Exam 2 study guide
1/159
Earn XP
Description and Tags
`
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
160 Terms
What are the components of an ECG waveform?
P wave: atrial depolarization
QRS complex: ventricular depolarization
T wave: ventricular repolarization
PR interval: atrioventricular conduction delay
ST segment: early ventricular repolarization
What is the name for sickness acquired at the hospital
Nosocomial
Bacterial infection versus viral infection
Bacteria is a single-celled organism that can reproduce and grow on its own, viral is a simpler infection that needs a host to live
What are key signs and symptoms of acute coronary syndrome (ACS)?
Chest pain/pressure (may radiate to jaw, shoulder, or arm)
Dyspnea
Diaphoresis
Nausea or vomiting
Anxiety or sense of doom
ECG changes: ST elevation/depression, T wave inversion
What is the prehospital management for a patient with suspected ACS?
Administer oxygen if SpO₂ < 94%
12-lead ECG and cardiac monitoring
IV access
Position of comfort
Rapid transport with early hospital notification
List common cardiac medications and their effects.
ASA: antiplatelet, prevents further clot formation
Nitroglycerin: vasodilation, reduces preload and myocardial workload
Beta blockers: slow HR, lower BP, reduce myocardial oxygen demand
ACE inhibitors: reduce afterload, improve cardiac output
Anticoagulants (e.g., heparin): prevent clot propagation
What are early signs of heart failure in a prehospital assessment?
Dyspnea (especially on exertion or lying flat)
Crackles on lung auscultation
Jugular venous distension (JVD)
Peripheral edema
Tachycardia
Fatigue or weakness
Pink frothy sputum (in severe pulmonary edema)
What complications should you anticipate in acute coronary syndrome?
Arrhythmias (V-fib, V-tach, bradycardias)
Cardiogenic shock
Cardiac arrest
Pulmonary edema
Re-infarction
Sudden death
What are the signs of respiratory distress and impending failure?
Increased respiratory rate (tachypnea)
Use of accessory muscles (neck, intercostals)
Tripod positioning
Nasal flaring (especially in pediatrics)
Cyanosis (late sign)
Inability to speak full sentences
Altered LOC or agitation
Silent chest (ominous sign of no air movement)
How does COPD present and how is it managed?
Chronic airflow limitation, typically from emphysema or chronic bronchitis
Pursed-lip breathing, barrel chest, productive cough, wheezing, cyanosis
Treatment:Controlled O2 (88–92% target sat) to avoid CO2 retention
Salbutamol and Ipratropium
Monitor for fatigue and CO2 narcosis
Transport in position of comfort
Pink puffers versus blue bloaters
Pink puffer is for emphysema and that relates to barrel chest whereas blue bloater is chronic bronchitis
What is pneumonia and how does it present?
Infection of alveoli or interstitial tissue
Fever, chills, productive cough, pleuritic chest pain, crackles/rales, dyspnea
Prehospital care:O2, supportive care, monitor vitals
Treat as sepsis if systemic signs are present
What is a pulmonary embolism (PE) and its classic presentation?
Blockage of pulmonary artery by thrombus (often from DVT)
Sudden unexplained dyspnea
Pleuritic chest pain
Cough with hemoptysis
Tachycardia
Clear lungs on auscultation
May lead to hypotension, shock, or cardiac arrest
Care:High-flow O2, cardiac monitoring, rapid transport
Abnormal (Adventitious) Lung Sounds
Crackles (Rales):
These are discontinuous, popping or clicking sounds, often described as like velcro being pulled apart. They are typically heard during inhalation and can be fine or coarse, moist or dry. They indicate air passing through secretions or the opening of collapsed airways. Crackles are most often heard in the bases of the lungs.
Rhonchi:
These are low-pitched, continuous, snoring-like sounds, caused by airflow obstruction in the larger airways, often due to mucus or other secretions. They can be heard during exhalation or both inhalation and exhalation, but not just during inhalation. Rhonchi are typically heard over the central airways, such as in the bronchi, especially in the chest’s anterior and posterior regions.
