UNIT 2 REVIEW - 118
1/201
Earn XP
Description and Tags
BEAST MODE!!!!!!!!!!!!!!!!!!!!!
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
202 Terms
What is the term for normal respiration rate, and what is the rate?
Eupnea, 12-20 breaths per minute
What is Tachypnea?
Fast Respiration Rate,
>24 breaths per minute
pt could have:
Pneumonia
Pulmonary Edema
Metabolic Acidosis
Sepsis
Pain
Fractures
What is Bradypnea?
Slow Respiration Rate
<10 breaths per minute
pt could have:
head injury
drug overdose
C02 >45
What is Dyspnea?
Difficulty Breathing, SoB.
What is Orthopnea?
Difficulty Breathing WHEN SUPINE.
What is Apnea?
Absent, no breathing
What is Kussmaul’s Respirations?
Fast & abnormally deep respiration,
(?) metabolic acidosis
What is Biot’s Respirations?
Irregular Cycles, Fast & Shallow USUALLY FOLLOWED WITH APNEA.
Brain Injury = Neuro
What is Cheyne-Strokes Respirations?
REGULAR CYCLES, FAST DEEP RESPIRATION THEN DECREASES DEPTH TO APNEA.
damage to respiration center
What is Stridor?
is a high-pitched, noisy breathing sound caused by narrowing or obstruction of the upper airway, such as the larynx or trachea
IT IS AN EMERGENCY IF HEARD
What are some ways to assess respiratory effort?
Nasal Flaring
Retractions
Use of Accessory Muscles
Grunting
Body Positioning
Conversational Dyspnea
Stridor
Wheezing
How do you auscultate lung sounds?
move from right to left or left to right, comparing BOTH SIDES!
What should lungs usually sound like?
Lung sounds should usually be clear.
Where can you find normal lung sounds?
Bronchial
Broncho-vesicular
Vesicular
What does rales (crackles) sound like?
Air bubbling through moisture/fluid in ALVEOLI
Usually heard on inspiration
remember rales in the tails (Alveoli are in the “tail end” of the lung)
What does Rhonchi sound like?
Rumbling snoring sound, air moving through mucous in large TUBULAR AIRWAYS.
Often heard on expiration
usually with pts that have
pneumonia
bronchitis
COPD
secretions
What does Wheezing sound like?
Narrow/constricted small airways from partial obstruction. very high pitch.
Usually on Expiration
usually with pts that have:
asthma
bronchospasms
What does Stridor do?
UPPER AIRWAY PARTIAL OBSTRUCTION! IS AN EMERGENCY. CAN LEAD TO FULL OBSTRUCTION
What does Pleural friction rub sounds like?
like leather rubbing togethers or fingers rubbing together.
Inflammation
Low Pleural Fluid
What does Grunting sound like?
Trapped air that is forced out on expiration
What WBC indicates an infection?
If the WBC are > 10,000
What is Hemoglobin?
A vital protein in red blood cells.
What is a Sputum C&S?
It identifies the actual infective agent
What does a Chest X-Ray do?
Shows images of the lungs & detect Pneumonia, infiltrates, COPD, atelectisis
Why do you have a sleep study for?
To check for sleep apnea
What is a Pulmonary Function Test?
is a series of non-invasive tests that assess lung function by measuring parameters including forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FEV1/FVC ratio, peak expiratory flow (PEF), total lung capacity (TLC), residual volume (RV), and diffusion capacity, providing valuable diagnostic information for various respiratory conditions.
What is a pulse oximetry test?
non-invasive test that measures the oxygen saturation level in the blood by shining light through a pulsating capillary bed (e.g., fingertip) to assess the percentage of hemoglobin that is saturated with oxygen, commonly used to monitor respiratory status in clinical and home settings.
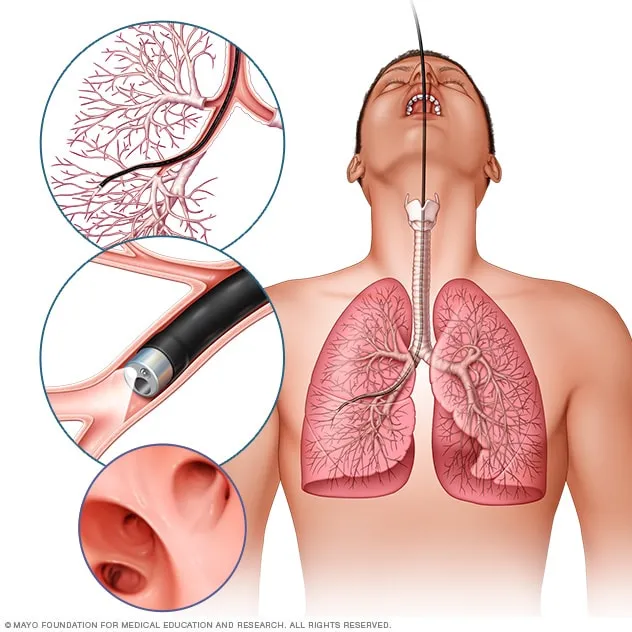
What is a Bronchoscopy?
