Cardiac Physiology
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
Composition of Blood
Nearly half its volume is composed of cells.
The most numerous cells are erythrocytes (red blood cells)
The remainder of the cells are leukocytes (white blood cells)
Present are platelets, which are not actually cells but rather cell fragments that play an important role in blood clotting. • The liquid portion of the blood, called plasma, is made up of water containing dissolved proteins, electrolytes, and other solutes.
Parallel arrangement of organs in a systematic circuit
Each organ is fed by a separate artery, each receives fully oxygenated blood.
Blood reaches the organs via parallel paths, blood flow to the organs can be independently regulated. Thus, blood flow can be adjusted to match the constantly changing metabolic needs of organs.
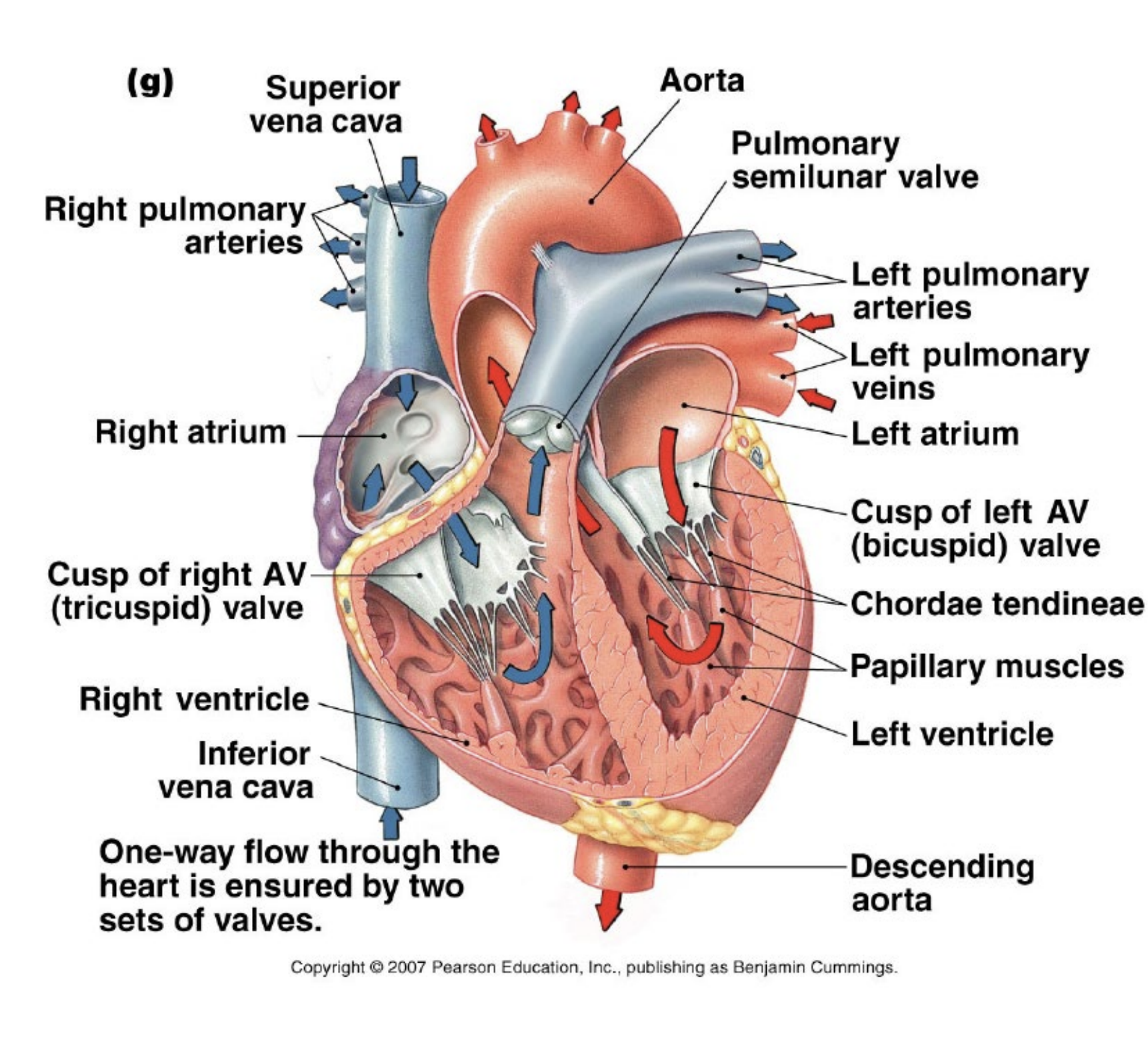
Anatomy of the heart
Atria
Ventricles
AV valves
Semilunar valves
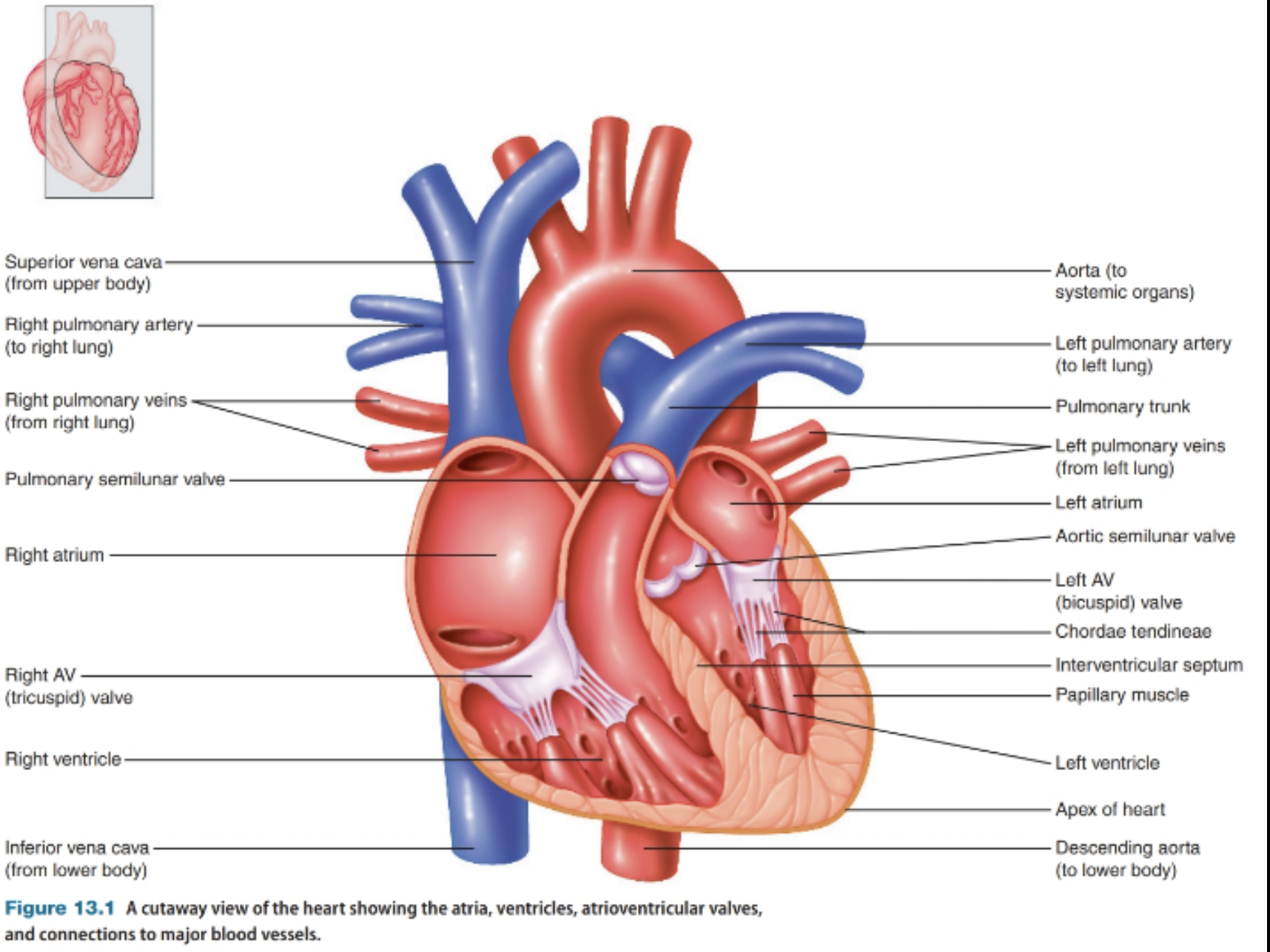
Blood flow through the heart
Right to lungs
Left to body
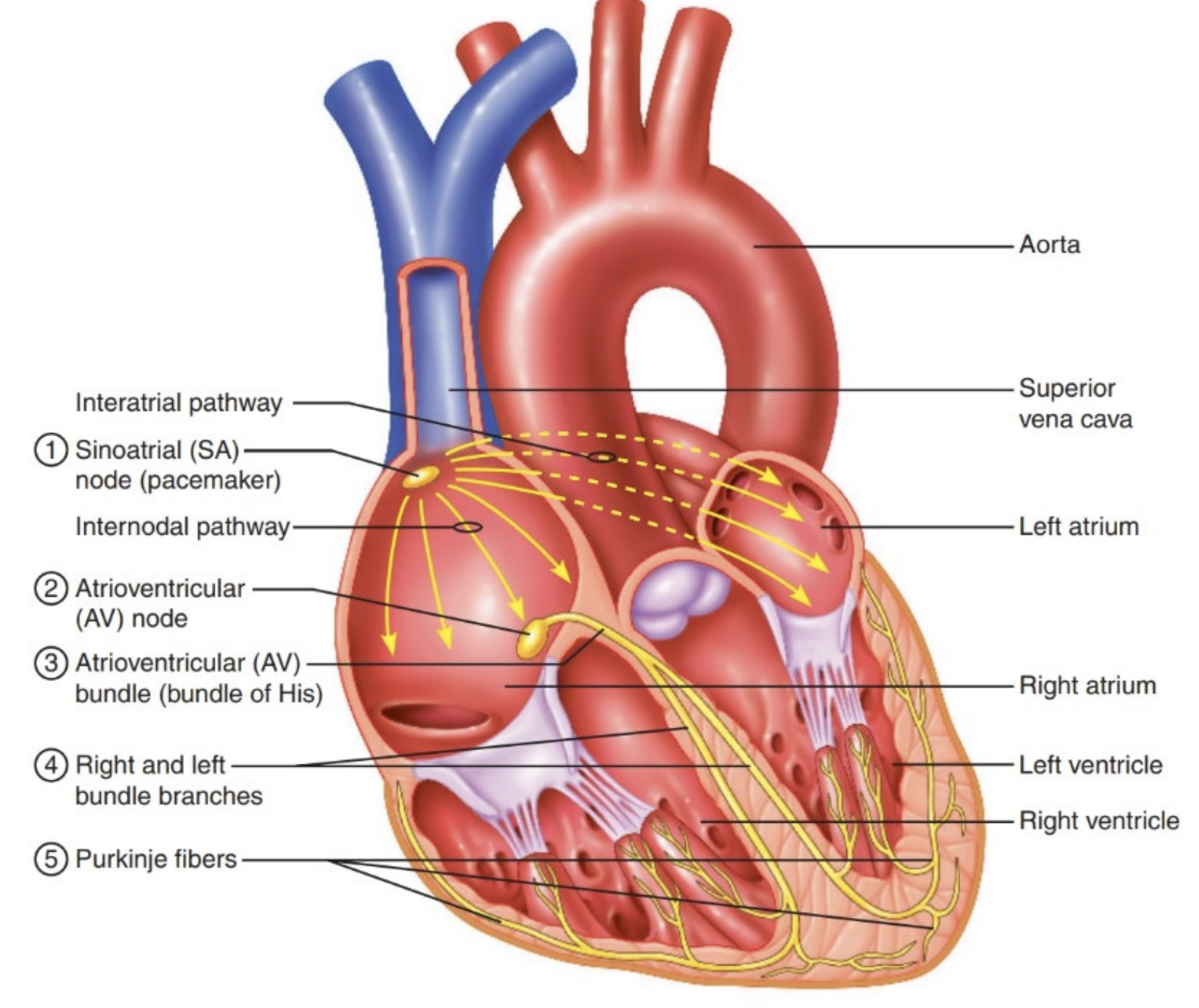
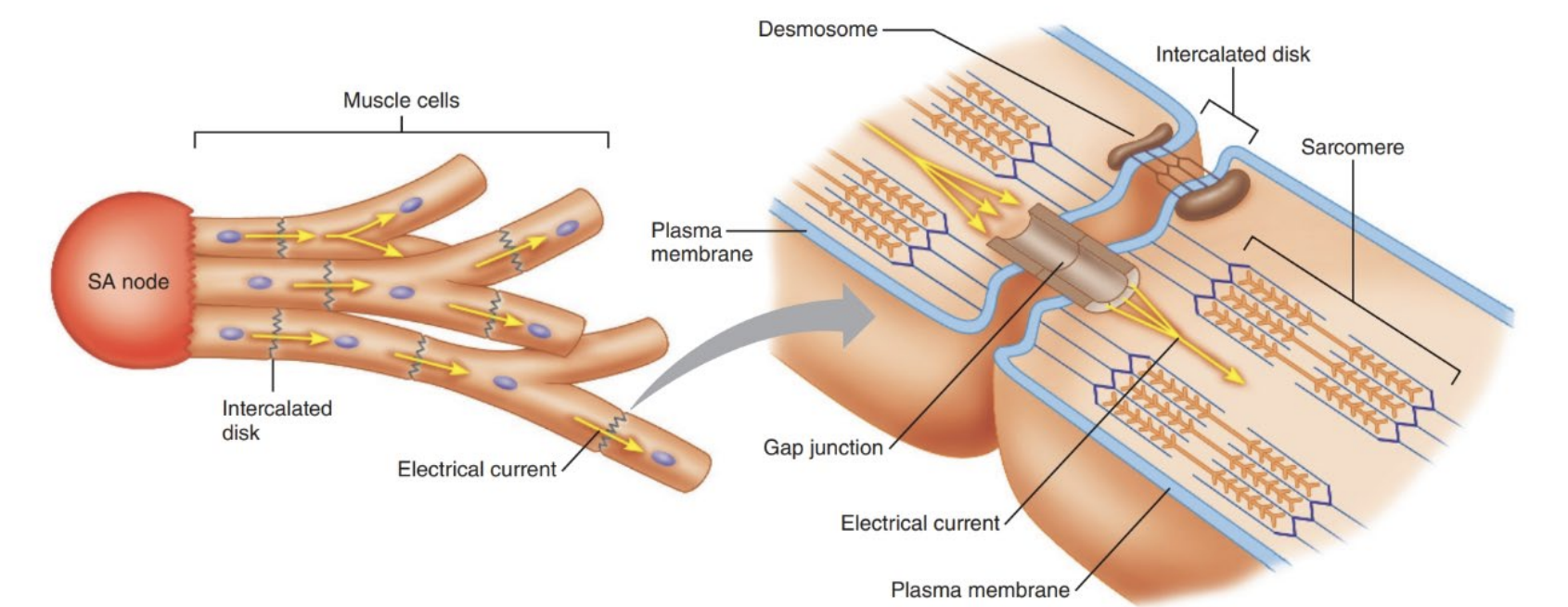
Cardiac Conduction
Contraction of the heart is systole and blood is ejected from the heart. First atria then ventricles contract.
Relaxation of the heart is diastole allowing the atrium and ventricles to fill with blood
Collections of specialised pacemaker cells (nodes) drive the heart beat. (sinoatrial node to AV node to AV bundle to right and left branches (bundle of His.) to purkinje fibres)
Specialised Cardiac Muscle Fibre Cells
Purkinje fibres and the bundle of HIS
Autorhythmic cells generate little contractile force but coordinate and provide rhythm to the heartbeat (pacemaker cells and conduction fibres)
