Ch 10: Gallbladder
1/169
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
170 Terms
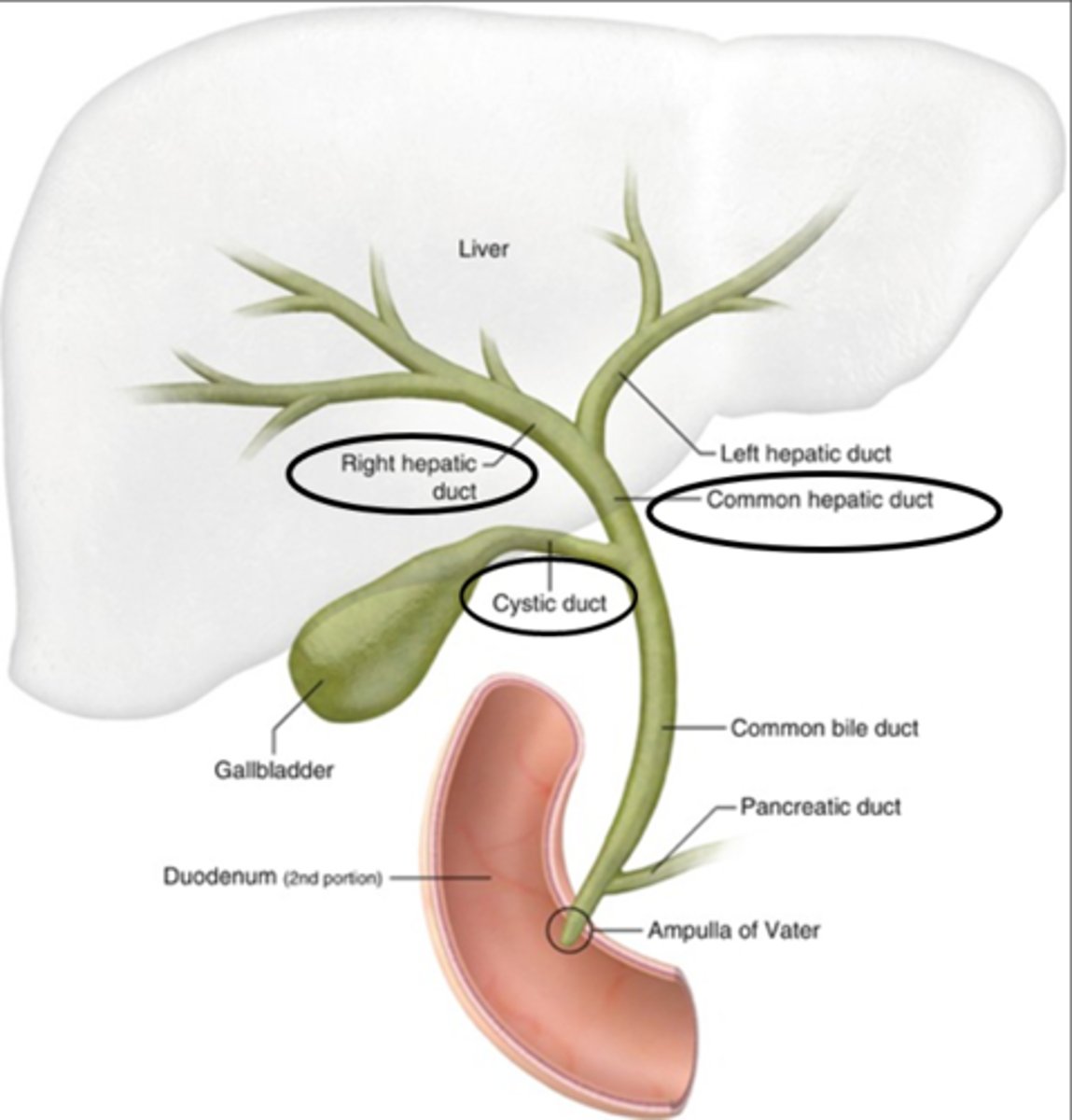
Biliary system includes:
- right and left hepatic ducts
- CHD
- cystic duct
- CBD
- gallbladder
CHD Diameter
4mm
CBD diameter
6-7mm
- increases in size w advancing age
The intrahepatic ducts:
right hepatic duct and left hepatic duct
The right and left hepatic ducts emerge from the _____________ and unite to form the ___________.
right lobe of liver in the porta hepatis; common hepatic duct
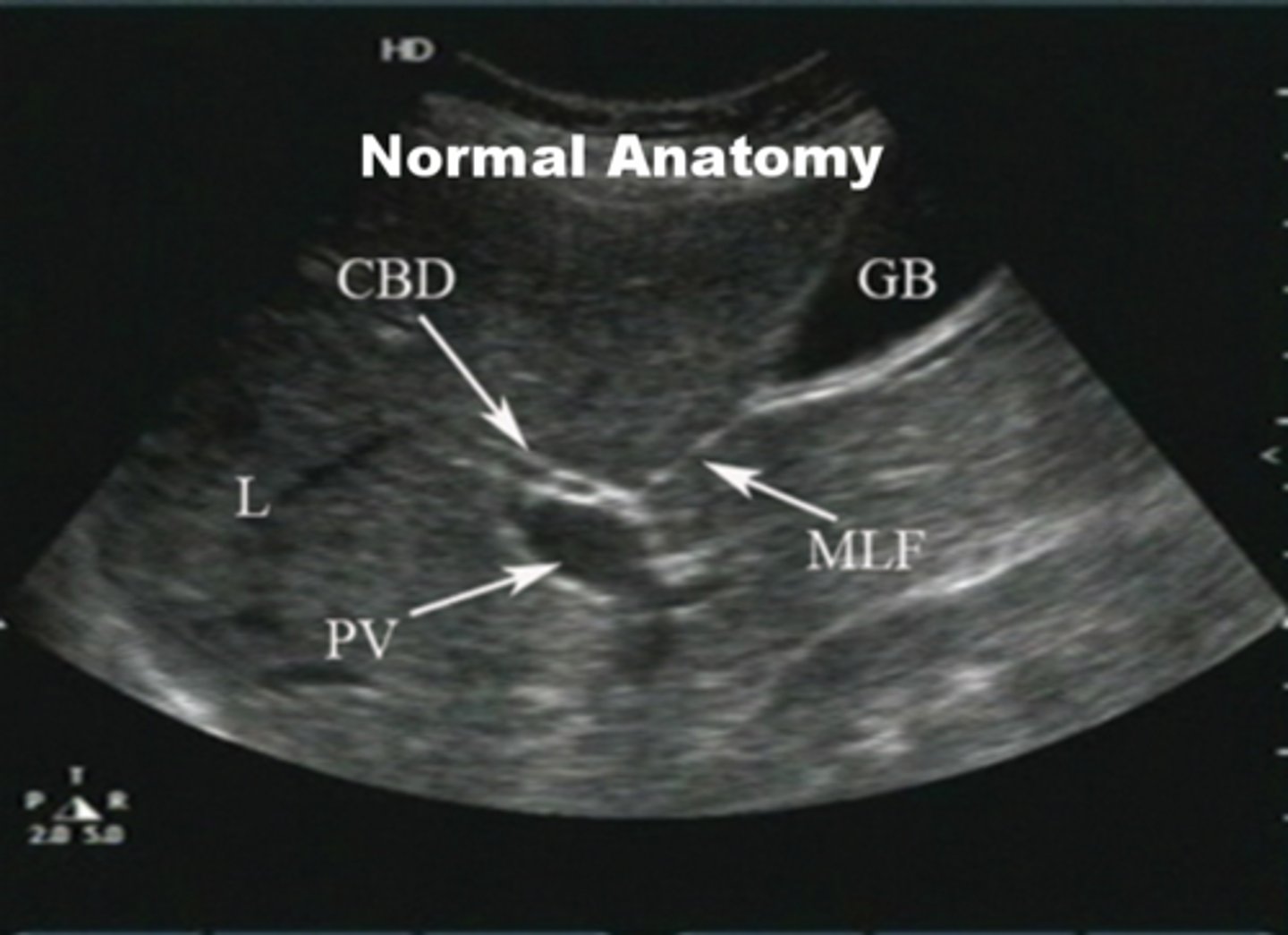
the hepatic duct runs parallel to the
portal vein
What segment is proximal/above the cystic duct?
CHD
What segment is below/distal to the cystic duct?
CBD
Which two ducts unite to form the CBD?
CHD and cystic duct
Common bile duct location:
posterior to the first part of the duodenum and lies in a groove on the posterior surface of the head of the pancreas
CBD is joined by ______ and they open through ____into the duodenum.