is a medical procedure in which a thin, flexible tube equipped with a camera and light is inserted through the mouth or nose into the airways to visually examine the lungs, obtain tissue samples for biopsy, or perform treatments to diagnose and manage various lung conditions.
What is Arterial Blood Gases?
Arterial blood gases (ABGs) refer to a blood test that measures the levels of oxygen (O2), carbon dioxide (CO2), and pH (acidity) in arterial blood, providing critical information about respiratory and metabolic function.
What is a Peak Flow Meter
A peak flow meter is a handheld device used to measure the peak expiratory flow rate (PEFR), which is the maximum speed at which a person can exhale air from their lungs. This measurement helps assess the function of the airways and is commonly used in the management of asthma to monitor lung function and track changes in airflow.
What do the colors mean on a Peak Flow Meter?
Green - all clear
Yellow - caution - take bronchodilator
Red - severe reduction in peak flow - go to ED
What is a Incentive Spirometer?
is a medical device used to help improve lung function by encouraging deep breathing and preventing lung complications, particularly after surgery or during illness.
What is the purpose of an incentive spirometer?
Facilitate sustained slow deep breath
prevent and reverse atelectasis when used regularly and appropriately
helps to liquefy, loosen, and prevent pneumonia
How often should you use an incentive spirometer?
10 to 20 times PER HOUR
What are some interventions to manage and improve respiratory function?
Position for MAXIMUM ventilation
High Fowler’s - Orthopneic position
Mobilize Secretions
Coughing, deep breathing, chest PT
Maintain hydration - increase fluids to thin secretions
Assist with incentive spirometry
Use to encourage patients to deep breath by reaching goal directed volumes of air
Respiratory medications
Promote ventilation and oxygenation, some need a prescription some do not.
ex - bronchodilators, anti-inflammatory agents (corticosteroids), cough suppressants
Teaching - help promotion (diet & exercise)
Provide oxygen therapy if needed
Suction if needed (remove excess secretions from airways)
Support Smoking Cessation (end smoking)
what are some interventions you can teach patients about managing respiratory function?
Weight Reduction
Diet - Low NA+, cholesterol
Exercise
Stress Reduction
Occupational Safety
Vaccines - influenza, pneumonia
Teach infection control
Limit exposure to crowds
What is “Hypoxemia”?
Low arterial blood oxygen levels
Poor diffusion across alveolar membranes
oxygen in the blood
Etiology:
Heart Failure
COPD
Sleep Apnea
Anemia
Asthma
pneumonia
Pulmonary edema (accum of fluids in the lungs)
What are some S/S of Hypoxemia?
Headache
SoB
Tachycardia
Tachypnea
Confusion
Cyanosis of skin finger lips
What are some treatments for Hypoxemia?
Raise O2 blood levels
Give medications to treat underlying causes
stop smoking
deep breathing
pursed lip breathing
H2O
eat healthy
walking
What is “Hypoxia”?
Inadequate oxygenation of organ or tissues
Etiology
Hypoxemia
circulatory/resp. disorders
Low Hemoglobin
What is Hypercarbia?
Excess of CO2 in the blood
Etiology -
hypoventilation, COPD sleep apnea
S&S
confusion, coma, arrhythmias, loss of consciousness, seizures
DX - ABG, XRAY, CBC, BMP, PFT
anesthetic effect
What can high blood levels of carbon dioxide do to you? (hypercarbia)
Can have an anesthetic effect on the nervous system, causing somnolence progressing to coma and death.
What is Hypocarbia?
Low level of CO2 in blood
Etiology
hyperventilation
low blood levels of carbon dioxide have a stimulating effect on the nervous system and lead to muscle twitching or spasm (esp in hands or feet)
What are signs of Hypoxia?
