Chapter 24: Nursing Care of Newborns
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Chapter 24: Nursing Care of Newborns
Newborn care consists of stabilization and/or resuscitation. This can include establishing a patent airway, maintaining adequate oxygenation, and thermoregulation for the maintenance of body temperature. A physical assessment (physical examination, measurements, and monitoring laboratory studies) is done every 8 hr or as needed.
Nursing interventions and family teaching (umbilical cord care, prophylactic measures, newborn screening, newborn feedings and bathing, and fostering baby-friendly activities) are integrated into a newborn’s plan of care.
QEBP
Using the facility’s preferred pain assessment tool, conduct a pain assessment on the newborn with routine assessments and following painful procedures. Q
Newborn hearing screening is required in most states. Newborns are screened so that hearing impairments can be detected and treated early.
Provide family education and promote family-newborn attachment.
The newborn should be warmed slowly over a period of 2 to 4 hr. Correct hypoxia by administering oxygen. Correct acidosis and hypoglycemia.
QPCC
Decreased risk of penile cancer and cervical cancer in female partners (Circumcision)
QS
Identification (using two identifiers) is applied to the newborn immediately after birth by the nurse. It is an important safety measure to prevent the newborn from being given to the wrong parents, switched, or abducted.
Newborns sleep approximately 16 to 19 hr/day with periods of wakefulness gradually increasing. Newborns are positioned supine, “safe sleep,” to decrease the incidence of sudden unexpected infant death (SUID).
Newborn Physical Assessment
Vital signs should be checked frequently per facility protocol.
Daily weight should be measured at the same time using the same scale.
Umbilical cord should be inspected for bleeding and secured to prevent hemorrhage.
Observe periods of reactivity within the first 6 to 8 hours after birth:
First period of reactivity (first 30 min)
Newborn is alert, active, and makes sucking sounds.
Heart rate rises to 160-180 bpm, then stabilizes at 100-120 bpm.
Respiratory rate is elevated.
Period of relative inactivity (lasts 60 to 100 min)
Newborn becomes quiet, rests, and sleeps.
Heart rate and respirations slow down.
Second period of reactivity (2 to 8 hours after birth)
Newborn reawakens, becomes active again.
Gagging and choking on mucus may occur.
Can last from 10 minutes to several hours.
Conduct a pain assessment using the facility’s preferred pain assessment tool.
First period of reactivity (first 30 min after birth) (1 of 3)
Newborn is alert, active, and makes sucking sounds.
Heart rate rises to 160-180 bpm, then stabilizes at 100-120 bpm.
Respiratory rate is elevated.
Period of relative inactivity (lasts 60 to 100 min after birth) (2 of 3)
Newborn becomes quiet, rests, and sleeps.
Heart rate and respirations slow down.
Second period of reactivity (2 to 8 hours after birth) (3 of 3)
Newborn reawakens, becomes active again.
Gagging and choking on mucus may occur.
Can last from 10 minutes to several hours.
Newborn Laboratory Tests
Routine Tests
Hemoglobin (Hgb) and Hematocrit (Hct) if prescribed.
Blood glucose for hypoglycemia per facility policy.
Serum bilirubin before discharge.
Metabolic Screening
Mandatory newborn genetic screening via heel stick
24 hours after birth.
Must have had breast milk or formula for at least 24 hours for accurate results.
Repeat test in 1 to 2 weeks if discharged before 24 hours.
Phenylketonuria (PKU) screening is required in all states.
Additional tests may include galactosemia, cystic fibrosis, maple syrup urine disease, hypothyroidism, and sickle cell disease.
Blood Sample Collection
Perform heel stick using sterile gloves.
Warm the heel to improve circulation.
Clean with antiseptic and dry before incision.
Use spring-activated lancet for quick and painless incision.
Use outer aspect of the heel, with lancet depth no more than 2.4 mm to prevent bone injury.
Follow facility protocol for labeling and specimen collection.
Apply pressure with dry gauze (not alcohol) until bleeding stops, then cover with a bandage.
Provide comfort and reassurance after the procedure.
Newborn Circumcision
Surgical removal of the foreskin of the penis.
Parents decide based on health, hygiene, religion, culture, or social norms.
