Male Repro and Embryogenesis/Repro System Development - Lectures 4/5
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
114 Terms
Testis function
Site of gamete/hormone production
Testis structure
Tunica albuginea
Seminiferous tubules/testis parenchyma
Interstitium
Tunica Albuginea
Testicular capsule
Testis parenchyma
Tissue made up of seminiferous tubules that house developing gametes
Sertoli and germ cells
Interstitium
Space between seminiferous tubules
Location of leydig cells
Order of structures in tubules (interstitial side to lumen side)
Peritubular myoid cells
Mitotic germ cells
Meiotic germ cells
Post meiotic germ cells
Sertoli cells surround everything
What are the 3 things a mammalian gamete needs?
Immune privilege
Correct hormone signaling
Temperature homeostasis
Lack of immune privilege effects
Loss of meiotic and post-meiotic germ cells
Mitotic cells are unaffected - the body still considers them "you" as they are diploid
Fertility is recoverable - mitotic cells still there
Blood Testis Barrier (BTB) parts
Basal compartment
Adluminal compartment (primary part)
Basal compartment of BTB
First barrier against immune system
Peritubular myoid cells
Partially protected - also location of mitotic germ cells
Adluminal compartment of BTB
Created by sertoli cells closing
Covers everything after the mitotic germ cells
Fully protected
How can the BTB be tested?
If the BTB is intact, dye will only be on the outside of tubules
If not, you can see the dye permeate the tubules
Sertoli cells
"nurse cells"
Somatic cells that surround the germ cells
Secrete AMH
Effect of loss of hormone signaling in gamete production
Loss of post-meiotic germ cells
Fertility is recoverable - mitotic cells intact
Lack of androgens (testosterone)
Leydig cells
Produce testosterone
Most stays in testicles, but some is spread by capillaries
Induced by LH
Structures in interstitium (outer to inner)
Peritubular myoid cells
Macrophages blocked by BTB
Leydig cells
Capillary (spreads T through body)
Temperature homeostasis effects of fertility
Loss of all germ cells
Causes complete infertility - unrecoverable
How do testis stay cool
Temperature needs to be steady and cool relative to body
Scrotal sack is covered in sweat glands
Pampiniform plexus
Spermatic cord function
Connects testis to body
Cremaster muscle
In spermatic cord
Ligament that connects testis to body
Spermatic cord structures
Cremaster muscle
Testicular artery
Ductus deferens
Pampiniform plexus
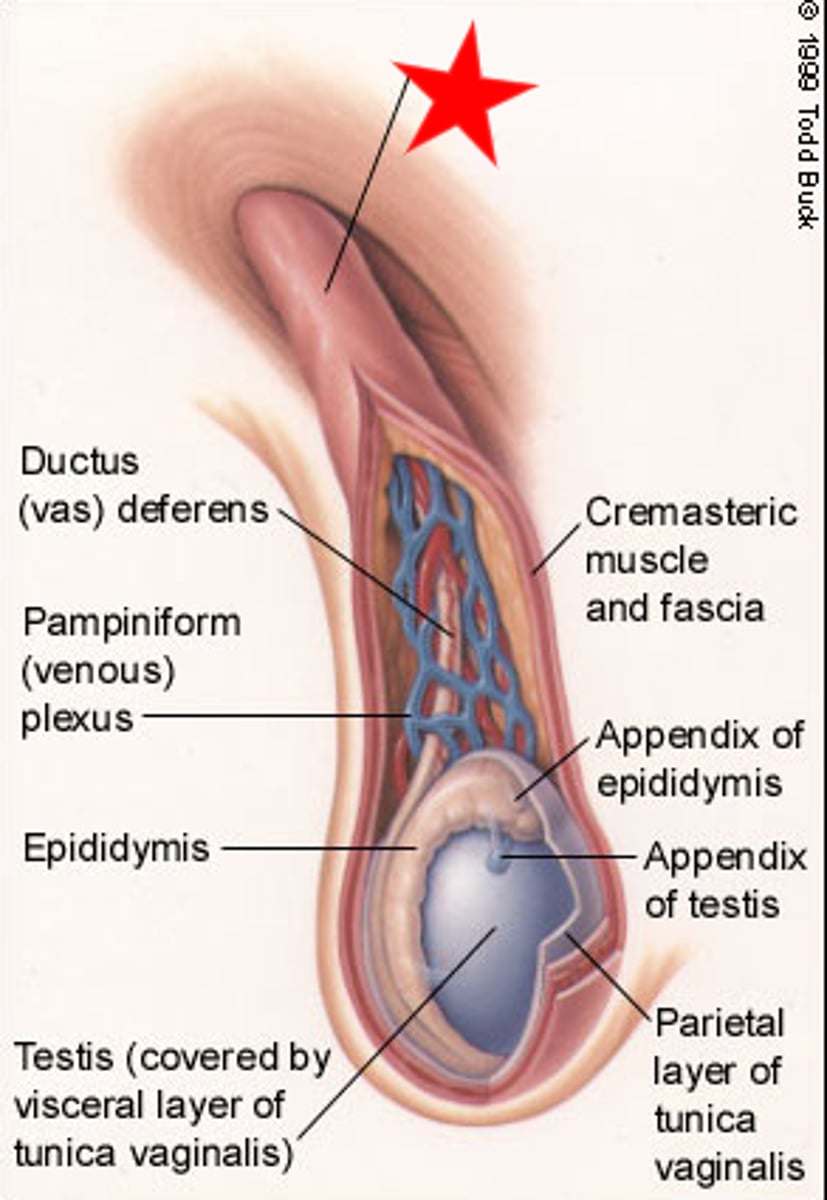
Pampiniform plexus
Series of veins/arteries to/from scrotal sack
Veins/arteries are intertwined for heat transfer - hot blood from arteries cools itself by heating blood from veins
