EXE 408: FINAL EXAM
1/80
Earn XP
Description and Tags
fall 2025
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
206
the human adult skeleton has _____ bones
270
babies are usually born with around _____ bones that fuse together as they grow
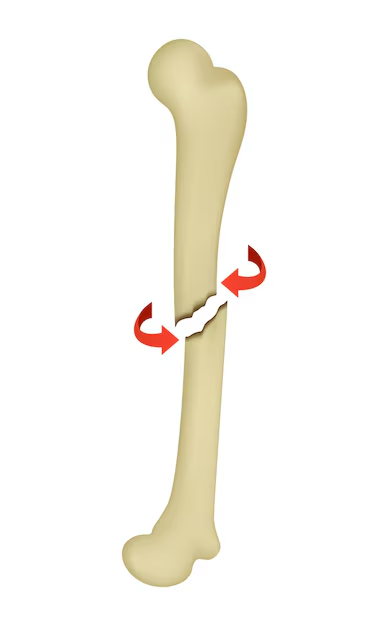
axial skeleton
skull, thoracic cage, vertebral column/spine
appendicular skeleton
upper and lower extremities, including shoulder and pelvis
clavicle
1 and 3
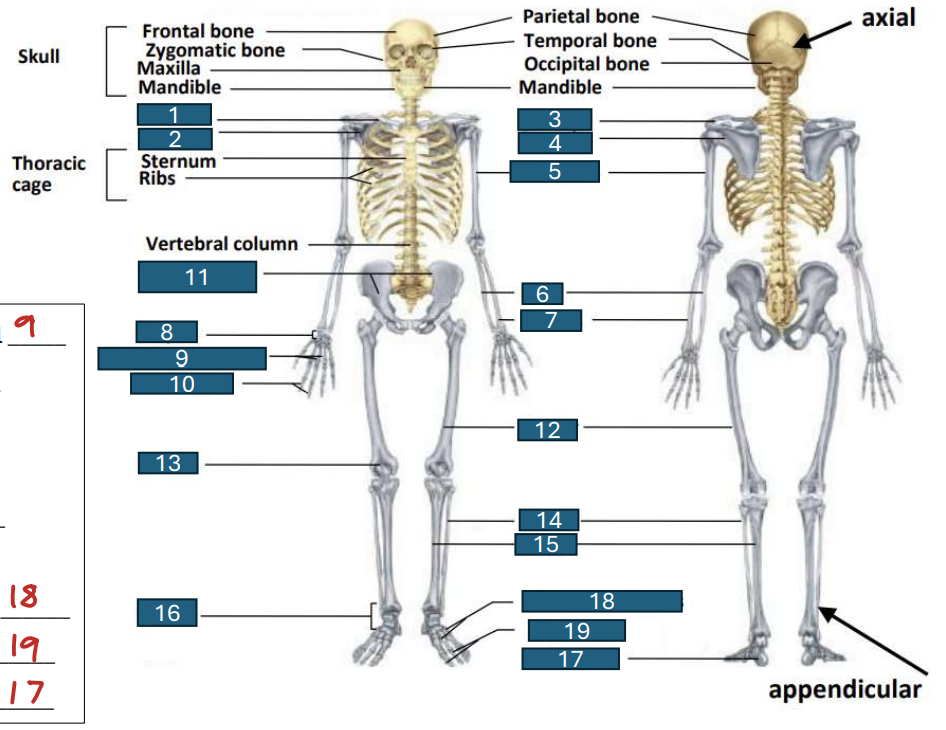
scapula
2 and 4
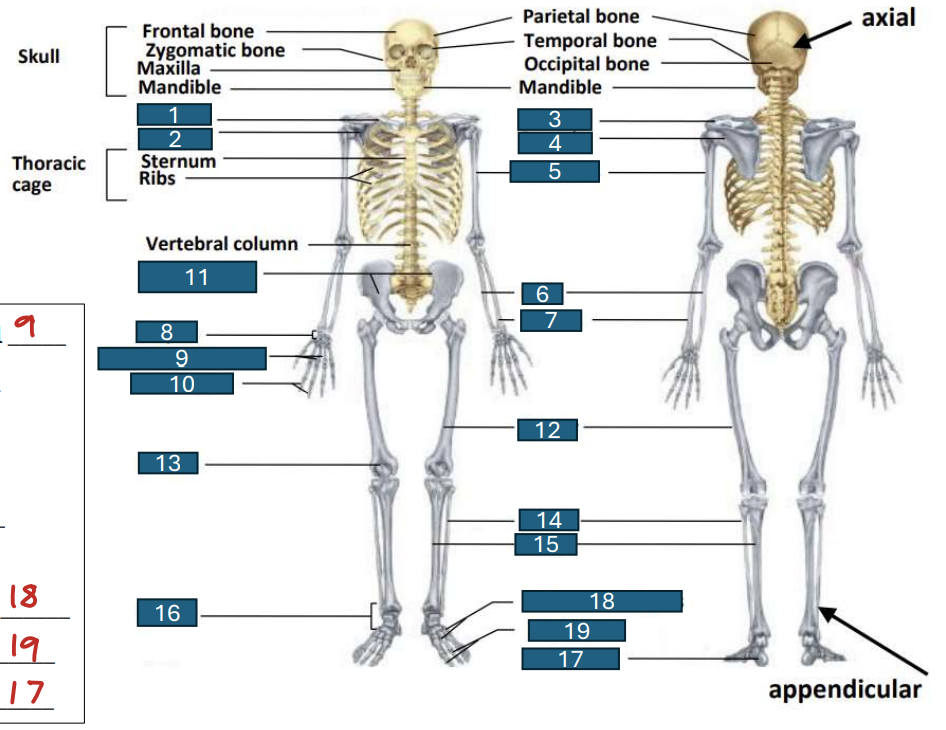
humerus
5
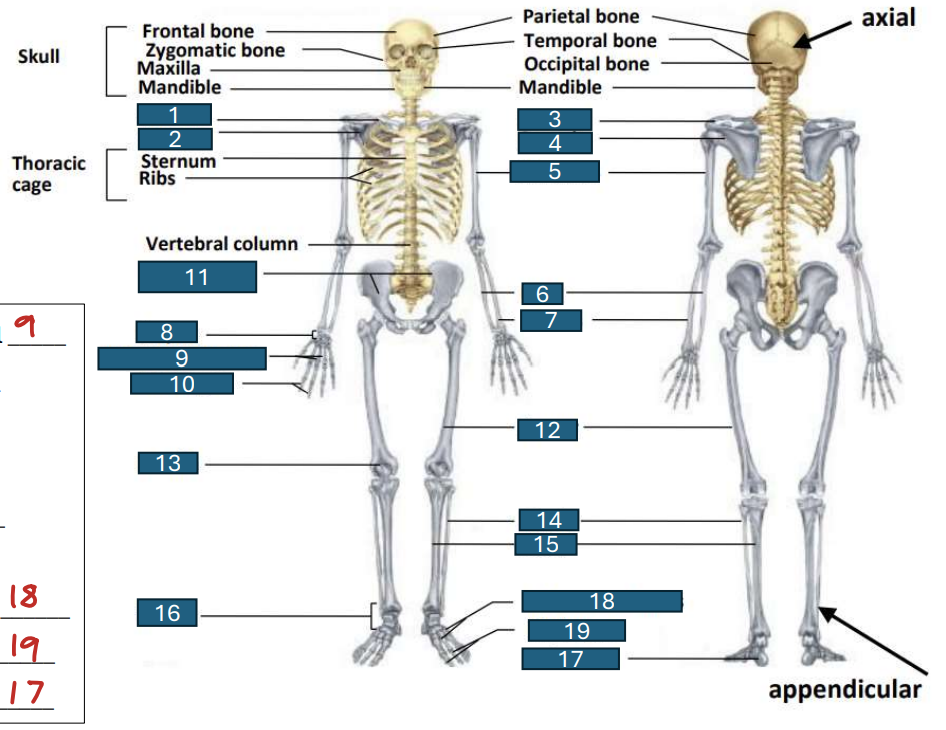
ulna
6
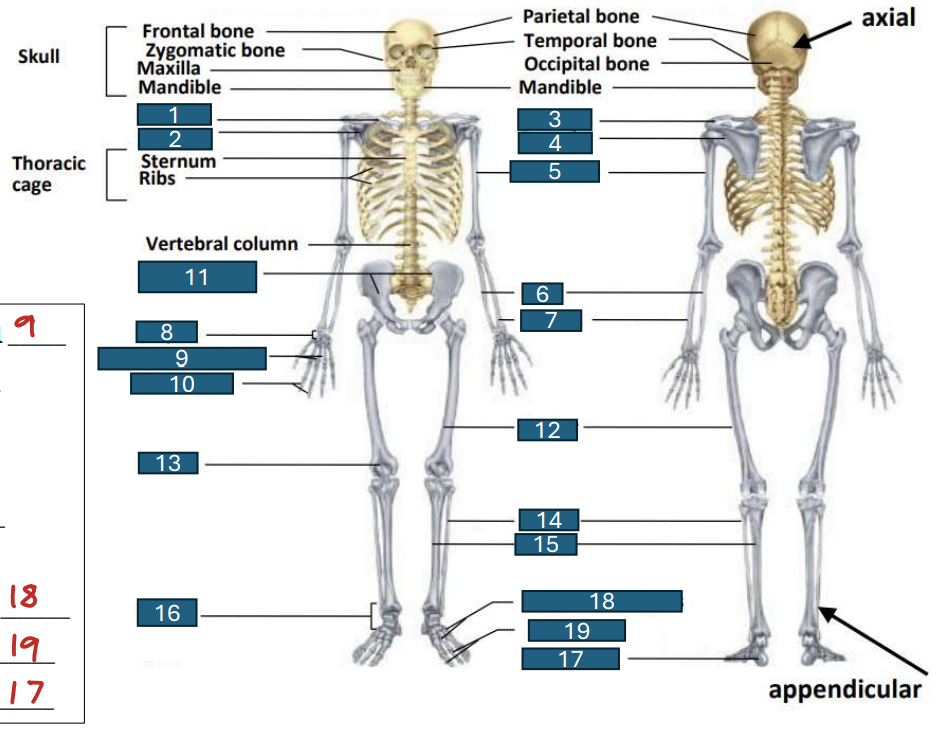
radius
7
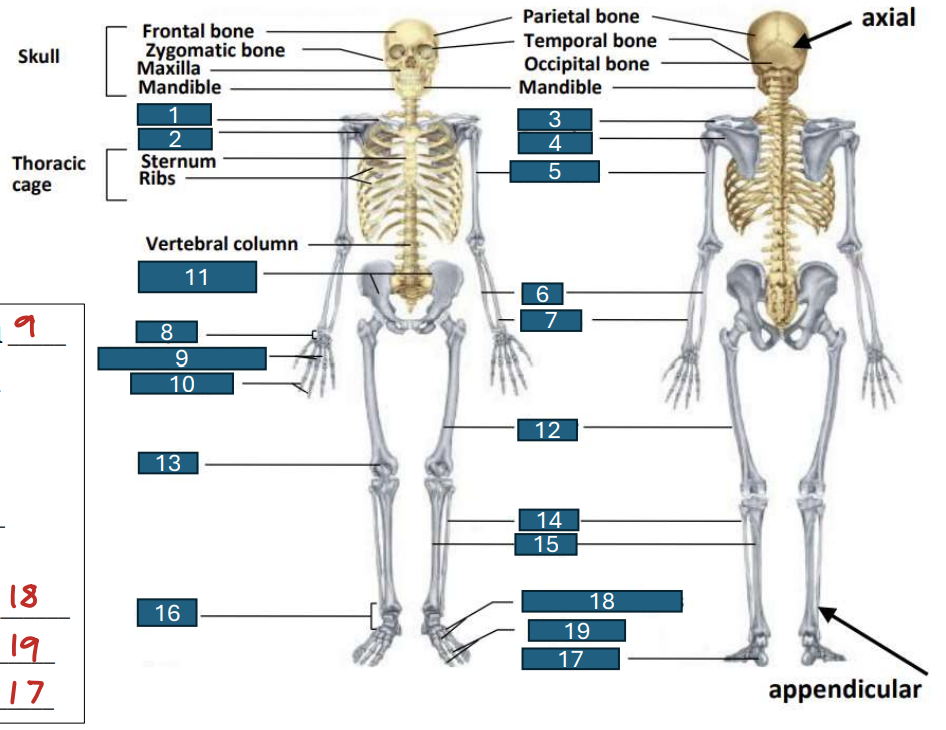
carpus
8
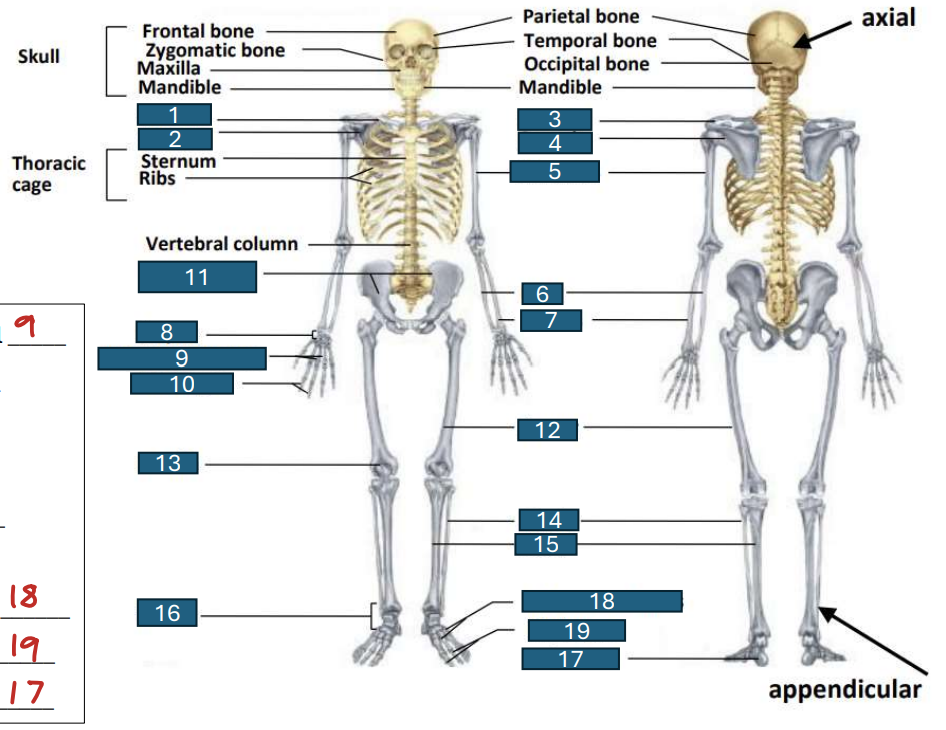
metacarpals
9
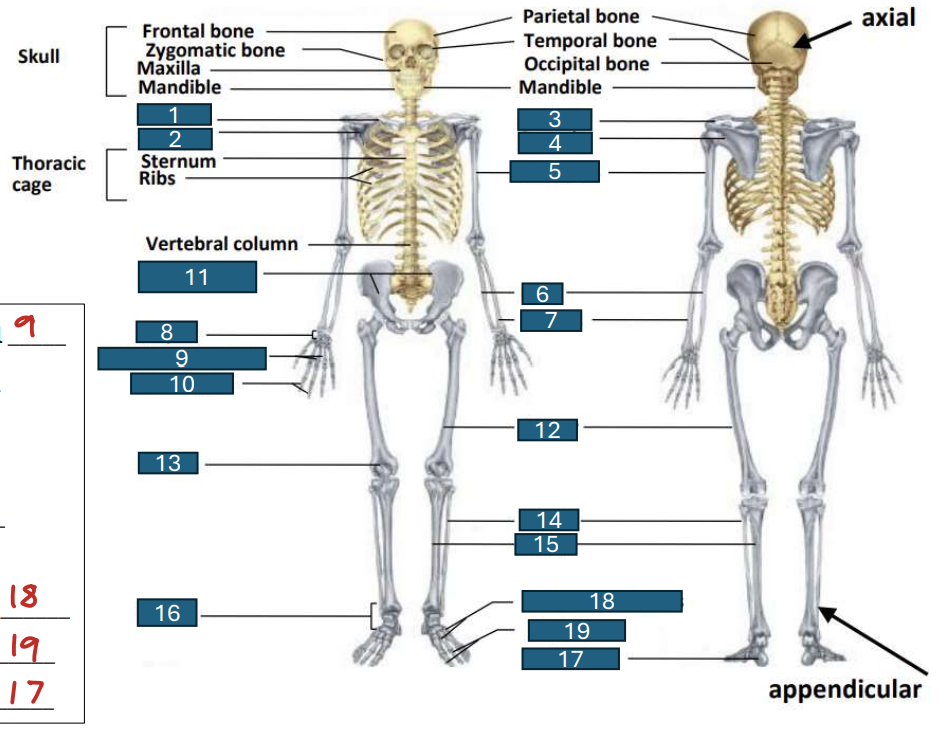
phalanges
10
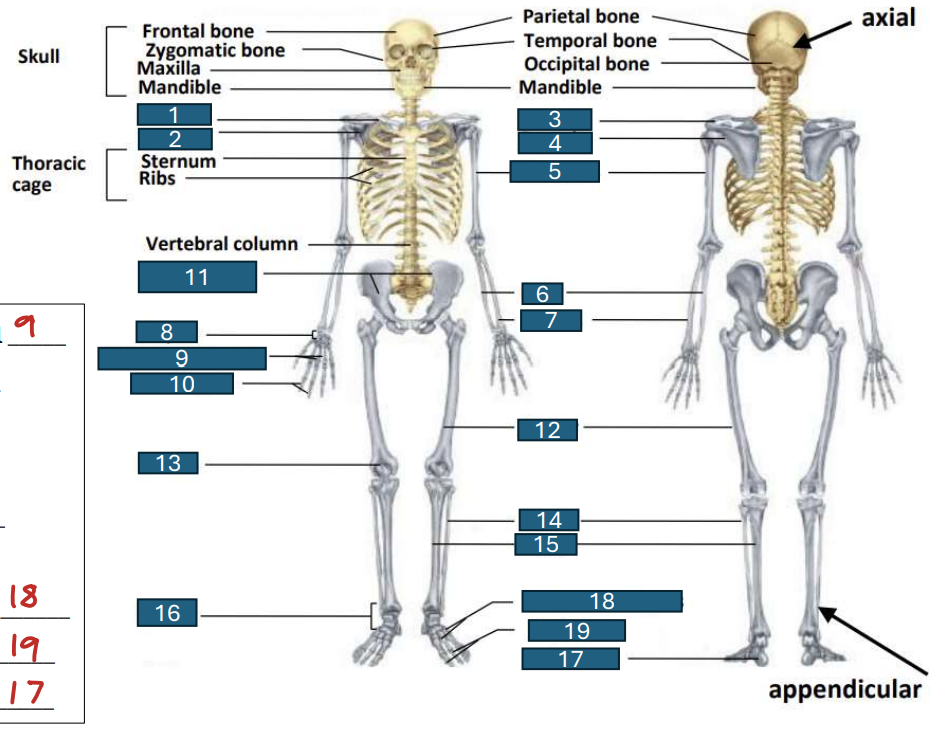
pelvic girdle
11
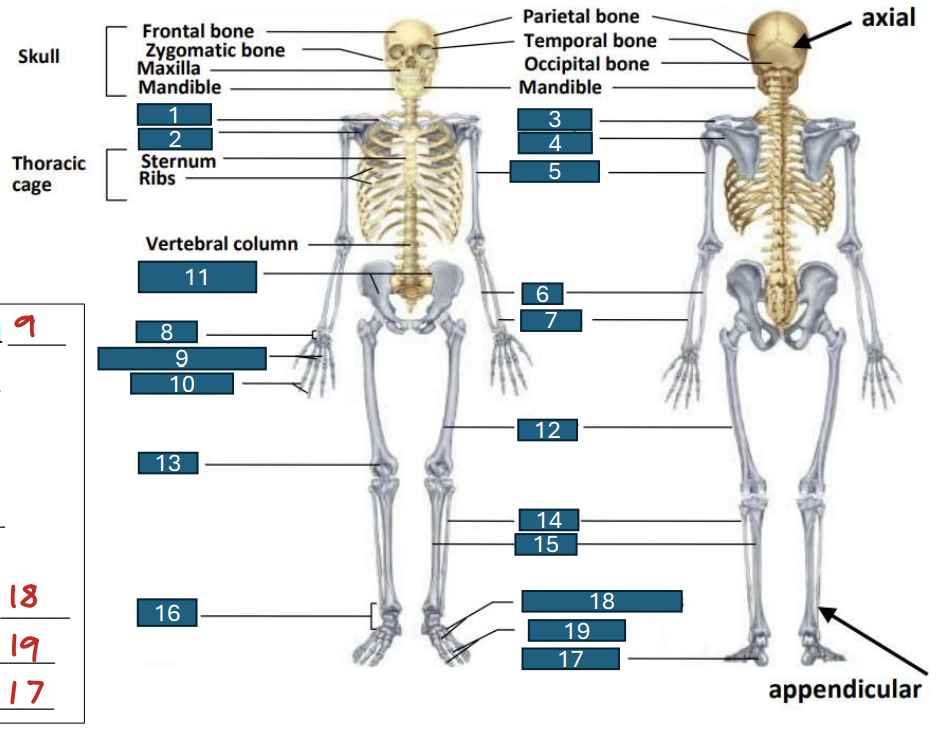