Timing:
Within the first few days but may be delayed for medical or cultural reasons.
Not performed immediately due to low vitamin K levels (risk of bleeding).
Health Benefits:
Improved hygiene.
Lower risk of sexually transmitted infections (STIs) like HIV and HPV.
Reduced risk of penile cancer and cervical cancer in female partners.
Newborn Circumcision Risks and Contraindications
Bleeding
Infection
Meatal stenosis (narrowing of the urinary opening)
Urethral fistula
Adhesions or dehiscence (skin separation)
Concealed penis
Hypospadias or epispadias (abnormal urethral positioning)
Family history of bleeding disorders
Newborns who have not received vitamin K (higher bleeding risk)
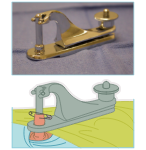
Circumcision Gomco Clamp (Image)
Preprocedure Care for Newborn Circumcision
Check for:
Bleeding disorders (family history of hemophilia or clotting disorders)
Hypospadias or epispadias (abnormal urethral positioning)
Ambiguous genitalia (unclear male or female characteristics)
Signs of illness or infection
Nursing Actions
Obtain signed informed consent from parents.
Prepare supplies and administer prescribed medications.
Assist during procedure:
Secure newborn on the restraining board and use a radiant heat source to prevent cold stress.
Keep a bulb syringe available for suctioning if needed.
Comfort the newborn as required.
Document procedure details, including:
Time and type of circumcision
Amount of bleeding
Voiding status post-procedure
Intraprocedure Care for Newborn Circumcision
Anesthesia
Types used:
Ring block
Dorsal-penile nerve block
Topical anesthetic (eutectic mixture of local anesthetics)
Oral sucrose for pain relief
Nonpharmacologic support:
Swaddling
Non-nutritive sucking
Equipment
Gomco (Yellen) or Mogen Clamp:
Clamp is applied to loosen the foreskin and provide a cutting surface for removal.
The clamp reduces blood loss.
Sterile petroleum gauze is used to prevent infection and control bleeding.
Plastibell Device:
A suture is tied around the foreskin at the coronal edge of the glans.
This cuts off circulation, leading the foreskin to fall off within 5 to 7 days.
No petroleum is used with the Plastibell method.
Circumcision Plastibell (Image)

Postprocedure Care for Newborn Circumcision
Nursing Assessment
Monitor for bleeding:
Every 15 to 30 minutes for the first hour
Then check hourly for the next 4 to 6 hours
Observe the first voiding
Nursing Actions
Remove the newborn from the board and swaddle for comfort
Monitor for bleeding and voiding
Apply light gauze pressure if oozing is present
Apply diaper loosely to avoid pressure on the circumcised area
Pain relief:
Liquid acetaminophen 10 to 15 mg/kg orally every 4 to 6 hours (max 30 to 45 mg/kg/day)
Provide discharge instructions to parents regarding infection signs, pain relief, and when to seek medical help
Client Education
Consent must be signed before the procedure
Feeding instructions:
No bottle feeding for 2 to 3 hours before the procedure (aspiration risk)
Breastfeeding is allowed
Diaper care:
Change diapers every 4 hours
Clean penis with warm water at each diaper change
For clamp procedures, apply petroleum jelly for at least 24 hours to prevent sticking
Do not wrap the penis in tight gauze to avoid circulation issues
No tub baths until fully healed, but warm water can be trickled over the penis
Normal healing signs:
A yellowish mucus film may appear by day 2 (do not remove it)
Avoid alcohol-based wipes
Healing process:
Circumcision heals within a couple of weeks
When to notify the provider:
Redness, swelling, strong odor, tenderness, lack of urination, excessive crying, or foul-smelling drainage
Complications and Nursing Management for Circumcision
Hemorrhage
Monitor for bleeding
Apply gentle pressure with a small gauze square
Use Gelfoam powder or sponge to help stop bleeding
If bleeding persists:
Notify the provider (may need vessel ligation)
Have a nurse continue applying pressure while another prepares suture material
Cold Stress / Hypoglycemia
Monitor for heat loss leading to increased respirations and low body temperature
Swaddle and feed the newborn immediately after the procedure
Respiratory Complications
Bradypnea: Respirations ≤ 30/min
Tachypnea: Respirations ≥ 60/min
Abnormal breath sounds: Expiratory grunting, crackles, wheezes
Respiratory distress: Nasal flaring, retractions, grunting, gasping, labored breathing
Interventions
Use bulb syringe for mouth first, then nostrils
Cesarean newborns have more fluid in the lungs
Use mechanical suction if bulb syringe is ineffective
Teach family proper suctioning techniques:
Compress bulb before inserting into side of the mouth
Avoid center of mouth to prevent gag reflex
Suction mouth first, then nostrils
Newborn Identification
Apply two identifiers immediately after birth to prevent mix-ups or abduction
Plastic ID wristbands with locks (cut for removal) placed on ankle and wrist
Info includes:
Newborn’s name, sex, birth date, time, health record number
Footprints of newborn & thumbprints of parents
ID must match parent's band before newborn is given to them
Staff wear ID badges for authentication
No one without an ID badge can remove the newborn from the unit
Many facilities use electronic security systems to prevent unauthorized removal
Thermoregulation
Helps maintain the newborn's core body temperature with minimal oxygen and energy use.