Allows for temperature homeostasis
Also helps distribute T through body
Primary functions of testis/testis support tissues
Gamete production
Hormone production
Excurrent ducts structures
Efferent ducts
Epididymis
Ductus deferens
Efferent ducts function
Deliver sperm to epididymis
Kinds of cells in efferent ducts
Mixed epithelium -
Smooth muscle & ciliated cells move spermatozoa
Short cells concentrate spermatozoa through water reabsorption
Epididymis function
Moving, modifying, and storing mature gametes
Epididymis structure
Single long tubule that goes back and forth
Multiple segments with different cell types to generate different environments
Surrounded by smooth muscle to help move sperm
Segments of epididymis (from efferent duct to ductus deferens)
Caput
Corpus
Cauda
Caput
Beginning of epididymis
Removal of abnormal spermatozoa
Membrane modification
Corpus
Middle section of epididymis
Sperm gain motility (ability to move on their own) as mitochondria form near tail
Cauda
End of the epididymis
Sperm gain fertilization (capacitation) ability
Long term storage
Primary site for sperm reserves
Ductus deferens function
Moving gametes
(from caudal epididymis to accessory sex glands)
Gamete maturation/delivery, seminal fluid production/delivery
Ductus deferens structure
Narrow epithelium surrounded by smooth muscle
Accessory sex glands function
Generate seminal plasma
Accessory sex glands parts
Ampulla
Vesicular gland
Prostate gland
Bulbourethral gland
Male repro - Ampulla
Widening of vas deferens
Continuation
Male repro - Ampulla cell types
Smooth muscle (moves sperm/fluid from vas to urethra)
Mucosa lining (secretes seminal fluid)
Male repro - Vesicular glands (seminal vesicles)
Similar morphology to ampulla but not contiguous (continuous/connected) to vas deferens
Vesicular glands function
Generate/store seminal fluid (majority of ejaculate)
Vesicular glands cell types
Smooth muscle
Mucosa - high surface area to produce seminal fluid
Prostate
Species specific morphology
Generates prostate fluid
Protects sperm after ejaculation
Prostate specific antigen (PSA)
Very hormone sensitive - imbalance can cause it to grow
Prostate specific antigen (PSA)
Reduces semen viscosity
Bulbourethral gland
Species specific morphology
Accessory sex gland functions
Seminal fluid production and delivery
Excretory tissues function
Gamete delivery
Seminal fluid production and delivery
Excretory tissues structure
Penis and urethra
Male repro - urethra
Contractile muscle around a duct designed for delivery
Penis
Highly evolved system with lots of variation
What part of the male reproductive tract is responsible for gamete and hormone production?
