Cornea
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Symptoms: Redness, lacrimation, photophobia, and slightly decreased vision.
Superficial punctate keratitis: corneal inflammation resulting in epithelial loss or damage.
Plan: if mild-mod - PFAT QID + gel + d/c contacts
Non-CL severe: ointment like Polysporin bacitracin/polymyxin 5 days, cyclo 1% TID for pain.
CL wearer severe: fluoroquinolone or aminoglycoside QID plus ointment and cyclo.
sudden/severe Pain when waking up in the morning, tearing, photophobia, redness, FB sensation
Recurrent corneal erosions: corneal epithelial breakdown, leading to pain, tearing, and sensitivity to light. Associated with trauma, BM dystrophy, dry eye.
Plan:
Erythromucyin ointment QID + oral doxycycling 50mg BID
Cyclopentolate 1% TID
PFAT QID
FML 0.1% BID for 2 weeks
Additional: Bandage CL, stromal micropuncture, debridement, phototherapeutic keratectomy - used in corneal scarring, RCE, corneal dystrophy, surface opacities. (excimer laser to treat corneal irregularities and improve vision)
RTC 2 days then 2 months.
Foreign body sensation, Eye irritation, Pain, Redness, and Blurred vision (in severe cases)
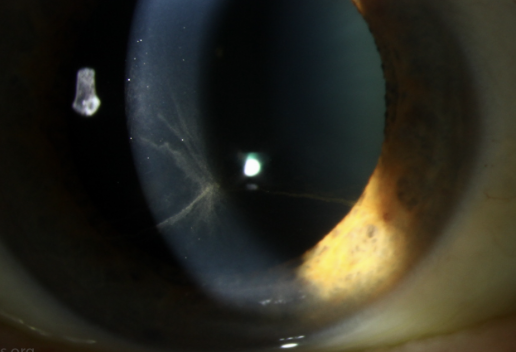
Filamentary Keratitis: caused by chronic corneal inflammation usually from dry eyes -> degenerated epithelial cells + mucous attached to create the filaments. Assocuated with dry eye, ocular infla, CL wear.
Plan:
debride filaments with Q-Tips and anesthetic
PFAT 6-8x a day + lubricating gel + punctal plugs
Acetylcysteine 10% QID (Dissolve mucus plaques)
RTC 1-4 weeks. Consider BCL if not better
Foreign body sensation, Eye irritation, Pain, Redness, and Blurred vision (in severe cases)
Exposure Keratopathy: corneal damage caused by prolonged exposure of the eye to the environment, often due to incomplete or inadequate eyelid closure, leading to dryness and potential complications.
Plan: treat underlying dx (CN7 palsy, TED, floppy lid syndrome, hx of lid surgery)
LUBRICATE: PFAT q4hrs, punctal plugs , lubricating ointment
Tape lids, can have gold weight in lid to keep them down
IF severe can use amniotic memrane
RTC 2 days if severe (to look for ulcer development), or 2 months if not severe.
Reduced or absent corneal sensation, Blurred vision, Dry eyes, Eye pain or discomfort, Sensitivity to light, may have white spot on eye
Neurotrophic Keratopathy: damage to the nerves that innervate the cornea, leading to a loss of corneal sensation and subsequent epithelial breakdown.
Causes: viral infection (HSV), trauma, chemical burns, Diabetes, MS
Objective: Corneal ulcer without infiltrate. Heaped up border. Oval in lower cornea.
Plan:
Mild: AT's and ointment. Punctal plugs.
Small defect: Erythro or bacitracin ointment QID
Mod: AT's, BCL, fluoroquinolone drop QID.
Antibiotic ointment Q2H.
Severe: Oral doxy 50mg bid, atologous serum.
Oxervate/Cenegermin human growth factor, scleral lens.
tarsorrhaphy, amniotic membrane.
Descemetocele: serious condition where Descemet membrane (a layer of the cornea) protrudes or bulges forward due to thinning of the corneal stroma, often caused by a corneal ulcer, and requires prompt intervention to prevent perforation
Causes of corneal ulcer: Microbial keratitis, neurotrophic keratopathy, dry eye disorders, and corneal inflammation (sterile ulcer) associated with immune-mediated disorders can lead to corneal ulcers
Plan: Refer for penetrating keratoplasty
Eye pain
UV keratopathy: temporary, painful eye damage from exposure to ultraviolet light that usually resolves on its own within a few days.
Plan: Cyclo 1% BID, antibiotic ointment 4-8 times per day for 7 days, oral pain killer.
-Alt: BCL with antibiotic drop.
Thygesons superficial punctate: chronic condition that comes and goes causing both eyes to have raised lesions in the center part of cornea resulting in dry eyes.
Plan: FML 0.1% or loteprednol 0.5% QID, slow taper. Optional BCL.
RTC 1 week then 3 months. Monthly if on steroid. Consider Restasis 0.05% BID or Xiidra 5% BID for further treatment if needed
Things that look like pterygium
CIN (conjunctival intraepithelial neoplasia) - abnormal changes in the cells of the conjunctiva that could convert to SCC
Limbal Dermoid - disruption in fetal development, leading to the trapping of skin cells, tissues, and glands creating a cyst between cornea and sclera
Corneal Pannus: growth of new blood vessels (neovascularization) into the cornea, the clear front part of the eye. Associated with chronic infla, injury, CL wear, hypoxia
asymptomatic. If central, vision may be affected. Ocular irritation (can develop if thick calcium plaques flake off and cause an epithelial defect.)
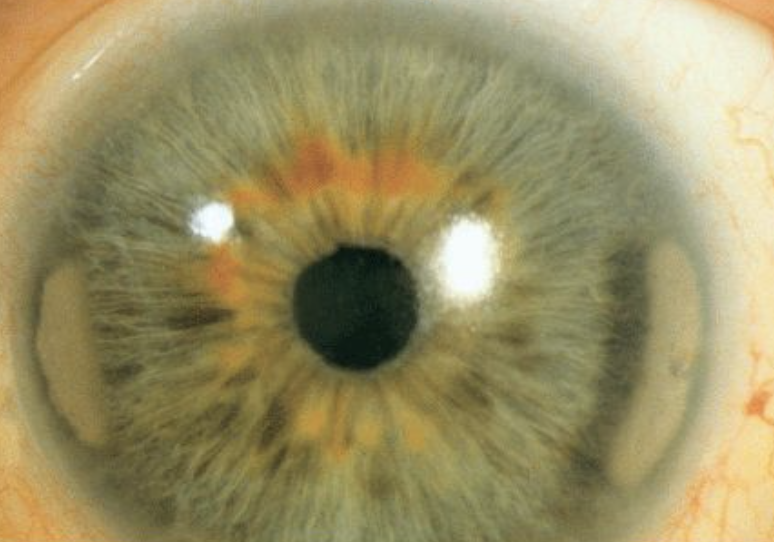
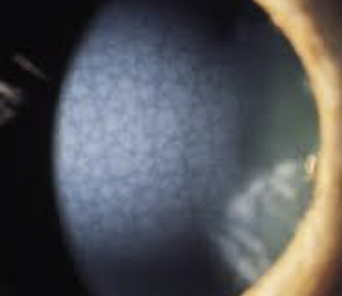
Band Keratopathy: calcium deposits forming a band-like appearance across the cornea (bowmans). May cause vision impairment or irritation.
Causes: Chronic uveitis, JIA, interstitial keratitis, corneal edema, phithsis bulbi, glaucoma, retinal surgery, renal failure
Objective: not at limbus (thin line of clear cornea), begins at 3/9 oclock, swiss cheese appearance
Plan:
Mild: Lubricants
Moderate: EDTA 3% chelation with cotton swab. Put on 10-60 minutes, saline rinse.
If epi defect: Antibiotic drop QID and ointment (if epi defect), cyclo 1%, BCL.
Severe: Consider PTK