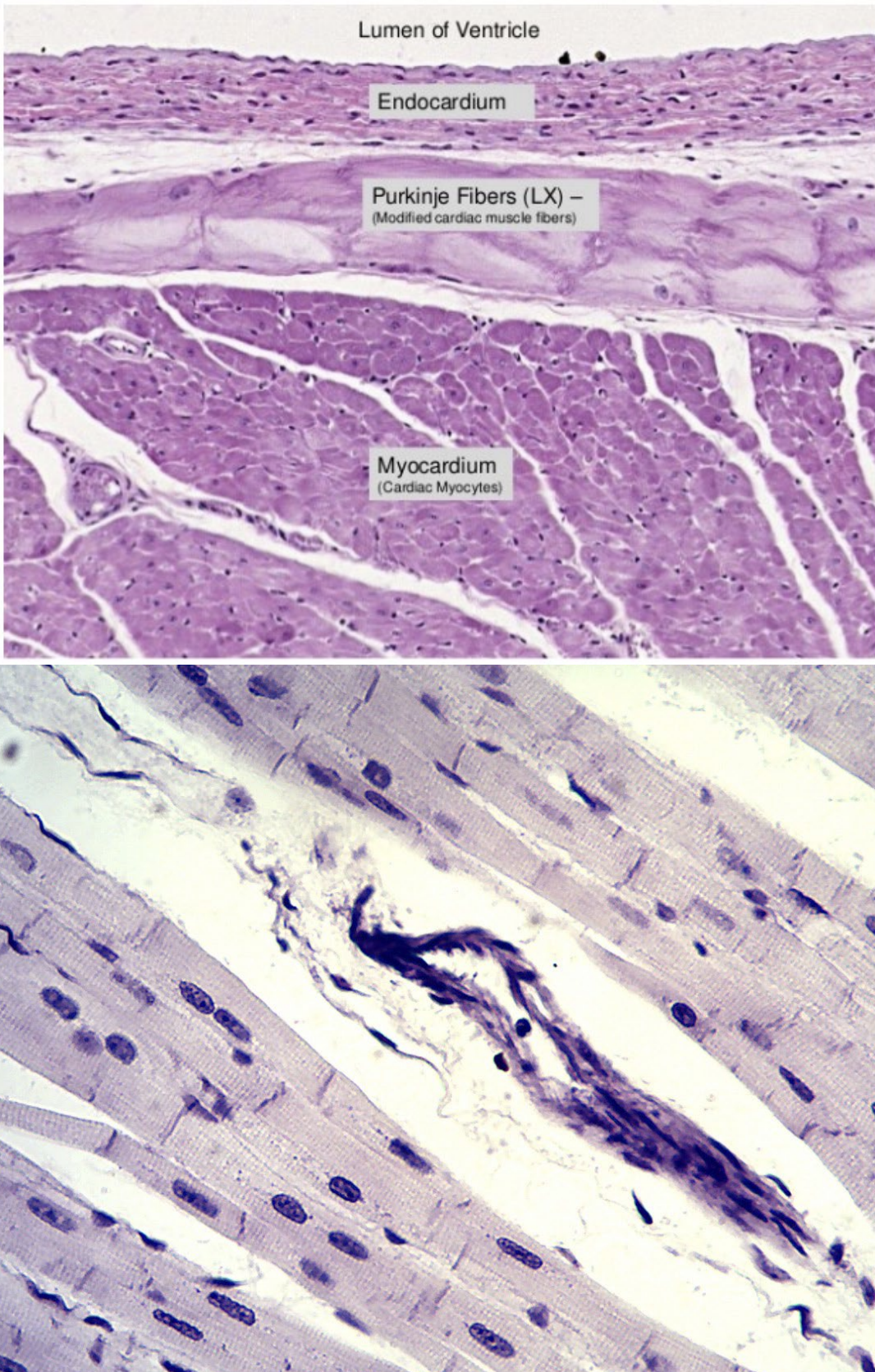
Cardiac Muscle Cells
Contractile cells
Branched
Connected by intercalated discs that have gap junctions that allow muscle AP’s to travel through cardiac muscle.
Larger diameter to conduct AP’s faster
Stable resting potential of 90mV and only depolarise when stimulated
At threshold (-70mV)
Na channels open causing depolarisation
Slow Ca channels open causing a slow and steady influx at -40mV
Near the peak Na channels close and K channels open
Small decrease in membrane potential called early repolarization
Ca and K balance causing plateau (contracts longer) and muscle contraction halfway through.
Ca is transported out and back to SR
Sodium potassium pump restores ionic balance with a longer absolute refractory period to prevent summation and tetnus
What triggers the heartbeat?
Signals originate from the muscle itself - myogenic
Impulse traveling from the AV node to the bundle of His.
Pacemaker Cells
Initiate contractions spontaneously generating AP’s
Usually generate contractions in 2 specific reigions
SA node - 80 AP’s per min - 80 beats per min
AV node
The SA and AV node spontanously generate AP’s at different rates - the SA node (pacemaker) is faster driving depolarisation of the AV node
SA controls heart rate, if damaged other parts may take its role
No true resting potential
Voltage starts at -60mV and spontaneously moves up until the threshold
This is due to funny channels that open when the membrane voltage is less than -40mV and allow slow influx of sodium causing pacemaker potential
At threshold calcium channels open depoalring further.