Early S/S - Restlessness, Anxiety/Apprehension, Confusion
Normal S/S
Tachycardia
TachypneaSoB
Cyanosis (look at tongue and oral mucosa)
Decreased level of consciousness
abnormal lung sounds (adventitious)
Best place to look for clubbing & cyanosis
CLUBBING of FINGERS = SEEN WITH CHRONIC HYPOXIA D/T CHRONIC PULMONARY & CARDIAC DISEASE
•Nail bed sponginess
•Excessive rounding of the nail plate
•Flattening of the angle between the nail plate and the proximal nail skin fold
What are some Hypoxia interventions?
Rapid Assessment - happens simultaneously
HoB - High Fowler’s
Call for Help
Count Respirations
Pulse Oximetry Stat
Apply Oxygen if Pulse Oxy <90%
Check vital signs
Listen to lung sounds
What is Chronic Bronchitis?
Inflammation and hypersecretion of mucus in bronchi & bronchioles caused by chronic exposure to irritants - causing airway obstruction
What are some causes of chronic bronchitis?
Smoking (90% of cases)
Occupational exposures
Air pollution
Asthma
Cystic Fibrosis
What are some S&S of Chronic bronchitis?
Chronic cough
Thick, tenacious sputum
Rhonchi in the Bronchi
Wheezing
Hypoxemia & Hypoxia = Dusky - Cyanosis
Tachycardia
Tachypnea
Dyspnea, SoB
Peripheral edema
Orthopnea
What are some ways to treat chronic bronchitis, AND COPD Emphysema?
Bronchodilators
Corticosteroids
Expectorant (loosens and expel mucus and secretions from respiratory tract)
Anti Infectives (if r/t infection)
Controlled Oxygen delivery or BiPAP (Bilevel positive airway pressure)
Pulmonary Rehabilitation
Stop Smoking
Get Vaccinations
What is COPD Emphysema?
Destruction of alveoli, narrowing of bronchioles, and air trapping of air resulting in loss of lung elasticity
Etiology:
Smoking (90% of cases) Occupational exposures, air pollution, asthma, CF
S&S
Difficulty exhaling
Barrel Chest
Weight Loss
Clubbing - from chronic hypoxia
Tripod positioning
Infrequent cough
Hypoxia
Dyspnea
Accessory muscle use
Purse lipped breathing
What is CNS stimulations to breath?
ASK FOR EXPLANATION. THIS IS WHAT SLIDE SAYS FUCK IT
Normal Person:
•Increased levels of CO2
COPD=chronic bronchitis, emphysema
•Decreased levels of O2
What is Hypoxic Drive? Talk about the amount of oxygen we can give them.
Refers to people with COPD
chronic bronchitis
emphysema
**THEIR STIMULUS TO BREATHE IS LOW ARTERIAL O2 LEVELS
There are limits to the amount of supplemental O2 we can give the patient, if we give them too much oxygen we can cause harm and death because it will worsen hypoxia.
What is Sleep Apnea?
A periodic interruption in breathing during sleep—an absence of air flow through the nose or mouth during sleep.
• Pauses that last 10 to 30 seconds. Episodes may occur several or a hundred times a night and may last up to 1 minute or longer.
• During periods of apnea, the oxygen level in the blood drops, and the carbon dioxide level rises, causing the person to wake up.
What is Obstructive Sleep Apnea (OSA)
• Typically, the soft tissue of the pharynx and soft palate collapse, tongue falls into the back of the throat, and obstructs the upper airway.
• OSA is diagnosed clinically by reports of at least five witnessed breathing interruptions or awakenings due to gasping or choking events per hour.
What are some treatments that can help patients with sleep apnea?
Continuous positive airway pressure (CPAP)
Bi-level positive airway pressure (BiPAP)
Lateral positioning
Dental Appliances
Weight loss
No Smoking
No alcohol
Nose tapes
What are some nursing interventions for sleep apnea?
•Assessment- recognizing symptoms
•Promoting-Teaching
•side lying positioning for sleep, to allow full relaxation and avoid blockage of airway
•weight loss of at least 10% of the patient's current body weight
•Use of oral mouth guards that push the tongue down and pull the jaw forward to open more space at the back of the throat
•Continuous positive airway pressure (CPAP) therapy.
What is Suctioning?
a medical procedure used to clear airway secretions and maintain breathing by removing mucus, fluids, or foreign objects using a suction catheter and negative pressure.
only done as needed, PRN
independent nursing intervention
What is a yankauer?
a type of suction catheter used for oral suctioning during medical procedures or to clear secretions from the mouth and airway.
How do you suction clean the upper airway?
