Oropharyngeal Disorders
1/54
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
55 Terms
Aphthous ulcer (canker sores)
The main cause of oral ulcers that are painful, localized, shallow, round/oval with a yellowish adherent exudate centrally that are more common in childhood/adolescence and typically heal spontaneously within 10-14 days.

familial tendency, trauma, hormones, emotional stress
Risk factors for aphthous ulcers
topical trimcinolone (kenalog orabase), sucralfate suspension, topical analgesics (benzocaine(oragel))
Patient presents to the clinic for mouth pain. On a physical exam you note round, clearly defined ulcers with a yellowish tint. Patient states that this usually happens like 2-4 times a year. What medications can we give to hopefully result in a more rapid healing and provide symptomatic relief?
Oropharyngeal candidiasis (thrush)
A common local infection seen in young infant, people who wear dentures, diabetics, patients on antibiotics, chemo, or radiation therapy, immunodeficient patients, or those on inhaled glucocorticoids.
Pseduomembranous (Most common), atrophic
Forms of oral candidiasis
clotrimazole troche, miconazole mucoadhesive tablets, nystatin suspension
Patient presents to the clinic for mouth pain. A history reveals the patient is a diabetic and wears upper dentures. On a physical exam you note a beefy red tongue and angular chelitis at the corners of the mouth. Inside the mouth you note erythema but no plaques. What medications can we use treat this disorder in non-immunosuppressed peeps?
psuedomembranous
What type of oral thrush is characterized by white plaques on the buccal mucosa, palate, tongue, or oropharynx.
KOH prep should show budding yeast
How can we double check a diagnosis of candidiasis?
immune status eval, HIV testing
If a patient has recurrent, recalcitrant (unresponsive), or extensive oral thrush, what do we need to do?
Sialadentitis
Inflammation of a salivary gland (mainly parotid/submandibular) usually due to an obstructive, infectious, or inflammatory etiology that leads a reduction in salivary flow leading to salivary stasis
dehydration, chronic illness (sjoergens, DM, renal failure, sarcoid), poor oral hygiene
Precipitating factors for sialadenitis
S. aureous
What organism is the most common cause of sialadenitis due to a pathogen from the oval cavity?
CT/US to rule out abscess, tumor, stone, or stricture
Patient presents to the ER for a tender, swollen mass. While collecting a history, your patient notes that her symptoms get worse when she eats. On a physical exam you note ductal opening red with the expression of pus, erythema on the overlying skin, and trismus (lock-jaw) as well as auricle protrusion. What should we order?

Refer to ENT, treat underlying disorder with rehydration, antibiotics, sialagogues (get saliva moving), massage, I & D for abscess
So our CT comes back positive for sialadenitis, how are we treating our patient?
sialolithiasis
A calculus formation in the salivary ducts usually found in patients with a history of sialadentitis and/or stricture
Surgical treatment by ENT (dilate duct, excise duct and gland)
Patient presents to the clinic for pain after eating (postprandial pain). On a physical exam you note local edema and a palpable stone near salivary duct opening. What is our treatment plan?
Ludwig Angina
A bilateral infection of the submandibular, sublingual, and submylohyoid (submaxillary) space, more commonly arises from an infected second/third mandibular molar tooth, typically aggressive, rapidly spreading cellulitis without lymphadenopathy.
CT, broad spectrum IV antibiotics with coverage for MRSA
Patient presents to the ER with respiratory distress. Patient is drooling and has muffled voice. She reports fever, chills, malaise, mouth pain, and a stiff neck. On a physical exam you note edema of the upper neck and displacement of tongue up and backward. Vitals are stable with the exception of fever. What is our treatment plan?

acute laryngitis
self-limited inflammation of the vocal cords lasting for less than 3 weeks that is often associated with rhinorrhea, cough, and mild sore throat
acute vocal strain, URI usually viral or Moraxella Catarrhalis, H. influenzae, S. pneumoniae, Others (GERD, alcohol/tobacco, harsh chemicals)
Etiology of acute laryngitis
Complete voice rest, hydration, humidification, oral glucocorticoids (for patients who need their voice), treat the cause (macroglide if bacterial or manage reflux)
Patient presents to the clinic with hoarseness. They also report a runny nose, cough, and mild sore throat. How are we treating this?
laryngoscopy by ENT
If hoarseness persist for greater than 2 weeks that do we need to do?
Pharyngitis
One of the most common conditions in family practice that can be infectious (viral and bacterial) or noninfectious
adenovirus, rhinovirus, coronavirus
Most common viral causes of pharyngitis
group A strep
Most common bacterial causes of pharyngitis
sensitive rapid antigen test (RADT)
Patient presents to the clinic for URI symptoms such as cough and congestion. She also reports ear pain, rhinorrhea, and hoarseness. What do we need to order?

Supportive care - oral NSAIDs, rest, adequate fluids, avoidance of respiratory irritants, soft diet
If your RADT test comes back negative, how are we treating the patient?
oral penicillin V
If your RADT test comes back positive, how are we treating adult patients?
oral penicillin V or amoxicillin
If your RADT test comes back positive, how are we treating pediatric patients?
cephalosporins, clindamycin, macrolides
If your RADT test comes back positive, how are we treating patients with a penicillin allergy?
Bacterial pharyngitis
Patient reports to the ER with an acute onset sore throat. Vitals are stable with the exception of a fever. Patient reports dysphagia and odynophagia. On a physical exam you note anterior cervical lymphadenopathy, patchy tonsillar exudate, palatial petechiae, and strawberry tongue. What are we thinking team?