Spreads to conduction system and contractile myocytes
Cellular Mechanisms
Resting potential is the potential for K
NS can make the AP go faster or slower but cannot generate them
Pacemaker and contractile myocytes have different forms of AP’s
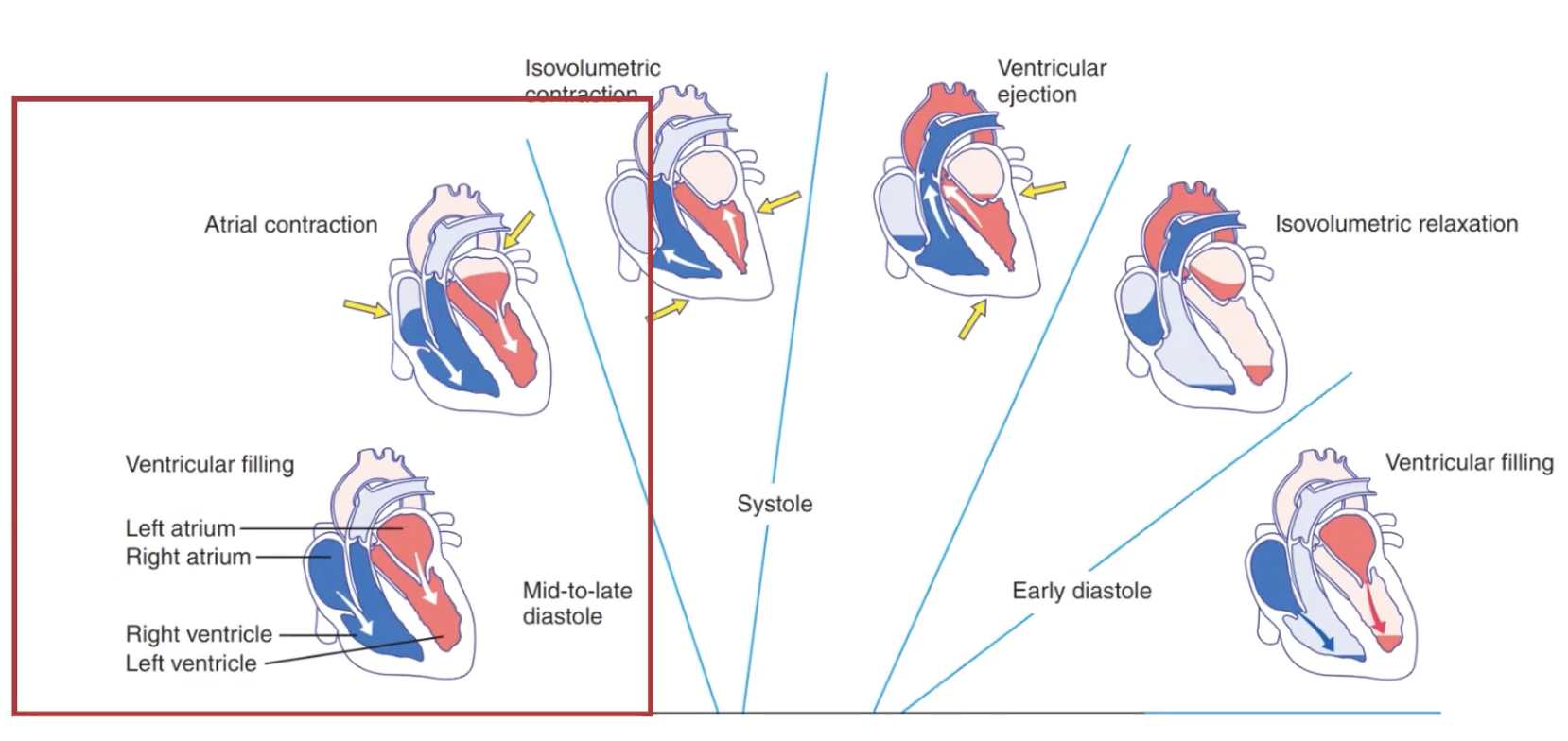
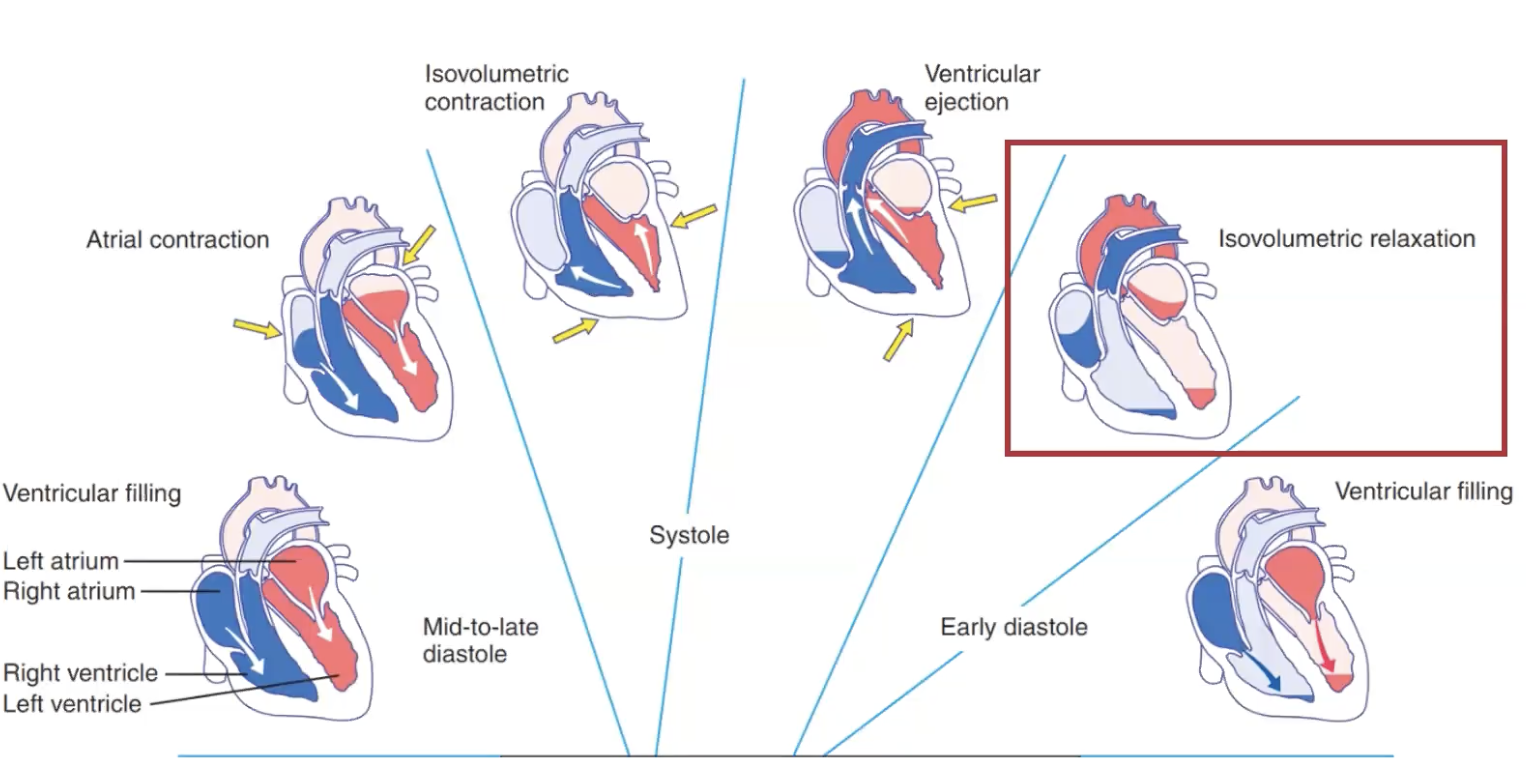
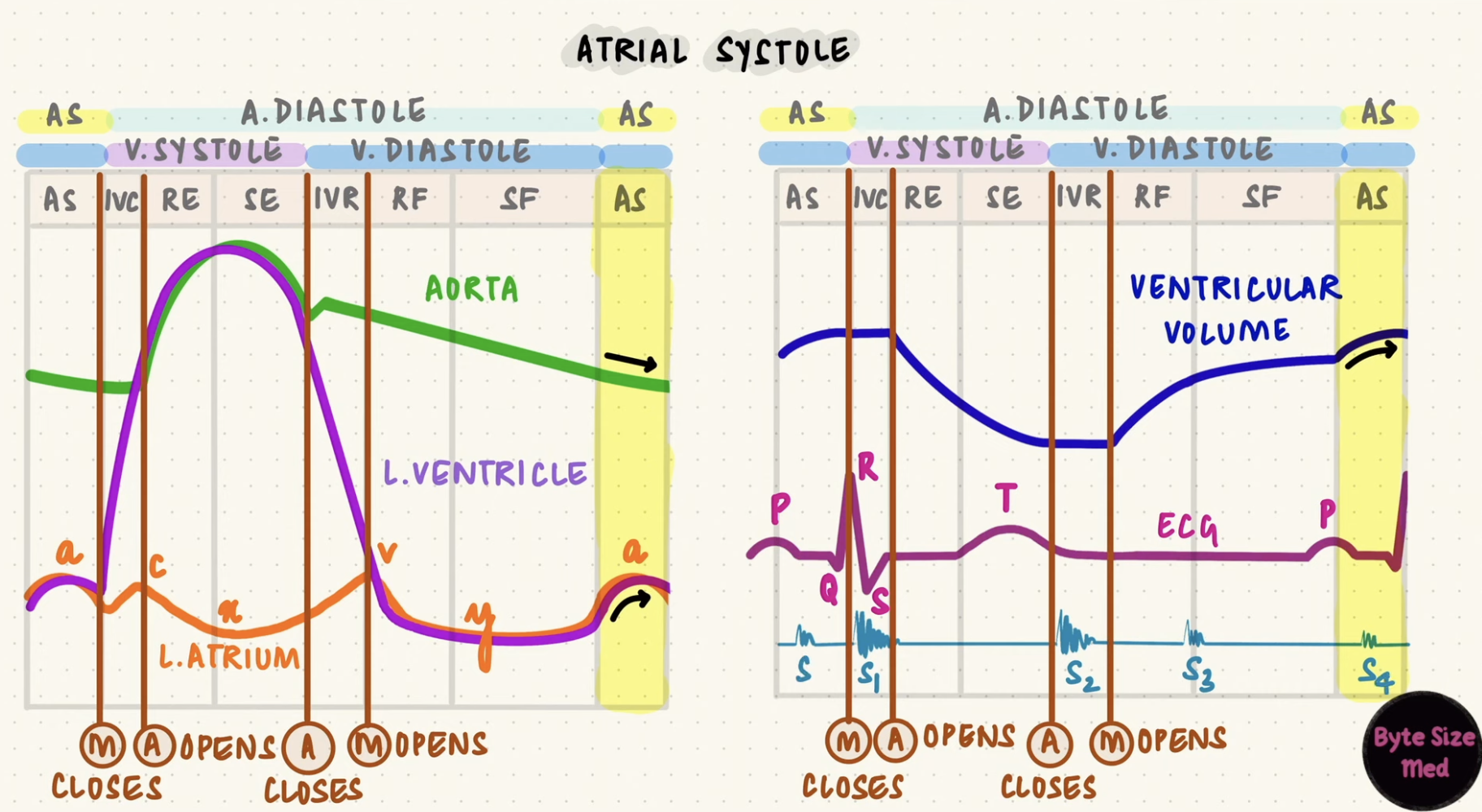
The Cardiac Cycle: Ventricular filling
Mid to late diastole
Blood returns to the heart via systemic and pulmonary veins and enters the relaxed atria.