Keratitis - Pain, Redness, Reduced visual acuity, Photophobia, Discharge
Keratitis is inflammation of the cornea.
It may result from infective or non-infective causes
Infectious keratitis can be classified as microbial keratitis (bacterial, fungi or protozoal) or viral keratitis (herpes viruses).
Bacterial keratitis represents the most common form of microbial keratitis
Risk factors: CL use, trauma, dry eye, lid disease, eye surgery
Objective: conj injection, corneal opacity
culture ulcer if 3mm or greater, 2 or more infiltrates, 1 mm from axis. !!!
Viral Keratitis: Herpes Simplex (cold sores or genital herpes), Zoster (chickenpox and shingles)
Primary infection: direct contact with infected secretions or lesions
Reactivation/ recurrence: systemic illness, trauma, sunlight, stress

Bacterial: White infiltrate in stroma with associated epithelial defect. Mucopurulent, stromal edema, descemet folds, AC reaction, UL edema, post synechiae, inc IOP, hypopyon
Plan: avoid steroids if active epi disease, 1% cyclo BID, Fluoroquinolone Q2H. discontinue CL wear
RTC daily
Fungul Keratitis: Satellite lesions/feathery edges, injection, mucopurulent, AC reaction, hypopyon.
Plan: Natamycin 5% or amphotericin 0.15% Q1-2H around the clock
Escalation: Oral fluconazole, epithelial debridement. Hospitalize
Acanthomoeba: PHMB 0.1% or chlorhexidine 0.02% Q1H. Oral antifungal itraconazole. RTC 1 day
Escalation: hopitalize
Noninfectious cause of corneal ulcer
Eye injuries. Burns, scratches (corneal abrasions), cuts (lacerations) and punctures can all lead to ulcers when they don’t heal correctly. They also make your eyes more vulnerable to infections, which can lead to corneal ulcers forming.
Exposure. If you can’t close your eyes fully (a condition called lagophthalmos), that leaves your corneas exposed for much longer than they should be. This can lead to corneal surface damage. Your corneas are also vulnerable to exposure damage in very hot or cold conditions.
Very dry eyes. This can be because of weather conditions, eye conditions or a combination of the two.
Toxic effects. These can be from toxic substances or, more rarely, from medications you’re taking.
Immune conditions. Sometimes, eye inflammation happens because your immune system malfunctions. That inflammation can weaken your corneal tissue, making it vulnerable to damage and ulcer formation
risk factors:
Contact lenses that you wear often or for long periods (especially if you sleep or swim with them still in, or don’t maintain them properly).
A current or past herpes simplex virus infection or varicella-zoster virus infection.
Dry eyes.
Conditions that make it harder or impossible to fully close your eyes (including different types of facial paralysis like Bell’s palsy, or conditions that make your eyes bulge, like Graves’ disease).
Steroid-containing medicated eye drops that you’re currently using or recently used.
An injury or burn on your cornea.
Type 2 diabetes.
A history of eye surgery.
A history of other eye diseases, especially corneal diseases.
Complications:
Astigmatism or other vision changes.
Cataracts.
Endophthalmitis.
Glaucoma.
Perforated or scarred cornea.
Recurrent corneal erosions (RCEs).
Vision loss.

