Immunoassay
1/14
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
15 Terms
COOMBS TESTING
The presence of inappropriate antibodies (i.e., antibodies against the body's own tissues) are detected with the Coombs test.
The direct Coombs reaction is used to detect antibody that has attacked the body's own erythrocytes. There are commercially available Coombs tests that can be performed in the in-house practice laboratory, but the test is more commonly performed at the reference lab. A positive direct Coombs test provides evidence of Immune-mediated hemolytic disease. The procedure involves incubating the suspect sample with antisera, which reacts with the species' immunoglobulins. If the erythrocytes in the sample are coated with immunoglobulin (self-antibody), then the antisera and immunoglobulin on the erythrocytes will react and result in visible agglutination of the erythrocytes.
Indirect Coombs testing detects circulating antibody. A positive indirect Coombs test result indicates the presence of circulating antibodies against the body's own tissues. To visualize the reaction, patient serum is incubated with erythrocytes from a normal animal of the same species. If antibody is present in the patient serum, it will bind to these erythrocytes just like it would to its own. The subsequent addition of an anti-gamma globulin for the species being tested results in hemagglutination.

IMMUNODIFFUSION
For immunodiffusion, patient serum samples that possibly contain antibodies and the antigen to these antibodies, which is supplied in the test kit, are placed in separate wells in an agar gel plate. Both components diffuse into the agar and form a visible band of precipitation when they combine. If no band forms, no antibody exists in the patient's serum sample, or the patient's antibody levels are insufficient to cause precipitation in the gel. Diseases that may be detected by immunodiffusion are equine infectious anemia and Johne disease.
RADIOIMMUNOASSAY
A competitive form of radioimmunoassay has primarily been used in research and diagnostic laboratories for many years. The test principle is similar to the competitive enzyme-linked immunosorbent assay (CELISA) technique except that a radioisotope is used in place of the enzyme. The assay typically consists of an antigen that is labeled with a radioisotope and an antibody. When combined with patient serum that contains the same antigen, both antigens compete for the antibody. With increasing amounts of patient antigen, more labeled antigen is displaced from the antibody. The remaining amount of radioactivity is measured and compared with a standard curve to determine the concentration of antigen in the patient's serum.
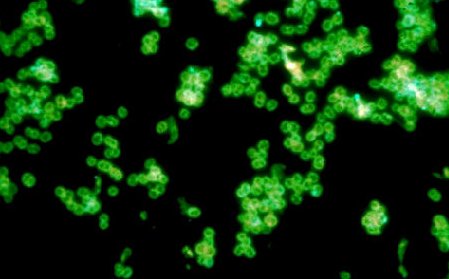
FLUORESCENT ANTIBODY TESTING
Although it is not commonly performed in veterinary practices, fluorescent testing is available at most veterinary reference laboratories. These test procedures are frequently used to verify a tentative diagnosis that has been made by the veterinarian. Two methods are available: direct antibody testing and indirect antibody testing. Both of these detect the presence of specific antibody in a sample. In the direct procedure, the patient sample is added to a test slide that has been precoated with a fluorescent-dye-conjugated antigen. The dye combines with a specific antibody if it is present in the patient sample. The slide is then examined with a special microscope that has been designed for fluorescent microscopy. For cellular antigens, the cell will appear to be outlined with fluorescent material. With an indirect fluorescent antibody (IFA) technique, the patient sample is incubated on a slide that contains the specific test antigen. The slide is then washed to remove any unbound antibody. Fluorescent-labeled antiantibody is added to the system, and the slide is then microscopically examined. Any fluorescence indicates a positive test result. Fluorescent techniques exist for antigen detection as well.