From there it passes through the AV valves into the ventricles under its own pressure
The return of blood from the veins to the heart - venous return - occurs because the pressure in the veins is greater than that in the atria.
During this time, the pulmonary and semilunar valves are closed because ventricular pressure is lower than the aorta and pulmonary artery pressure.
In late diastole the atria contract driving more blood into the ventricles and the atria relax as systole begins.
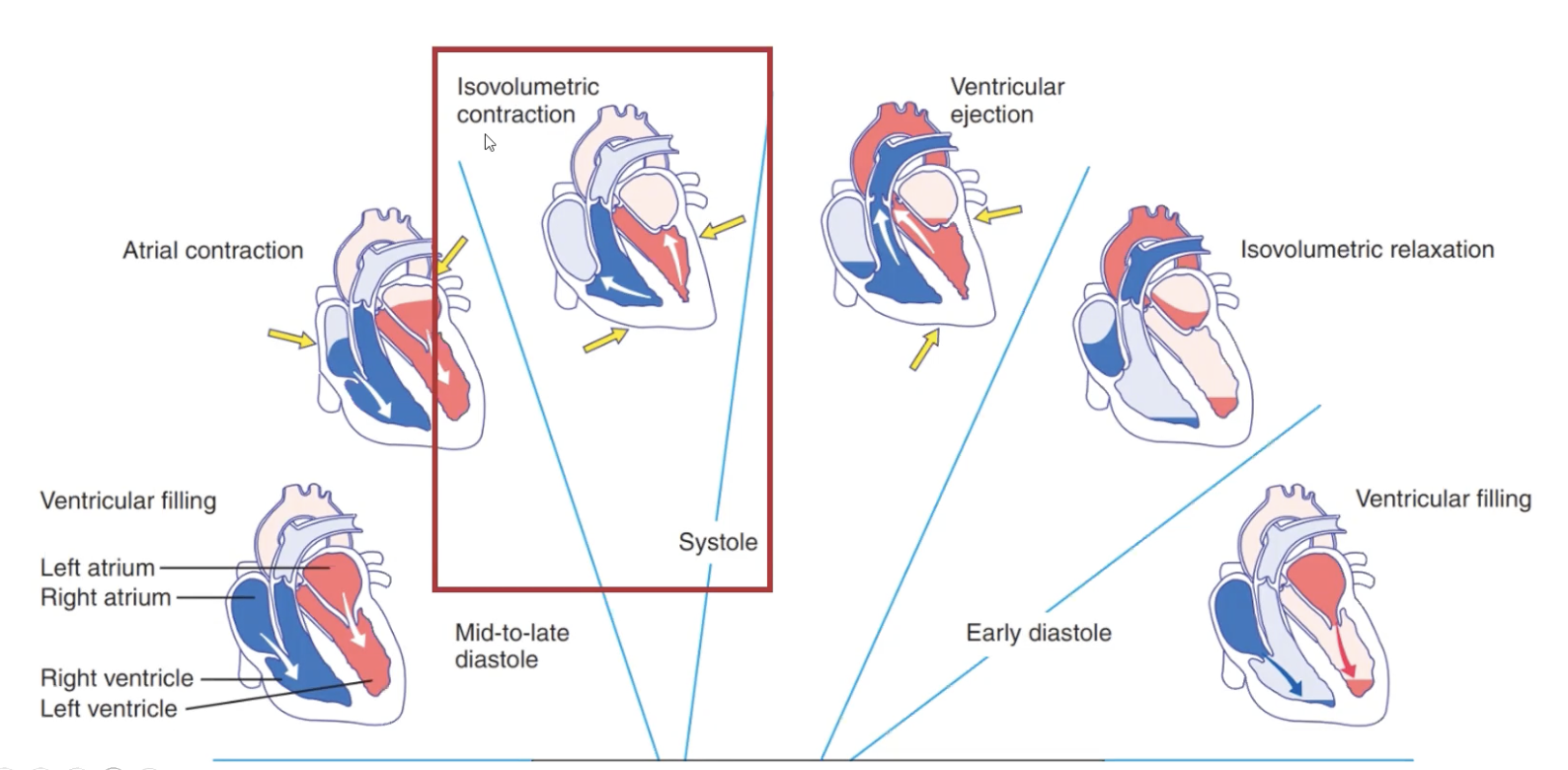
The Cardiac Cycle: Isovolumic Contraction
Ventricles contract raising pressure as the blood stays in
When the ventricular pressue exceeds the pressure in the atria (early systole) AV valves close and semilunar valves remain closed (ventricular pressure isn’t high enough yet)
Ends when ventricular pressure is large enough to force open the semilunar valves so blood can leave the ventricles.
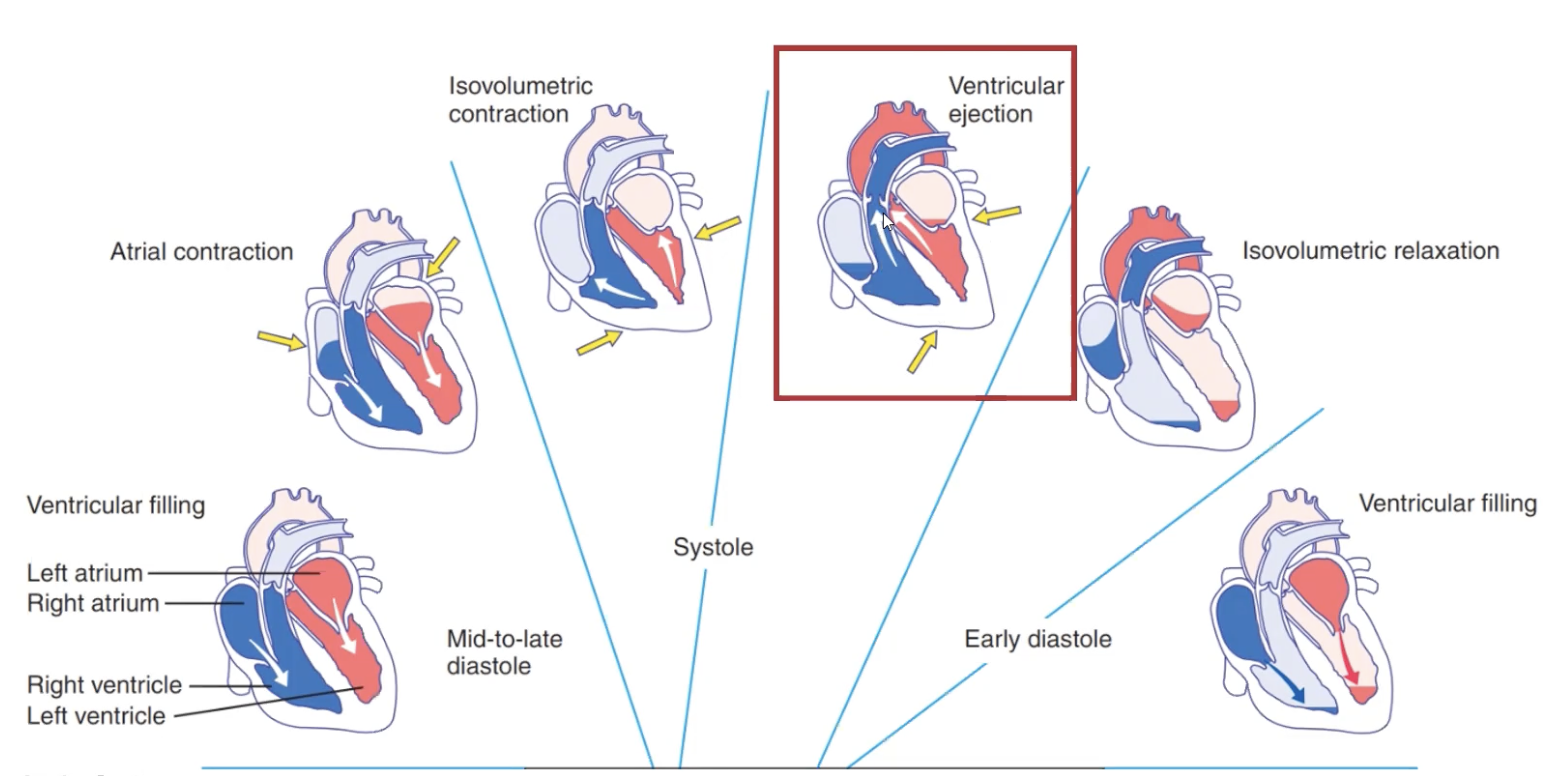
The Cardiac Cycle: Ventricular Ejection
Blood is ejected into the aorta and pulmonary arteries through the semilunar valves
Ventricular volume decreases falling below aortic pressure.
This causes the semilunar valves to close (marks being of diastole as blood is no longer being ejected)
The Cardiac Cycle: Isovolumetric Relaxation
Ventricular myocardium relaxes
Some blood is present in the ventricles under pressure as it takes a long time for the ventricles to relax.
Ventricular pressure is too low for the semilunar valves to remain open and too high for the AV valves to open.
Volume of blood is constant and valves are closed.