duct of Wirsung; ampulla of Vater
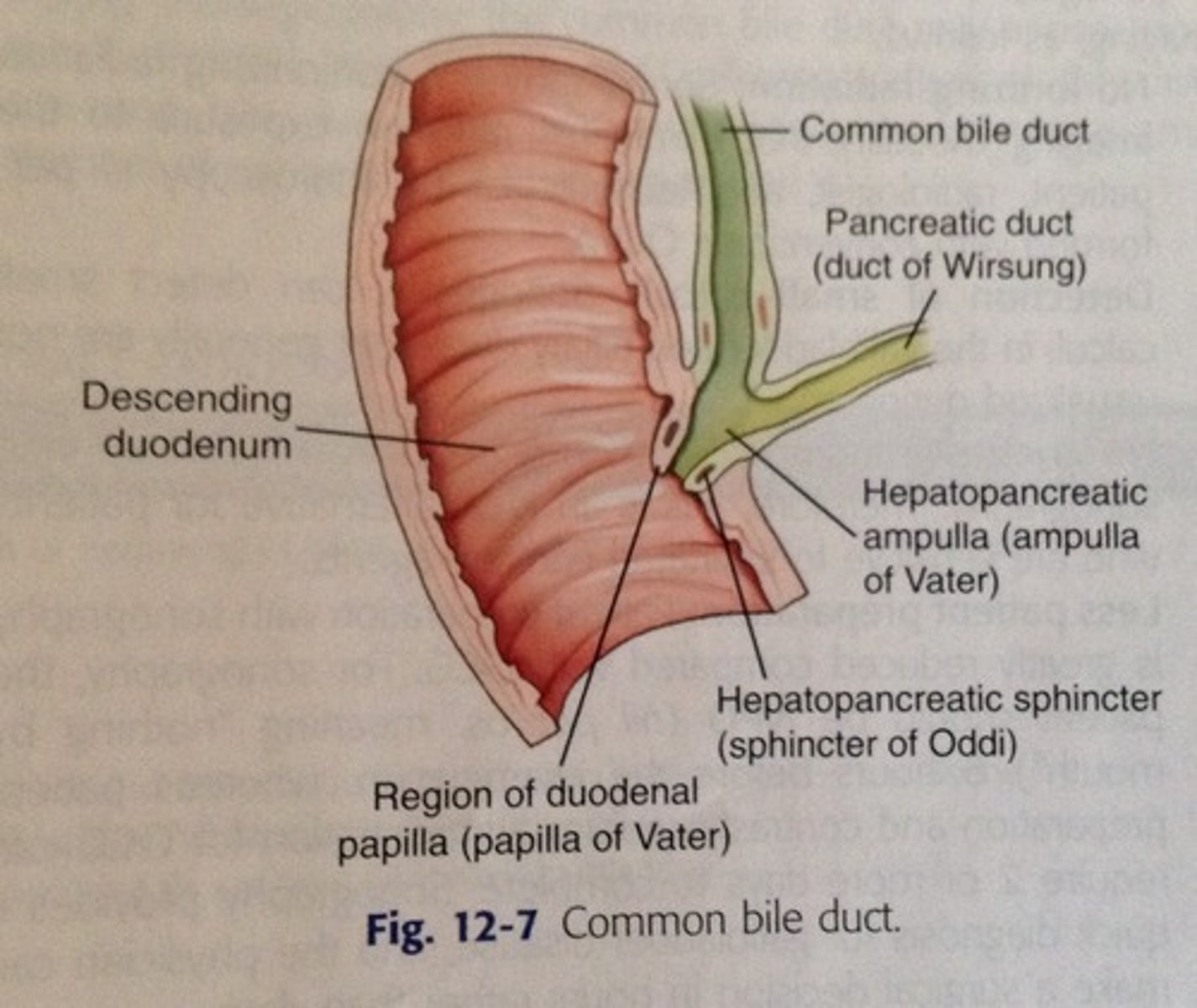
circular muscle fibers that surround the end parts of the CBD, Wirsung duct, and Ampulla of Vater
sphincter of Oddi
portal triad
CHD, MPV, PHA (mickey mouse sign)
The _____ branches from the celiac and travels anterior to the portal vein and medial to the common duct.
PHA
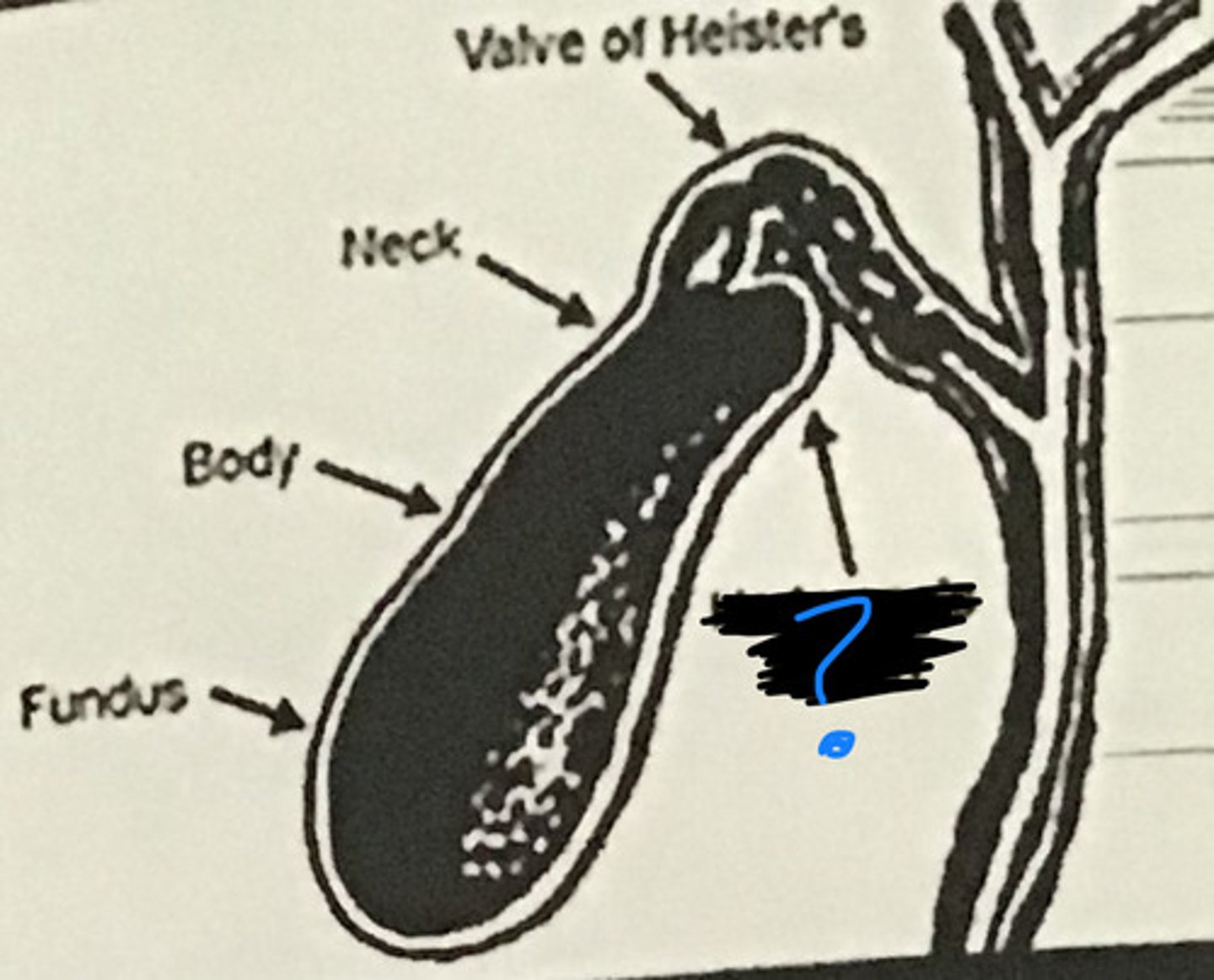
connects the neck of the gallbladder and the CHD to form the CBD
cystic duct
controls flow of bile in the cystic duct and prevents kinking of the duct
spiral valves of Heister
Is the GB intraperitoneal or retroperitoneal?
intraperitoneal
GB is located on the ____ margin of the liver.
inferior
Landmarks of the gallbladder:
MHV and interlobar fissure (main lobar fissure), PV
Parts of the gallbladder
Fundus, body, neck:
most dependent portion of GB
fundus
- also most common location for gallstones
what part of the GB is contiguous with the cystic duct?
neck
Normal size of GB and GB wall
- 7 or 8-10 cm long,
- 2.5-4 or 5 cm diameter (transverse)
- GB wall less than 3mm thick
What makes the gallbladder wall thicker than normal?
cirrhosis
small out pouch or infundibulum at the neck where gallstones may collect
Hartmann's pouch
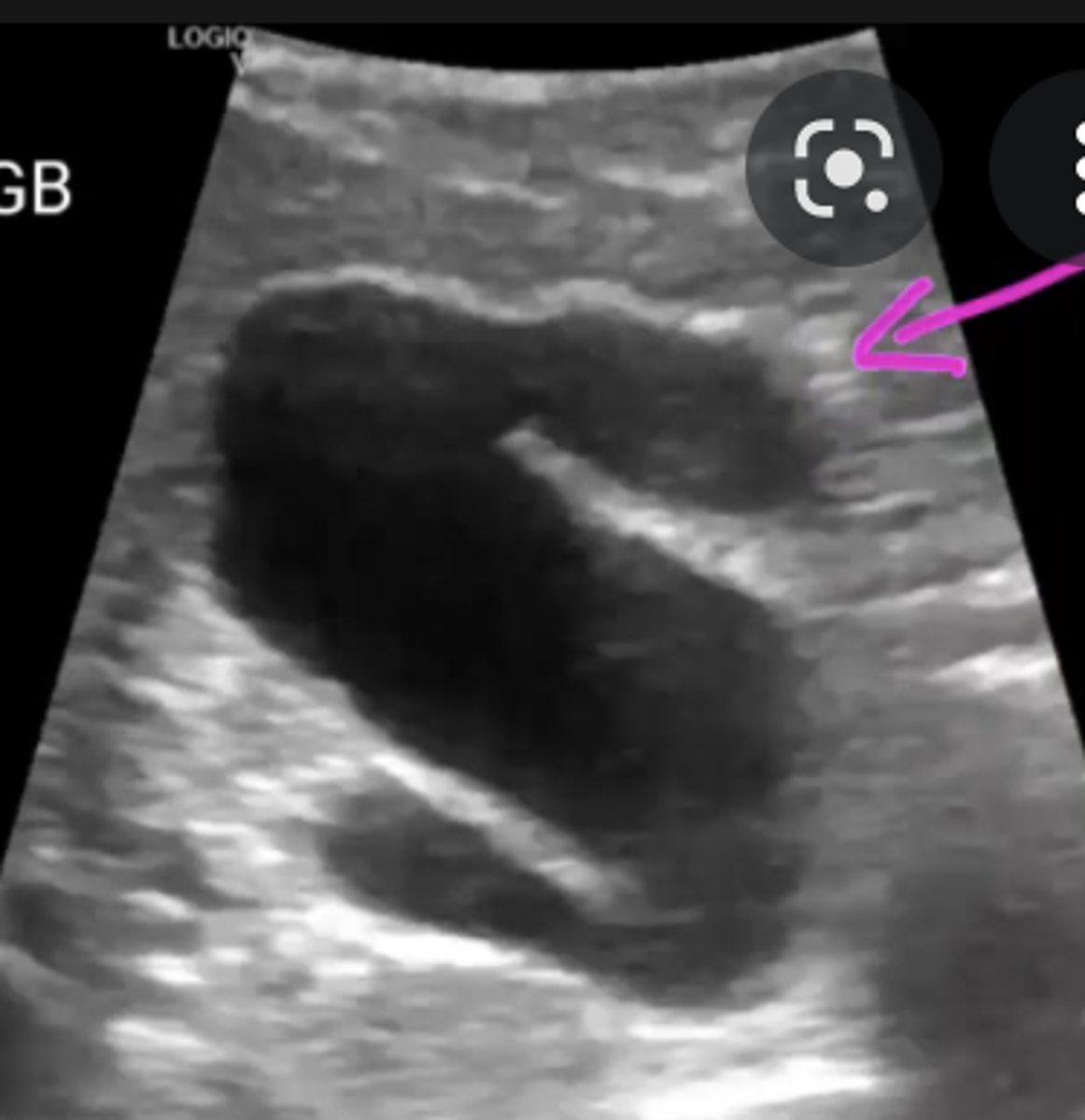
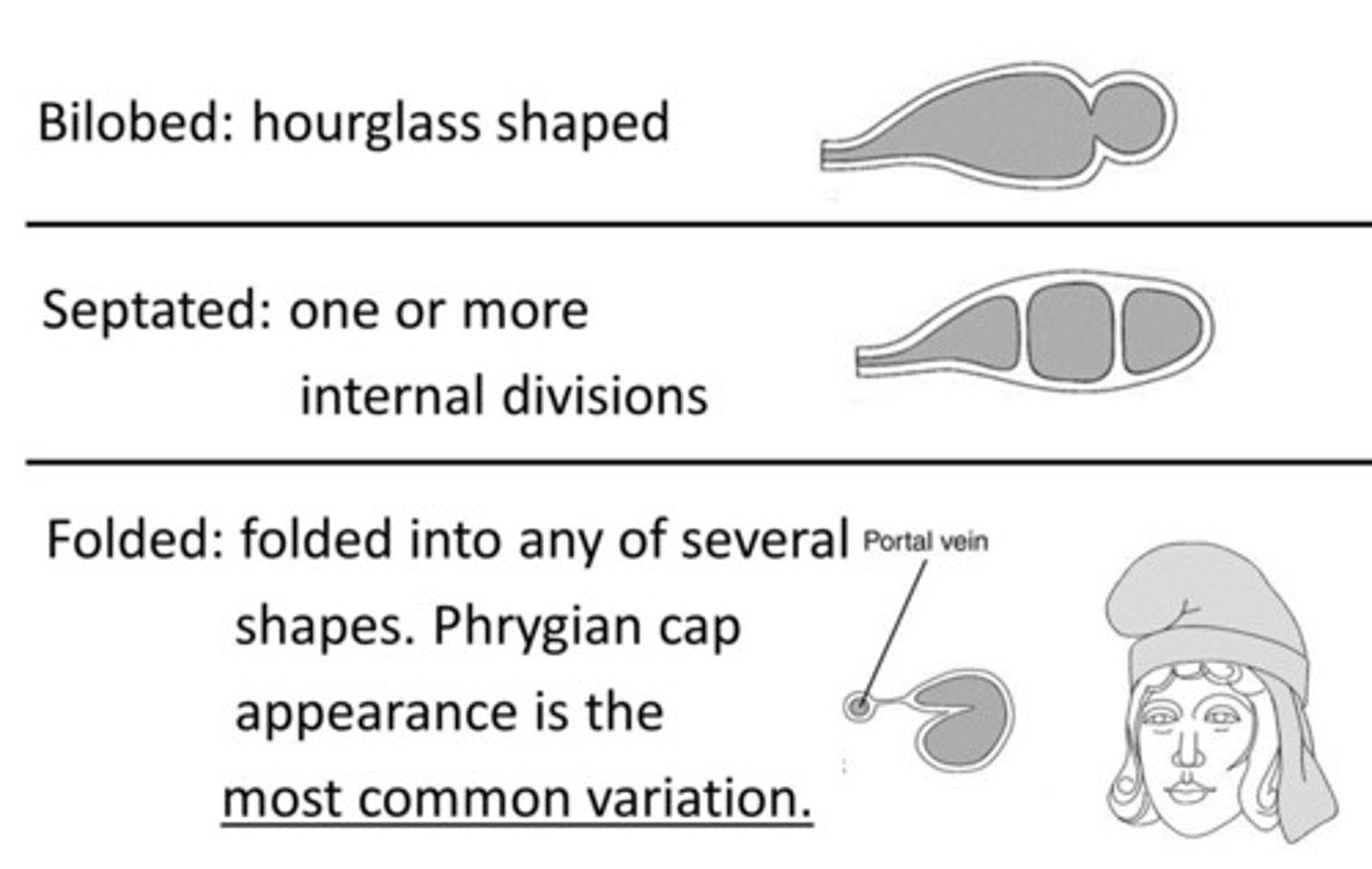
GB folded at fundus is what variation?
Phrygian Cap