Wheezing:
These are high-pitched, whistling sounds, usually heard during exhalation, caused by narrowed airways. They are common in conditions like asthma and COPD. Wheezing is often heard throughout the lung fields but is typically louder in the upper lobes or over areas of narrowed airways.
Stridor:
This is a high-pitched, wheezing sound, usually heard during inhalation, caused by a severe narrowing of the upper airway (trachea or larynx). It is a serious sign and requires immediate attention. Stridor is best heard over the neck and upper chest area.
Pleural friction rub:
This is a creaking or grating sound, caused by the inflamed pleura (lining of the lungs and chest wall) rubbing together. It can be painful and is often heard during both inhalation and exhalation. Pleural friction rub is usually heard in the lower anterolateral chest wall, where the pleural surfaces are in closest contact.
What is a pneumothorax and how can it escalate to a tension pneumothorax?
Air in pleural space collapses lung
Decreased breath sounds on affected side, dyspnea, chest pain
Tension pneumothorax adds: tracheal deviation, JVD, hypotension, cyanosis
Treatment:O2, needle decompression (if trained and authorized), rapid transport
What is the pathophysiology of sepsis?
Systemic inflammatory response to infection → vasodilation, capillary leak, clotting dysregulation → poor perfusion → organ failure
Often triggered by pneumonia, UTI, skin infections, or catheter infections
What are the early signs of sepsis?
Fever or hypothermia
Tachycardia
Tachypnea
Hypotension
Altered mental status
Mottled or flushed skin
Decreased urine output
How should you manage sepsis prehospital?
Administer high-flow oxygen
Establish IV access, give fluid bolus (NS)
Monitor LOC, respiratory rate, BP
Notify receiving hospital (Sepsis Alert)
Keep patient warm
Avoid unnecessary delays — rapid transport
What are the components of a neurological assessment?
Fast Van
What is the difference between a CVA (stroke) and a TIA?
CVA: Permanent neurological damage due to ischemia or hemorrhage
TIA: Temporary interruption of blood flow, symptoms resolve in <24 hours
Symptoms: Facial droop, arm drift, speech difficulty, visual loss, weakness/numbness
has it been more or less than 6 hours? if they woke up like this it counts as less
What are the signs of increased intracranial pressure (ICP)
Headache
Vomiting (often without nausea)
Altered LOC
Unequal pupils
Bradycardia, irregular respirations, widened pulse pressure (Cushing’s triad)
Seizures
: What is SIRS and how is it defined?
SIRS (Systemic Inflammatory Response Syndrome) is a widespread inflammatory reaction to a variety of clinical insults (infection, trauma, burns, etc.).
SIRS criteria (≥2 of the following):
Temperature >38°C or <36°C
Heart rate >90 bpm
Respiratory rate >20 breaths/min or PaCO₂ <32 mmHg
WBC >12,000 or <4,000 or >10% bands
What is sepsis, and how is it related to SIRS?
Sepsis = SIRS + suspected or confirmed infection.
It is a dysregulated immune response to infection, leading to tissue damage and potential organ failure.
Progression:
Sepsis → Severe Sepsis (with organ dysfunction) → Septic Shock (with persistent hypotension despite fluids)
What organ systems are affected by sepsis, and how?
A:
Respiratory: Hypoxia, ARDS
Cardiovascular: Vasodilation → hypotension → shock
Renal: Decreased perfusion → acute kidney injury → low urine output
Hepatic: Coagulopathies, jaundice
Neurological: Altered LOC, confusion
GI: Poor perfusion → ileus or gut ischemia
What are early and late signs of sepsis in the field?
A:
Early: Fever or hypothermia, tachycardia, tachypnea, flushed or warm skin, anxiety or confusion
Late: Hypotension, mottled/cool skin, altered LOC, decreased urine output, cyanosis
What is the pathophysiology of Parkinson’s disease?
Degeneration of dopamine-producing neurons in the substantia nigra of the brain.