Testis
What part of the male reproductive tract is responsible for gamete maturation?
Excurrent ducts (efferent ducts, epididymis, vas deferens)
What part of the male reproductive tract is responsible for gamete delivery?
Excurrent ducts (efferent ducts, epididymis, vas deferens)
Excretory tissues (penis/urethra)
What part of the male reproductive tract is responsible for seminal fluid production and delivery?
Everything but testis -
Excurrent ducts (efferent ducts, epididymis, vas deferens)
Accessory sex glands
Excretory tissues (penis/urethra)
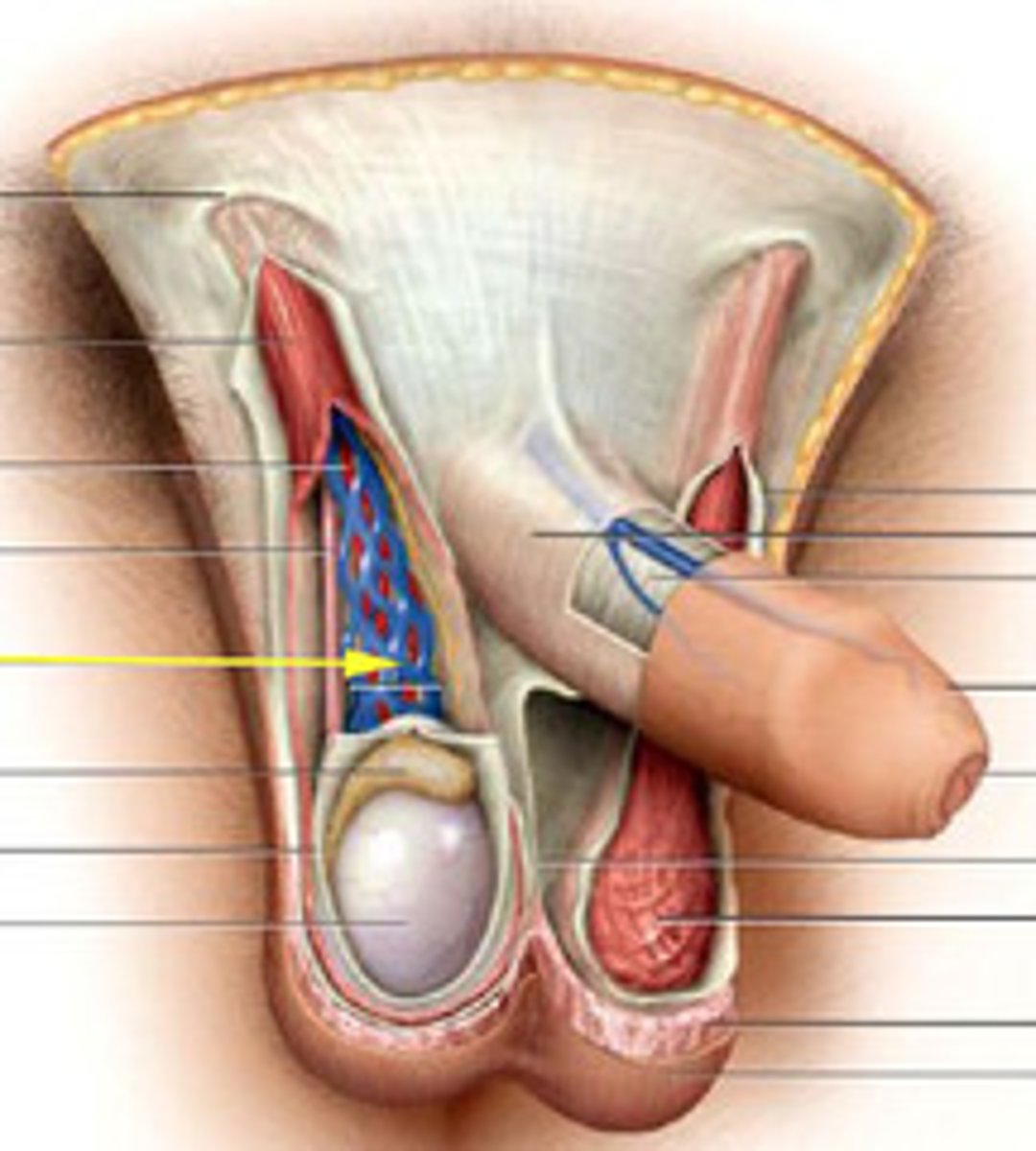
Target tissue for sterilization in men
Ductus deferens
2.4% worldwide
Cause of sterility in men with cystic fibrosis
Ductus deferens
Mammalian fertilization
Combines chromosomes of egg and sperm
Inherited sex chromosomes typically determine gonadal/genetic sex
Parents are diploid XX or diploid XY
Egg = haploid X
Sperm = haploid X or Y
Why is sex considered a mosaic of traits?
It is dependent on a number of factors and is not binary
Factors include:
Hormones
Genotypes
Phenotypes
Secondary sex characteristics
Internal/external genitalia
Difference between the X and Y chromosomes
X is ~3x larger
Y has the SRY gene
SRY gene
Sex determining region of the Y chromosome
Directs development of male phenotypes
Methods of sex determination
Genotypic sex determination
Temperature-dependent sex determination
Behavioral sex determination
Embryogenesis
Post fertilization process
Stages of an ovulated egg
Oocyte
Ootid (after fertilization, 2 separate nuclei)
Zygote (pro nuclei join together)
Two celled stage
Four celled stage
Eight celled stage
Morula
Early blastocyst (occurs once embryo leaves fallopian tubes)
Hatching blastocyst
Hatched blastocyst
Blastocyst
Fertilized egg divides until it is a blastocyst with 2 parts
Inner cell mass and trophoblast
Inner cell mass (ICM)
Part of the blastocyst that becomes the embryo
Trophoblast
Part of the blastocyst that becomes the placenta
ICM differentiation
During early embryogenesis the ICM differentiates to form the layers of the embryo
Ectoderm
Mesoderm
Endoderm
Ectoderm
"Outer skin"
Part of the ICM that differentiates into skin, hair, and nervous system.