what has potential to cause twisting of blood supply and therefore causing GB torsion or GB volvulus?
floating GB
Other anatomic variations to be familiar with:
septated
double GB
Agenesis
Hypoplasia
What makes up the vascular supply of the GB?
cystic artery and cystic vein
cystic artery is a branch of ___
right hepatic artery
cystic vein drains into _______
portal vein
function of GB and biliary tract
serves as a reservoir for bile and ducts that regulate the flow of bile.
bile is transported from the ______ to the ________
liver, intestine
What hormone causes the GB to contract? How is it stimulated and what releases it?
CCK; stimulated when chyme (partially digested food from the stomach) is released by the duodenum
cholecystectomy
surgical removal of the GB
_______________ of extrahepatic bile ducts occurs after removal of the GB because bile is no longer retained in the bile ducts and is free to flow into the duodenum during fasting and digestive phases.
Dilation
NPO for at least
4-6 hours, 8 is optimal
What frequency is best to scan GB?
2.5 to 5 MHz curvilinear probe
Patient position to scan GB
supine and LLD
-must change patient position to document mobility of stones (or polyp if no movement occurs)
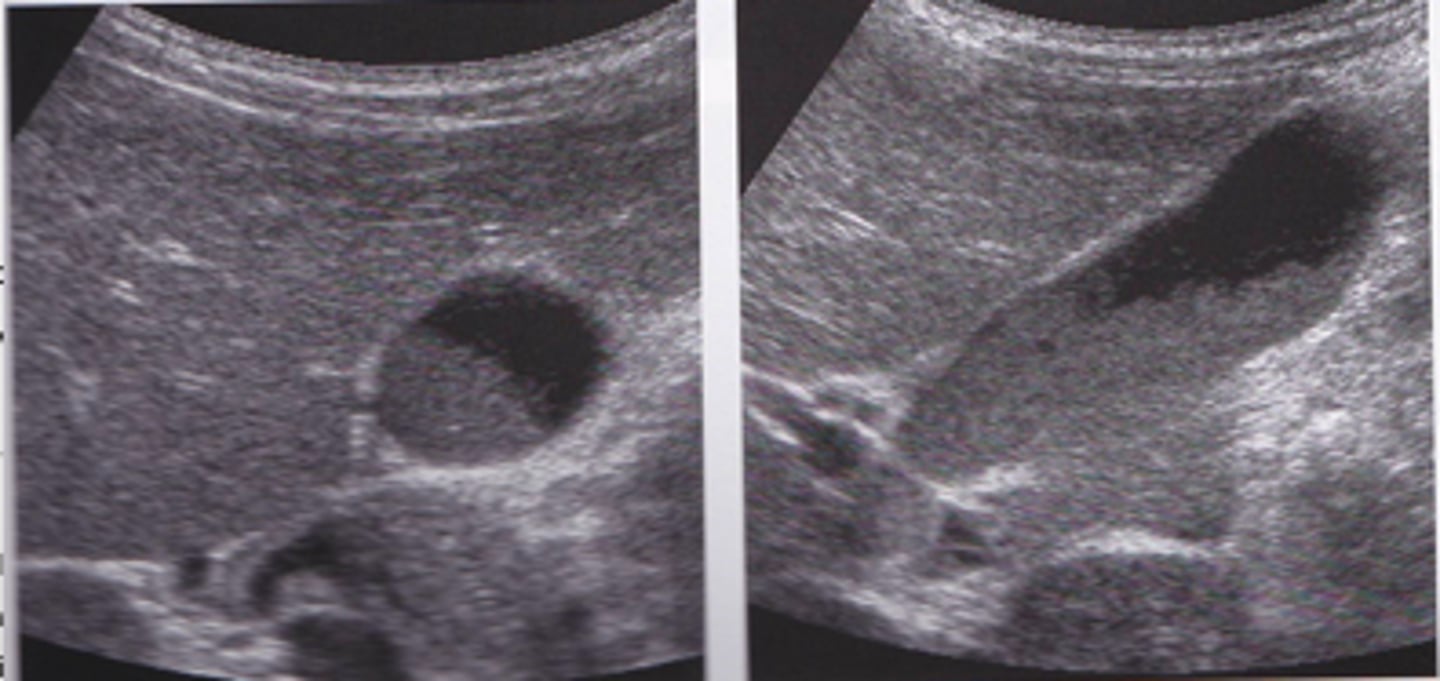
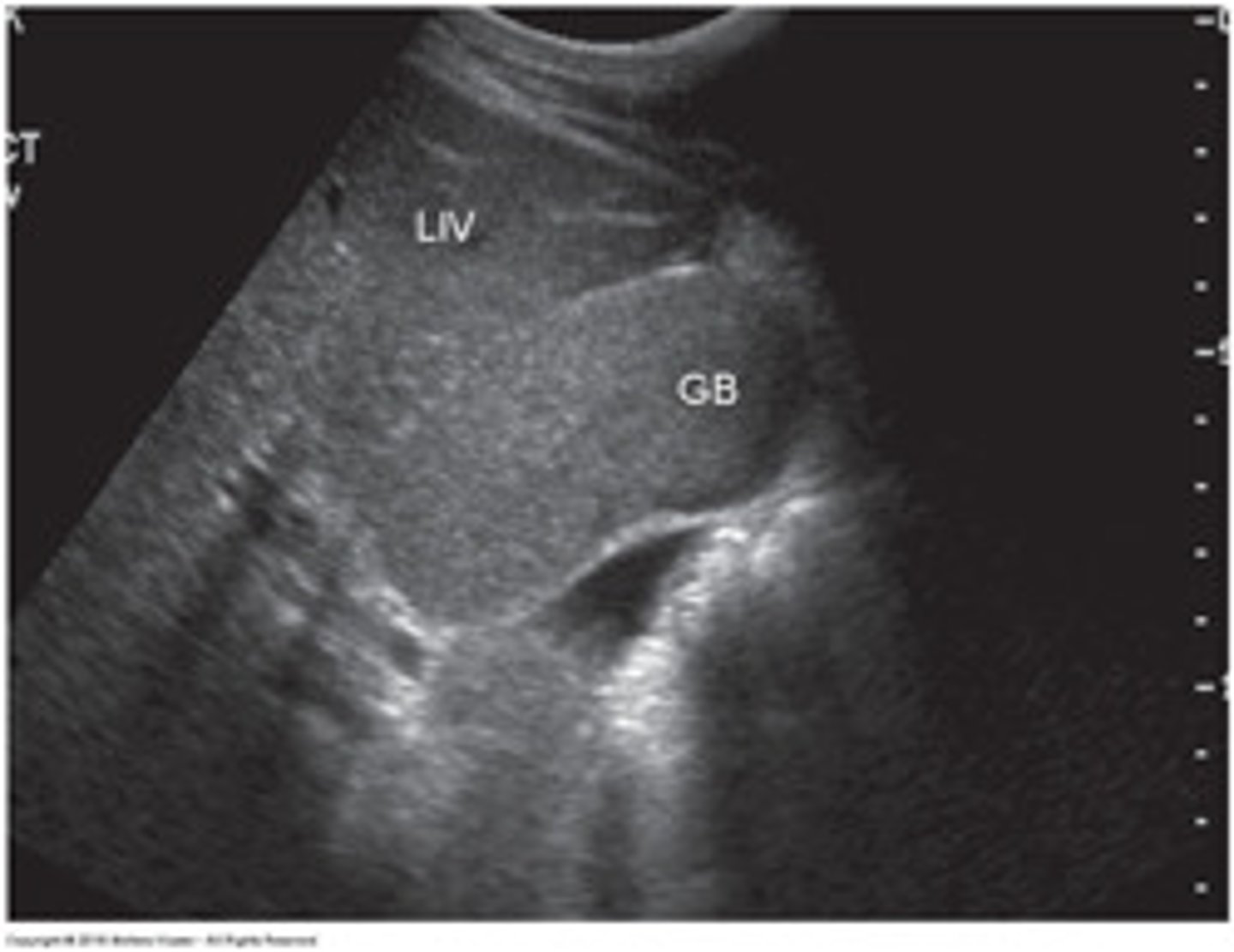
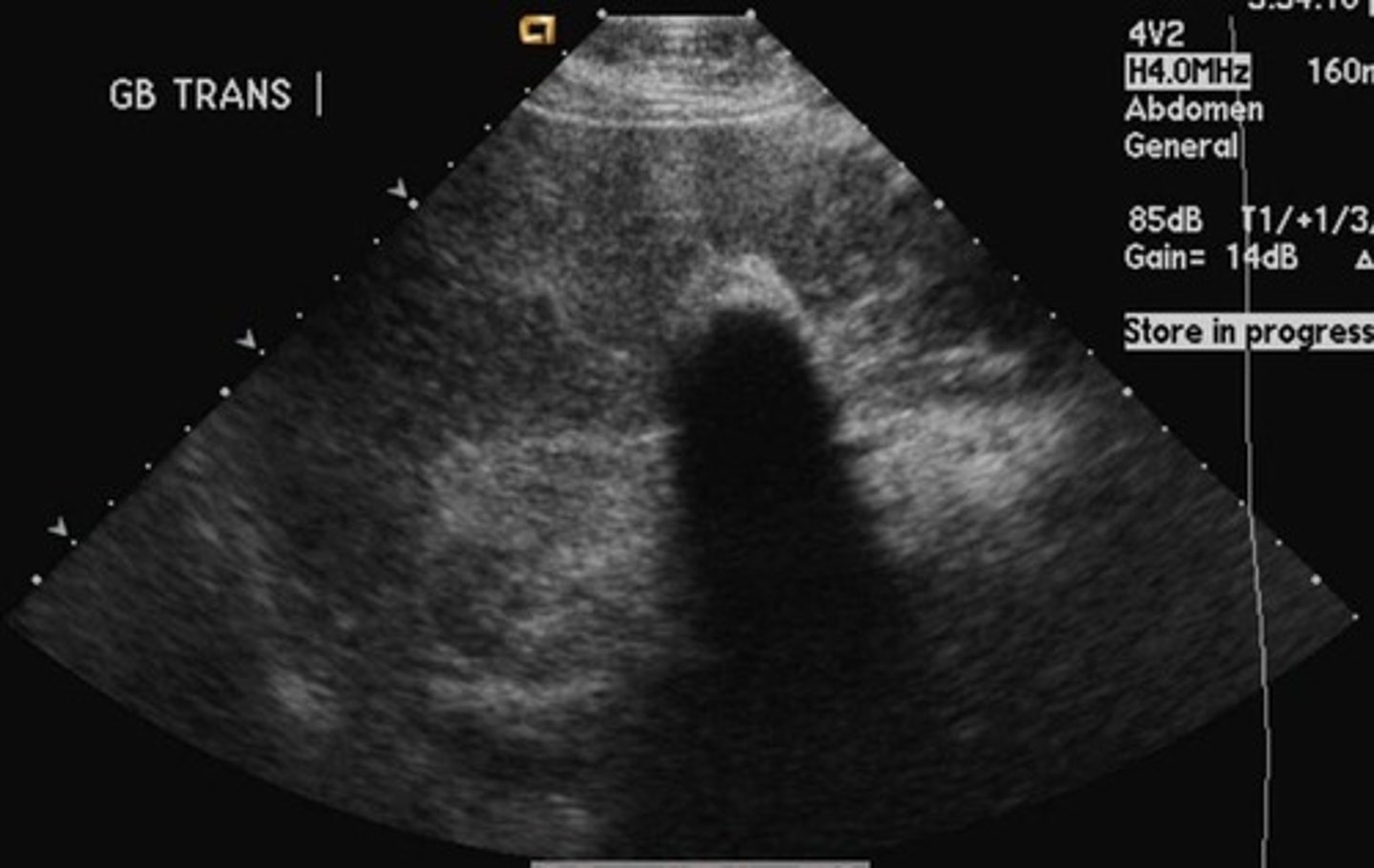
In the sagittal plane, the GB appears as an:
anechoic, pear-shaped structure located anterior to the right kidney and lateral to the head of the pancreas and duodenum
In the transverse plane, the GB appears as an:
anechoic and rounded
landmarks for identifying GB
Interlobar fissure/Main Lobar Fissure - appears as echogenic
linear structure connecting GB to MPV.
if the GB has been removed, the fossa appears as
an echogenic indentation as the result of remaining connective tissues
What is the most common clinical symptom of GB disease? Other symptoms?
-RUQ abdominal pain after eating greasy foods
- nausea and vomiting may indicate stones
- Right shoulder pain
- Jaundice
Nausea and vomiting may indicate________.
gallstones
Helpful labs to evaluate/check for elevation in the presence of suspected
GB disease are:
• ALP
• ALT
• Bilirubin
• GGT
• WBC
Courvosier Gallbladder
enlarged gallbladder that does not contract
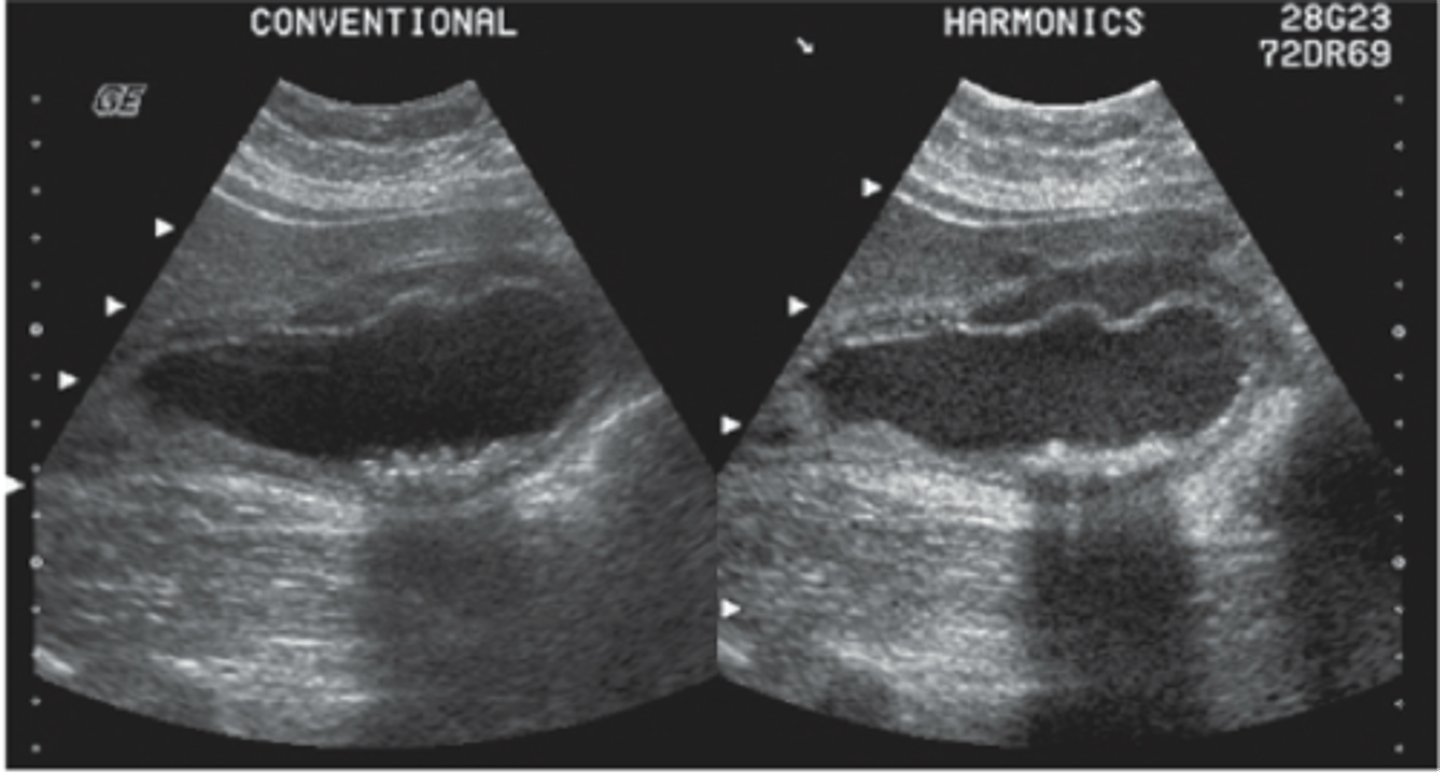
Sludge
- thickened/viscid bile that occurs from bile stasis
Sludge is composed of
calcium bilirubinate and cholesterol crystals
Causes of sludge
- prolonged fasting
- parenteral nutrition
- obstruction of GB or cystic duct
- GB cancer
- liver disease
- jaundice
- sepsis
*may be seen with cholelithiasis or cholecystitis
Sludge clinical symptoms
asymptomatic
Sludge sonographic findings
GB may be packed with sludge and difficult to distinguish from liver parenchyma because it will appear isoechoic (aka hepatization).