Dopamine is critical for smooth, coordinated muscle movements. Its depletion causes resting tremor, rigidity, and bradykinesia.
What is the pathophysiology of Multiple Sclerosis (MS)?
Autoimmune attack on the myelin sheath of CNS neurons → demyelination and plaque formation → disrupted nerve conduction.
Leads to motor weakness, vision issues, fatigue, and sensory disturbances.
What is the pathophysiology of Amyotrophic Lateral Sclerosis (ALS)?
Progressive degeneration of upper and lower motor neurons → muscle atrophy and paralysis.
Cognitive function usually preserved, but death typically results from respiratory failure.
What is the pathophysiology of Muscular Dystrophy?
Genetic defect in dystrophin (a muscle-supporting protein) → progressive muscle fiber breakdown and weakness.
Begins in childhood, especially affecting pelvic and shoulder muscles.
What is the pathophysiology of appendicitis and how does it present?
Obstruction of the appendix (often by fecalith) → inflammation, ischemia, and possible rupture.
Presentation: RLQ pain (McBurney's point), rebound tenderness, fever, nausea, vomiting, guarding.
Treatment: Pain management, antiemetics, IV fluids, NPO, transport to surgical facility.
What is the pathophysiology and field management of bowel obstruction?
Mechanical blockage (tumor, hernia, adhesions) or functional paralysis → backup of contents.
Presentation: Abdominal distension, cramping pain, vomiting (possibly fecal-smelling), no bowel movement or gas.
Treatment: Monitor airway, IV fluids, antiemetics, NPO, rapid transport.
What is peritonitis and how does it present?
Inflammation of the peritoneum, often due to perforation of a hollow organ.
Presentation: Severe abdominal pain, rebound tenderness, rigid abdomen, fever, nausea, tachycardia, signs of shock.
Treatment: O2, fluids, NPO, monitor vitals, rapid transport.
How does pancreatitis present and what causes it?
Caused by gallstones, alcohol use, or high triglycerides.
Presentation: Epigastric or LUQ pain radiating to the back, nausea, vomiting, fever, abdominal guarding.
Treatment: Supportive care, pain control, fluid resuscitation, monitor for shock.
What are key signs and concerns in gastrointestinal bleeding (GI bleed)?
Upper GI bleed: Hematemesis (vomiting blood), melena (black stools)
Lower GI bleed: Bright red blood per rectum
Concerns: Hypovolemic shock, anemia
Treatment: O2, IV fluids, monitor for hypotension and tachycardia, NPO, transport upright unless hypotensive
What is the pathophysiology and presentation of a urinary tract infection (UTI)?
Bacterial infection (usually E. coli) ascends from the urethra into the bladder.
Symptoms: Dysuria, urgency, frequency, suprapubic pain, foul-smelling or cloudy urine
Treatment: Supportive care, monitor for signs of sepsis if fever/LOA present, transport
What is pyelonephritis and how does it differ from a UTI?
Infection spreads to the kidneys → systemic symptoms
Presentation: Flank pain, fever, chills, nausea/vomiting, CVA tenderness
Treatment: Monitor for sepsis, IV fluids, pain control, transport
What are renal colic and kidney stones, and how do they present?
Calculi form in the kidney and obstruct ureter
Symptoms: Sudden severe flank pain radiating to groin, hematuria, restlessness, nausea/vomiting
Treatment: Pain management, antiemetics, fluids, position of comfort, rapid transport
What is urinary retention and how might it present?
Inability to void despite full bladder — common in males with BPH
Symptoms: Suprapubic pain/distension, urgency, no urine output, restlessness
Treatment: Monitor vitals, support ABCs, transport
What are red flags in GI/GU emergencies that suggest critical illness?