Wiggers Diagram
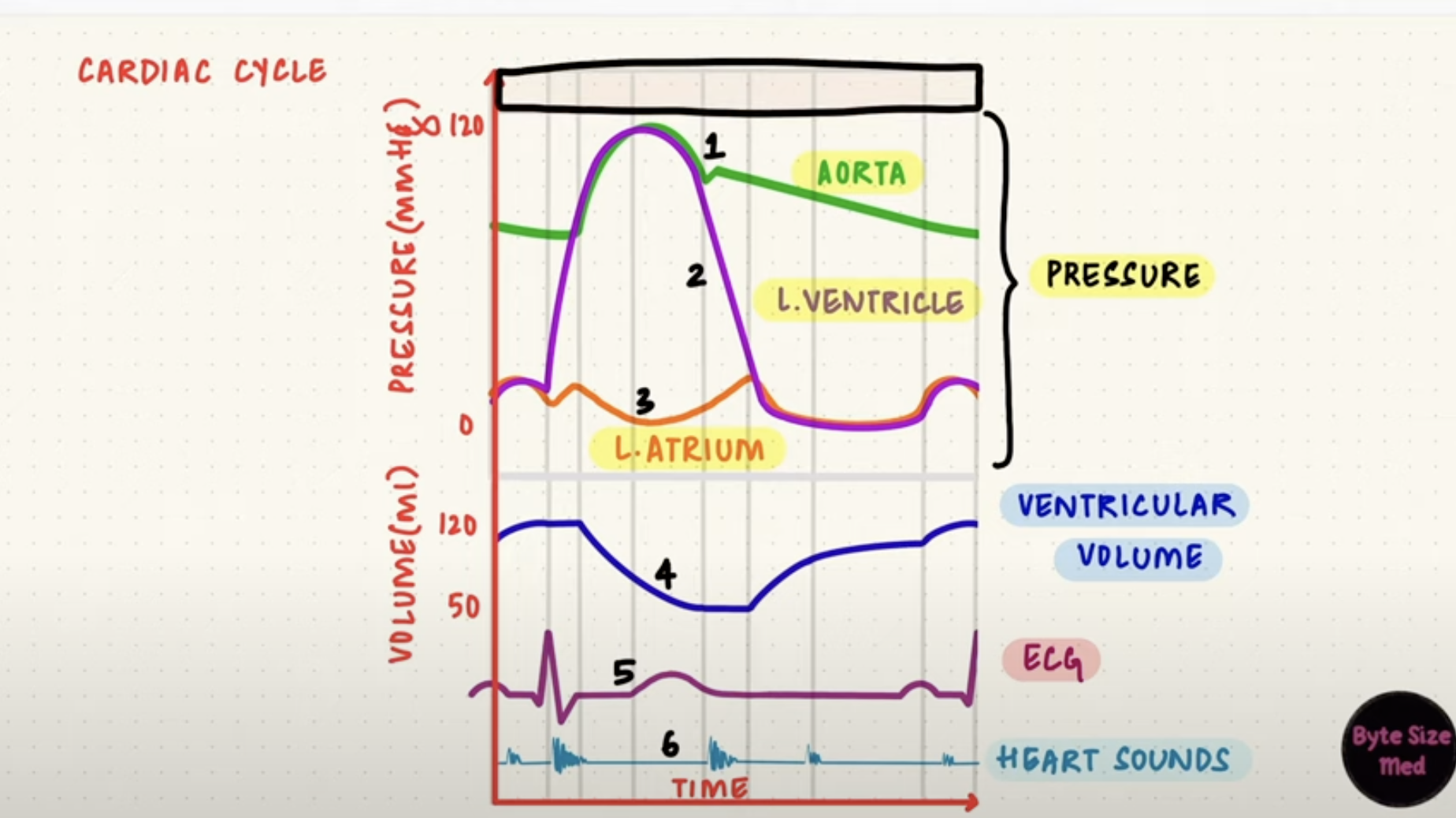
Mean Arterial Pressure (MAP)
Average pressure in the arteries throughout one cardiac cycle.
Cardiac Output x Total Peripheral Resistance
Stroke volume (ml/beat) x HR (beats/min) x Total Peripheral Reistance
Regulated extrinsically via the nervous, renal and endocrine systems.
Detected via atrial baroreceptors
Cardiac Output
Stroke Volume (volume of blood pumped out of each ventricle per min) x Heart Rate
Rate ventricle pump blood (L/min)
Determined by stroke volume and HR
Regulation of Contraction of Cardiac Muscle
Cardiac output
Controlled by intrinsic and extrinsic factors
Intrinsic: Heart, starlings law
Extrinsic: Nervous system and hormones
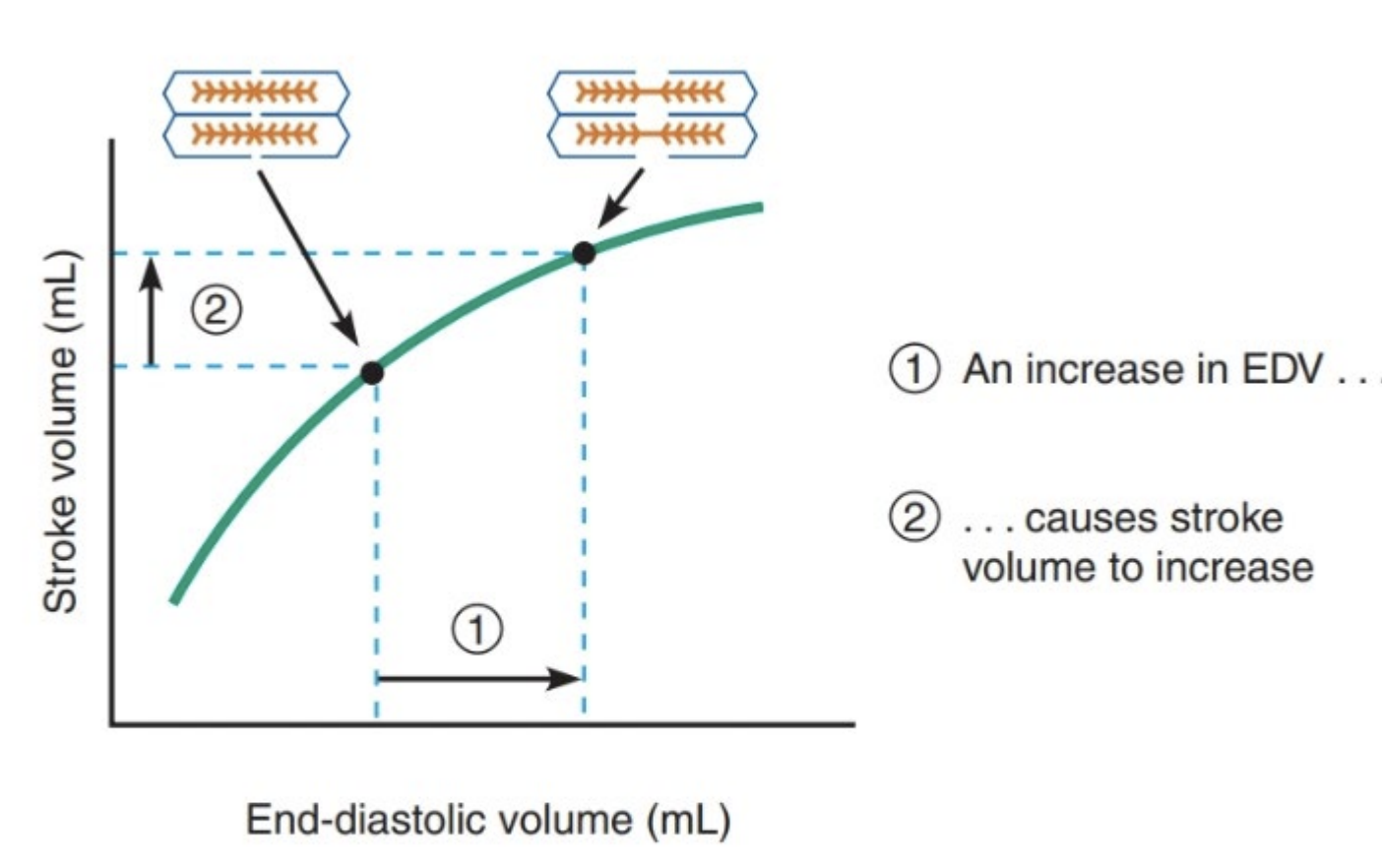
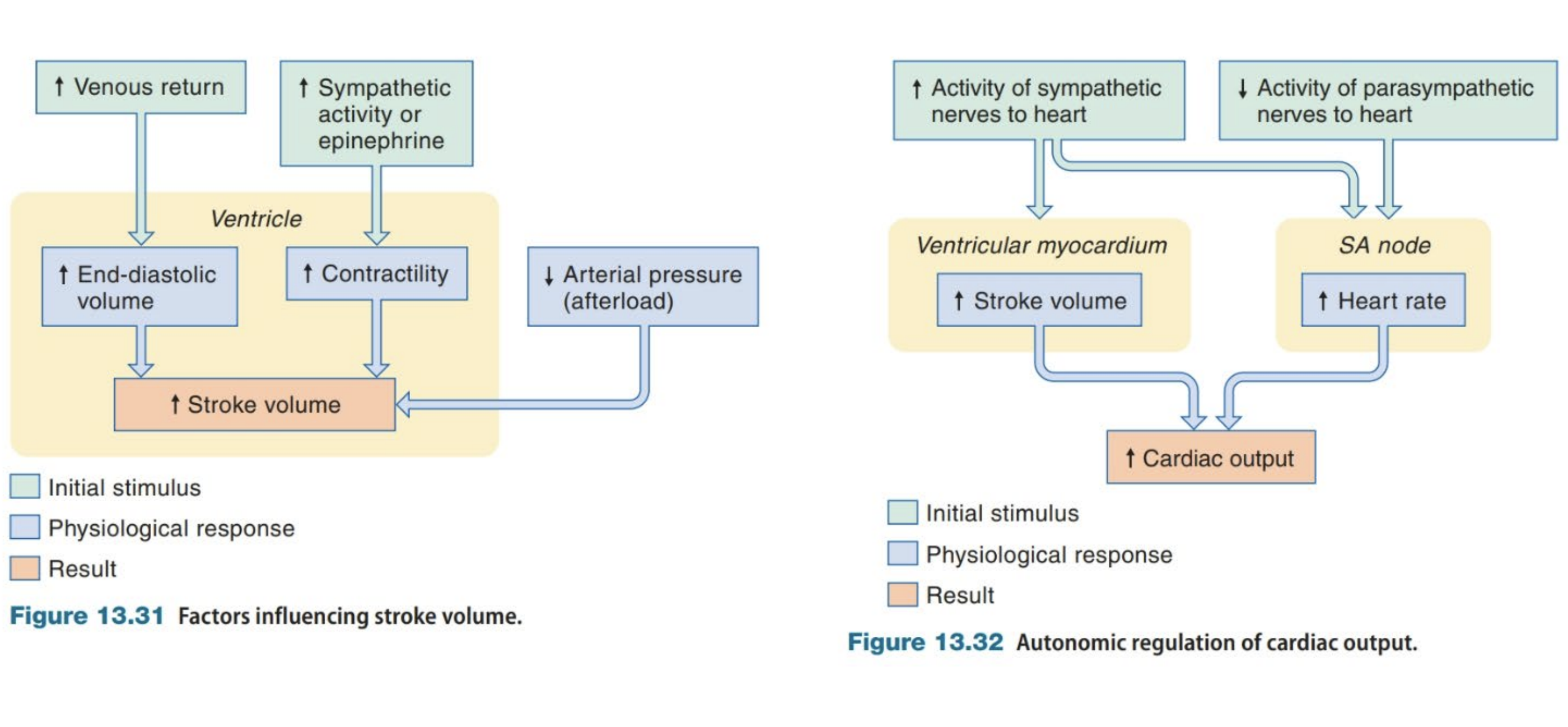
Starling’s Law
Starling’s Law
Stroke volume is proportional to preload (volume of blood in ventricles before contractions) (end diastolic pressure stretches the walls of ventricles to largest dimensions)
Volume ejected = pressure
Greater amount of blood in ventricles increases contractile strength of ventricles increasing stroke volume.
