6 BORELLIOSES AND OTHER VECTOR-BORNE INFECTIONS
1/23
Earn XP
Description and Tags
contagious
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
What bacteria cause Lyme disease?
Borrelia burgdorferi sensu lato complex (including B. burgdorferi sensu stricto, B. garinii, B. afzelii)
= Borelliosis
Burg(er) D’Or Ferry
Which hosts are affected by Lyme disease?
Ruminants, horses, carnivores, birds, humans (all except pig ??)
What are the primary reservoirs for Lyme disease?
Small rodents and birds
How is Lyme disease transmitted?
Via ticks (Ixodes genus), including I. ricinus (EU), I. persulcatus (China), I. scapularis (North America), I. pacificus (West USA), through transtadial and transovarial transmission
Can Lyme disease be transmitted transplacentally?
Yes, possible transplacental transmission
What is the life cycle of Lyme disease vectors?
1st host: larvae → nymph (infection from reservoir host)
2nd host: nymph → imago (high transmission)
3rd host: imago → adult (high transmission)
What is the pathogenesis of Lyme disease?
after tick bite the bacteria migrate from tick midgut to salivary glands, Bacteria penetrate the skin, replication in the dermis near bite site, and transport via blood/lymph (systemic spread)
Preferential localizations are joint and kidney (Formation of immunocomplexes affecting joints and kidneys)
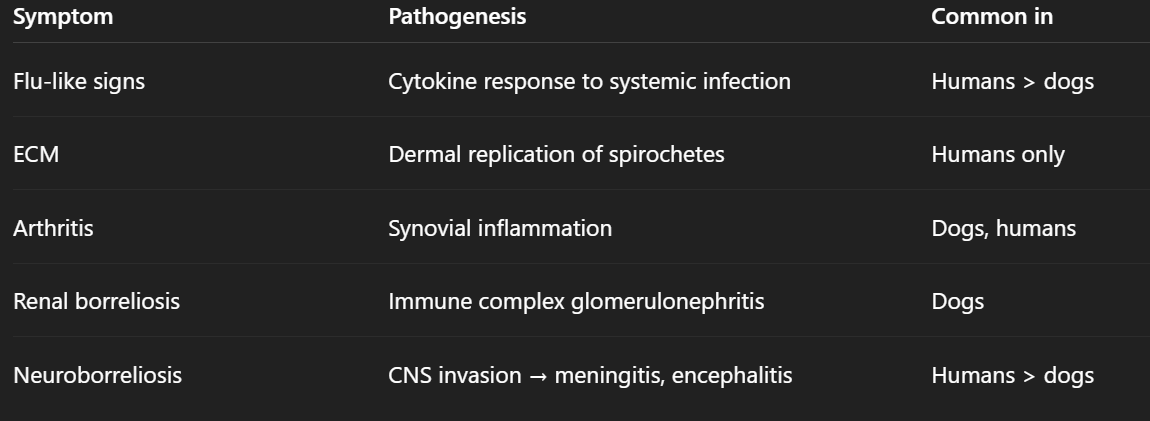
What are the clinical signs of Lyme disease?
Influenza-like symptoms, erythema chronicum migrans, joint degeneration and pain, renal borreliosis (glomerulonephritis), neuroborreliosis (meningitis, encephalitis)
What are Lyme disease symptoms in dogs?
Lymphadenomegaly, swollen painful joints, polyarthritis, lameness
How is Lyme disease diagnosed?
Isolation from blood, urine, CSF on Barbour-Stoner-Kelly II medium, antigen detection via dark-field microscopy or PCR, antibody detection via ELISA, indirect IFA
What cross-reactions must be considered in Lyme disease diagnosis?
Leptospira, Treponema, Borrelia species
What is the treatment for Lyme disease?
Antibiotic therapy (Penicillin, Doxycycline for 30 days PO or IV if CNS symptoms), symptomatic analgesics, antiflogistics
What bacterium causes tularemia?
Francisella tularensis
What are the subspecies of Francisella tularensis?
Type A (F. tularensis tularensis) affects humans and rabbits in North America
Type B (F. tularensis palaearctica) affects aquatic rodents in North America, hares, and small rodents in North Eurasia
Epizootologycal calssification (Susceptibility and Sensitivity Classification)
1) Highly susceptible + highly sensitive: Severe disease: septicemia, death within 5–12 days (ex: hare)
2) Highly susceptible, less sensitive : mild CS & chronic carrier (rats, hedghogs, squirrels).
3) Low susceptibility + low sensitivity :Mild or inapparent infections, no significant bacterial shedding. foxes, cat/dog, Ru
—> host species differ in their role as reservoirs or dead-end hosts depending on susceptibility and sensitivity
Which hosts are affected by tularemia?
Ruminants, swine, dogs, cats, humans (no common horse/bird)
Which animals serve as tularemia reservoirs?
Rodents, rabbits, hares
How is tularemia transmitted?
Via tick vectors (Ixodes, Amblyoma, Dermacentor, Haemaphysalis)
What is the pathogenesis of tularemia?
Intracellular bacterium living in macrophages, spreading via the lymphatic system to multiple organs (lungs, liver, spleen), causing systemic failure
What is the mortality rate for different tularemia forms?
Pneumonic and typhoidal forms: 50%
Untreated cases: 7%
Treated cases: 1%
What are the acute clinical signs of tularemia?
Peracute: septicemia (2-3 days post-infection),
Acute: fever, enlarged suppurative lymph nodes and spleen, facial and eye inflammation/cunjuctivitis, lethargy, anorexia, … non specific signs
What are the chronic clinical signs of tularemia?
Sheep: rhinitis, conjunctivitis, paresis
Bov: abortion, inappetence
Swine: cough, polypnea
Dogs: mild fever, decreased appetite
Cats: high fever, lymph node edema
How is tularemia diagnosed?
Agent identification via culture on agar, serology, PCR
What is the treatment for tularemia?
Antibiotics (streptomycin, erythromycin, tetracycline), resistant to penicillin and sulfonamides