Absent bowel sounds with distension
Rigid abdomen
Vomiting fecal matter
Tachycardia with hypotension
Rectal bleeding or hematemesis
Severe dehydration or altered LOC
melana
hematochezia
Where do you put the three lead ECG
On the shoulders or wrists and calves
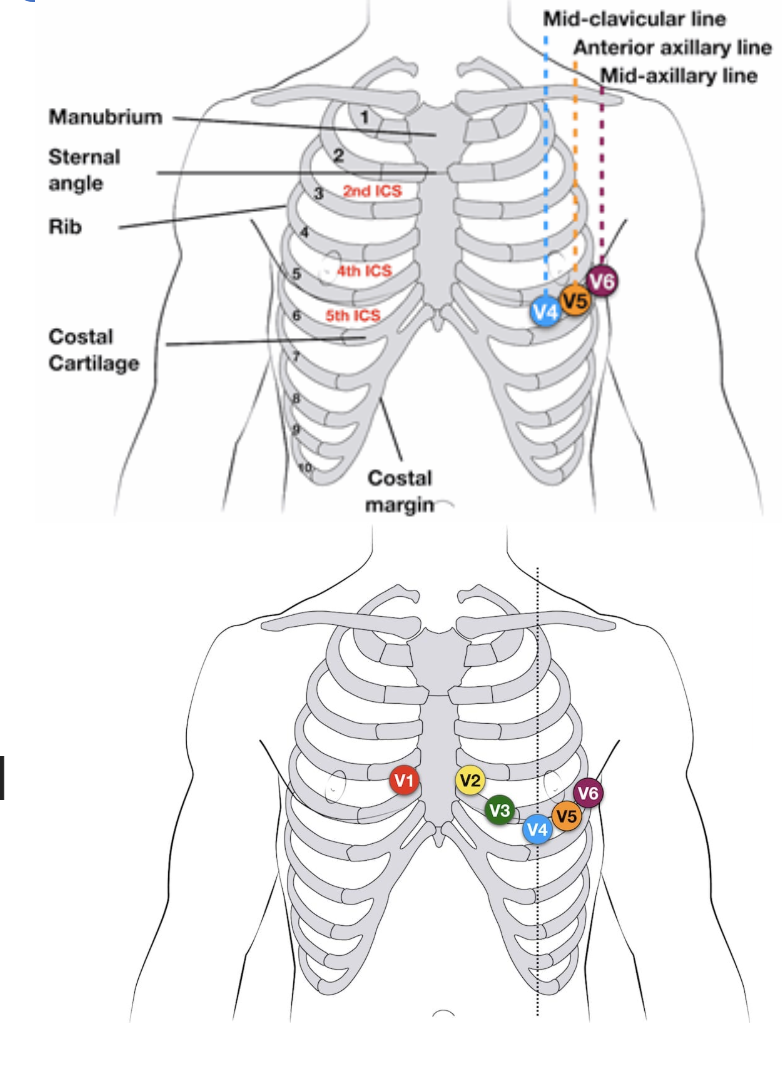
12 lead ECG placement
Name the steps for IM injection
Hopefully you didn't forget aspiration
What age-related changes affect pharmacology in geriatric patients?
Decreased renal and liver function slows drug metabolism/excretion
Altered body composition (↑ fat, ↓ muscle) affects distribution
Increased sensitivity to CNS depressants and anticoagulants
Polypharmacy increases risk of adverse effects and interactions
What are common geriatric presentations that differ from younger patients?
A:
Silent MIs (no chest pain)
Infections without fever (e.g., UTI → delirium)
Falls with fractures or head injury without major mechanism
Hypoglycemia with confusion instead of diaphoresis
Pneumonia without cough or sputum
What is the difference between delirium and dementia?
Delirium: acute onset, fluctuating consciousness, often reversible (infection, medication, metabolic)
Dementia: chronic, progressive cognitive decline (e.g., Alzheimer’s), usually irreversible
What is the difference between right-sided and left-sided heart failure?
Left-sided heart failure results in pulmonary congestion due to the left ventricle failing to pump blood effectively, causing fluid to back up into the lungs.
Signs: dyspnea, orthopnea, crackles, pink frothy sputum, fatigue.Right-sided heart failure leads to systemic venous congestion due to failure of the right ventricle, causing blood to back up into the body.
