a pleomorphic adenoma?
1. it is the most common benign parotid tumour
2. it consists of mixed cells (epithelial, myoepithelial and stromal)
3. it can have small satellite tumours which means if not fully excised can reoccur
4. can undergo malignant transformation to for a carcinoma ex-pleomorphic adenoma
Who and where does warthins tumour tend to present in?
It tends to present in elderly males at the parotid tail (part of the parotid which sits between the notch of the mandible and the ear lobe.
What are the risk factors for Warthins tumour? (3)
1. smokers
2. EBV sufferers
3. Those exposed to radiation
What are 4 features of a mucoepidermoid carcinoma?
1. it is a large slowly enlarging malignant mass
2. commonly occurs in the parotid gland (most common parotid malignancy) but can occur elsewhere
3. has a close association with the facial nerve so need to check for perineurial sperad
4. can be low or high grade on a case by case basis
What is an adenoid cyst tumour?
A malignant tumour which presents in both the parotid and submandibular glands.
Who does adenoid cyst present in and how does it present?
It tends to present with pain in 40-70 year olds.
Why do adenoid cysts pose an issue to treatment?
It has a predisposition for late local recurrence.
What is an acinic cell carcinoma and what is it associated with? (2)
It is a malign tumour which is a variant of an adenocarcinoma but the main cells present are acinar cells (saliva producing). It is associated with prior radiation exposure and family history.
What can acinic cell carcinoma result in? (3)
1. facial paralysis
2. may reoccur locally
3. may metastasise to the lungs/ bone
How does a secondary tumour in the intra parotid lymph nodes present?
Presents as a hard fixed lump in the parotid gland.
What are the 2 warning signs which indicate that there may be a secondary tumour present?
Should be v aware if the patient has a history of head and neck cancer and if the patient has scars on scalp or forehead from previous surgery.
What type of cancer does a secondary tumour in the intra parotid lymph nodes usually spread from?
From a squamous cell carcinoma of the scalp.