Prominet GB with amorphous, low-level echoes without posterior shadowing located in the dependent portion of the gallbladder
Sludge is gravity dependent- will move with change in patient position
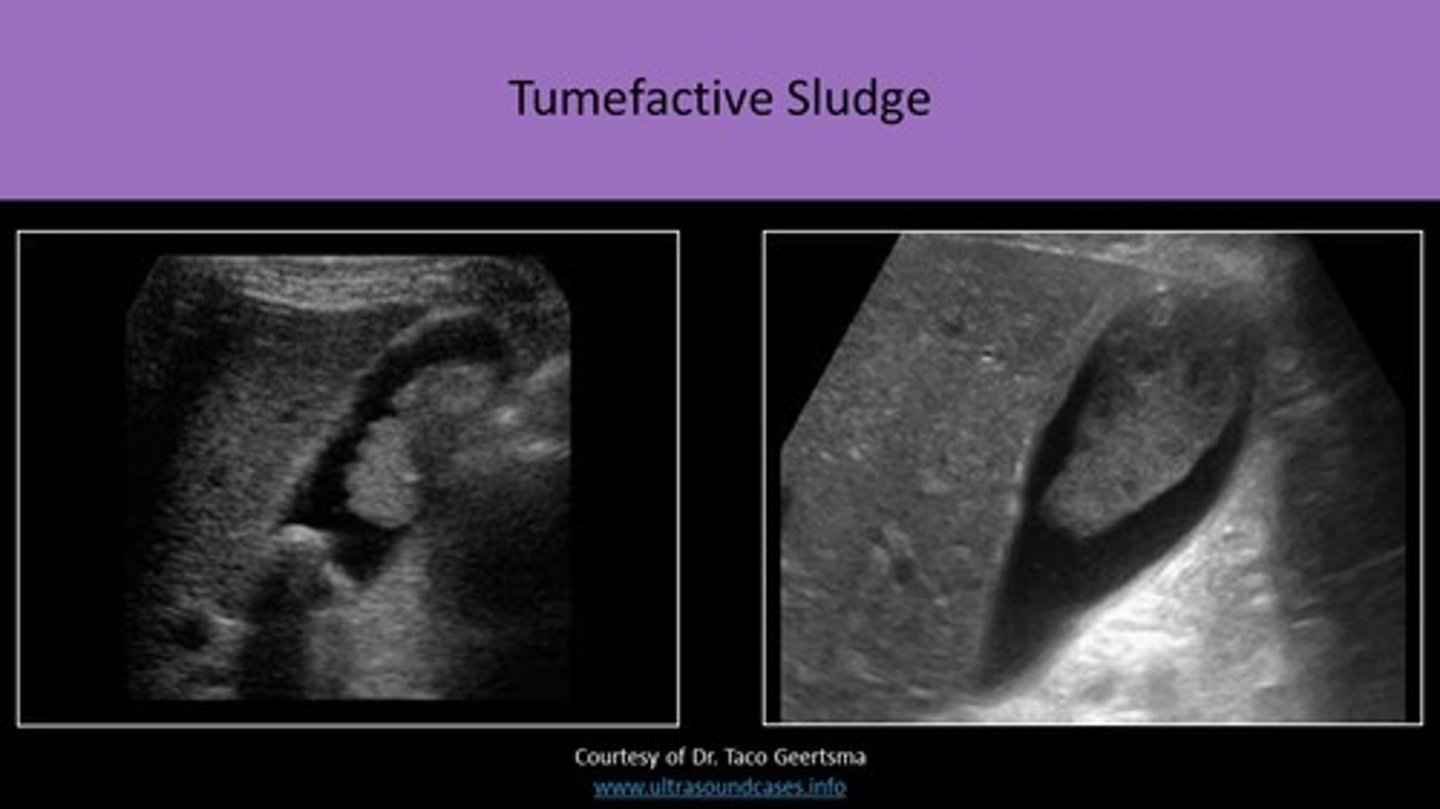
tumefactive sludge is
sludge that mimics polypoid tumors/GB mass
normal GB wall thickness
less than 3mm
Most common cause of wall thickening:
Other causes?
cholecystitis- most common
-hypoalbuminemia
-acsites
-hepatitis
-congestive heart failure
-pancreatitis
How do you measure wall thickness of GB?
Measure outer wall to outer wall. typically in transverse plane
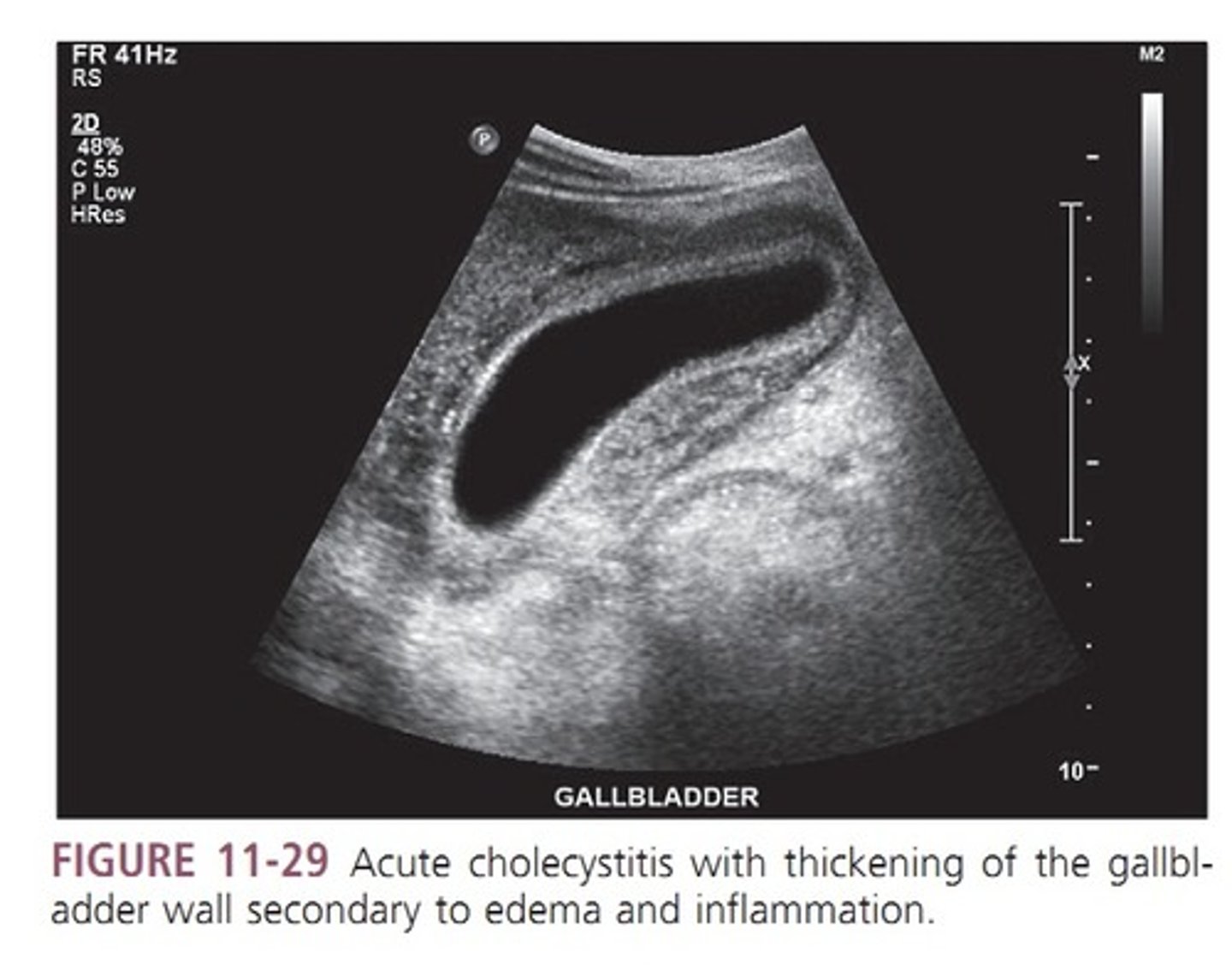
Cholecystitis
inflammation of the gallbladder (can be acute or chronic)
Acute cholecystitis
sudden onset of GB inflammation
Most common cause of acute cholecystitis:
What can this do?
persistent obstruction of the cystic duct or GB neck by an impacted stone
-impacted stones result in obstruction and distention of the GB lumen, ischemia, and infection with eventual necrosis and potential perforation of the GB
Who is more frequently impacted by acute cholecystitis?
females
-impact decreases as you age
Clinical Findings of acute cholecystitis
Acute RUQ or epigastric pain, fever, nausea and vomiting, pain radiating to shoulders, leukocytosis, elevated ALP, ALT, GGT, elevated bilirubin if duct is obstructed.