Signs: peripheral edema, JVD, ascites, hepatomegaly.
What is the normal range for blood glucose levels?
4.0–7.0 mmol/L fasting; <10.0 mmol/L postprandial (after eating) .
What are the classic signs and symptoms of hypoglycemia?
Diaphoresis, tachycardia, confusion, weakness, hunger, altered LOC, seizures .
How should hypoglycemia be managed in the field?
If the patient is conscious and can swallow, give oral glucose. If unable to take oral glucose start an IV and give dextrose, if unable to obtain an IV give glucagon.
What is diabetic ketoacidosis (DKA)?
A serious complication of uncontrolled diabetes (mainly type 1), involving hyperglycemia, ketone production, and metabolic acidosis .
What are the key signs and symptoms of DKA?
Polyuria, polydipsia, fruity-smelling breath, Kussmaul respirations, nausea, vomiting, dehydration, altered LOC .
How is DKA managed in the prehospital setting?
Support airway, provide high-flow oxygen, establish IV access for fluid resuscitation, and transport urgently. Do not administer insulin in the field .
What is Hyperosmolar Hyperglycemic Syndrome (HHS)?
A complication of type 2 diabetes characterized by extreme hyperglycemia and dehydration without significant ketoacidosis .
What are signs of HHS?
hyperglycemic hyperosmolar syndrome Profound dehydration, extremely high BGL (>33 mmol/L), confusion, weakness, possible seizures .
What is Addisonian crisis?
A life-threatening condition caused by adrenal insufficiency, usually triggered by stress or infection in someone with Addison's disease .
What are signs of Addisonian crisis?
Hypotension, dehydration, nausea, vomiting, abdominal pain, hypoglycemia, shock .
What is thyroid storm?
A hypermetabolic emergency caused by excessive thyroid hormone, often due to untreated hyperthyroidism .
Symptoms of thyroid storm include:
Tachycardia, hyperthermia, agitation, altered LOC, vomiting, diarrhea, possible cardiac dysrhythmias .
Name common classes of psychiatric medications.
Antidepressants (SSRIs), antipsychotics (e.g., haloperidol), mood stabilizers (e.g., lithium), anxiolytics (e.g., benzodiazepines) .
What is hypothyroidism and what causes it?
A condition in which the thyroid gland does not produce enough thyroid hormone.Causes: Autoimmune disease (e.g., Hashimoto’s), iodine deficiency, or post-thyroid surgery.
What are the signs and symptoms of hypothyroidism?
Fatigue, cold intolerance, bradycardia, weight gain, dry skin, constipation, depression, slow reflexes, and menstrual irregularities.
What is the PCP management for a hypothyroid patient?
Supportive care. Be alert for myxedema coma in severe cases — treat with oxygen, warming, fluid resuscitation, and urgent transport.
What is hyperthyroidism and what causes it?
A condition where the thyroid gland produces excessive thyroid hormones.
Causes: Most commonly Graves’ disease, toxic multinodular goiter, or thyroiditis.
What are the signs and symptoms of hyperthyroidism?
Weight loss, heat intolerance, tachycardia, anxiety, tremors, palpitations, diarrhea, and exophthalmos (bulging eyes).
What are the signs and symptoms of pericardial tamponade?
Hypotension, muffled heart sounds, and jugular venous distension — known as Beck’s triad. Other signs include tachycardia, dyspnea, and pulsus paradoxus.
What is a Transient Ischemic Attack (TIA)?
A TIA is a temporary interruption of blood flow to the brain causing stroke-like symptoms that resolve within 24 hours. It’s a warning sign of potential future stroke.
What is Amyotrophic Lateral Sclerosis (ALS)?
A progressive neurodegenerative disease affecting motor neurons. Patients lose voluntary muscle control but maintain mental awareness. It eventually affects respiratory muscles.
Explain how the hormonal system regulates blood glucose levels, including the roles of the pancreas, liver, insulin, glucagon, glycogenesis, and glycogenolysis.