•Secretions in mouth or back of throat that can not be expectorated
•May be heard as gurgling, moist conversations
•We can use yankauer to suction & clear
How do you suction clean the lower airway?
•Will use suction catheter
•A sterile procedure
•Pre-oxygenate with 100% O2
•Duration of each suction pass should be limited to ten seconds and only on way out
•The number of passes should be limited to three or less
What are Electrolytes?
They are in lab tests refer to essential minerals or ions, such as sodium, potassium, chloride, bicarbonate, calcium, and magnesium, which carry electric charges and are vital for various physiological functions in the body.
•Too much or too little of certain electrolytes affect cardiac function
•Potassium (K+) levels have a very strong influence on the function of the heart, both too much or too little (K+ = heart function)
What is PT/PTT?
Laboratory test that assess different aspects of the blood clotting process, helping to evaluate bleeding disorders or monitor anticoagulant therapy.
•Both are used to assess the intrinsic system and the common pathway of clot formation
•We will discuss in more detail when we discuss the anticoagulant drugs on your unit 2 drug list: warfarin, heparin, enoxaparin
What is CK-MB?
an enzyme found in the heart muscle that is measured in blood tests to diagnose and monitor acute myocardial infarction (heart attack).
•A blood test used to diagnose a myocardial infarction and subsequent cardiac muscle damage
•If the blood serum levels show an elevated creatinine kinase MB, this indicates cardiac muscle damage
•Usually rises 3-6 hours after cardiac event
What is Troponin?
a protein that is a biochemical marker for cardiac injury.
•They can become elevated as early as 2-3 hours after myocardial injury
•This test is faster than CK-MB
What is BNP? (B-type natiuretic peptide)
is a hormone produced by the heart in response to increased pressure and volume, and its blood levels are used as a diagnostic marker for heart failure and to assess cardiac function.
•Used to identify and stratify patients with congestive heart failure (CHF)
•The more elevated BNP – the more severe the CHF
What is an Electrocardiogram? (EKG)
looks for abnormalities in the heart's electrical impulses using electrodes
•Records the electrical impulses that stimulate the heart to contract
•Used to evaluate arrhythmias, conduction defects, myocardial injury and damage, left and right hypertrophy, and pericardial disease
What is an ECHO Cardiogram?
is an ultrasound of the heart that provides moving pictures and provides information on the structure and function of the heart.
•A noninvasive ultrasound procedure used to evaluate the structure and function of the heart & how they move blood through the heart
•Used to detect heart wall function, specifically left ventricle function
•Used to detect disease of heart valves
Determines cardiac output & ejection fraction
What are some nursing interventions used for cardiovascular disease?
Patient Teaching
Diet
Weight loss
Exercise
Modifiable & non-modifiable risk factors
quitting smoking
substance abuse
reduce stress
What the nurse can do:
•Manage Anxiety
•Promote Venous Return
•Promote Peripheral Arterial Circulation
•Prevent Clot Prevention
•Administer Medications
What is heart failure?
•Heart becomes inefficient pump
•Unable to circulate blood to organs & tissues
•Leads to systemic and pulmonary edema
•Results in fatigue and organ dysfunction
What is Right Heart Failure?
This causes blood to build up in the veins (the blood vessels that carry blood from the organs and tissue back to the heart). The increased pressure inside the veins can push fluid out of the veins into surrounding tissue. This leads to a build-up of fluid in the legs, or less commonly in the genital area, organs or the abdomen (belly).
PERIPHERAL VENOUS CONGESTION
PERIPHERAL S/S
•Peripheral Edema of lower extremities, feet
•Ascites – edema of abdomen
•Jugular vein distention (JVD)
•Weight gain from build up of fluid
•Fatigue* (any chronic heart disease)
•weakness
•Exercise intolerance
•Lack of appetite
What is Left Heart Failure?
•As a result, blood builds up in the pulmonary veins (the blood vessels that carry blood away from the lungs). This causes shortness of breath, trouble breathing or coughing – especially during physical activity.
LUNGS S/S
Cough, SOB
Wheezing, Crackles
Pink frothy sputum
Orthopnea, Dyspnea
PLUS THESE S/S
Tachycardia
Mental confusion, change in LOC
Fatigue* (any chronic heart disease)
weakness
Exercise intolerance
Lack of appetite
What is Peripheral Arterial Disease? (PAD)
is a condition characterized by narrowing or blockage of the arteries in the limbs (usually the legs) due to atherosclerosis, leading to reduced blood flow and potential complications such as pain, numbness, or tissue damage.