EBV, viral, bacterial, post-nasal drip, peritonsillar abscess, diphtheria
Differentials for pharyngitis
muffled (hot potato) voice, drooling/pooling of saliva, stridor, respiratory distress, tripod positions, severe unilateral sore throat, bulging of pharyngeal wall/soft palate/floor of oropharynx, crepitus, stiff neck or trismus, toxic appearence, fever, rigors, hx of penetrating trauma to oropharynx
What are some red flags in pharyngitis that require urgent management?
5-7 episodes of strep pharyngitis in 1 year
At what point in pharyngitis do you refer to ENT for possible tonsillectomy?
Peritonsillar abscess
An infection and collection of pus in the tonsillar fossa and is generally preceded by tonsillitis or pharyngitis and processes from cellulitis to abscess.
CBC, CMP (serum electrolytes), rapid strep, gram stain/culture of abscess fluid
Patient presents to the ER with a severe unilateral sore throat. Vitals are stable with an exception of a fever. Patient is having a hard time speaking due to pooling of saliva and a muffled voice. She does report ear pain on the same side as her sore throat and lockjaw. On a physical exam, you note an extremely swollen, fluctant tonsil with deviation of the uvula to the opposite site. What labs do you need to order?
intraoral/submandibular US
In the case of a peritosillar abscess what can help distinguish it from cellulitis and guide the needle for aspiration?
ENT referral, drainage (needle aspiration) + culture, antibiotics, supportive care
What’s our treatment plan for peritonsillar abscesses?
amoxicillin-clavulnate (augmentin), clindamycin (cleocin)
Concerning peritonsillar abscess which anitbiotics do we use?
asphyxia, aspiration pneumonia, retropharyngeal abscess, brain abscess, meningitis, cavernous sinus thrombosis
Complications with peritonsillar abscesses?
Angioedema
A hypersensitivity reaction that involves deeper subcutaneous tissue with swelling of lips, eyelids, palms, soles, and genitalia associated with systemic complications such as laryngeal edema and hypotension
family hx, GI/respiratory symptoms
In hereditary angioedema theres is generally a positive
ER (MY HOUSE)
Since ABCs are step 1 in managing angioedema, where we going fam?
Start CPR
Patient presents to the ER after being sent over from their PCP for an allergic rxn. You note severe swelling of the lips, eyelids, palms, and soles. Vitals are as follows BP 30/dead, 0 bpm, 0 RR. What’s are we doing team?
2nd gen H1 antihistamines (fexofenadine, cetirizine, loratadine), 1st gen antihistamines (hydroxyzine, cyproheptadine), or Doxepin (a TCA that has antihistamine properties)
Mainstay of treating angioedema includes
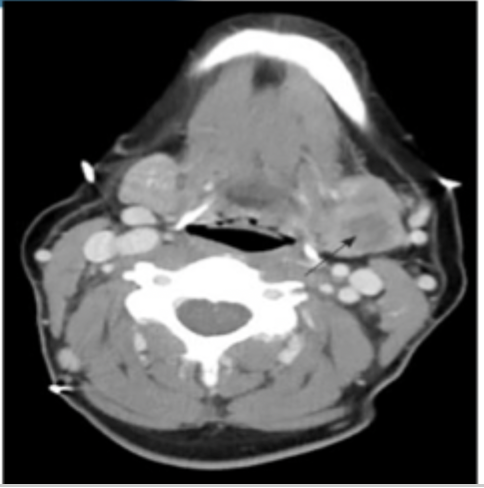
deep neck infection
An infection that affects the neck’s cervical spaces and can rapidly progress to life-threatening that typically arise from local extension of infections in the tonsils, parotid glands, cervical lymph nodes, and ondontogenic structures
CBC, x-ray, u/s of neck, CT, MRI, culture/sensitivity
Patient presents to the ER for neck pain that is exacerbated on movement. Patient notes a history of IV drugs use. Patient reports dental pain and dysphagia. While conducting a physical you note stridor and trismus. The neck looks asymmetrical, red, swollen, and regional lymphadenitis. What can we order to assist in the diagnosis?
s. pyogenes, strep viridans, S. aureus, Klebsiella, gram negative rods, anaerobes, fusobacterium species
Possible microbes that cause a deep neck infection
immunocompromised, recent oral/dental procedures, recent neck/oral trauma, recent neck trauma/radiation, IV drug use, DM
Predisposing factors in deep neck infections
IV nafcillin/vancomycin + gentamycin/tobramycin combination, OR amplicillin/sulbactam or clindamycine, IV vanc/linezoid + cefepime
Treatment and management of deep neck infections includes
metronidazole, imipenem, meropenem, piperacillin-tazobactam
Alternative meds for treatment and management of deep neck infections includes
meningitis, apical pneumonia, subarachnoid hemorrhage
Neck pain with fever can also be caused by
trauma (cervical fractures/dislocation)
Acute neck pain, especially with asymmetry can be a result of
acute epiglottitis, bacterial tracheitis, croup
For patients presenting with stridor think
spread to carotid sheath (septic thrombophelbitis), acute midiostinitis,(empyema/pericarditis), Respiratory failure due to obstructed airway, sepsis, intracranial infections
Complications of deep neck infections