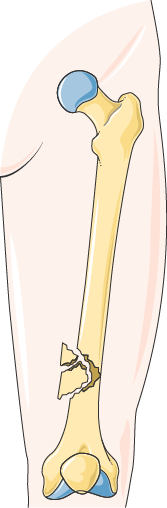
femur
12
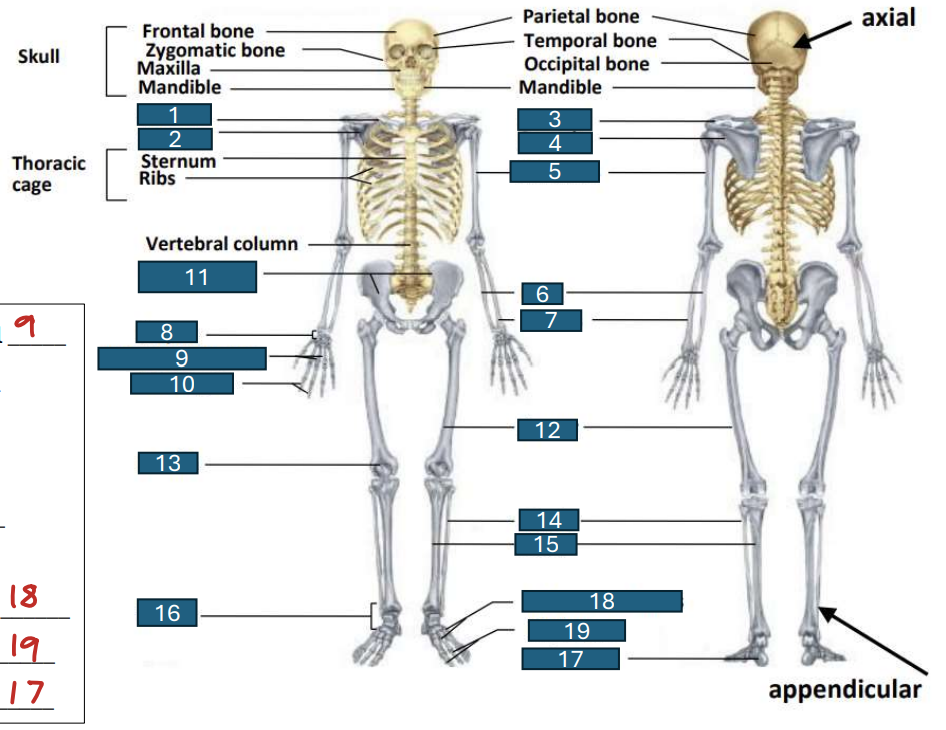
patella
13
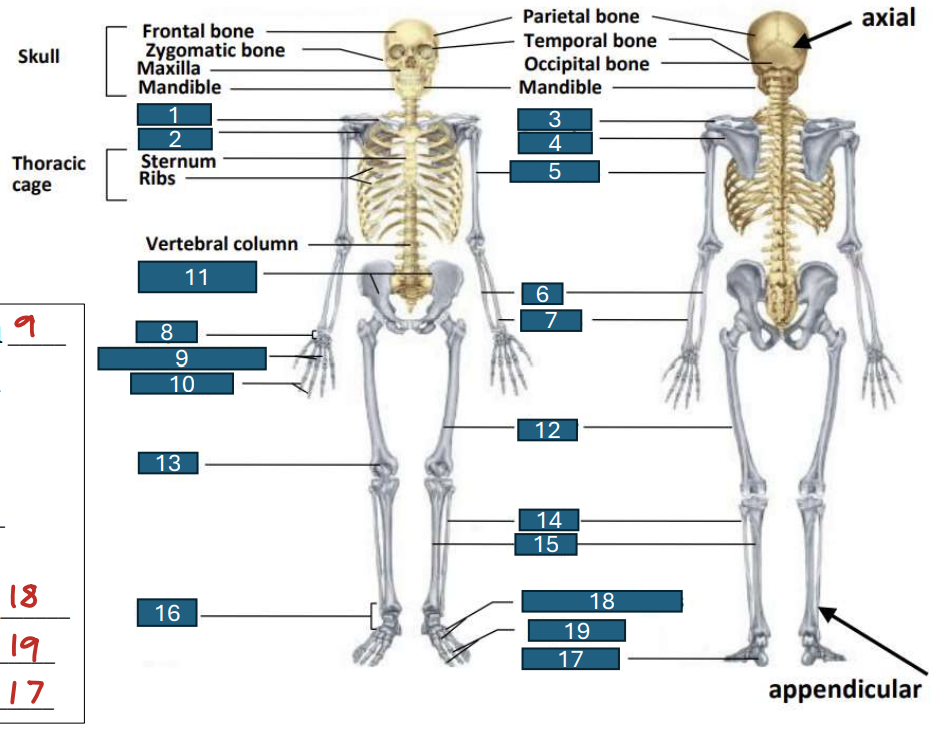
fibula
14
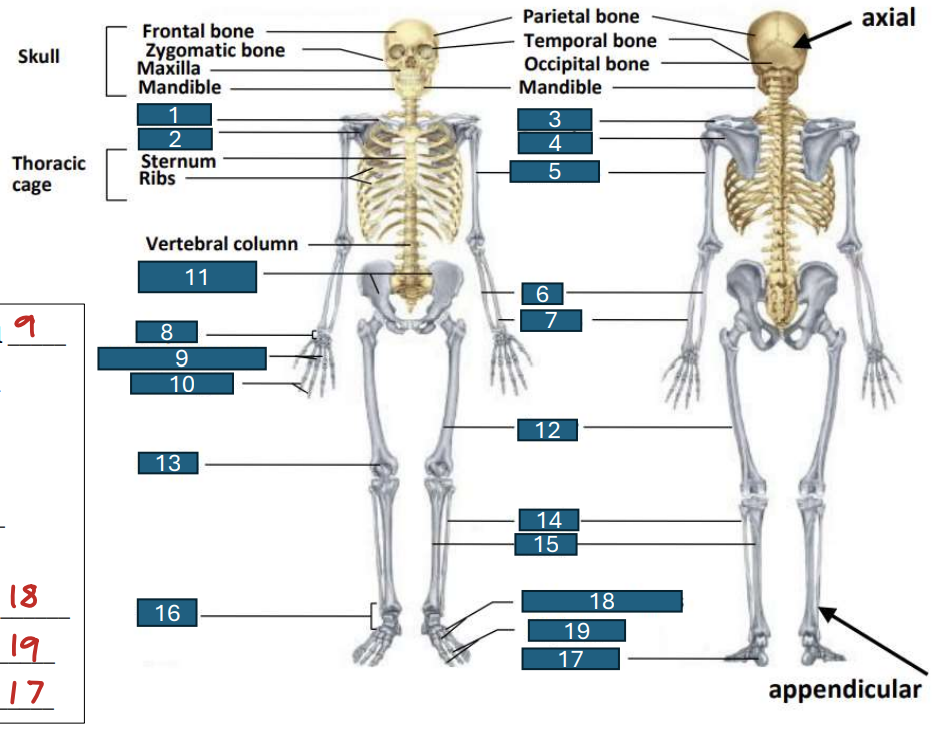
tibia
15
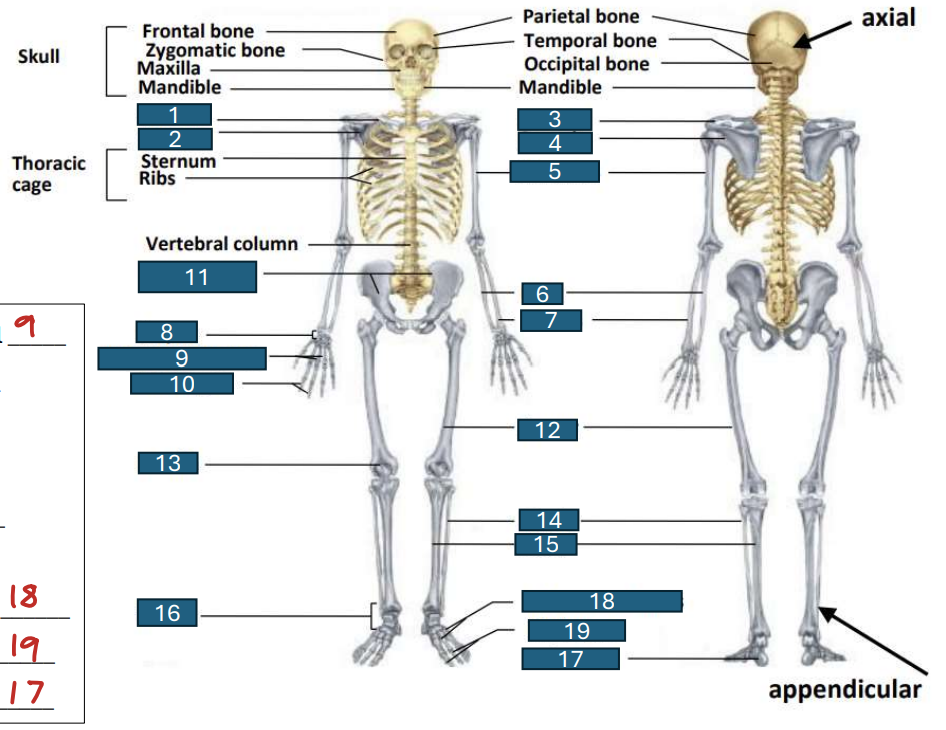
tarsus
16
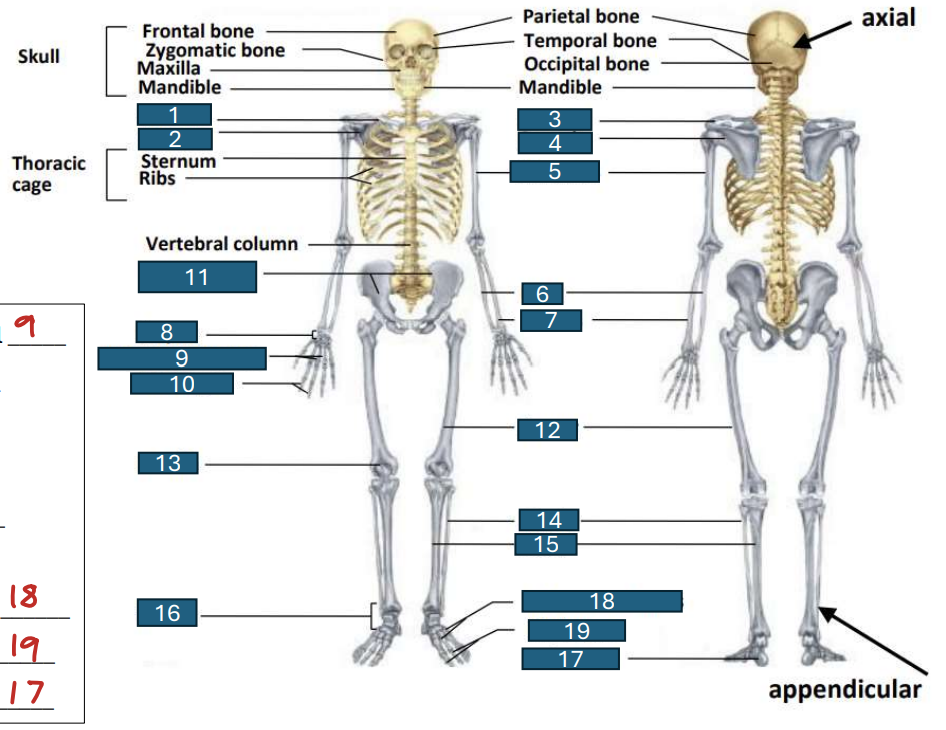
calcaneus
17
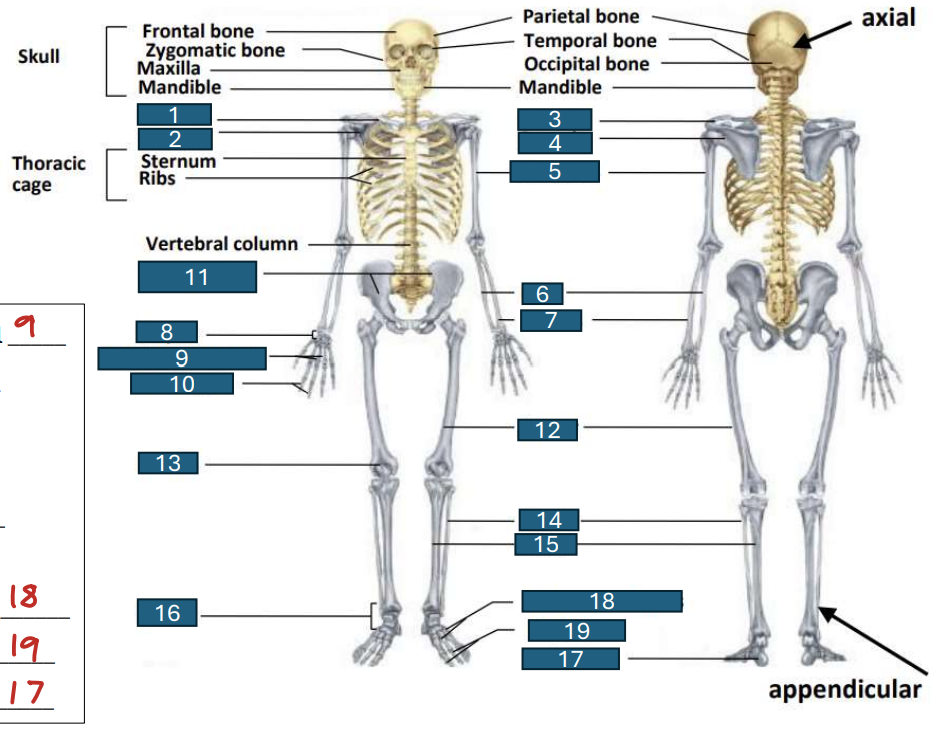
metatarsal
18
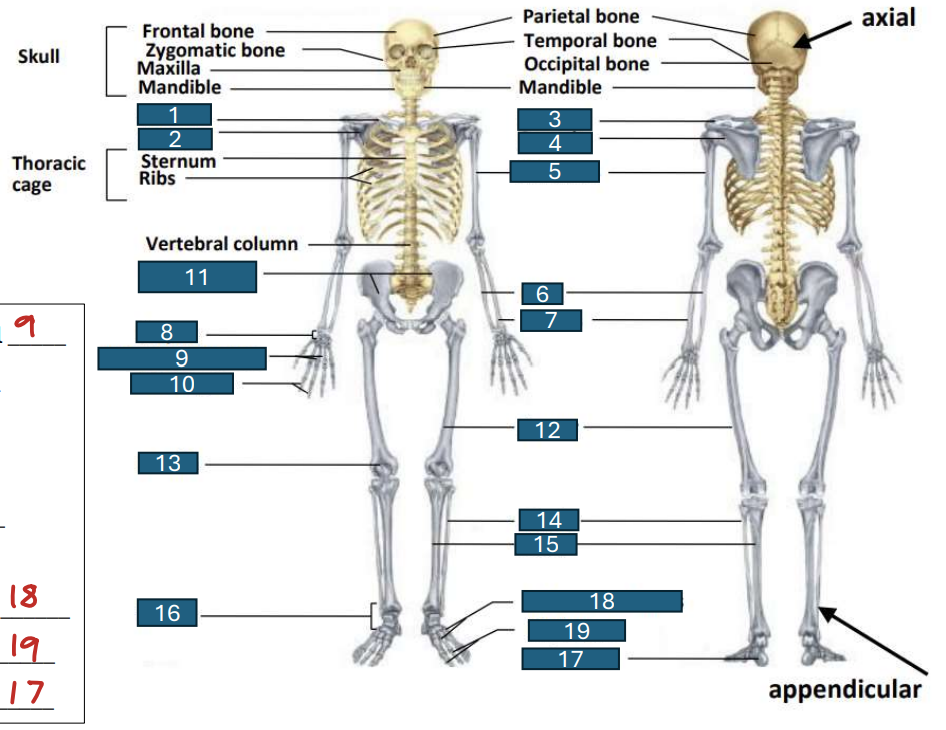
phalanges
19
long bone
examples: femur, tibia, radius
function: levers to transmit longitudinal force
short bone
examples: carpal, tarsal
function: levers to transmit longitudinal force
flat bone
examples: sternum, ribs, skull, iliac crest
function: protection, points of attachment for ligaments
irregular bones
examples: vertebrae
function: providing protection, support, attachment points for muscles, and contributing to blood cell production and mineral storage
sesamoid bones
examples: patella
function: improved lever
osteoblast
form new bones
osteoclast
resorb old bone
ruffled border allows osteoclast to secrete calcium as consequence of killing of bones
osteocyte
mature bone cell
support, protection, system levers to allow motion
3 important mechanical functions of bones
mineral component (calcium carbonate, calcium phosphate)
60-70% of weight of bone
water
25-30% of weight of bone
mineral component
what contributes to stiffness and compressive strength in bone?