The hormonal system regulates blood glucose through two main hormones released by the pancreas:
Insulin (from β-cells of the islets of Langerhans)
Glucagon (from α-cells of the islets of Langerhans)
🟩 When Blood Glucose Is High (e.g., after a meal):
Insulin is released
Stimulates glucose uptake by muscle and fat cells
Stimulates the liver to perform glycogenesis: converting glucose → glycogen for storage
Inhibits glycogenolysis and gluconeogenesis
Overall effect: Lowers blood glucose
🟥 When Blood Glucose Is Low (e.g., fasting, exercise):
Glucagon is released
Stimulates the liver to break down glycogen (glycogenolysis) into glucose
Stimulates gluconeogenesis: creation of glucose from non-carbohydrate sources
Overall effect: Raises blood glucose
🏥 Organs Involved:
Pancreas: Senses blood glucose and secretes hormones (insulin, glucagon)
Liver: Main site for glycogen storage and glucose production/release
Muscles and adipose tissue: Sites of glucose uptake and storage
What is peritonitis and how does it present?
Inflammation of the peritoneal lining, usually from infection or organ rupture. Signs include diffuse abdominal pain, rigidity, guarding, fever, and rebound tenderness.
What are signs of bowel obstruction?
Crampy abdominal pain, bloating, vomiting, absence of bowel movements or flatus, and high-pitched bowel sounds. Can lead to peritonitis or shock if untreated.
What is cardiogenic shock and what causes it?
A condition where the heart cannot pump effectively, leading to poor perfusion. Commonly follows an extensive MI. Signs: hypotension, pulmonary edema, weak pulses, cold skin.
What is Cushing’s syndrome and what are its signs?
Caused by prolonged exposure to excess cortisol (e.g., from steroids or adrenal tumors). Signs: moon face, central obesity, easy bruising, muscle weakness, hypertension.
What is the pathophysiology of Guillain-Barré Syndrome (GBS)?
An autoimmune disorder in which the immune system attacks the peripheral nervous system, often following a viral illness. It causes demyelination of peripheral nerves, leading to impaired nerve signal transmission and progressive, symmetrical weakness beginning in the legs.
What are the signs and symptoms of Guillain-Barré Syndrome?
Symmetrical ascending weakness, paresthesia, loss of reflexes, facial weakness, dysphagia, and risk of respiratory failure. Autonomic instability (e.g., blood pressure swings) may also occur.
What is vertigo, and how is it different from general dizziness?
Vertigo is the illusion of movement or spinning, typically caused by vestibular dysfunction. Dizziness is a broader term that can include lightheadedness, imbalance, or presyncope.
What is Bell’s Palsy and how does it differ from a stroke?
Bell’s Palsy is an acute peripheral facial nerve paralysis affecting one side of the face, including the forehead. It is often idiopathic or viral and typically resolves over time. In stroke, forehead movement is often preserved.
What is Crohn’s disease and how does it present?
A chronic inflammatory bowel disease affecting any part of the GI tract, most commonly the terminal ileum. Presents with RLQ pain, diarrhea, weight loss, fatigue, and possible obstruction or bleeding.
What is ulcerative colitis and how does it differ from Crohn’s disease?
Ulcerative colitis is limited to the colon and rectum and involves only the mucosal layer. It presents with bloody diarrhea, abdominal cramping, and urgency. Unlike Crohn’s, it does not involve the small intestine or deep tissue layers.
What is diverticulitis and how does it present?
Inflammation or infection of diverticula in the colon, usually presenting with LLQ pain, fever, tenderness, constipation or diarrhea, and possible risk of perforation.
What is an abdominal aortic aneurysm (AAA), and how might it mimic GI pain?
A weakened, bulging area in the aorta that may rupture. Presents with sudden, severe abdominal or back pain, hypotension, and possibly a pulsatile mass. Mimics GI pain but is a life-threatening vascular emergency.
What is testicular torsion and how is it managed?