Myocardium is stretched more (more volume) increasing sarcomere length, increased sensitivity to Ca2+, resulting in stronger contractions.
Ensures all blood entering the ventricles is expelled and both sides have the same cardiac output.
Allows the demands of circulation to regulate cardiac output.
Influence of afterload
Afterload is the atrial pressure load on the myocardium after contraction starts.
Stroke volume depends on how large a force it works against (atrial pressure)
When the heart ejects blood ventricular muscle works against atrial pressure
Increase in atrial pressure decreases stroke volume
Decrease in atrial pressure increases stroke volume
Neural Control of the Heart
Medulla provides parasympathetic output to the SA & AV nodes via the vagus nerve
Sympathetic nervous system provides output to SA & AV nodes and ventricular myocardium via the sympathetic cardiac nerve.
Increased activity increases stroke volume
Autonomic nervous system regulates both HR and stroke volume.
Sympathetic Control of Ventricles
Sympathetic neurons trigger AP’s that release noradrenaline in the SA node triggering contractile cells to contract faster and harder in the ventricles
AP’s open funny and T-type Ca2+ channels causing depolarisation of the SA node
They project to the AV node and other parts to influence speed of AP’s
More sympathetic activity increases rate of AP’s decreasing the delay between the atrium and ventricles contracting
Ventricular contraction starts faster and happens faster decreasing systole duration
Critical when HR increases as ventricles are only filled in diastole
Diastole decreases more than systole
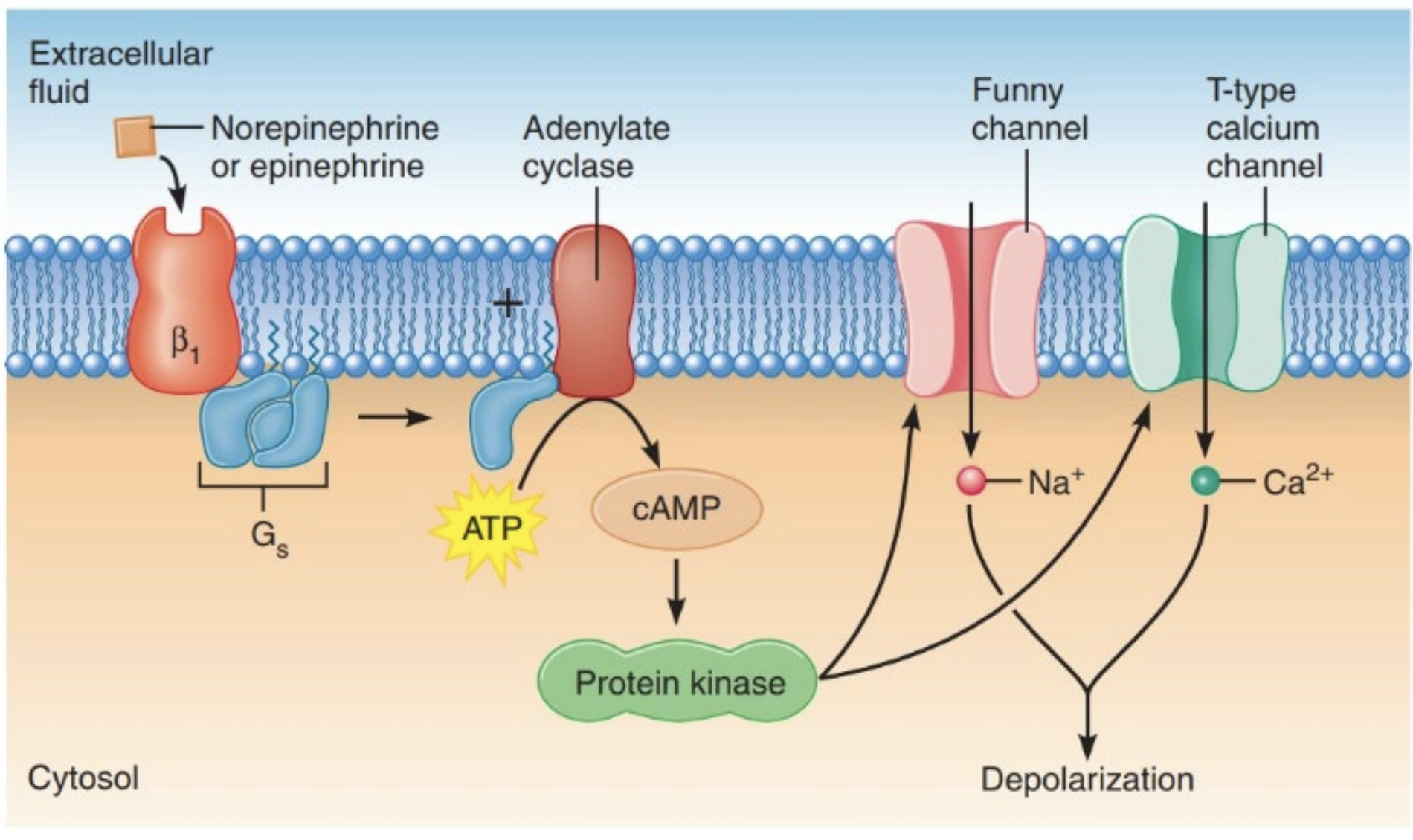
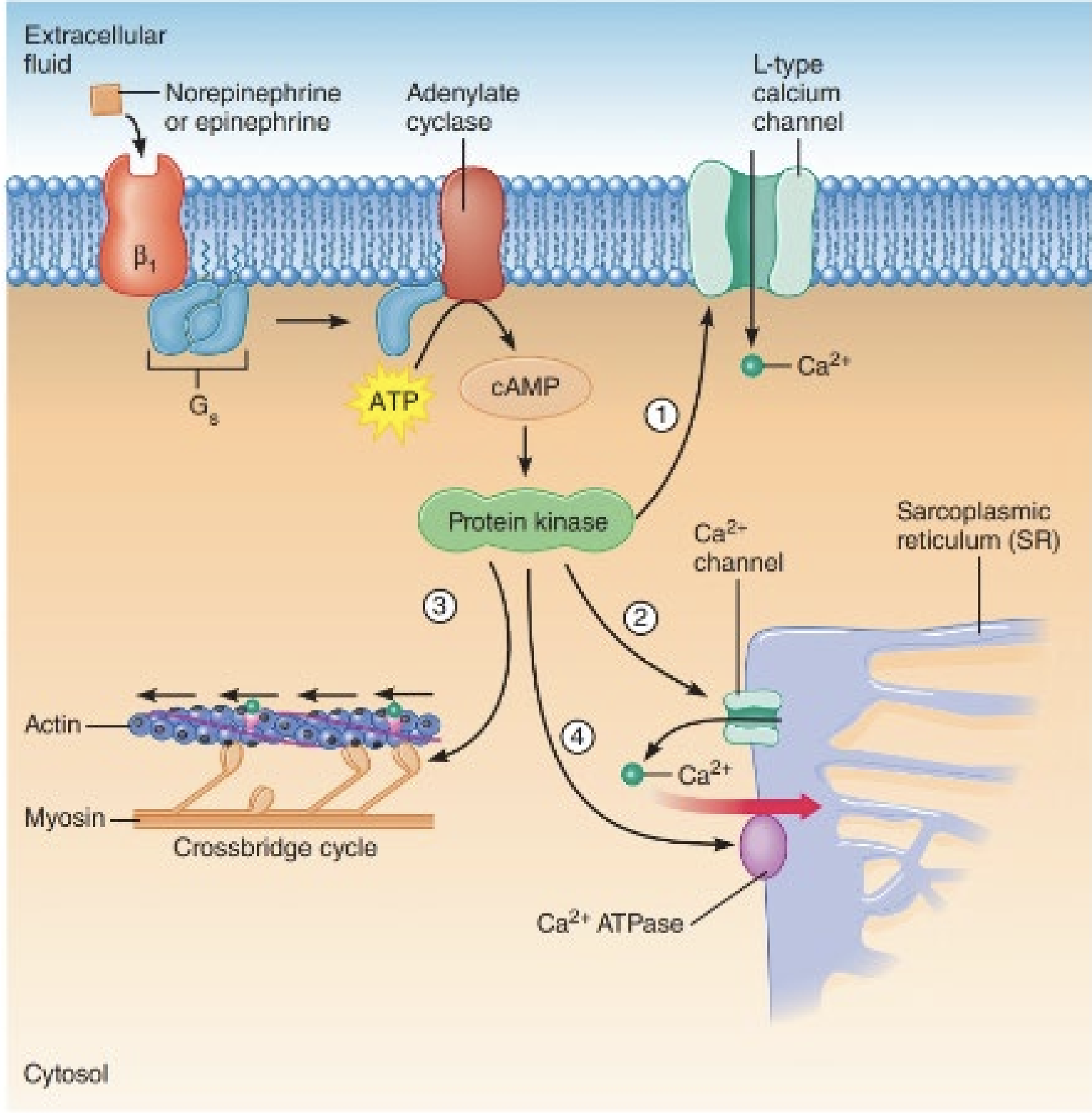
Noradrenaline in the CNS
Sympathetic AP’s release noradrenaline causing a cascade that
Opens Ca2+ channels in the plasma membrane T-type and the sarcoplasmic reticulum
Phosphorylates myosin increasing cross bridge cycling