Corneal opacification: occurs when the cornea's transparency is lost, often due to scarring or edema, disrupting the regular arrangement of collagen fibrils and leading to light scattering/opacification
Scar tissue, which can form after injury, infection, inflammation, or neovascularization is composed of irregular collagen fibers that disrupt the cornea's normal structure and transparency
Swelling of the cornea, or edema, can cause a loss of transparency by disrupting the spacing and arrangement of the collagen fibrils
Corneal hydrops, a serious complication of keratoconus, occurs when a tear in Descemet's membrane allows fluid from the eye to leak into the corneal stroma, causing swelling and clouding
Peter's anomaly or sclerocornea, can cause corneal opacification due to abnormal development of the corneal layers during embryogenesis
Dry Eye: Burning, itching, increased blinking, photophobia, CL intolerance
Aqueous deficient: Cause:
Sjogrens or non-sjogrens
lacrimal dysfunction or secondary – ABC (attacked gland, blocked gland, cut nerves)
Evaporative:
intrinsic cause – MGD, lid position issue, low blink rate
Extrinsic – dec Vitamin A, CL wear, topical preservatives
pain, redness, serous discharge, tearing, photophobia, dec vision, dec corneal sensitivity bc V1 compromised
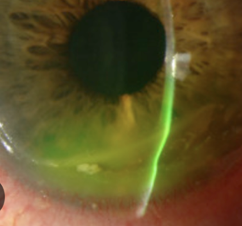
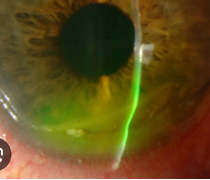
Herpes Simplex: Leading infectious cause of blindness in US and most common virus in humans (cold sores T1, or genital herpes T2). Usually dormant in trigeminal nerve but eruptions occurs, triggered by stress, sun, fever etc. 25% who get HSV keratitis will have inc likelihood of recurrence.
Signs:
skin lesions adjacent to eyes - vesicles/pustules that crust over and heal – earliest sign.
Uni follicular conjunctivitis, preauricular Lymphadenopathy.
Ulcers: Dendrites, can have geographic ulcer wider than dendrite AND marginal ulcer.
Uveitis and acute retinal necrosis
Intersitial keratitis and endotheliitis present similarly - stromal opacity
Side note: endotheliitis, either secondary inflammation caused by the virus and/or direct infection of endothelial cells is thought to cause endothelial dysfunction and subsequent stromal edema and opacity.
interstitial keratitis - associated with corneal neovascularization, and recurrent episodes can lead to irreversible stromal scarring and vision loss.
Most commonly associated with syphilis or viral infections - treat with steroid pred forte 1% q2-6h + treat underlying condition
RTC if active 3-7 days then 2-4 weeks. Taper steroid. If inactive then annual
Workup: Immunoassay (Herpchek), RPS HSV detector, NAFL stain
Plan: Oral acyclovir 400mg 5 times per day with ganciclovir 0.15% 5 times for 7-10 days.
If ulcer/stroma, Acyclovir 800mg 5 times per day
If IK/endotheliitis: add Pred forte 1% QID with slow taper.
RTC 2-7 days
malaise, tingling, fever prodrome.
Back and shoulder pain
Vesicular rash that respects midline (when active)
Post-herpetic neuralgia (pain that persists beyond one month of rash onset or resolution.)
Herpes Zoster: Reactivation of VZV virus (shingles - painful rash with blisters), which remains dormant in nerve cells after a previous chickenpox infection. Factors that reactivate include weakened immune system, stress, aging, steroid meds.
Objective: Pseudo dendrite (Zoster– tapered ends, thick, elevated, ropy, can wipe off). Hutchinson sign. similar ocular presentation to HSV
Plan: acyclovir 800mg 5x a day and ganciclovir 0.15% 5 times for 7-10 days., hospitalize if severe.
If uveitis: cyclopentolate 1% BID, pred forte q3h, timolol BID if inc pressure
Conditions that cause this