*positive sonographic murphy sign- focal tenderness over the GB with transducer pressure*
complications of acute cholecystitis
- Empyema (collection of pus)
- Emphysematous or gangrenous cholecystitis
- perforation of GB
- pericholecystic abscess
acute cholecystitis sonographic findings
- GALLSTONES
- pericholecystic fluid
- sludge
- thickened GB wall
- distended lumen greater than 4cm
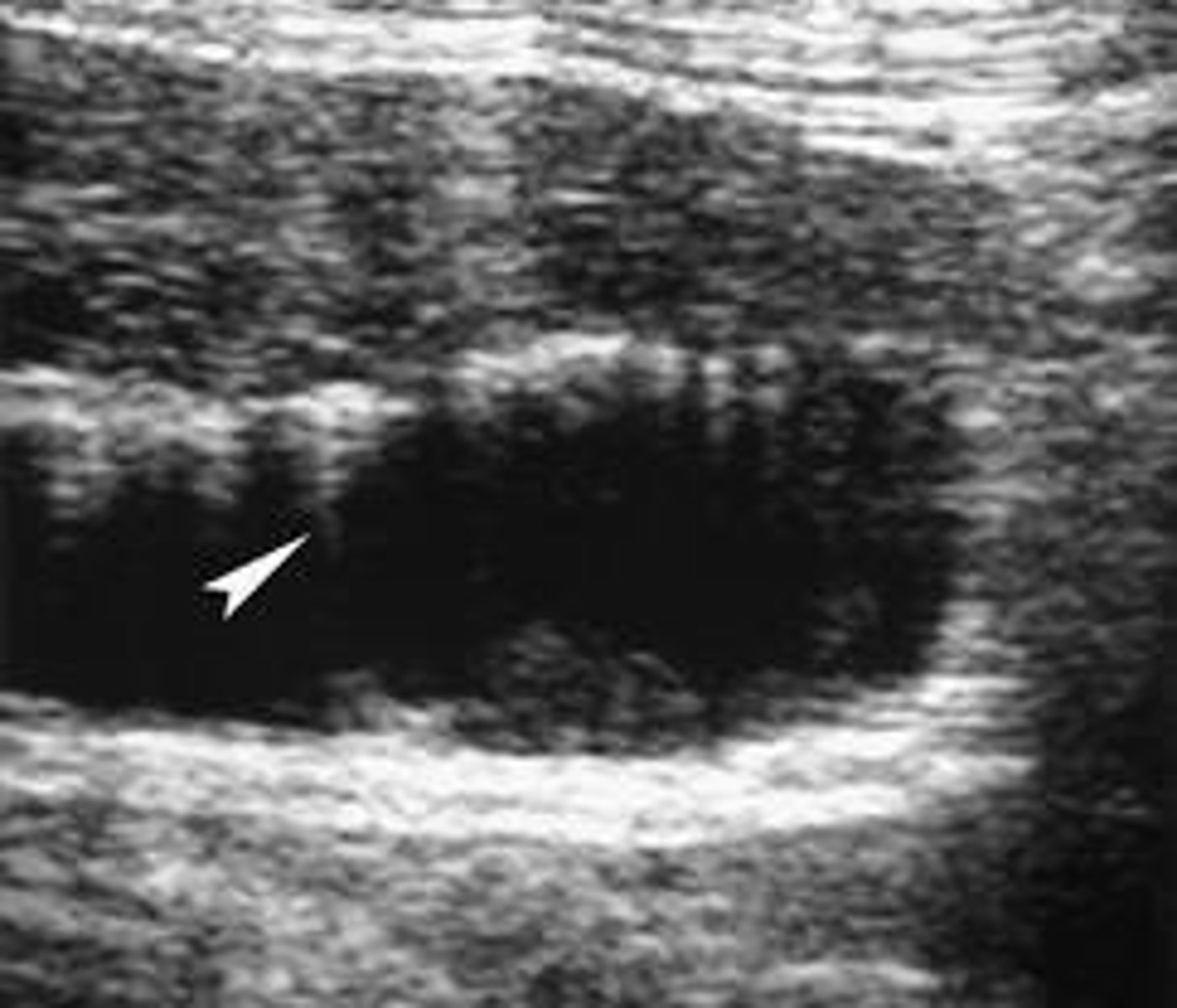
Emphysematous Cholecystitis
-rare complication of acute cholecystitis
-due to ischemia and infection
-gas-forming bacteria in the GB wall, lumen, biliary tree
-occurs in elderly, diabetic men
Complications can lead to perforation, sepsis, become fatal
*surgical emergency*
Clinical symptoms of Emphysematous Cholecystitis
-RUQ pain, possibly without positive murphy sign
-fever
Sonographic findings of Emphysematous Cholecystitis
- Bright echo along anterior GB wall
-gas bubbles in the wall that cause dirty shadowing, reverberation, or ring-down artifact
-bubbles will rise to the non-dependent wall, causing the champagne sign
-WES sign if large amount of gas is present
WES sign
wall echo shadow
Gangrenous Cholecystitis and Gallbladder Perforation
-GB fundus is the most common site for perforation
-rare, life-threatening complication of acute cholecystitis
-gangrenous can lead to perforation which has a high mortality rate secondary to peritonitis
-occurs after prolonged infection, causing GB to undergo necrosis
Gangrenous cholecystitis differential diagnosis
empyema of the GB (aka suppurative cholecystitis) which is acute cholecystitis with bacteria-containing bile which leads to infection and the GB fills with purulent material (pus).
Gangrenous cholecystitis clinical symptoms
-patient may not have + murphy sign
-RUQ, epigastric, or abdominal pain
-leukocytosis
-possible elevation of ALP, ALT, GGT and bilirubin
-fever
-pain radiates to shoulders
-nausea and vomiting
Gangrenous cholecystitis sonographic findings
-diffuse medium to coarse echogenic densities filling the GB lumen
-thickened GB wall
-focal wall necrosis, hemorrhage, or exudate (mass of cells and fludi thats seeped out of blood vessels or organ)
-bulges of GB wall