Activates SR Ca2+ pump, more Ca2+ enters sarcoplasmic reticulum and free Ca falls2+ faster
Cases faster contraction of muscle due to increase calcium ions
Noradrenaline activates G-protein that binds to adenylyl cyclase → ATP → CAMP → Protein kinase →cascade
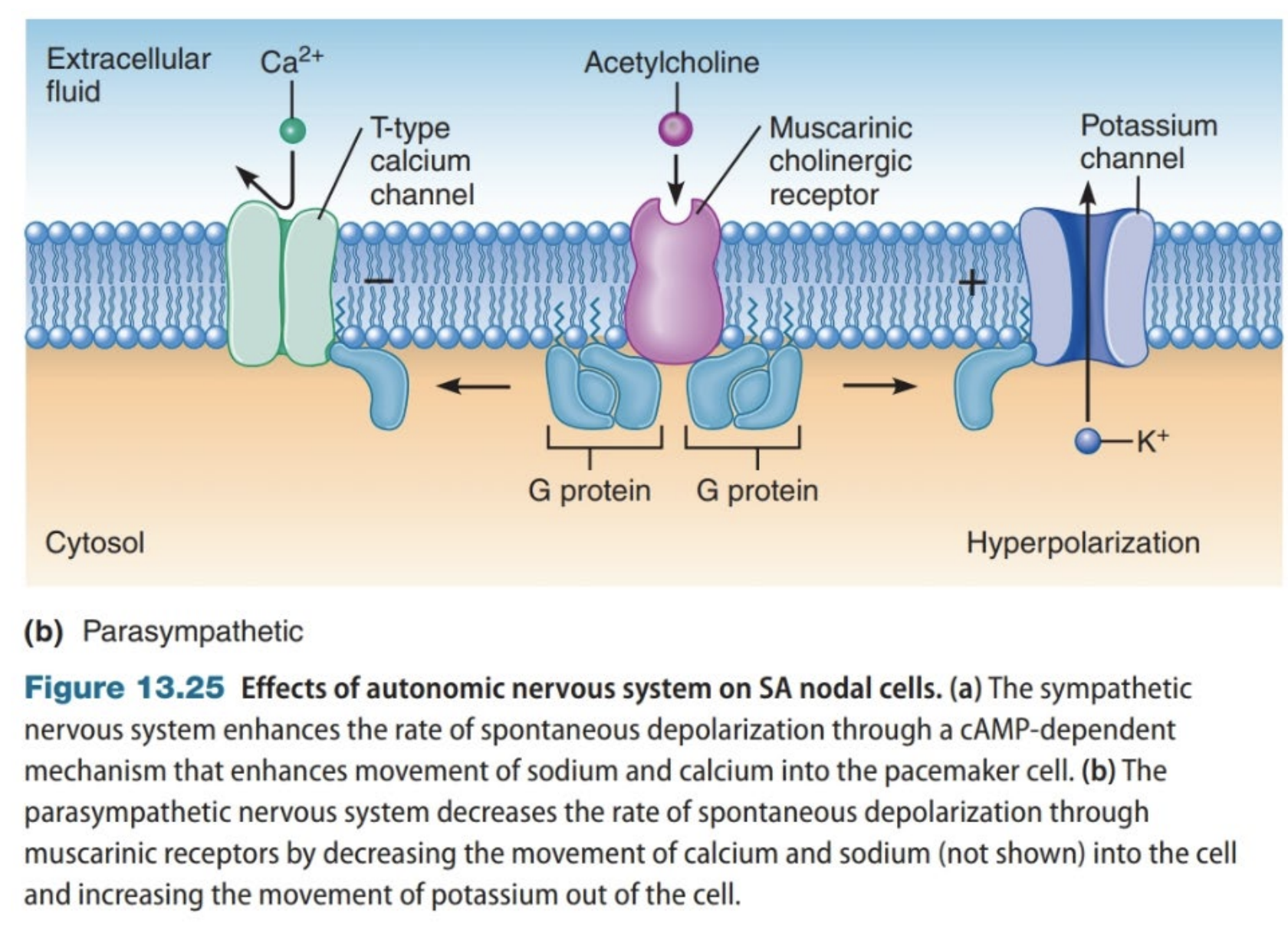
Parasympathetic Regulation of the Nervous System
Effects SA node
Acetylcholine → G-protein → more K+ efflux
Hyperpolarization decreases spontaneous depolarisation.
Regulation of Contraction of Cardiac Muscle
Arterioles
Vary resistance to regulate distribution of blood flow, control total peripheral resistance and blood pressure.
BP = Cardiac Output x Total Peripheral Resistance
Lots of smooth muscle to regulate resistance
Reduces the mean and pulse pressures for exchange in capillaries to prevent damage.
Muscular (smooth muscle) for resistance distribution
Endothelium
Made of epithelial cells that line the cardiovascular system
Secrete vasoactive substances
Express enzymes (ACE & Carbonic Anhydrase) on their luminal membranes
Inner lining.
Smooth Muscle
Relaxes and contracts blood vessels
Connective Tissue
Collagen and Elastin
On the outside for stretch at high pressures
Prevents overexpansion
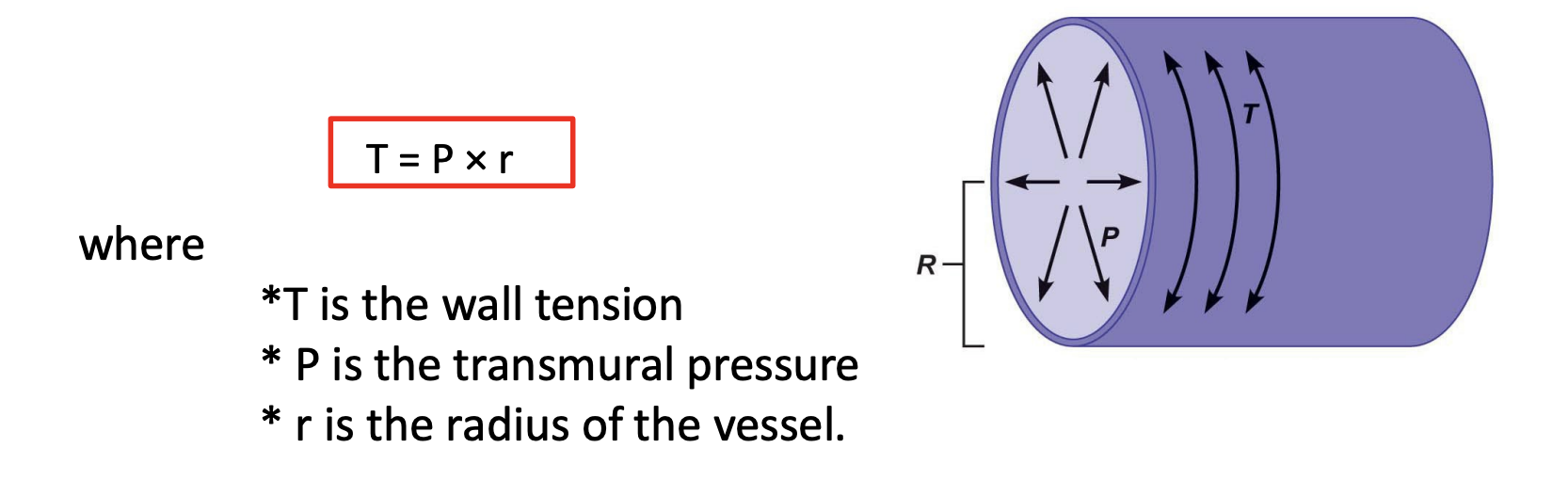
Laplace Equation
T = P X R
Large diameter needs thick wall due to pressure
Determinants of Cardiac Output
Spontaneous AP’s via pacemaker cells in the SA node
Input from autonomic nervous system to SA controls rate AP’s are fired (but heart has its own rhythm)
Intrinsic HR | No input from ANS | 100 bmp |
Resting HR | Parasympathetic input | 55-70 bmp |
HR during stress | Sympathetic input | 130 - 190 bmp |
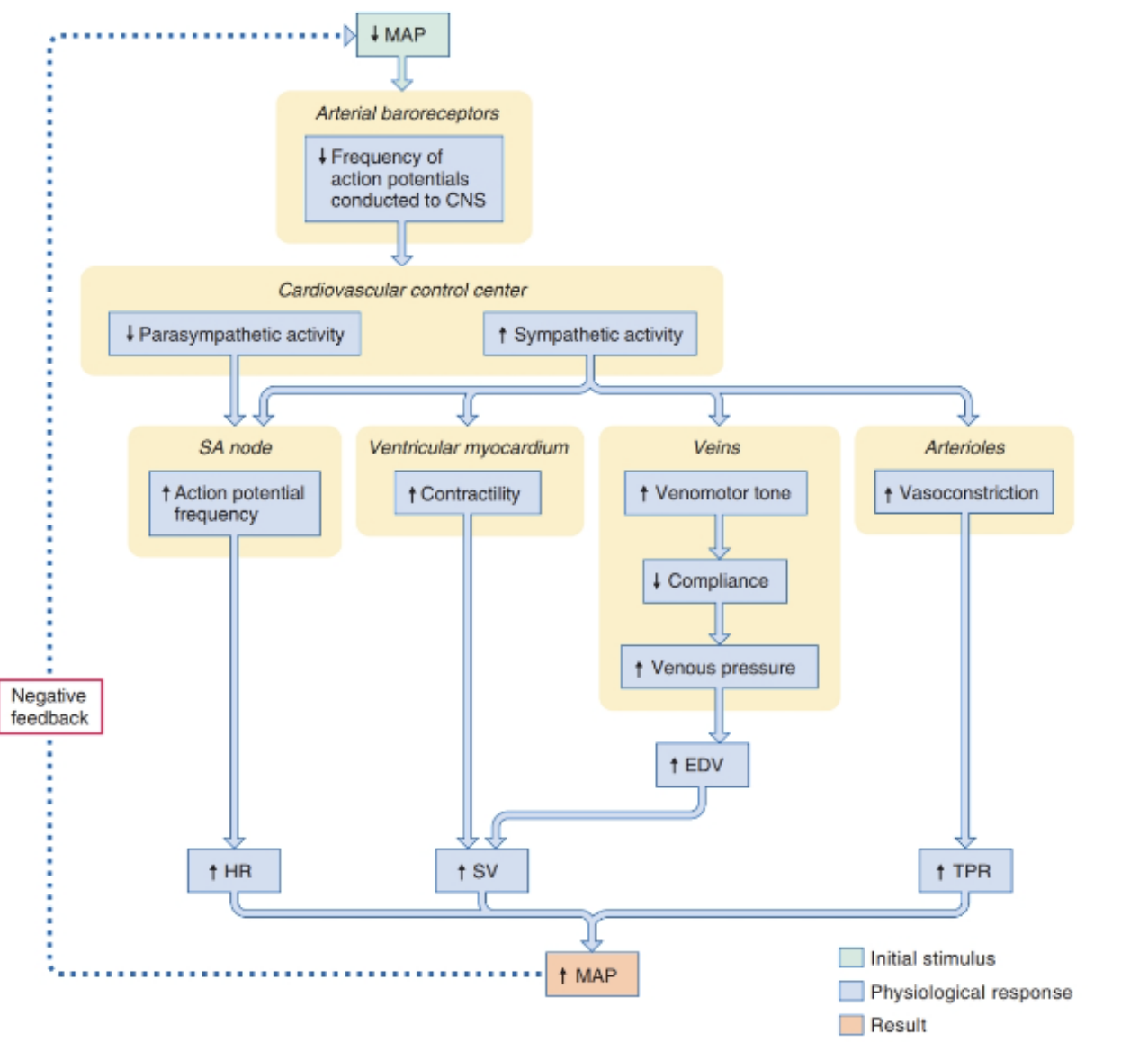
Regulation of MAP
Increase in CO2 same TPR = increased MAP
Same CO2 with increased TPR = increased MAP
At rest extrinsic mechanisms keep MAP consistent via a negative feedback loop
Controlled neurally and hormonally