Key Points:
Newborns use brown fat metabolism to stay warm but have limited reserves.
Cold stress can increase oxygen demands and deplete energy.
Monitor for Hypothermia:
Axillary temperature below 36.5°C (97.7°F)
Cyanosis
Increased respiratory rate
Aim to keep core temperature at 36.5 to 37°C (97.7 to 98.6°F)
Temperature Stabilization: Newborn’s temperature usually stabilizes at 37°C (98.6°F) within 12 hours after birth.
Brown fat metabolism
A specialized type of fat tissue that plays a crucial role in energy metabolism and thermogenesis (heat production).
Heat Loss Mechanisms
Conduction (Direct Contact Loss)
Loss of heat to cooler surfaces through direct contact.
Preventive Actions:
Preheat warmer and stethoscope
Place baby on parent's chest and cover with a warm blanket and cap.
Convection (Air Currents)
Heat loss due to cool air around the newborn.
Preventive Actions:
Avoid fans or air conditioning drafts
Swaddle newborn in a blanket and cover the head
Maintain room temperature between 22 to 26°C (72 to 78°F)
Evaporation (Liquid to Vapor Loss)
Heat loss from evaporation of moisture on the skin.
Preventive Actions:
Dry newborn thoroughly with a warm blanket after birth
Delay bath until temperature stabilizes
Radiation (Indirect Surface)
Heat loss to nearby cold surfaces without direct contact.
Preventive Actions:
Keep crib away from windows or air conditioners
Conduction (Direct Contact Loss)
Loss of heat to cooler surfaces through direct contact.
Preventive Actions:
Preheat warmer and stethoscope
Place baby on parent's chest and cover with a warm blanket and cap.
Convection (Air Currents)
Heat loss due to cool air around the newborn.
Preventive Actions:
Avoid fans or air conditioning drafts
Swaddle newborn in a blanket and cover the head
Maintain room temperature between 22 to 26°C (72 to 78°F)
Evaporation (Liquid to Vapor Loss)
Heat loss from evaporation of moisture on the skin.
Preventive Actions:
Dry newborn thoroughly with a warm blanket after birth
Delay bath until temperature stabilizes
Radiation (Indirect Surface)
Heat loss to nearby cold surfaces without direct contact.
Preventive Actions:
Keep crib away from windows or air conditioners
Newborn Care: Bathing, Feeding, and Sleep
Bathing
Bathe only when temperature stabilizes at ≥ 36.5°C (97.7°F).
Delay sponge bath until thermoregulation is stable.
Wear gloves until the newborn’s first bath to prevent exposure to body secretions.
Feeding
Start feeding immediately after birth.
Breastfeeding: Begin as soon as possible (baby-friendly initiative).
Formula Feeding: Start around 2 to 4 hours after birth.
Feed every 3 to 4 hours for bottle-fed infants, more frequently for breastfed infants.
Monitor and document feedings as per protocol.
Sleep
Newborns sleep 16 to 19 hours per day with increasing wakefulness.