collagen
what contributes to flexibility and tensile strength (ability to resist tension) in bone?
cortical bone
compact mineralized bone with low porosity; found in the shafts of long bones
trabecular (cancellous) bone
less compact bone with high porosity; found in the ends of long bones and the vertebrae
epiphyseal plates/epiphyses
growth centers where new bone cells are produced until the epiphysis closes during late adolescence or early adulthood
Epiphysis
develop from secondary ossification centers
found at the ends of long bones
protected by layer of articular cartilage
Metaphysis
meta: after
wide portions of long bones
Diaphysis
between (dia) two epiphyses
develop from primary ossification centers
hollow structure surrounding the medullary cavity
Medullar cavity
used for fat storage site
not in flat bone
periosteum
outer layer of the bone
periosteum is well supplied with blood vessels and nerves
hypertrophy
just like muscle, bones respond to certain kinds of training
Wolff’s law
the densities, and to a lesser extent, the sizes and shapes of bones are determined by the magnitude and direction of the acting forces
what diminishes bone density?
lack of weight bearing exercise
spending time in water
bed rest
traveling in space outside of the earth’s gravitational field
osteopenia
pre-stage to osteoporosis
osteoporosis
disorder involving decreased bone mass and strength with pain and one or more fractures resulting from daily activity
osteoporosis
collapse in a wedge shape
cannot straighten up
often associated with aging, especially women
osteoblast < osteoclast
cortical bone: thinner, less dense
trabecular bone: less trabeculae, thinner, most vulnerable
true
dynamic loading during exercise has been shown to affect bone size and strength more than muscle mass
weight bearing exercise
since the larger the forces the skeletal system sustains, the greater the osteoblast response
type 1: postmenopausal
osteoporosis affects about 40% of women after age 50
type 2: age-associated
osteoporosis affects most women and men after age 70
female athlete triad
osteoporosis, disordered eating, amenorrhea (loss of menstrual cycle)
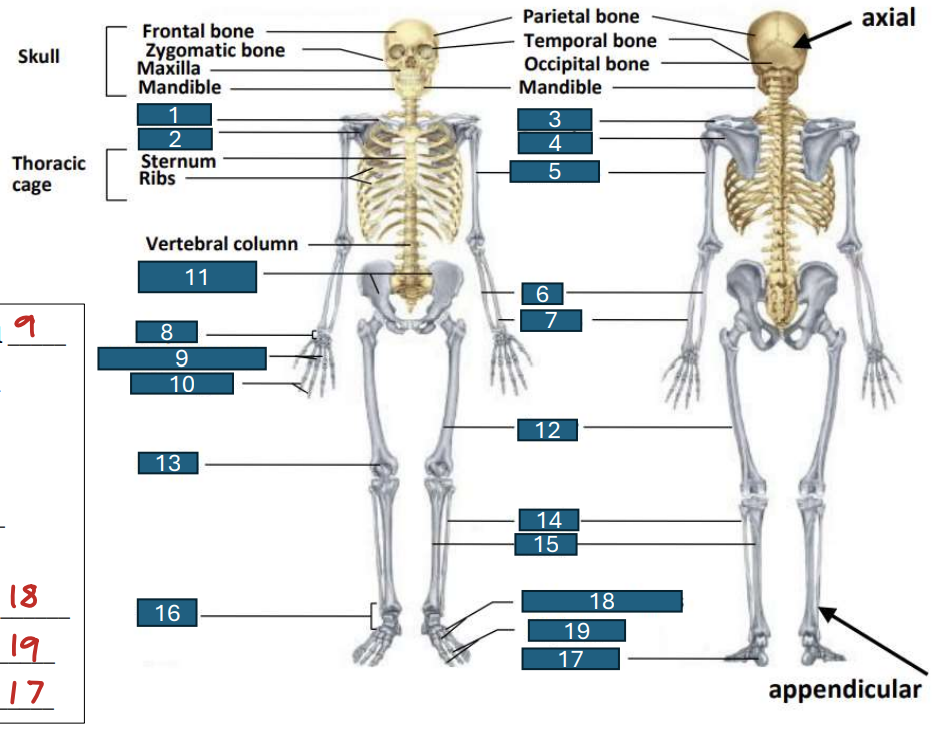
transverse bone fracture

linear bone fracture

oblique, nondisplaced bone fracture

oblique, displaced bone fracture
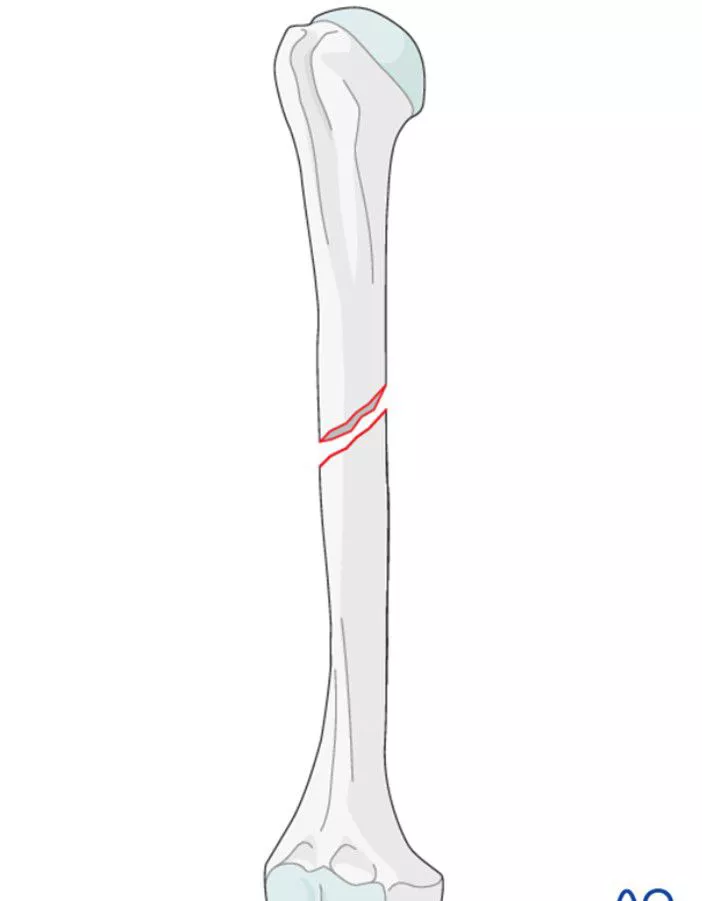
spiral bone fracture
greenstick bone fracture
