BIOL 2044 - Skin infections and dwelling diseases
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
15 Terms
primary and secondary infections
primary site of infection - mouth, catheters, implanted medical devices
secondary infections - brain, kidneys, intermembranal spaces, bones, around implanted device
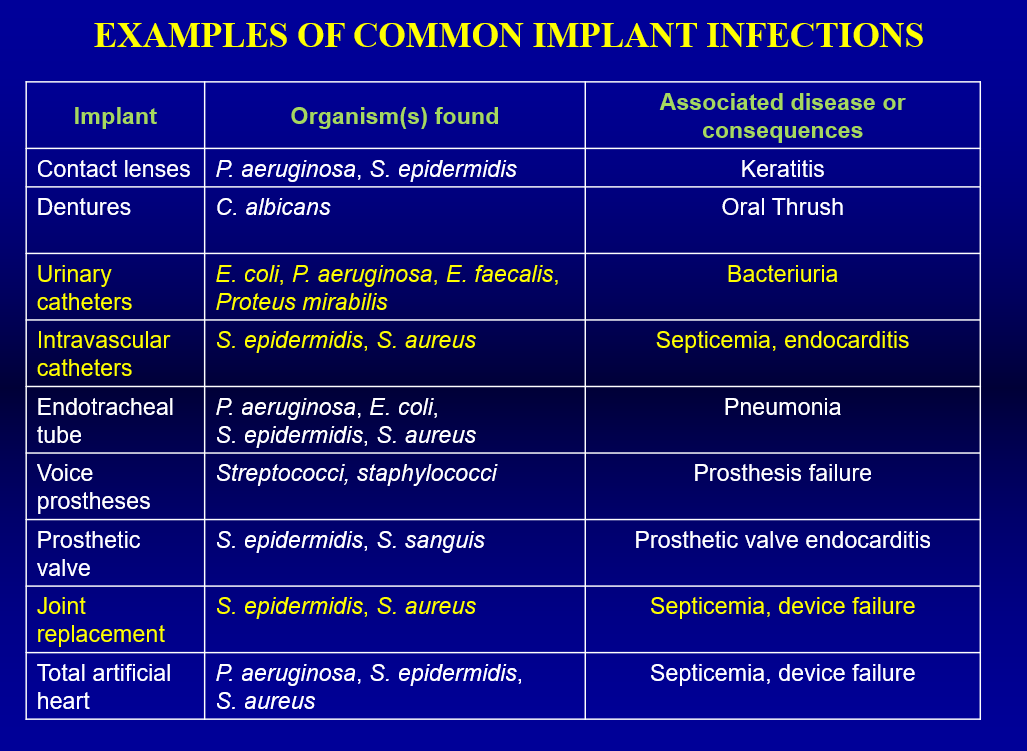
examples of common implant infections
normal skin flora
sebaceous gland secretes a lubricant fluid (rich in microbial nutrients: lactic acid, AAs, salt, lipids)
pH of human secretion 4-6
variety of aerobic/anaerobic bacteria, yeast, filamentous fungi
normal flora either transeints/residents
most transients die shortly
residents are long term and multiply
most skin infections are S. Aureus, S. pyogenes, P. auruginosa
immune cells are present around hair follicles to control whats going on
primary bacteria recovereed are mainly gr+ve bact S. epidermidis, S. mitis, Micrococcus sp.
aerobic/anaerobic corynobaceria imbalance causing secretion of subaceous glad causing acne in hormonal imbalance
gr-ve bacteria are a minor consituent, only long term resident detected Acinetobacter Johnsonii
thought that gr-ve ouldnt compete well with gr+ve —> is the latter is eliminated then gr-ve might thrive
skin microbiome
each area has its own community
1000 species from 19 phyla
10m2 of skin
major constituents from culture only male up a small constitution of flora
were now detecting more gr-ves - proteobacteria 1.7%, bacteriodetes 6%
P. aeruginosa thought to be a pathogen but can be mutualistic as it secretes an antibiotic which inhibits staph/strep tRNA sythetases
areas around the body
SEBACEOUS (hair/chest)
mainly propoinibacteria and staph species
greater species richness and more nutreints
MOIST AREAS
crynobacteria and staphylococci
DRY AREAS
mixture but beta proteobacteria and flabobacteria dominate
CHRONIC WOUND
polymicrobial biofilm - many bacteria present
hip infections
pain/arthristis lead to hip replacements
0.6% deep infections despite surgical procedures
cause: pain, prolonged immobilisation, lifetime antibiotic treatment due to persistant biofilm
treated by surgical revision —. replace joint and clean the area
one stage - 30% replaced
two stage - 60% replaced
even surgical revision causes a 10% reinfection
how do we know about reinfections?