Part of the reproductive tract - vagina & vestibule, penis & clitoris
Becomes hypothalamus and pituitary
Mesoderm
"Middle skin"
Forms a lot of the reproductive system - gonads, uterus cervix, vagina, epididymis, ductus deferens, accessory sex glands
Basically everything internal
Endoderm
"inside skin"
Part of the ICM
Doesn't differentiate into anything relevant to reproductive system (except endocrine system)
Hypophysis
Another word for pituitary
Produces LH/FSH which stimulates the testis/ovaries to produce testosterone and estrogen/progesterone
Neurohypophysis
Posterior hypophysis//pituitary
From neural tissue of brain floor
Stores/secretes Oxytocin and ADH (BUT DOES NOT SYNTHESIZE THEM! Hypothalamus makes them)
Ectodermal layer
Adenohypophysis
Anterior hypophysis/pituitary Derived from ectoderm in roof of embryonic mouth
Synthesizes and secretes LH, FSH, PRL, GH, TSH, ACTH
Mesodermal layer
Diverticulum
A sac/pouch diverting from a main tube/cavity
Infundibulum
Specific diverticulum from the brain that forms the posterior pituitary
Rathke's pouch
Specific diverticulum from the mouth that forms the anterior pituitary
Process of development of pituitary
Brain infundibulum bulges downward and Rathke's pouch bulges upwards to meet
Stalk of Rathke's pouch regresses, leaving it stranded with infundibulum
Rathke's pouch connects with the posterior lobe, posterior lobe hugs Rathke's pouch
Both lobes become surrounded with growing sphenoid bone (sella turcica)
Sella turcica
"Turkish saddle"
Saddle shaped depression in the sphenoid bone that protects the pituitary
Hypophysectomy
Removal of pituitary
Endoscope inserted through nose or upper lip
Done to treat cancer due to out of control hormones
Primordial Germ Cells (PGC)
Common origins of spermatozoa and oocytes (primordial follicles
PGC migration
PGC migrate from base of hindgut (near yolk sac) by ameboid movement
PGC seek out and colonize the genital/gonadal ridge (area along dorsal body wall)
Arrival of PGC initiates formation of bipotential gonads
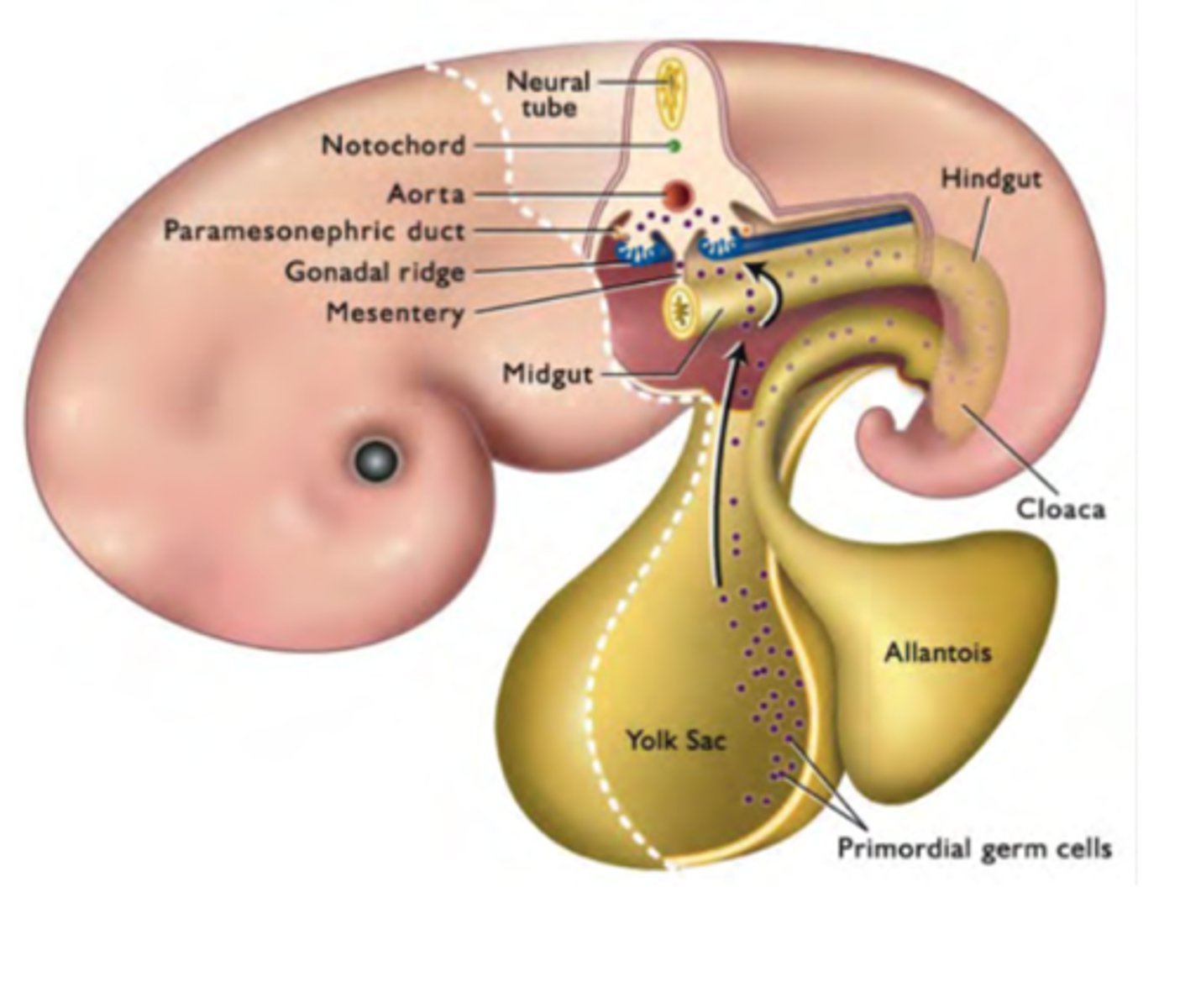
What do PGC do once they get to the gonadal ridge?
Divide and make more
Stimulate genital ridge growth, forming primitive sex cords that will become gonads (seminiferous tubules or cortex of ovary)
Close to kidneys
Bipotential gonads
Indeterminate preliminary gonads that have yet to differentiate towards ovaries/testis
How do PGC know where to go?