-ulcerations or perforations resulting in pericholecystic abscess
-gallstones or fine gravel
-distinct GB wall tear
-GB appear irregular in shape
-sludge

acalculous cholecystitis
(acalculous mean no stones)
-inflammation without cholelithiasis (gallstones)
-more commonly found in children, recently hospitalized patients, or someone immunocompromised.
-caused by decreased blood flow through the cystic artery
-associated with parenteral IV nutrition (not eating by mouth), post op abdominal surgery, severe trauma and burns, sepsis, HIV/aids, and blood transfusion reaction
Acalculous cholecystitis clinical symptoms
- same as acute cholecystitis EXCEPT NO GALLSTONES
-RUQ tenderness
-epigastric/abd. pain
-leukocytosis
acalculous cholecystitis sonographic findings
- POSITIVE murphy sign
- Gb wall extreme thickening > 4-5 mm
-pericholecystic fluid
- sludge
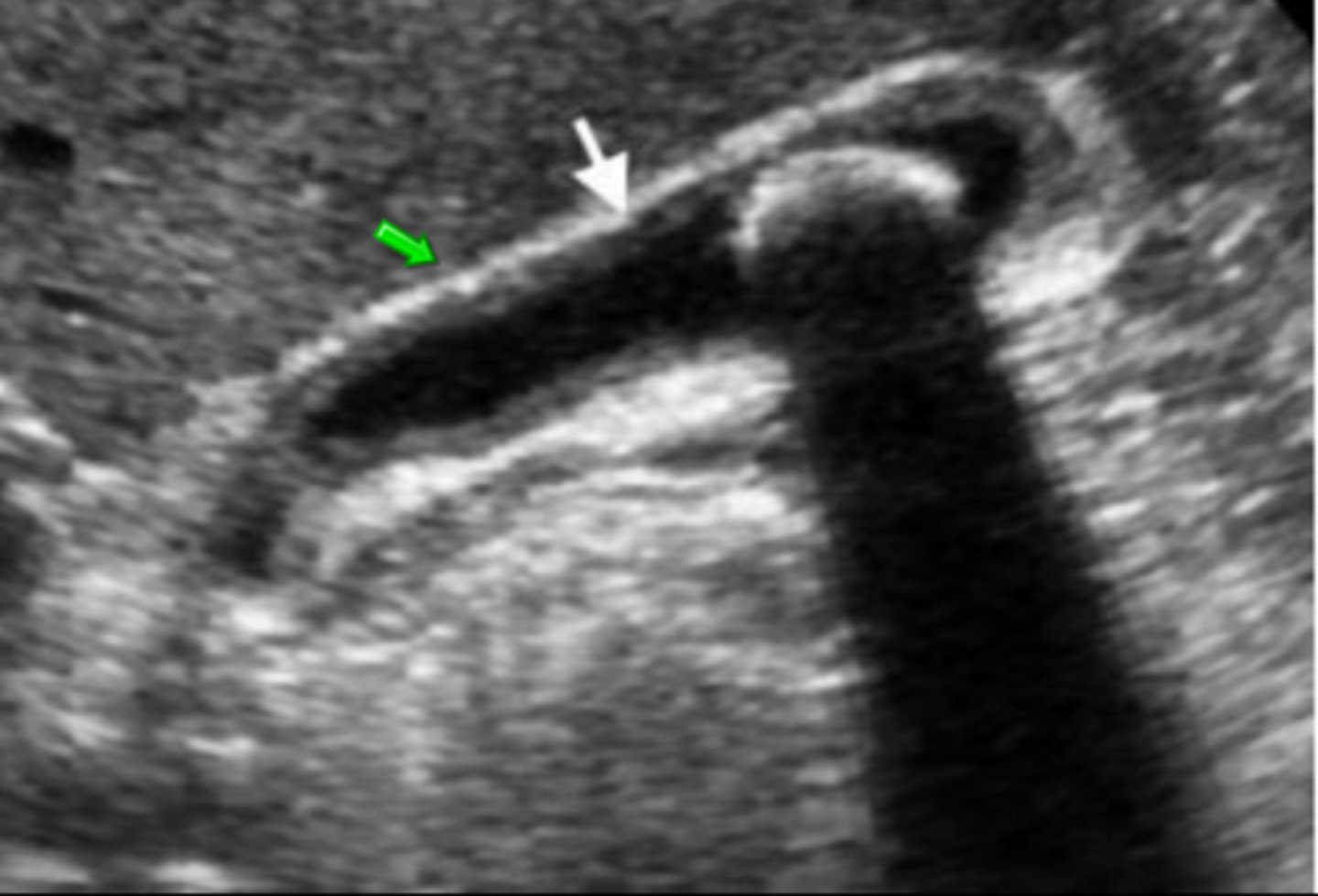
chronic cholecystitis
*Most common form of cholecystitis*
-results from multiple attacks of acute cholecystitis/intermittent obstruction of the cystic duct by gallstones
Chronic cholecystitis clinical symptoms
- intolerance to fatty foods
- nontender gallbladder (no murphy sign)
Chronic cholecystitis sonographic findings
similar to acute cholecystitis
-thickened GB wall
-contracted GB
-gallstones
-WES sign
Torsion of the GB aka _______ is where the GB _______
gallbladder volvulus (GV), twists on itself
-rare, found in elderly females
-associated with mobile/floating GB
-surgical intervention as treatment
Torsion of the GB clinical symptoms
- same as acute cholecystitis
- can mimic cardiac event/symptoms
Torsion of the GB sonographic findings
- Massively inflamed, distended gallbladder
- cystic artery and cystic duct become twisted
- gangrene may develop
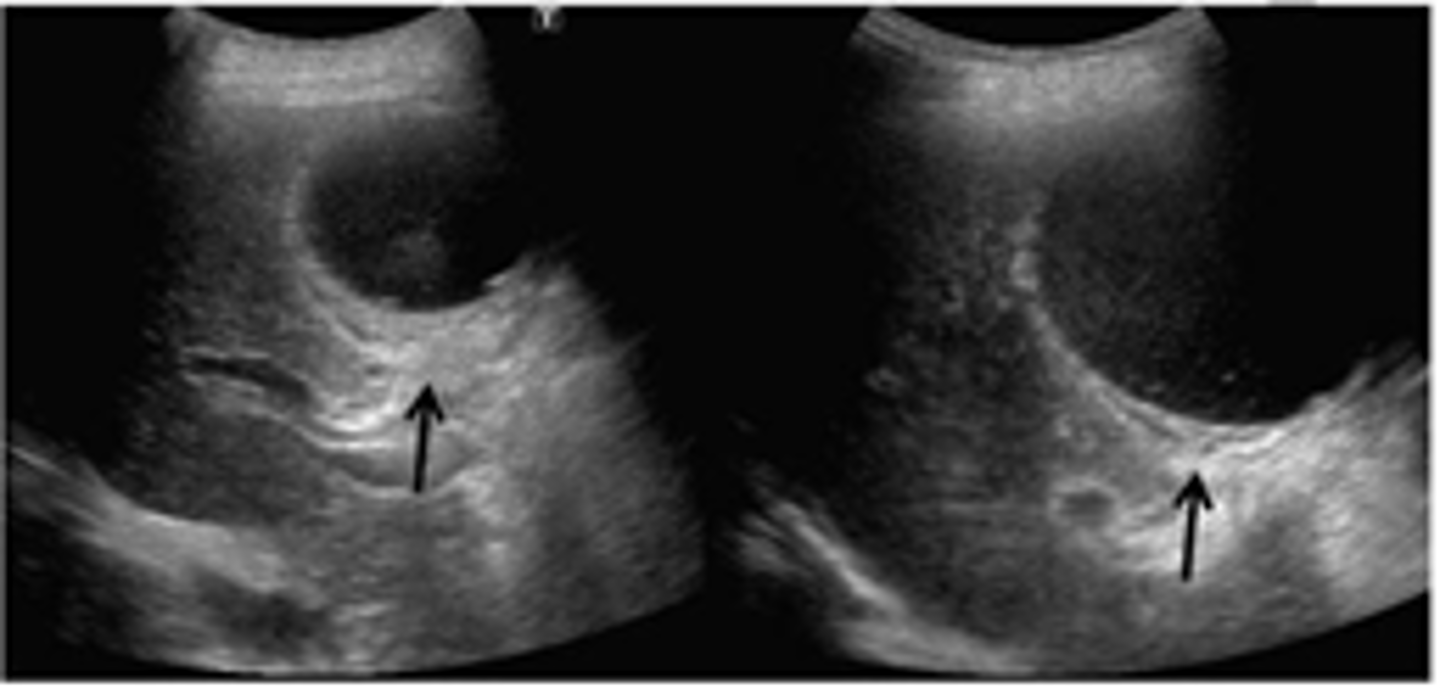
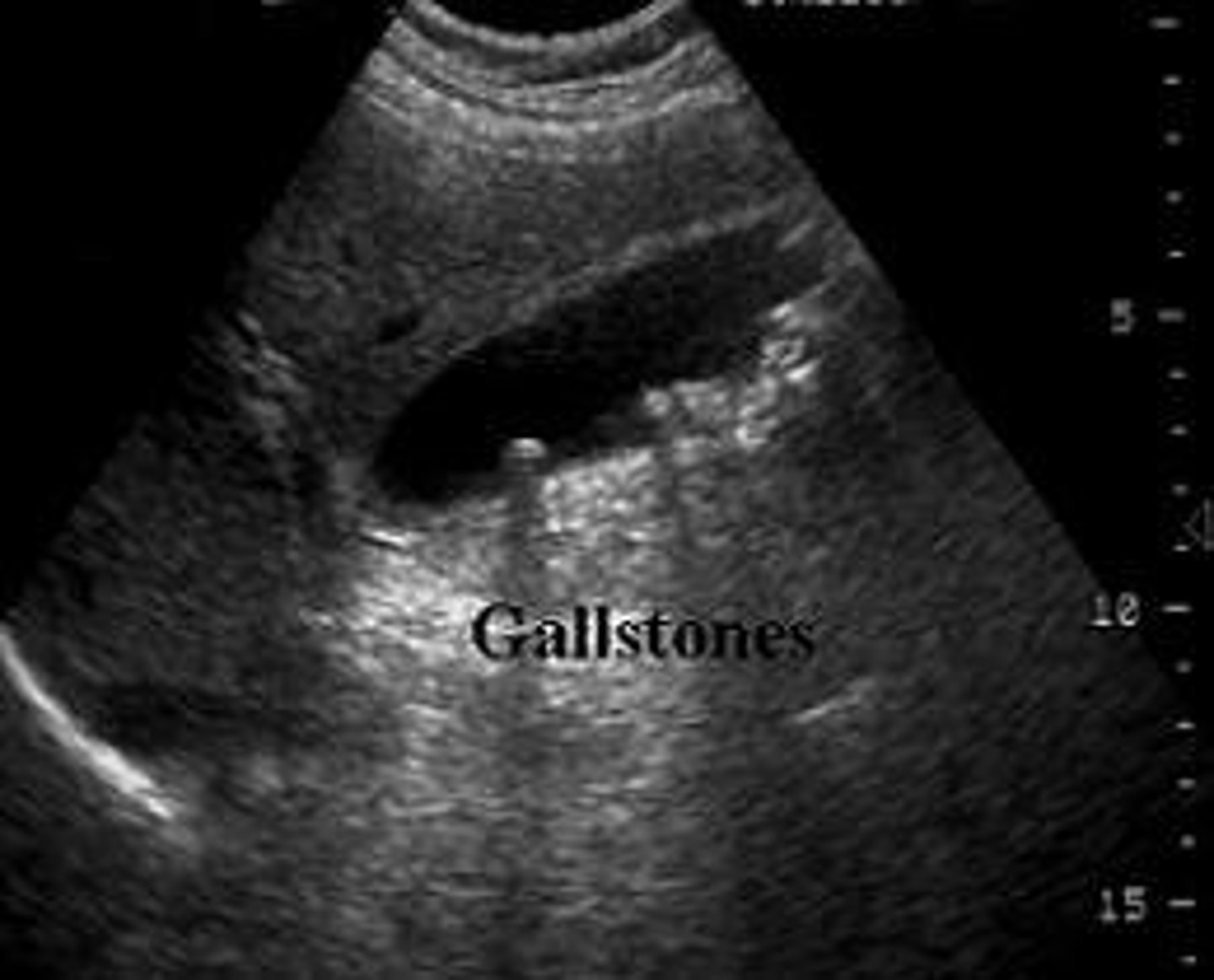
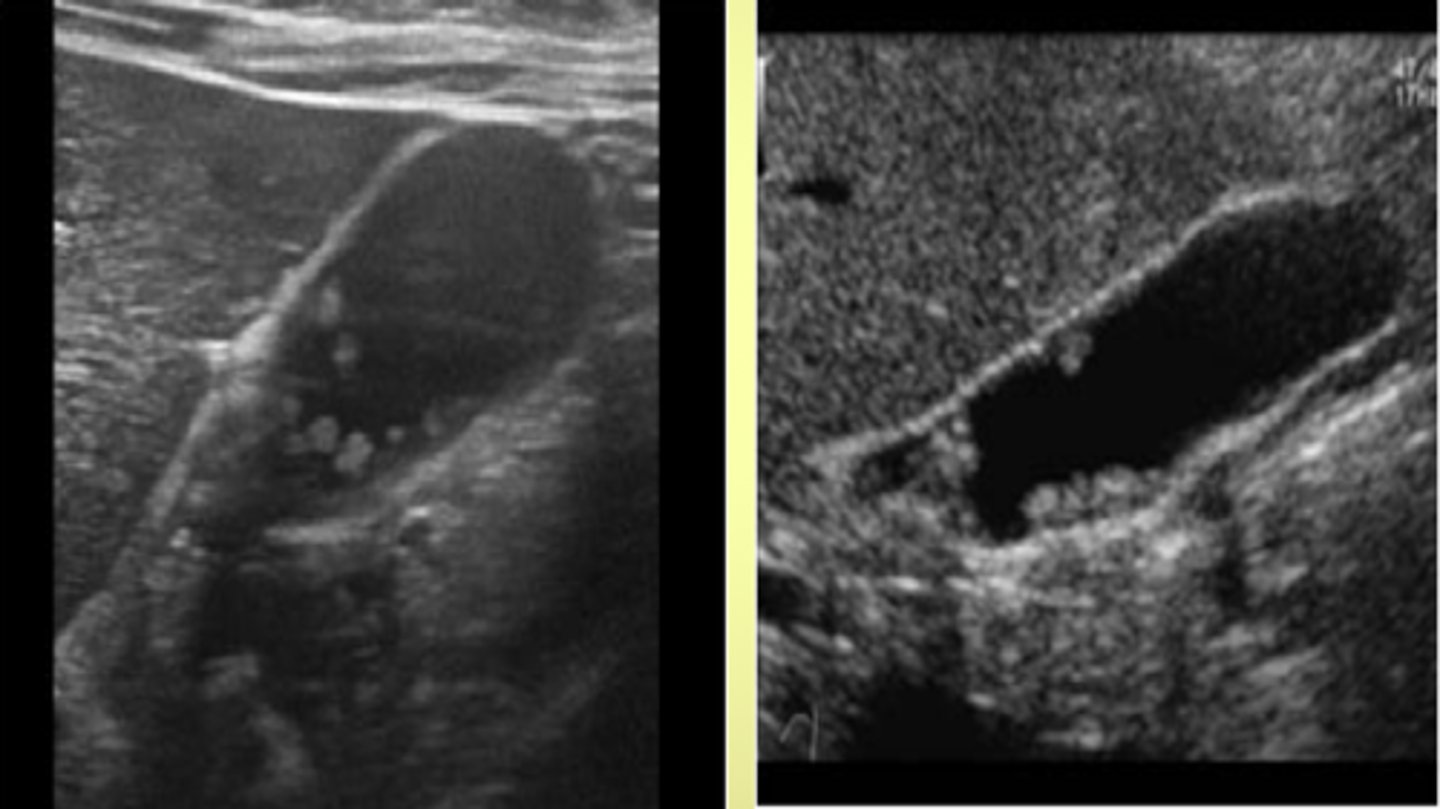
Cholelithiasis
*****MOST COMMON DISEASE OF GB*****
- biliary stones found in the GB are called gallstones
gallstones consist of:
cholesterol
calcium bilirubinate
calcium carbonate
6 F's of cholelithiasis
fat, female, fertile, flatulent, fair, forty
Who is at increased risk for developing gallstones?