ARTERIAL
•Pale or bluish (cyanotic)Legs/feet
•Weak or absent peripheral pulse
•Cool Legs / Feet
•Loss of hair in lower extremities
•Thick toenails
•Paresthesias
•Un-healing wounds on toes, feet
What is Intermittent Claudication?
pain in legs with exercise, especially walking, relieved with rest – tissue is ischemic, ischemic tissue is painful
What are some interventions for Peripheral Arterial Disease (PAD)?
•Interventions: *keep legs down in dependent position, if legs are hanging down gravity helps blood flow to lower extremities
•If patient has intermittent claudication, have them sit and rest
•Patient Teaching:
pt has CAD
•Regular exercise
•Diet
•Weight Loss
•Exercise
•Modifiable & Non-modifiable Risk Factors
•Quitting Smoking
•Substance Abuse
•Reduce Stress
Foot care
What is Peripheral Venous Disease? (Venous insufficiency)?
involves damaged or blocked veins that carry blood from the hands and feet back to the heart. While peripheral venous disease can occur anywhere in the body, it is most often seen in the arms and legs.
•Edema - Pitting or non-pitting
•Incompetent valves in veins (valves do not close and blood leaks back down and pools)
•Varicose veins (veins are enlarged, twisted, swollen, and overfilled with blood)
•Brownish red discoloration of lower extremities (hyperpigmentation due to poor blood flow, breakdown of blood hemoglobin [iron in rbc])
•Ulcers on lower extremities
What are some interventions you can do for patients with PVD? (peripheral venous disease)?
•Promote Venous Return
•Encourage patient to ambulate – contracting leg muscles help to push venous blood back to heart
•When patient not ambulating, have patient elevate legs or sit in a recliner – keeping legs elevated or up uses gravity to help return blood to heart - Encourage leg/ankle exercises.
•Instruct not to cross legs
•Can use compression stockings, or possible venodynes (alternate compression devices)
How to remember PAD?
•Keep legs DOWN to get more blood to lower extremities
Leg artery blockages, decreased blood flow, leg pain with walking.
Intermittent Claudication: leg pain during exercise due to reduced blood flow
How to remember PVD?
•Keep legs ELEVATED (up) to facilitate venous return back to heart
•Regular exercise is beneficial – the exercise causes contraction of the leg muscles which helps to push venous blood back to heart
•If unable to walk or exercise encourage leg exercises
How can you promote venous circulation and what does that do for you?
•Adequate circulation ensures that oxygenated blood reaches tissues and organs and that venous blood returns to heart
PROMOTE VENOUS RETURN
•Elevate legs above level of heart
•Encourage and support early and frequent ambulation
•Anti-embolism stockings, sequential compression devices
•Encourage or provide range of motion, ankle circles, “calf pumps”
•Teach patient not to cross legs
•Anticoagulant
How can you promote arterial circulation?
•Teach smoking cessation
•Teach foot care
•Inspect feet daily for any signs of breakdown or potential breakdown
•Keep feet clean and dry
•Teach patient to wear well-fitting shoes with smooth dry socks
•Regular exercise improves circulation
•Prevent long periods of exposure to cold (causes vasoconstriction)
What is Hypovolemia?
Fluid Deficit
Causes:
Inadequate fluid intake
Active fluid loss
Increased metabolic rate - Fever - Infection
Failure of regulatory mechanisms
Fluid shifts - Burns
could possibly be dehydration
What is Hypovolemic shock?
a life-threatening condition characterized by a severe decrease in blood volume (hypovolemia) due to excessive fluid loss, leading to inadequate perfusion of vital organs and tissues, resulting in symptoms such as low blood pressure, rapid heart rate, altered mental status, and cold, clammy skin.
What are some Hypovolemia S/S?
•Sensations of thirst
•Dry mucous membranes
•Weakness, dizziness
•Poor skin turgor
•^ capillary refill time - >3
•Changes in LOC
•Acute Weight Loss
•Elevated BUN
•Na+ increased (>145)
•^ Hematocrit
•^ Urine Specific Gravity
•Oliguria <400ML/24HR
Vital Signs
Weak, thread pulse
Tachycardia
Tachypnea
Hypotension
Elevated temp
What are some nursing interventions for Hypovolemia?
Correct fluid volume status
IVF - Isotonic - 0.9% Normal Saline
Encourage Increased Intake of Oral fluids
Identify and treat cause - ie. Vomiting/diarrhea
Monitor VS & LOC
Daily weights
Monitor I&O
Monitor Lab values - Electrolytes
Medications
What is Hypervolemia?