Twisting of the spermatic cord, cutting off blood supply to the testicle. Presents with sudden, severe testicular pain, swelling, high-riding testicle. Requires immediate surgical intervention. Transport rapidly and gently.
What is benign prostatic hyperplasia (BPH) and how does it present?
Non-cancerous enlargement of the prostate that obstructs urinary flow. Symptoms include urinary retention, weak stream, urgency, and nocturia. Can lead to post-renal failure if untreated.
What is epididymitis and how does it differ from testicular torsion?
Inflammation of the epididymis, usually due to infection. Presents with gradual-onset scrotal pain, swelling, and fever. Unlike torsion, the testicle remains in a normal position and symptoms evolve over time.
What is Cushing’s Triad, and what does it indicate?
Cushing’s Triad is a set of three classic signs indicating increased intracranial pressure (ICP):
Hypertension (widening pulse pressure)
Bradycardia
Irregular or abnormal respirations (e.g., Cheyne-Stokes)
It suggests possible brain herniation and is a late, life-threatening sign of ICP.
What is excited delirium and what are its risks?
A state of agitation, aggression, hyperthermia, and altered strength, often related to stimulant use.
Risks: Sudden cardiac arrest, especially after physical restraint.
What are signs of meningitis, and how is it transmitted?
Fever, headache, photophobia
Nuchal rigidity (stiff neck)
Altered LOC
Possible petechial rash
Transmission: Droplet
What is anaphylaxis and how is it different from a mild allergic reaction?
Anaphylaxis is a life-threatening systemic allergic reaction involving ≥2 systems or hypotension.
Mild reactions are localized (rash, itch, sneezing).
What is an abscess and how is it transmitted?
A bacterial infection transmitted through direct contact. It causes a localized, pus-filled pocket of infection due to the body’s response to bacteria.
What is cellulitis and how does it present?
bacterial infection spread through contact with an open wound. Causes red, swollen, warm, and tender skin, usually on the legs. May lead to sepsis if untreated.
What are key features of chickenpox?
A viral infection spread through airborne or droplet transmission. Presents with fever, fatigue, and an itchy rash that evolves from red spots to scabs. May reactivate later as shingles.
What are key features of diphtheria?
A bacterial illness spread via respiratory droplets. Produces a gray pseudomembrane in the throat, fever, and may cause airway obstruction, nerve damage, or myocarditis.
What are the symptoms and risks of COVID-19?
A viral illness spread via respiratory droplets. Causes fatigue, dry cough, fever, and loss of taste or smell. Severe cases may lead to ARDS, pneumonia, or multi-organ failure.
What is gastroenteritis and how is it transmitted?
A viral or bacterial infection transmitted through fecal-oral contamination. Causes vomiting, diarrhea, stomach cramps, and dehydration.
What are symptoms of encephalitis?
inflimation of the brain. A viral or bacterial infection transmitted via vectors, blood, or respiratory droplets. Causes brain inflammation, headache, fever, seizures, confusion, and altered LOC. May result in permanent brain damage.
What is Hepatitis A and how is it spread?
A viral infection spread via fecal-oral route. Causes temporary liver inflammation, jaundice, fatigue, nausea, and dark urine. Usually not chronic.
What are key features of Hepatitis B?
A viral illness transmitted via bodily fluids. Can be acute or chronic. Causes liver cell injury, jaundice, fatigue, and right upper quadrant pain.
What are the effects of Hepatitis C?
A viral infection transmitted through blood. Causes progressive and often chronic liver damage. May lead to cirrhosis or liver cancer but can be managed with modern treatment.
What does HIV/AIDS do to the immune system?
A viral infection spread through bodily fluids. HIV attacks CD4 and T-cells, weakening immunity. Initially flu-like, it progresses to AIDS, where opportunistic infections and cancers occur.
What are the symptoms of influenza?
A viral illness transmitted via respiratory droplets. Causes fever, chills, sore throat, cough, and systemic symptoms. Strains vary seasonally.