Antibody Titers
Although they are not routinely performed in all veterinary practices laboratories, antibody titer tests may be needed by the clinician to distinguish between active infection and prior exposure to certain antigens. This is particularly important when no reliable antigen test is available. titer refers to the greatest dilution at which a patient sample no longer yields a positive result for the presence of a specific antibody. The test as it is performed in the reference laboratory requires the making of serial dilutions of a sample. Each dilution is then examined for the presence of the antibody. The reciprocal of the greatest dilution that still elicits a positive test is the titer. A high titer often indicates active infection. Low titer usually indicate previous exposure to the specific antigen. Recently, a number of titer kits have been made available for use in the in-house veterinary practice laboratory. The tests primarily use enzyme-linked immunosorbent assay (ELISA) technology, and they provide rapid and accurate results. Some clinicians will request these tests when determining the need to vaccinate a patient.
Molecular Diagnositics
Leptospira spp. a slow growing bacteria on a culture plate, are one of many bacteria that can now be identified with the use of molecular diagnostic testing. The DNA molecule of this bacteria, which contains its genetic information, is the molecule of interest for the test. Molecular diagnostic testing is based on the analysis of DNA or RNA. Veterinarians can send samples out to be tested in a short amount of time via methods that are too sophisticated for use in veterinary practices. Many of the state veterinary diagnostic laboratories now offer several molecular tests. The obvious use for the veterinarian is to identify the presence of pathogens such as viruses, fungi, or bacteria, but there are many other uses for this technology. The branches of medicine and science that use these types of DNA tests include microbiology, genetics, immunology, pharmacology, forensics, biology, food science, agriculture, archaeology, and ecology. DNA tests are available to classify cancers, detect genetic defects, verify animal pedigrees, and determine bacterial contaminants in food science applications, to name but a few uses. The advantages of these kinds of tests are increased sensitivity and increased specificity. The amount of specimen needed for the test can be exceedingly small. The tests are safe, and many factors that influence other procedures-such as the age and condition of the sample, fastidious growth requirements, and the viability of the organism-are not as crucial with molecular diagnostic tests. The newer techniques also have faster turnaround times. Whereas the traditional identification of a bacterium may take 2 or 3 days or more, molecular diagnostic testing can be accomplished in a matter of hours, depending on the test. Disadvantages include contamination that leads to false-positive results, the high level of technical expertise needed to run the tests, the need for more than one room in which to perform the tests, and high costs, Many of these problems are being solved, and commercial kits and automated instruments are making these tests available to clinical diagnostic laboratories. Many varieties of molecular diagnostic tests are available, but perhaps the most familiar, is the PCR. This test detects the DNA segments of interest in the specimen submitted and amplifies its amount.
Reverse Transcriptase Polymerase Chain Reaction
Sometimes RNA is the nucleic acid used for the molecular test, such as when testing for RNA viruses. The process used is called reverse transcriptase PCR. It is similar to PCR, but the single-stranded RNA must first be converted to double-stranded DNA before the PCR process can continue.
Real-Time Polymerase Chain Reaction
Another significant test is real-time PCR. Compared with PCR, this method decreases the risk of contamination, is more easily automated, and is generally faster and easier to run. A fluorescent probe is added to the sample mix. This probe attaches to the DNA segments; as the quantity of segments is amplified, fluorescence increases. At a set amount of fluorescence, the sample is considered positive.
Polymerase Chain Reaction
PCR is called an amplification assay because a small amount of a DNA segment detected in the sample is amplified to run the test better and to determine the results. In other words, a PCR test produces many copies of a small, select region of the DNA molecule. Before performing the test, the nucleotide sequence of this section of DNA must be known so that the proper reagents are used. The region of the DNA that will identify the virus or bacterium is predetermined. The amplification process consists of three basic steps: denaturation, annealing, and extension. After amplification, the DNA segments are separated on an electrophoretic gel for identification. The sample mixture contains the specimen with the original DNA in question (if present), primers, nucleotides, and Taq DNA polymerase.
Denaturation
The sample is heated to break apart the double-stranded DNA molecule into two separate strands. Each strand serves as a template to which new nucleotides will attach.
Annealing
The temperature is lowered to cause the primers to bind anneal) to the separated strands. Primers mark the beginning and the end of the section of DNA to be copied. This will only happen if DNA is present in the sample that is complementary to the primers.