During exercise resistance is controlled by local mechanism including intrinsic factors (metabolites)
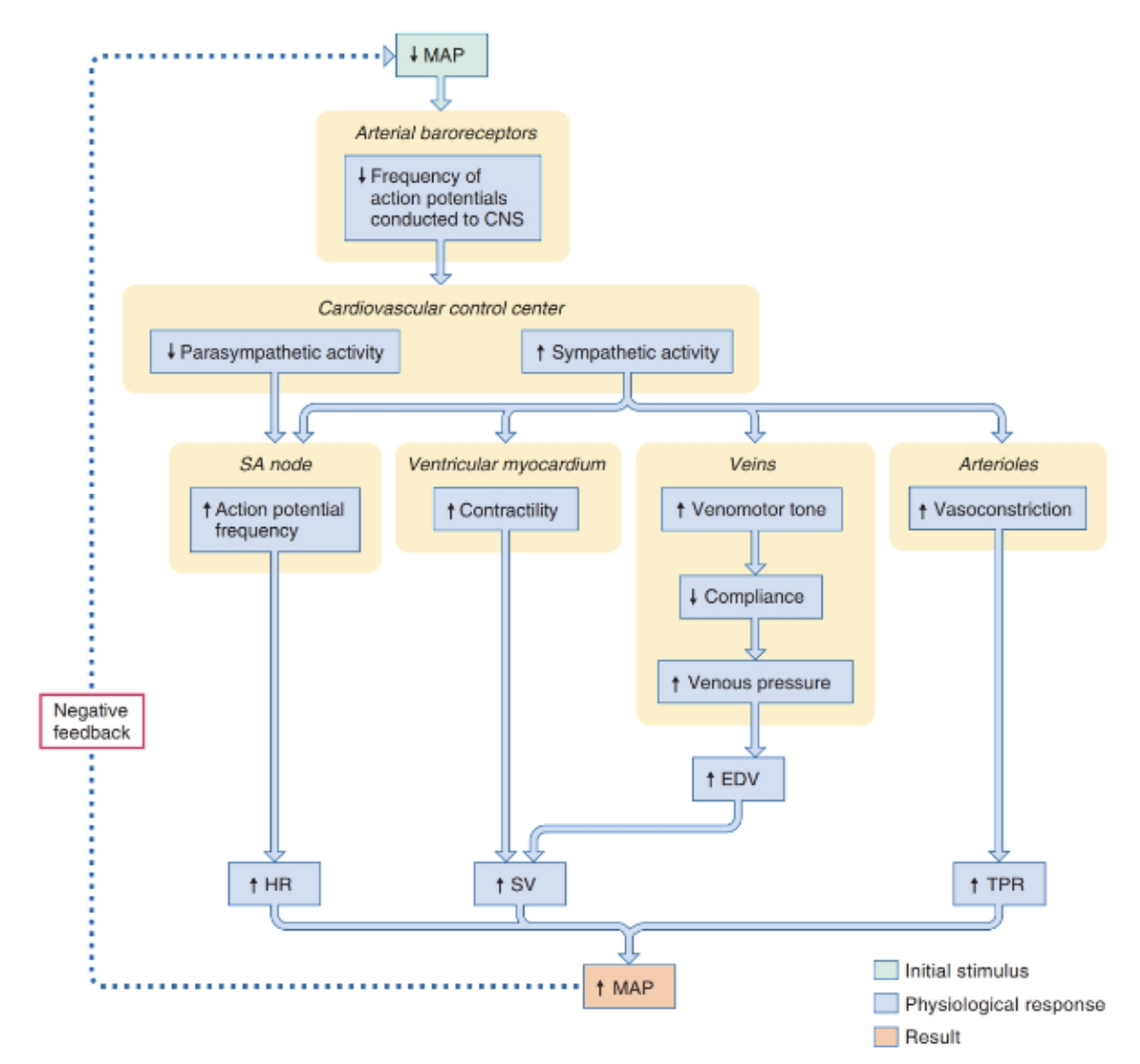
Neural Control of MAP
Medulla controls the collective response and assesses indicators of cardiovascular performance, imput from the hypothalamus for stress response & instructs cardiac system with changes via automatic nervous system.
Sensor | Location |
Arterial baroreceptors | Aortic arch & carotid sinus |
Low pressure baroreceptors | Right atrium & large systemic veins |
Chemoreceptors | Carotid Arteries Proprioceptors Skeletal Muscle & Joints |
Atrial Baroreceptors
Located in aortic arch & carotid sinus
Sense mean arterial pressure
Depolarise when stretched - high BP
Autonomic Inputs
Sympathetic and parasympathic input to SA node to control HR
Sympathetic nerves go to
Ventricular myocardium to control ventricular contractility
Veins and arterioles for vascular resistance
Baroreceptor Reflex
Hormonal Control of MAP
Atrial baroreceptors secrete adrenaline, vasopressin & angiotensin II.
Adrenaline is released when atrial pressure drops
Opens calcium ion channels (for more contractions to increase cardiac output)
Increases MAP total peripheral resistance through vasoconstriction in vascular beds and vasodilation in skeletal and cardiac muscle.
Vasopressin & Angiotensin II
Vasopressin | Angiotensin II |
|
|
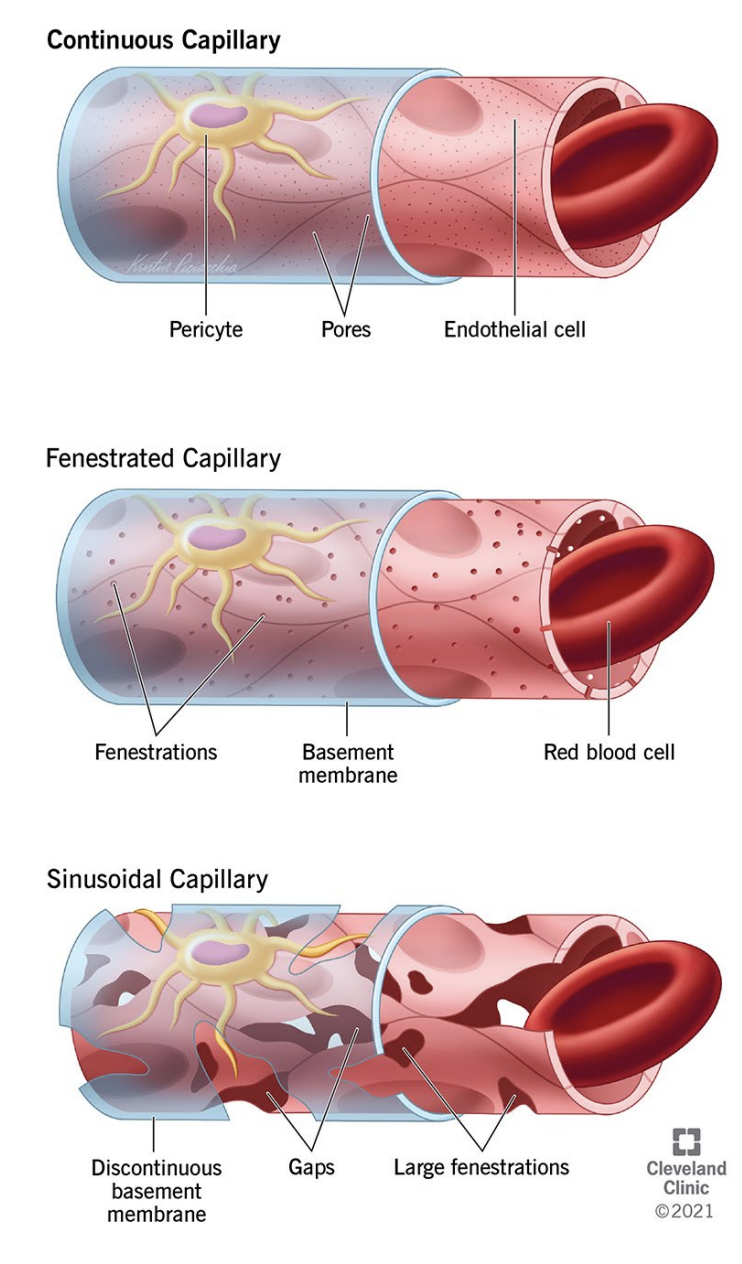
Types of capillaries
Continuous (muscles & CNS): Uninterrupted endothelium lining and only allow diffusion of small molecules.
Fenestrated (kidneys and endocrine glands): Allow for rapid diffusion of larger molecules through small pores (fenestrations) in their walls.
Discontinuous (liver spleen and bone marrow): Large gaps and fenestrations and an incomplete basal membrane allowing cells, plasma, and blood to pass through
Types of arteries
Elastic | Muscular |
|
|
Venules VS Veins
Venules | Veins |
|
|