Place newborn supine (on the back) to reduce Sudden Unexpected Infant Death (SUID) risk.
No bumper pads, loose linens, or toys in the bassinet.
Parents should sleep near but not share a bed with the newborn.
Educate parents about immunizations to prevent SUID.
Newborn Care: Infection Control & Family Education
Infection Control
Prevent cross-contamination between newborns and staff.
Use individual bassinets with diapers, T-shirts, and supplies.
Hand hygiene: Scrub with antimicrobial soap before entering the nursery.
Follow facility hygiene protocols between newborn care.
Use gowns or uniforms to avoid direct contact.
Family Education
Educate family during nursing care to encourage involvement.
Guide parents in performing newborn care under supervision.
Encourage holding the newborn for eye contact and bonding.
Promote sibling interaction in newborn care.
Newborn Care: Umbilical Cord
Goal: Prevent infection and hemorrhage.
Nursing Actions:
Clamp stays for 24-48 hours.
Clean with water, using cleanser sparingly if needed.
Assess stump for redness, swelling, or drainage during diaper changes.
Fold diaper down to keep the cord dry.
No submersion in water until the cord falls off (10-14 days).
Medications: Erythromycin Eye Prophylaxis
Prevents ophthalmia neonatorum (eye infection from gonorrhea/chlamydia).
Infections occur during birth from exposure to maternal bacteria.
Nursing Actions:
Use single-dose unit to prevent cross-contamination.
Apply a 1-2 cm ribbon to lower conjunctival sac, moving outward.
May cause temporary conjunctivitis (redness, drainage, blurred vision for 24-48 hrs).
Delay application for 1 hour to allow initial bonding and breastfeeding.
Vitamin K (Phytonadione)
Purpose: Prevent hemorrhagic disorders (newborns lack intestinal bacteria to produce Vitamin K).
Nursing Actions:
Administer 0.5 - 1 mg IM into the vastus lateralis soon after birth.
Hepatitis B Immunization
Purpose: Protect against hepatitis B.
Nursing Actions:
Given to all newborns (requires parental consent).
Standard schedule: Birth, 1 month, 6 months.
If mother is hepatitis B-positive
Give hepatitis B immunoglobulin (HBIG) + vaccine within 12 hrs of birth.
KICK LEFT, BE RIGHT
Important: Do NOT inject Vitamin K and Hepatitis B vaccine in the same thigh.
Cold Stress
Signs: Skin pallor, mottling, cyanotic trunk, tachypnea.
Increased oxygen consumption → Can result in hypoxia.
Increased glucose metabolism → Risk of hypoglycemia.
Increased metabolic rate → Can cause metabolic acidosis.
Peripheral vasoconstriction → Can lead to hypothermia anp;d bradycardia.
Nursing Actions:
Monitor for signs of cold stress.
Warm newborn slowly over 2-4 hours.
Administer oxygen for hypoxia.
Correct acidosis & hypoglycemia as needed.
Best Practices for Thermoregulation
Dry immediately after birth to prevent evaporative heat loss.
Use skin-to-skin contact to enhance thermal stability.
Maintain a warm environment to reduce convection and radiation losses.
Prewarm all surfaces before placing the baby to prevent conduction heat loss.
Monitor temperature frequently to detect cold stress early.
Educate parents about proper newborn thermoregulation at home.
Hypoglycemia
Cause: Sudden drop in blood sugar after birth.
Normal newborn tolerance: Blood glucose as low as 30 mg/dL.
At-risk newborns: Preterm, SGA/LGA, infants of diabetic mothers.
Intervention needed if: Blood glucose <40-45 mg/dL.
Nursing Actions:
Monitor for jitteriness, tremors, weak/high-pitched cry, decreased tone, apnea, respiratory distress, seizures, or poor feeding.
Initiate breastfeeding or formula in stable newborns.
Monitor glucose and feed every 2-3 hours for at least 24 hours.
Promote skin-to-skin contact for thermoregulation and blood sugar stabilization
Hemorrhage
Cause: Improper cord care or clamp placement.
Nursing Actions:
Ensure cord clamp is tight.
If blood seepage is noted, apply a second clamp.
Notify provider if bleeding continues.