Interstitial keratitis: inflammation of the middle layers of the cornea, often linked to infections (HSV, late complication of congenital syphilis) or autoimmune responses (Cogans syndrome, RA, lupus, sarchoid) and corneal neovascularization.
Other infection causes: Lyme, TB (PPD, IGRA, chest x-ray), Epstein-BArr Virus
Plan: Pred forte 1% 6-8 times per day with slow taper.
RTC: if active 3-7 days then 2-4 weeks. Taper steroid. If inactive then annual
Cogan’s Syndrome: Autoimmune disease causing infla of inner ears and eyes. (IK, vertigo/hearing loss, vasculitis → muscle aches/pain)
Plan: treat IK
Phlyctenulosis: Hypersensitivity to staph bleph or tuberculosis resulting in white nodule at limbus. Can progress to epi ulceration and migrate to central cornea with neo. Can scar so need to treat if progressed.
Plan: Tobradex QID, lid hygeine if bleph, AT
Escalation: Doxy 100mg BID, can add cyclosporine
RTC 14 days to taper steroid
CL Complications!!
CLARE: Contact Lens-induced Acute Red Eye - inflammation from CL complication
Red, edema, iritis, stromal infiltration.
Plan: Discontinue contacts then refit into flatter lens with higher DK. Tobradex 0.3%/0.1% oph suspn QID 10 days
Steroid if infiltrate
Tight lens syndrome: CL too tight causing inflammation and discomfort. Occurs 1-2 days after dispensed CL
Objective: corneal edema, SPK, AC reaction, sterile hypopyon, no movement on blink.
Plan: refit contact with flatter lens with higher DK. Avoid sleeping with lenses
Corneal neo from CL - from lack of O2 to the cornea cause fragile BV development. Asymptomatic
Objective: 1mm superficial neo is fine.
Plan: Pred Forte 1% QID then taper. Inc DK, flatten lens.
Dimple Veiling: too steep contact lens causing CO2 bubbles to be trapped under lens causing indentation on epi.
Symptoms: asymptomatic/irritation/tear/blur
Plan: Resolves if remove lens for a while
Flatten lens, dec OAD, dec optic zone. Helps tear flow
Mucin Ball: mucin/protein/lipids balls form between CL and epi. Occurs if too flat or on CL that are EW.
Plan: steeper BC, decrease wear time and add re-wetting drops. NaFl will pool but not stain sincei its raised
Protein deposits: Superficial, white, translucent on CL surface. Protein integrated into high water content of lens. can cause GPC.
Plan: for GPs use enzyme-based cleaning solutions or hydrogen peroxide cleaning systems. For SCL daily rub and rinse and store well with multipurpose solution.
Jelly Bumps: Calcium protein complex on CL due to scratched/ridged/ polishing error/ or hydrophilic lens
Plan: replace lens
Giant papillary conjunctivitis: inflammed lid casued by excessive CL movement/ high riding lens / CL coating. Feel contact lens a lot more due to the bumps on conj.
Plan:
Mild: Refit contacts/switch to dailies/reduce wear time/ clean with hydrogen peroxide
Moderate/severe: d/c contacts for 1-4 months then refit to dailies. + FML 0.1% then taper + pataday BID
RTC 2 weeks, continue being on Pataday BID long term
DDx:
Vernal KC (bilateral/allergy/trantas dots/shield ulcer)
Atopic KC (atopy hx, papillae mostly lower lid)
INFLAMMATION, painful, unilateral
Moorens ulcer: inflammation of BV at limbus Associated with hepatitis C
Objective: White marginal infiltrates that develop into a chronic serpiginous limbal ulceration over 3-12 month (peripheral crescent grey infiltrate → ulcers).
does not involve sclera unlike Peripheral ulcerative keratitis - CT disease related to RA/SLE/ etc. (PUK can be asymptomatic/pain/red/scleritis/episcleritis). Contact rheumatology. PUK below. Plan: Immunomodulator like cyclosporine, doxycycline, oral steroid,
Plan: Responds poorly to steroids, may speed perforation. Refer to specialist for excision/reconstruction