pediatric patients with hemolytic anemia (sickle cell disease) and patients with Crohn's disease
Risk factors for developing gallstones (not six F's)
pregnancy, diabetes, oral contraceptives, diet-induced weightloss, total parental nutrition
Cholelithiasis clinical symptoms
-may be asymptomatic
-biliary colic (pain in RUQ around GB) once obstruction occurs
-abdominal pain after fatty meals
-epigastric pain
-nausea and vomiting
-pain radiates to shoulders
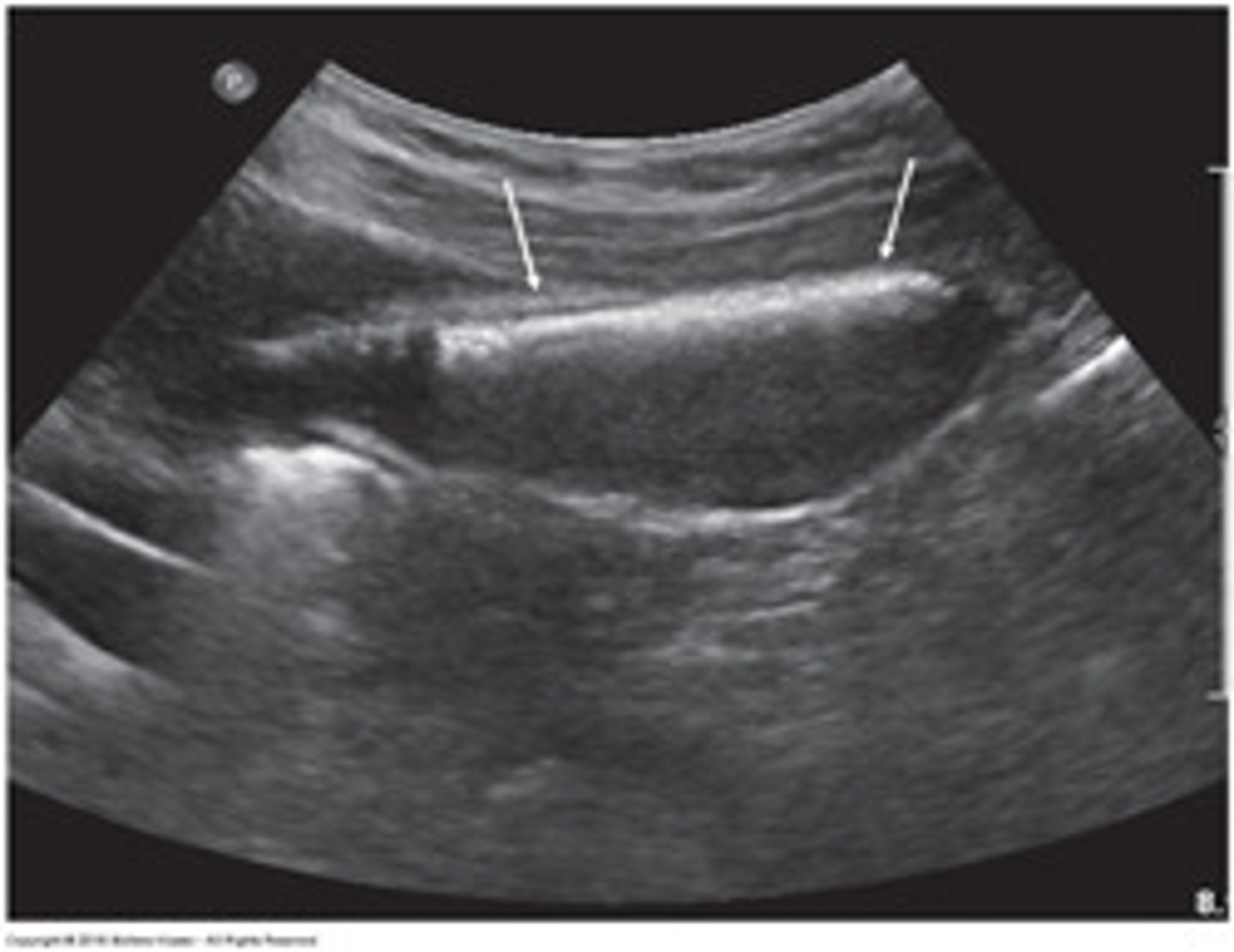
Cholelithiasis sonographic findings
- mobile, echogenic structure within GB lumen that produces posterior shadowing
-WES sign if completely filled with stones
-change in patient position that shows movement
-some stones may adhere to the wall and not cause shadow- twinkle artifact may be used to differentiate b/w a small stone and polyp:
-twinkle occurs posterior to a strong, granular surface like crystals or calcifications
porcelain gallbladder
- results from the calcification/incrustation of the gallbladder wall
-associated with gallstones and chronic cholecystitis
-found in elderly females
-potential for increased risk of GB carcinoma
porcelain gallbladder clinical symptoms
asymptomatic
porcelain gallbladder sonographic findings
-bright echogenic echo with posterior shadowing,
-no WES sign just the "ES"- echo and shadow only
-Identifing calcification of the posterior GB wall is helpful to differeniate porcelain BG from WES sign.
if it was WES sign the posterior wall would be shadowed out!
hyperplastic cholecystosis
a group of proliferative and degenerative gallbladder disorders which includes both adenomyomatosis and cholesterolosis
cholesterolosis (aka polyps)
- Results from the disturbance in cholesterol metabolism & accumulation of cholesterol typically within a focal region of the GB wall.
- May be diffuse = strawberry gallbladder.’
Polyps are often seen w Cholesterolosis:
- small, well-defined projections from the GB wall
-attached to the wall by a stalk
-if over 10 mm has the potential to be malignant
cholesterolosis clinical symptoms and sonographic findings
clinical symptoms = asymptomatic
Sonographic:
-hyperechoic, non-shadowing, non-mobile mass that projects from GB wall into GB lumen ("ball on the wall")
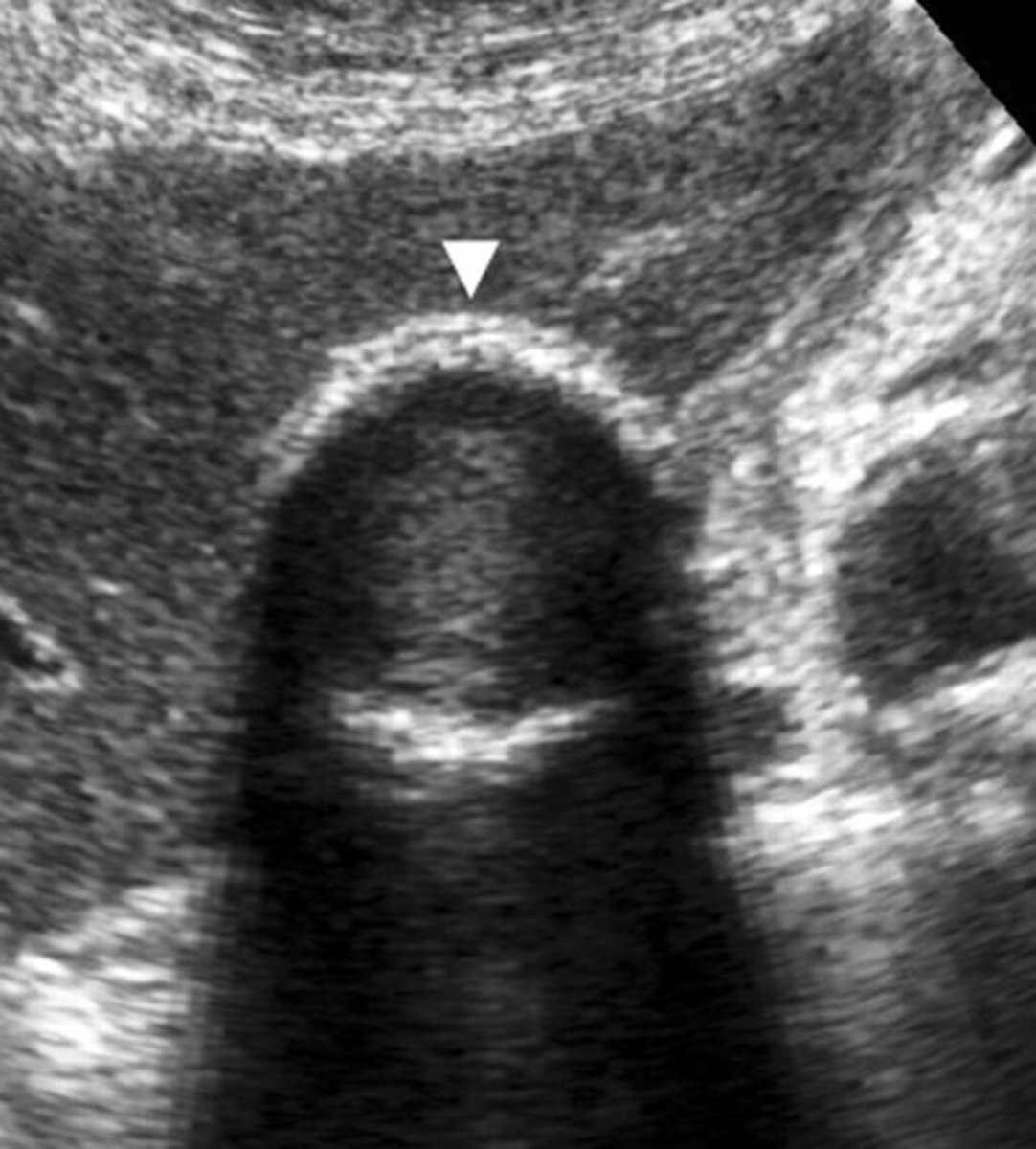
adenomyomatosis
- a hyperplastic change in the GB wall (polyp projection, no stalk)
- may be focal or diffuse
- the condition of glands within the muscle of the gallbladder
- muscular layer becomes thickened producing diverticuli or tiny pockets called Rokitansky-Aschoff sinuses
*the sinuses contain cholesterol crystals that produce comet-tail artifact seen protruding into the GB from the ANTERIOR wall*
Adenomyomatosis clinical symptoms and sonographic findings
-asymptomatic
-small, echogenic foci seen in GB wall with comet tail/reverberation artifact seen posterior
-no movement with change in patient position
Gallbladder enlargement
- GB should not exceed 4 to 5 cm in width
- trans measurement more indicative of enlargement
-caused by blockage of cystic duct or other parts of the biliary tree
- aka hydropic gallbladder or mucocele
Gallbladder enlargement clinical findings
-asymptomatic or
-epigastric pain
-nausea and vomiting
-palpable GB on physical examination
-painless jaundice
-possible elevation of ALP, ALT, GGT, and bilirubin (w/ obstruction)
Gallbladder enlargement sonographic findings
- GB measure over 4 to 5 cm width or 8-10 cm length
- look for obstructive entities such as choledocholithiasis (stones in ducts) or pancreatic mass
gallbaldder carcinoma
-rare
-caused by chronic inflammation of the GB wall by stones
-associated with gallstones in 80-90% of cases
-mass may contain gallstones
- tumor arises in BODY of GB
-mass most often fills the entire GB!!!
Who is at an increased risk of developing gallbladder carcinoma?
patients with chronic cholecystitis and women 60+