18F fluoro-deoxyglucose positron emission tomography
activated inflammatory cells accumulate FDG
biofilm infections in knee replacements/hip can cause secondary infection
vascular catheter
eneters directly in to venus system
when infected erythema and discharge omon at the exit site
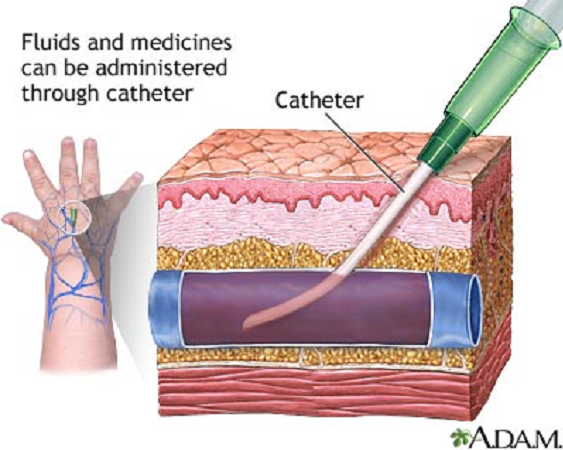
catheres major cause of UTI
difficult to keep sterile
biofilms can have translocation - urine in catheter flows down but we usually see ascending infections as the bacteria move against flow
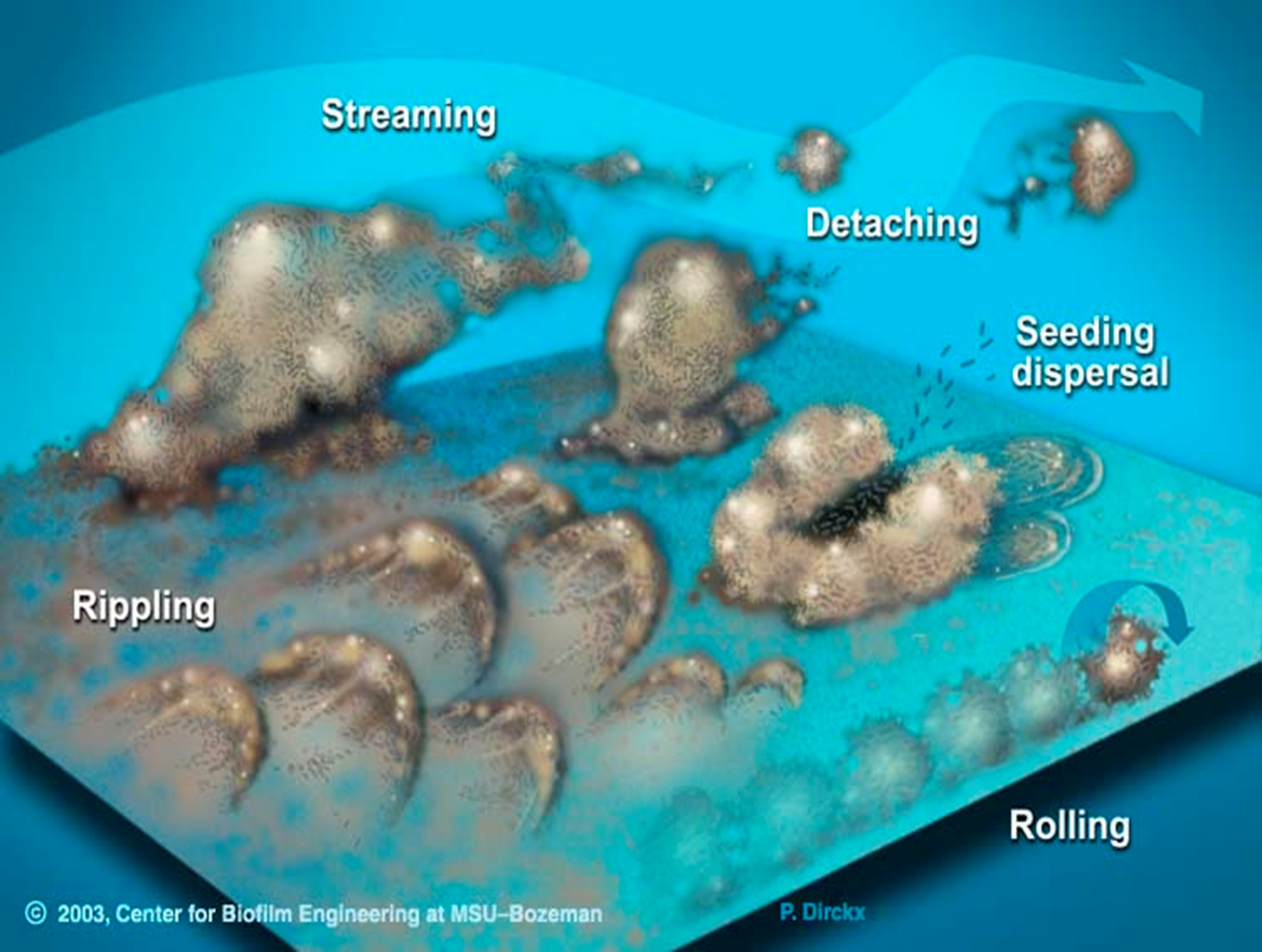
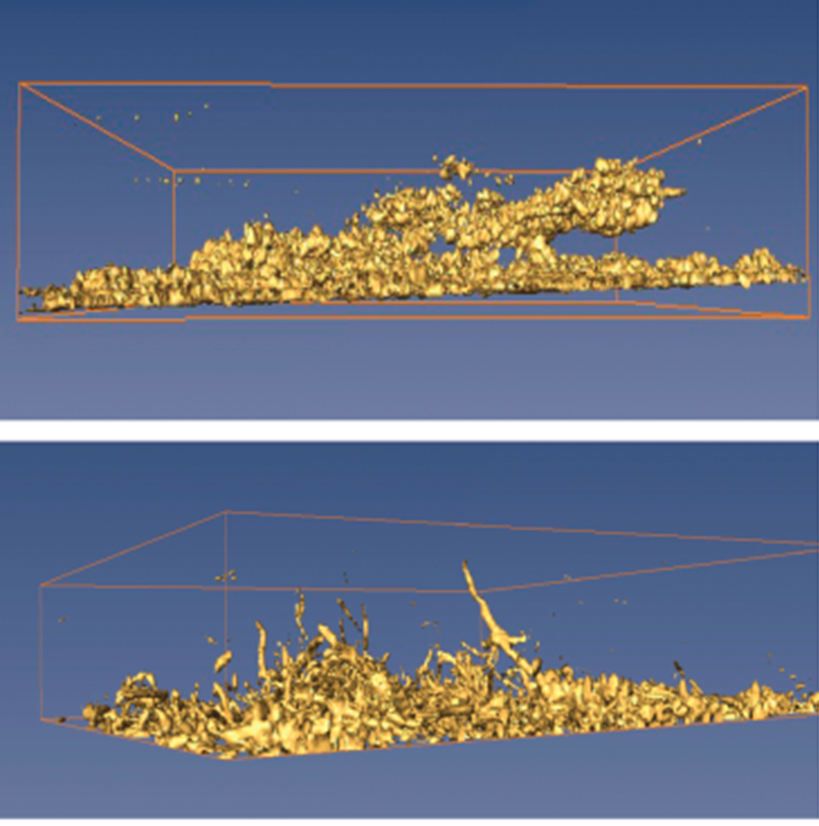
can have rippling, rolling, streaming of biofilm (streaming is where long streams form and detach)
blockage of catheters
some catheter infections cause blockage of the catheter —> requires fast treatment as theres nowhere for the urine to go
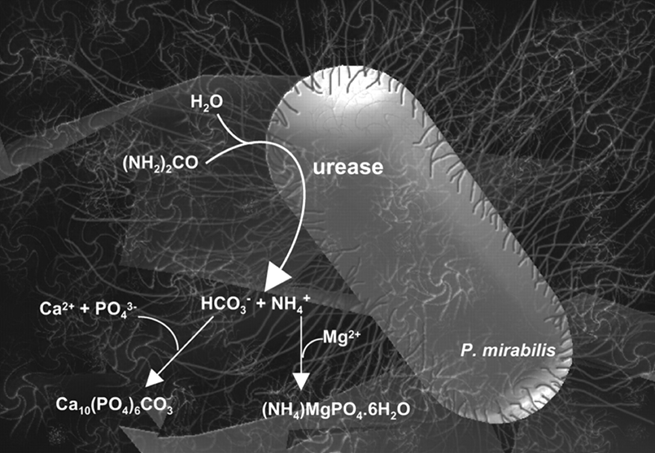
crystalline structure deposits (magnesium ammonium phosphate) and a poorly crystalline form of apatite (hydroxylated calcium phosphate)
bacteria on top of the crystals guide the formation of crystals