acute photophobia, pain, tearing
Staphylococcal Marginal Keratitis: overactive immune response causing sterile ulcer to form.
Objective: corenal stroma infiltrates at 2,4,8,10
Plan: Self resolves in 3-4 weeks if left untreated. Tobradex qid if symptomatic


Pain, dec VA, irreg astigmatism, bilateral, NO INFLAMMATION
Terrien’s marginal Degeneration: non-inflammatory eye condition that causes thinning of the peripheral corneal stroma, typically in the superior or inferior quadrant. Idiopathic
Objective: may have neo (superiorly), yellow line on cornea. anterior stromal opacities, leaving a clear area between the opacities and the limbus
Plan: topical steroid for pain and inflam, lubricant, keratoplasty. Avoid trauma bc can rupture easily.

Bilateral, reduced VA, dry eyes
Salzmann Nodular Degeneration: chronic inflammation causing small, gray-white or bluish nodules to develop on the surface of the cornea. Associated with females.
Objective: RCE, Hyaline deposits in epithelium and Bowman’s → blue grey nodules in Midperiphery
Plan: Monitor 3-6 months. Treat corneal abrasion if present. Potential keratoplasty or use of amniotic membrane

Dellen: corneal thinning at lumbus with adjacent corneal or connj elevation. Results in poor tear speading → stromal dehydaration. Adjacent to heme, bleb, pterygium, tumor, strab surgery.
Plan: Lubricating drops or ointment AM and PM. Treat causative lesion. RTC 7 days
Asymptomatic, reduced vision, irregular astigmatism
Pellucid Marginal degeneration: collagen abnormalities causing thin weak area of cornea inferiorly in early adulthood.
Objective: bilateral inferior thinning, irregular astigmatism, can have hydrops
Workup: corneal topography - kissing grab
Plan: SCL/GP/scleral lens for irregular astigmatism.
corneal crosslinking if Kmax: 65D, VA 20/30 or worse, pach minimum >400 um, age less than 35. Contraindicated if current infection, past herpes infection, severe corneal scar or hx of poor wound healing.
Refer for keratoplasty (DALK or PKP) if indicated
treat hydrops if indicated
RTC 3-12 months

Sudden vision loss, painful, light sensitive
Hydrops: Occurs due to Descemet layer damage resulting in edema. Complication of pellucid and keratoconus and trauma/eye surgery. Can lead to scarring and reduced vision. May need corneal transplant if severe. Most resolve within a few months with proper treatment at proper times.
Plan: Descemet heals in 3 months. During the 3 months, need to reduce risk of scarring by using Muro 5% BID, brimonidine 0.1% BID, steroid if neo and eye shield.
RTC 4 weeks
Frequent changes in Rx, hx of eye rubbing, progressive reduction of BCVA. ghost image/monocular diplopia, hx of asthma/allergies/atopia
Keratoconus: non inflammatory, progressive thinning and bulging into a cone-like shape, causing distorted vision.
Objective:
Early signs: Fleischer ring, scissor reflex, inferior steepening
Late: Vogt’s Striae, Hydrops, Munson sign, Rizzuti sign
Mild: <48D, Mod: 48-54D, Severe: >54
workup: Corneal topography

Plan: SCL/GP/scleral lens for irregular astigmatism.
corneal crosslinking if Kmax: 65D, VA 20/30 or worse, pach minimum >400 um, age less than 35. Contraindicated if current infection, past herpes infection, severe corneal scar or hx of poor wound healing.
Refer for keratoplasty (DALK or PKP) if indicated
Treat hydrops if indicated
RTC 3-12 months
Random corneal findings, asymptomatic
Furrow degeneration: bilateral thinning in or adjacent to arcus
Limbal girdle of vogt: bilateral age related chalk like opacity at limbus, aging

Cornea farinata - aging, bilateral flour dusting

Crocodile Shagreen - bilateral grey/white cracked pattern
Whorl keratopthy (CHAI T + Fabry)
Rust ring: metallic FB

Hudson Stahli line - iron deposit in lower third of cornea, older pt, associated with dryness