Extension
The temperature is raised once more, and the Taq DNA polymerase (the enzyme that can read the DNA code and assemble the nucleotide bases to form new complementary strands) causes new DNA segments to be produced (extended). Portions of two DNA molecules have been obtained, each with two strands. They are not the complete DNA molecule, but they do contain the desired segment. This process is repeated 25 to 30 times in an automated thermal cycler (Fig. 53.7). The timing, temperature, and number of cycles are regulated by the instrument. The amount f DNA segments produced is far greater than the original amount of DNA in the specimen. This is why PCR is useful for detecting minute quantities of the unknown in a mixed specimen. Finally, to see if the microbe was present in the specimen, agarose gel electrophoresis is used. The DNA segments are negatively charged particles and will move along the gel toward the positive electrode when a current is applied. The segments separate according to size, and they appear as separate bands on the gel. Controls are run at the same time as the test samples. By knowing the identity of the control bands, the test bands can be compared and identified. The interpretation of PCR tests must be done carefully. A microbe may be present in the sample but may not be the cause of the patient's disease. As with any laboratory test, the results must be evaluated along with all of the other information from the clinical case.
Intradermal Tests
Skin tests are used to diagnose various allergies to allergens in the environment. Allergies are mediated by immunoglobulin E (IgE) antibody molecules. They can be detected by using allergenic extracts of grasses, trees, weed pollens, molds, dust, insects, and other possibly offending antigens. The extracts are injected intradermally, and the injection sites are monitored for allergic reactions. A positive reaction appears as a raised welt and means that the animal is allergic to that antigen.
Patients with hypersensitivity reactions may manifest with urticaria (hives), wheals, or angioedema (edema of the dermis and subcutaneous tissues). These reactions are triggered when basophils or mast cells release their histamine-containing granules and trigger the inflammatory response. Many substances and environmental parameters have been demonstrated to cause urticaria and angioedema.
Allergens are chosen on the basis of the patient's history and geographic area. Common allergens include dust mites, house dust, human dander, feathers, molds, weeds, grasses, and trees.
Intradermal skin testing for food allergens has not been well validated. Dogs are frequently allergic to more than one substance. False-positive and false-negative reactions can occur for a variety of reasons.
When performing the test, the patient is placed in lateral recumbency, and the hair is shaved from the lateral thorax. The skin is not scrubbed. A felt-tip marker is used to mark the injection sites, which should be 2 cm apart. A 26-gauge needle is used to inject a small volume (generally 0.05 mL) of suspected individual allergens. Most patients tolerate the injections well and do not require sedation. An intradermal injection of saline is used as a negative control, and an injection of a histamine product is used as a positive control. The injection sites are then evaluated at 15 and 30 minutes after the injection, and the reactions, if any, are graded. The saline injection is graded as 0, and the positive control is graded as +4. The test sites are scored in relation to the two controls. Each test site is evaluated for the presence of erytherna. The diameter of each wheal should be measured
enzyme-linked immunosorbent assay (ELISA)
available for the determination of allergen-specific IgE antibodies in dogs, cats, and horses (ALLERCEPT, Heska, Loveland, Colorado). The test uses a high-affinity IgE receptor and is available for testing dozens of grasses, trees, weeds, mites, insects, and fungi
Tuberculin Skin Test
correlates with a specific cell-mediated immune reaction. Animals infected with Mycobacterium spp. bacteria develop characteristic delayed hypersensitivity relations when exposed to purified derivatives of the organism called tuberculin. The test is commonly performed on cattle and primates. For the tuberculin skin test, tuberculin is injected intradermally at a site in the cervical region or in a skinfold at the base of the tail in large animals. A delayed local inflammatory reaction is observed if the animal has been exposed to Mycobacterium, The reaction to injection is delayed because a day or more passes before the T lymphocytes migrate to the foreign antigen injected into the dermis.