Chemical signals
Chemoattraction and repulsion create gradients that repel PGC from hindgut and attracts to gonadal ridge
Development of urogenital system
Mesonephros
Primitive kidneys
Metanephros
What eventually becomes the real kidneys
Mesonephric duct
Wolffian duct
Forms the male tract
Connected to metanephros and bipotential gonads
Paramesonephric duct
Mullerian duct
Forms the female tract
Anti mullerian hormone = mullerian duct regresses
Not connected to bipotential gonads - hovers over like infundibulum hover over ovaries
How is SRY created?
Synthesized by sex cords carrying a y chromosome
Starts being created once PGC arrive
Effect of SRY on reproductive development
Testes form in the presence of SRY
Ovaries form in the absence of SRY
How does SRY develop the male tract?
SRY causes testis development
Sertoli cells in the testis make AMH (anti mullerian hormone)
AMH prompts leydig cells to make testosterone
Testosterone and AMH cause the mullerian duct to degenerate, causing the male duct system to develop
What would happen if SRY was deleted?
Female reproductive tract would develop
Female tract with XY chromosomes
What would happen if SRY was added to an X chromosome in an XX individual?
Male reproductive tract would develop
Male tract with XX chromosomes
What would happen if someone was XY but had androgen receptor insensitivity
AMH is still generated causing degeneration of paramesonephric duct
External genitalia would not develop, causing a mismatch of external and internal gonads
Where do the testis develop?
Next to kidneys near ribs
Outside the peritoneal cavity
What are the phases of the descent of the testis
1. Trans-abdominal phase - growth of fetal body pushes testis against peritoneum
2. Inguinal-scrotal phase - rapid growth of gubernaculum
3. Gubernaculum regression - testes pass through inguinal canal
Gubernaculum
Ligamentous cord attached to bottom of testis
Trans abdominal phase of testis descent
Growth of fetal body pushes against testis
Testis are outside peritoneum and become enveloped
Dependent on INSL3
Inguinal-Scrotal Phase of testis descent
Rapid growth of gubernaculum mechanically pulls testis towards the inguinal canal
Gubernaculum Regression Phase of testis descent
The regression of the gubernaculum pulls testes through the inguinal canal
Peritoneum pinches off around testicular artery, basically surrounding it in its own tube of peritoneum