Stockers line - iron deposit, usually vertical, edge of pterygium
Ferrys line - filter bleb
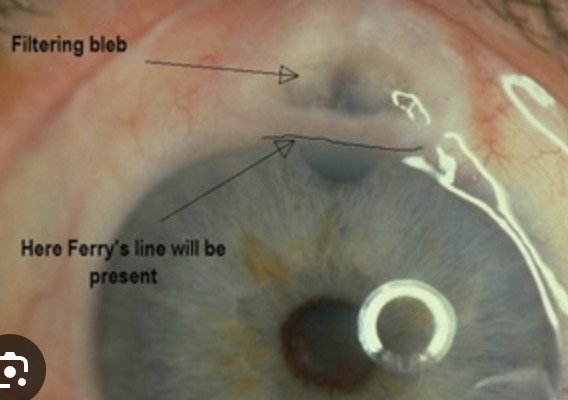
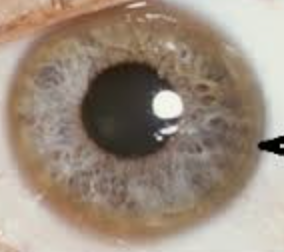
Kaiser Fleischer ring - copper accumulation in Wilsons disease
Band keratopathy: calcium deposits in bowmans layer
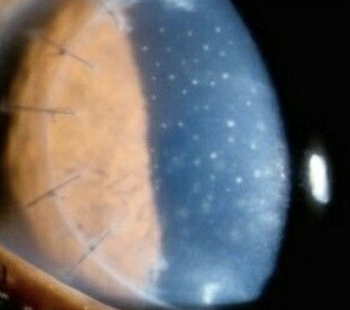
Khodadoust line: WBC in endothelium after transplant rejection

Krachmer’s spots: stromal injection (SEI) after transplant rejection
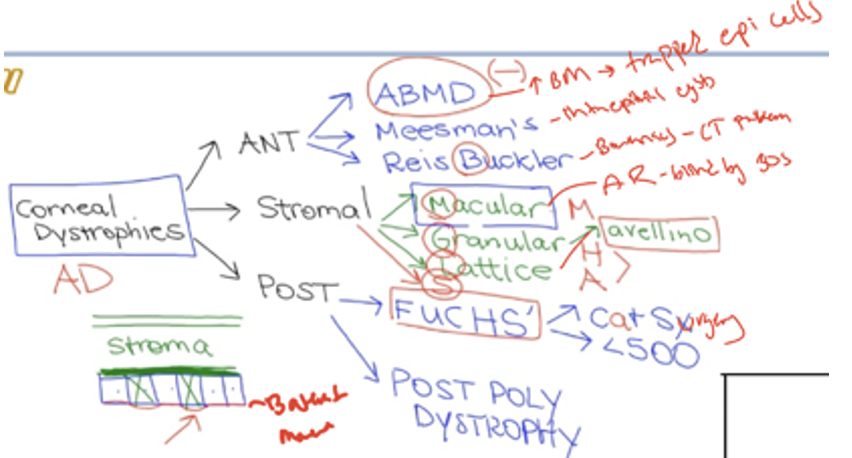
Epithelium Dystrophies
Epithelial Basement Membrane Dystrophy: Abnormal excessive basement membrane
Symptoms: irritation/fluctuating/reduced VA/glare/monocular diplopia
Hx of RCE with pain → inc risk of infection bc recurrent spontaneous RCE
Objective: Map = gray patch. Dot = white cyst. Fingerprint = refractile lines. RCE, shadowing, negative stain.
Plan:
Mild: Hypertonic Saline 5% (to reduce corneal edema) ung at night, PFAT PRN
Mod-severe (RCE plan) - Muro 128 q4h, Erythromycin ung QID, ketorolac 0.5% BID, cyclopentolate 1% BID. PTK
RTC:
Messman Dystrophy: Bilateral clear intraepithelial cysts spread diffusely across cornea
Symptoms: minor reduced VA. RCE around 40 - pain
Objective: irregular astigmatism
Plan: treat RCE if needed. Routine follow up
Reis Buckler’s Dystrophy: abnormal development of Bowman’s with collagen.
Symptoms: severe reduced vision in 20s and 30s
Objective: RCE or stromal opacification
Plan: Low vision aids + referral to corneal specialist for keratoplasty.
RTC yearly /PRN
Thiel Behnke: honeycomb opacities in Bowmans and stroma
Plan: PTK with excimer or PKP
Stromal Dystrophy
blurred vision, glare, and irregular astigmatism
Macular Dystrophy (AR) - diffuse central superficial stromal with grey opacities. Stromal haze by 5-9. Blindness by 20s
Plan: Low vision aids + referral to corneal specialist for keratoplasty.
Granular Dystrophy: small, white, crumb-like deposits to form in the cornea's middle layer.
Symptoms: VAs gradullay drop, Low vision by 60.
Objective rare RCE, spreads towards epi and deep stroma
Plan: Low vision aids + referral to corneal specialist for keratoplasty.
Lattice Dystrophy: deposition of amyloid resulting in steadily progressive loss of vision
Symptoms: blurred vision, glare, and irregular astigmatism. Low vision by 40s due to corneal scarring.
Plan: Low vision aids + referral to corneal specialist for keratoplasty.
Schnyder/crystalline dystrophy: white ring of crystals in stroma from high cholesterol. No symptoms
Plan: Refer for blood work up due to high cholesterol. Monitor yearly.
Endothelium/descemet dystrophy
Fuchs endothelial dystrophy: inc in post lamina production causing guttata on BM of endo. This results in dec endo cell (<500 cells/mm2) resulting in stomal edema. Female over 60
Symptoms. blurred/hazy vision. Early signs are glare/light sensitivity. Late signs: pain/edema
Objective: Guttata starting 20-30s, early cataract, inc irsk for POAG, >600 pachymetry. May have bullae or RCE
Plan: Hypertonic 5% NaFl drops and ung at night. Bandage SCL if bullae or RCE.
Congenital hereditary dystrophy - fuchs but EARLY onset - nystagmus (if AR, no nystagmus if AD), dec VA.
Plan: Hypertonic 5% NaFl drops and ung at night. AT, Low vision aids and keratoplasy.
Posterior Polymorphous Dystrophy: endo changes shape bc descemet pushes on it.
Symptoms: FB sensation, photophobia, dec vision, Pain if RCE
Objective: Cloudy cornea at birth, slow progression, corectopia, ectropion, glaucoma bc PAS from endo cells spreading to angle
Plan: Hypertonic 5% NaCl drops and ung at night. Bandage SCL, RCE treatment, Secondary glaucoma treatment