bacteria then colonise the crystals —> caused by proteus morabilis
highly motile and covered in flagella
has urease enzyme which allows it to hydrolyse urea and increase urinary pH
as urine becomes alkaline magnesium and calcium phosphate crystals are precipitated which blocks the flow of urine
the urea is then broken down into ammonia and hydrogen carbonate ion:
hydrogen carbonate ion and the calium phosphate combine whilst the ammonia combines with the magnesium
effects of crystal formation
struvate can damage glycosaminoglycan layer of epithelium which protects the urothelial surface against infection
P. mirabilis can cause reccurent infection - blockage of new catheter
ascending reflux - ascends to kidneys causing pyelonephritis —> sepsisemia, endotoxic shock
crystalline aggregates can form stones in the bladder which are resistant to antibiotics
strategies for treatment: lower urine pH with cranberry juice, increase fluid uptake, surgically remove bladder stones
can also cause urinary stones which penetrate down into the urinary epithelium
variations of catheters
can we coat in antimicrobial materials
no - silver cathters not effective
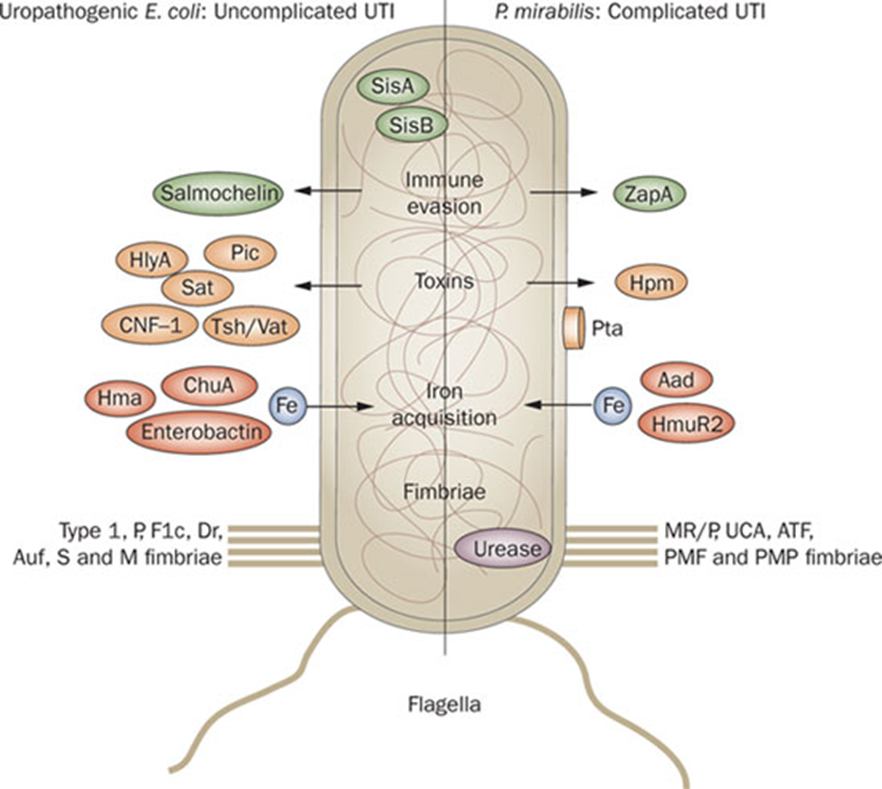
virulence factors of UTI
E. coli causing uncomplicated UTIS
P. mirabilis causing complicated UTIS
both have fimbrae and pilli to help adhere to the surface
produce toxins such as HlyA, Pic, Sat (E. coli) and Hpm (P. mirabilis)
growth environment
latex catheters - not smooth, lots of niches
in standard LB broth forms large collection of microcolonies whereas in urine forms swarm cells —> flagell start to swarm and form much longer finger like appendages
if the E. coli have been able to form stones the leukocytes are unable to bind and engulf bacteria
stones form pods and coat in europlakin
inside a polysaccharide strain used lost of polysaccharides by the interior surface
E. coli right in the centre
coinfection
gerdenella vaginalis found in vaginal flora but may get into urinary tract
debrines surface of urinary tract and exposes the surface to UTI
a lot more E. coli infection when polymicrobial —> this suggests that E. coli does better when it’s a coinfection