Fluid excess
too much fluid in intravascular spaces (the spaces within the blood & lymph vessels)
Edema – excess fluid volume in interstitial spaces (The space between blood vessels and cells)
Causes:
•Excessive fluid intake
•Excessive Na+ intake
•Decreased Cardiac Output conditions
•Renal failure -
•Liver failure - ASCITES
•Malnutrition - LOW ALBUMIN - CKD
What is some Hypervolemia S&S?
S&S:
Weight Gain
Distended Neck Veins (JVD)
Dependent Edema or Pitting
Skin pale & cool
Crackles, dyspnea, ascites
Hemodilution: BUN, HCT, Urine Specific decreased
Mental status changes
LOW NA+ OR HYPOXIA
Vital Signs
Bounding pulse
Hypertension
raised RR rate
What are some nursing interventions for Hypervolemia?
•Correct fluid volume status
•ID and treat underlying cause
•Monitor VS & I&O
•Monitor weight
•Monitor mental status
•Skin condition (positioning)
•Monitor cardiac status
•Labs
•Medications: diuretics
•Electrolyte replacement
•Diet:
•Decrease Na+
•Fluid restriction
What could we teach the patient if they need a fluid restriction?
•Reserve liquids for between meals, not with meals
•Limit intake of foods that increase thirst
•Offer Ice chips
•Frequent oral hygiene
•Bring liquids in for medications then take away
•Do not leave liquids at bedside
What is Isotonic Fluid?
are used intravenously to restore fluid balance in patients who are dehydrated or need hydration support.
•SAME OSMOLARITY & TONE OF BLOOD
•DOES NOT MOVE INTO OR PULL FLUID OUT OF THE CELLS OR BLOOD VESSELS
•EXAMPLES = 0.9% NS & LR
•WHEN GIVEN IV, THE FLUID REMAINS IN THE INTRAVASCULAR COMPARTMENT
•AS A RESULT INTRAVASCULAR FLUID VOLUME INCREASES
•PREFERRED FOR IMMEDIATE RESPONSE FOR HYPOTENSION & HYPOVOLEMIA
•MUST ASSESS FOR FLUID VOLUME OVERLOAD.
What is the normal concentration of sodium in the blood?
Sodium Na+ 135 – 145 mEq/L
Sodium -
Resides in extracellular fluid
Regulates Fluid volume and blood volume
Helps maintain muscle contraction
Stimulates conduction of nerve impulses
examples of food with sodium
table salt, soy sauce, processed foods, canned products, cheese
What is Hyponatremia?
condition where the level of sodium in the blood becomes abnormally low, which can cause symptoms ranging from mild fatigue and confusion to more severe complications like seizures or coma.
What is the range of sodium to be “Hyponatremia”?
Na+ < 135
What are the causes, S&S of Hyponatremia?
Causes:
Diuretics
GI Fluid loss
Excessive intake of hypotonic
solution: water
S&S
Behavioral changes - AMS
Confusion - disorientation
ANV - anorexia, nausea, vomiting
Weakness
Lethargy
muscle cramps
seizures
What are some treatments of hyponatremia?
Treatment:
•Increase oral sodium intake
•Administer IV saline infusion
•When sodium levels in the blood are too low, extra water goes into body cells causing them to swell. This swelling can be especially dangerous for brain cells, resulting in neurological symptoms such as headache, confusion, irritability, seizures or even coma.
What is the range of sodium to become “Hypernatremia”?
Na+ > 145
What are some causes of Hypernatremia?
Cause:
•Excessive sodium intake
•Water deprivation
•Increase water loss through profuse sweating, heat stroke
•Administration of hypertonic tube feeding
S/S
•Thirst
•^ temperature
•Dry mouth, sticky mucus membranes
SEVERE!!!!!!!!!!!!!!!! S/S
Lethargy
Seizures
IRRITABILITY - DISORIENTATION - AMS
Hallucinations
What are some treatments for Hypernatremia?
•Restrict Na in diet
•Increase water intake
•Administer iv solutions that don’t contain sodium
•D5W - HYPOTONIC
What is the normal range of Potassium in the blood?
K+ 3.5 – 5.0 mEq/L
HOW!!! does a normal range of potassium benefit you?
•Maintains ICF osmolality
•Muscle contraction - helps muscles contract better
•Regulates conduction of cardiac rhythm* -
•Assists with acid-base balance