Foreign body sensation, blur, pain, tearing, red, Hx of cataract surgery
Bullous Keratopathy: blister-like swelling (bullae) of the cornea due to corneal endothelial dysfunction, leading to fluid accumulation and vision impairment
Objective: Corneal edema, bullae, Descemet folds, sub-epi haze, corneal neo, gutatta. Might even be cystoid macular edema
Workup: Stain, IOP, mac oct (RO CME)
Plan: Muro 128 ung and gtt. Timolol to reduce IOP (avoid prostglandin)
Plan if ruptured: treat epithelial defect with moxifloxacin, BCL, cyclo
1-3 days for bullae. 7 days initially then 1-6 months
Escalation: PTK, amniotic membrane, DSEK
recent LASIK
Epithelial ingrowth following LASIK enhancement. More susceptible with EBMD and flap trauma.
Plab: lift and clean at flap. YAG laser at the spot
A, B, and E: Posterior embryotoxon (yellow arrows), increased intraocular pressure in the right eye. C: Iris transillumination and atrophy (red arrow). D and E: High iris strands adherent to the posterior embryotoxon, ranging from fine threadlike strands to broad bands of iris tissue (green arrows)
Axenfeld Rieger Syndrome
Posterior Embryotoxin (displaced SL anteriorly), 15% of normal pts
Axenfeld Anomaly – PE + glaucoma
Rieger Anomaly – Axenfeld + iris stroma issues + corectopia
Rieger Syndrome – RA + Systemic issues
Plan: treat Glaucoma, CL if corectopia to dec photosensitivity. Follow up yearly or q6-12 months for glaucoma managment