comminuted bone fracture
stress fracture
relatively low load but repeated load
increase training duration or intensity
no time for bone remodeling
abrupt change in running surface
synarthroses
immovable
sutures
dense fibrous tissue binds the bones together
amphiarthroses
slightly movable
symphyses: a place where two bones are closely joined
hyaline cartilage disc separating the bones of the pubic symphysis
diarthroses or synovial
freely movable
articular (hyaline) cartilage
a protective layer of dense white connective tissue covering the articulating bone surfaces
articular (joint) capsule
a double-layered membrane that surrounds the joint
synovial fluid
clear, slightly yellow liquid that provides lubrication inside the articular capsule
bursae
small capsules filled with synovial fluid that cushion the structures they separate
Collateral ligaments
a
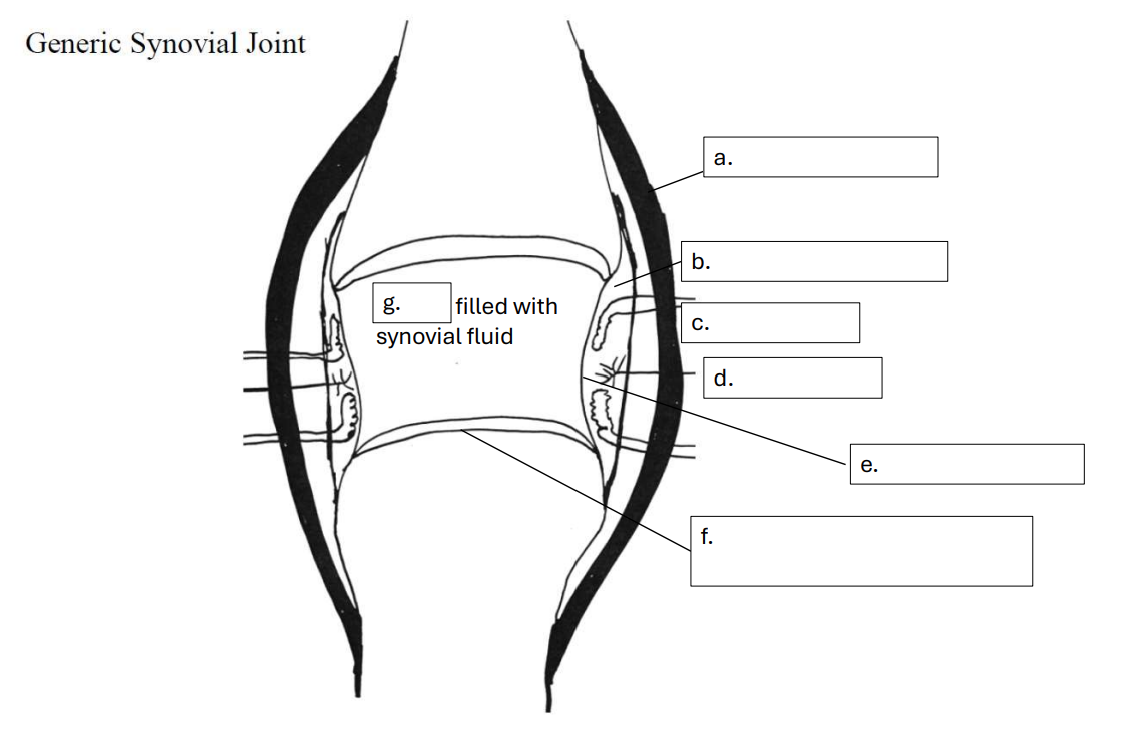
articular (joint) capsule
b
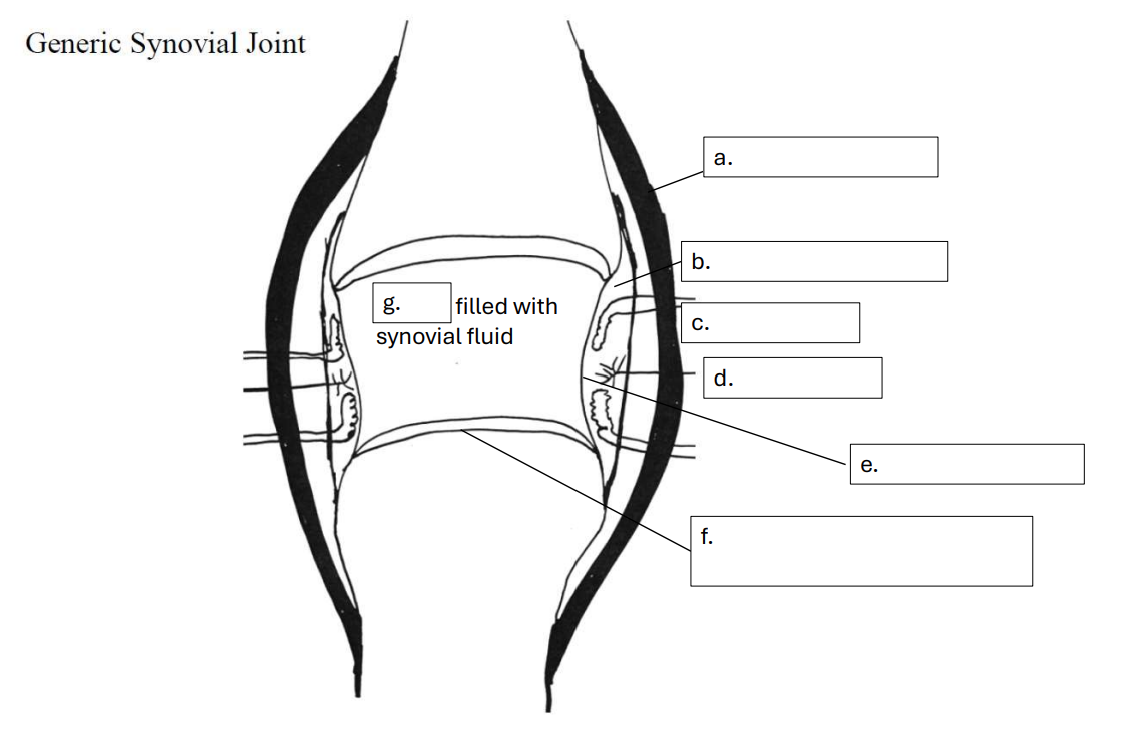
blood vessels
c
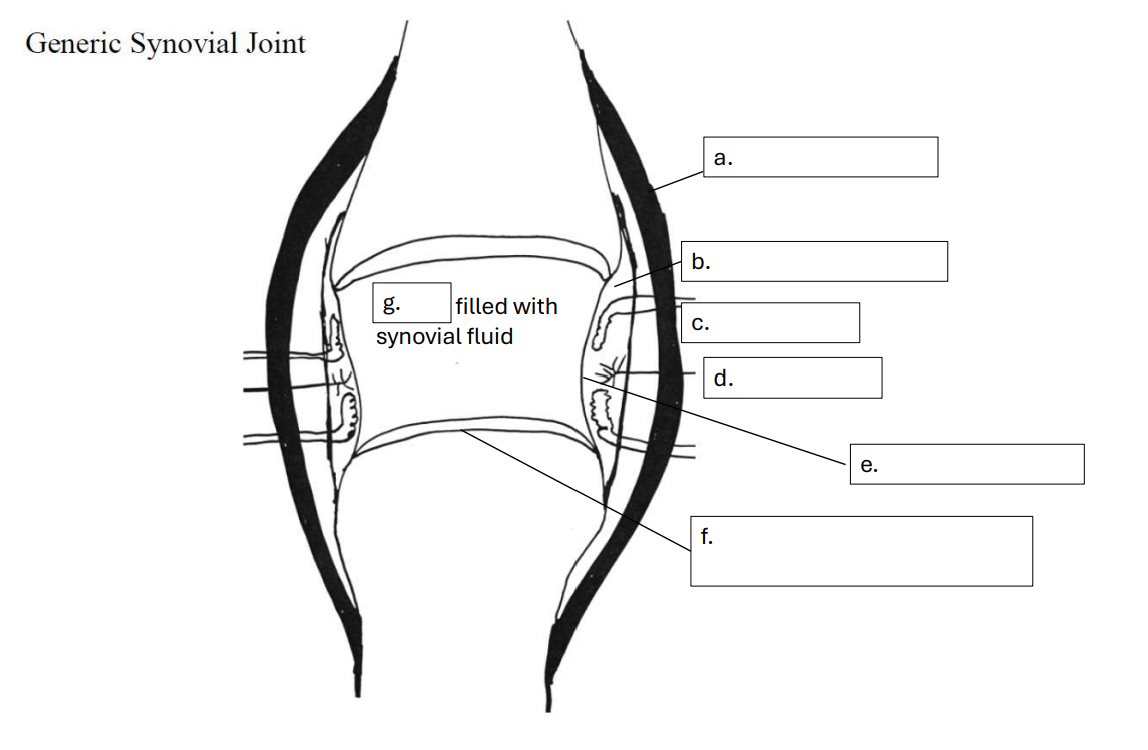
nerves
d
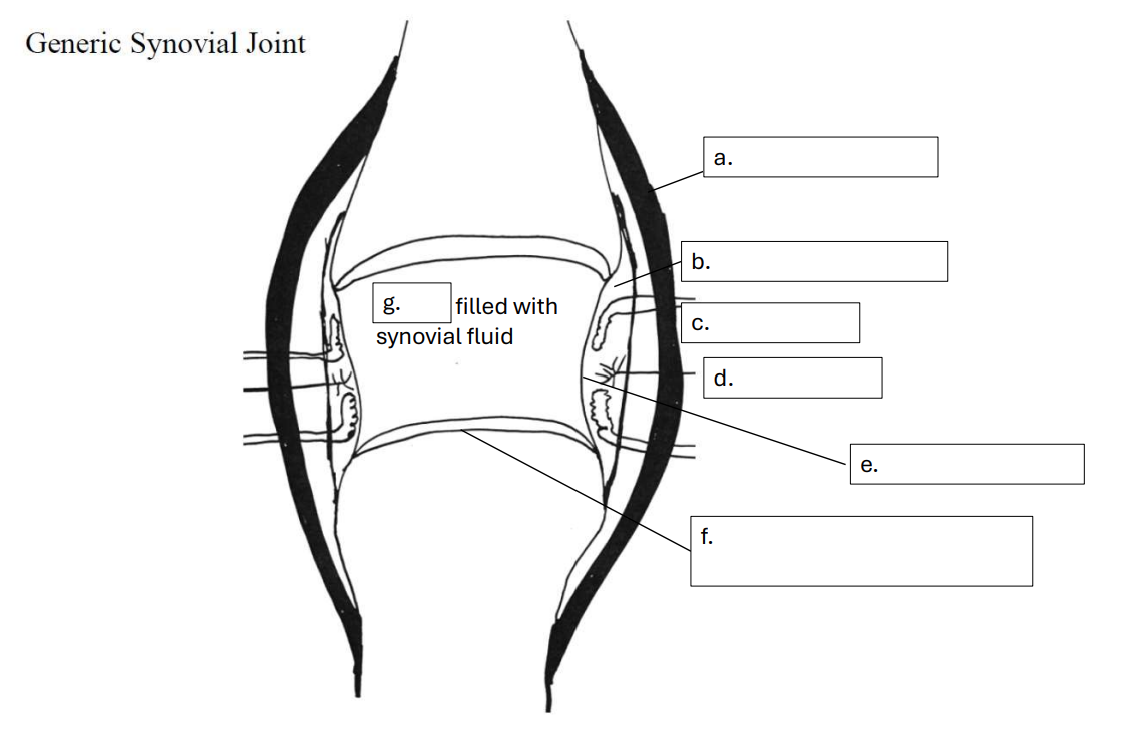
synovial membrane
e
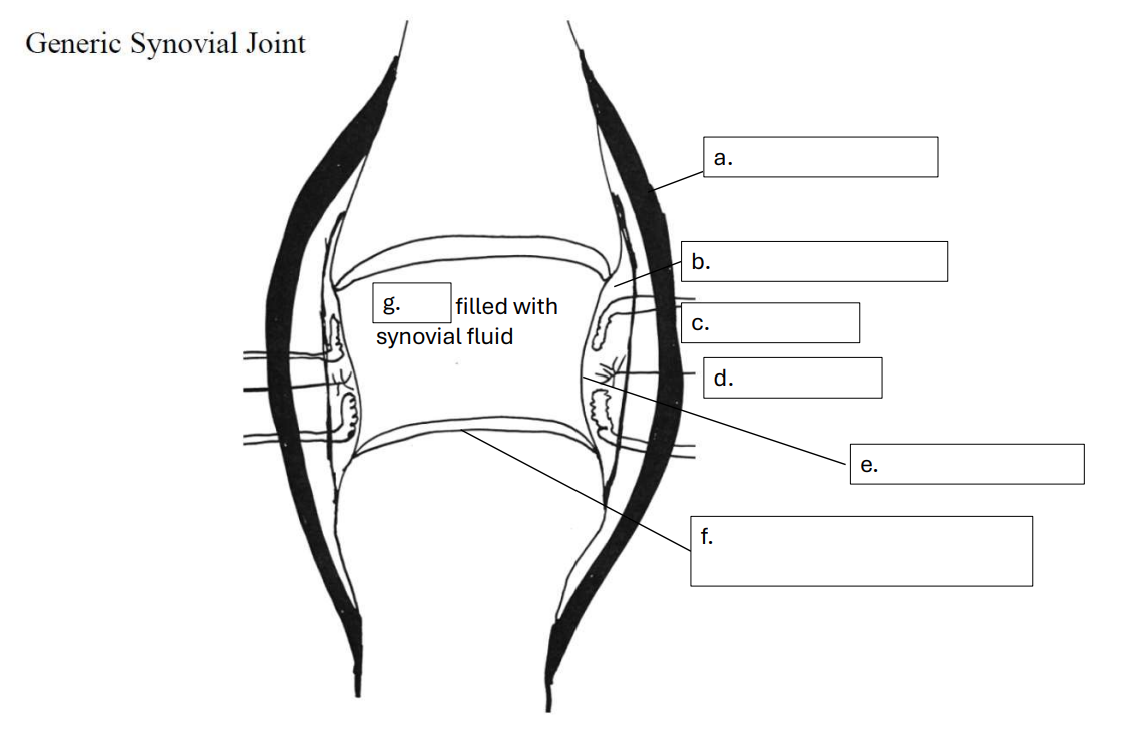
articular (hyaline) cartilage - no blood vessels or nerves
f
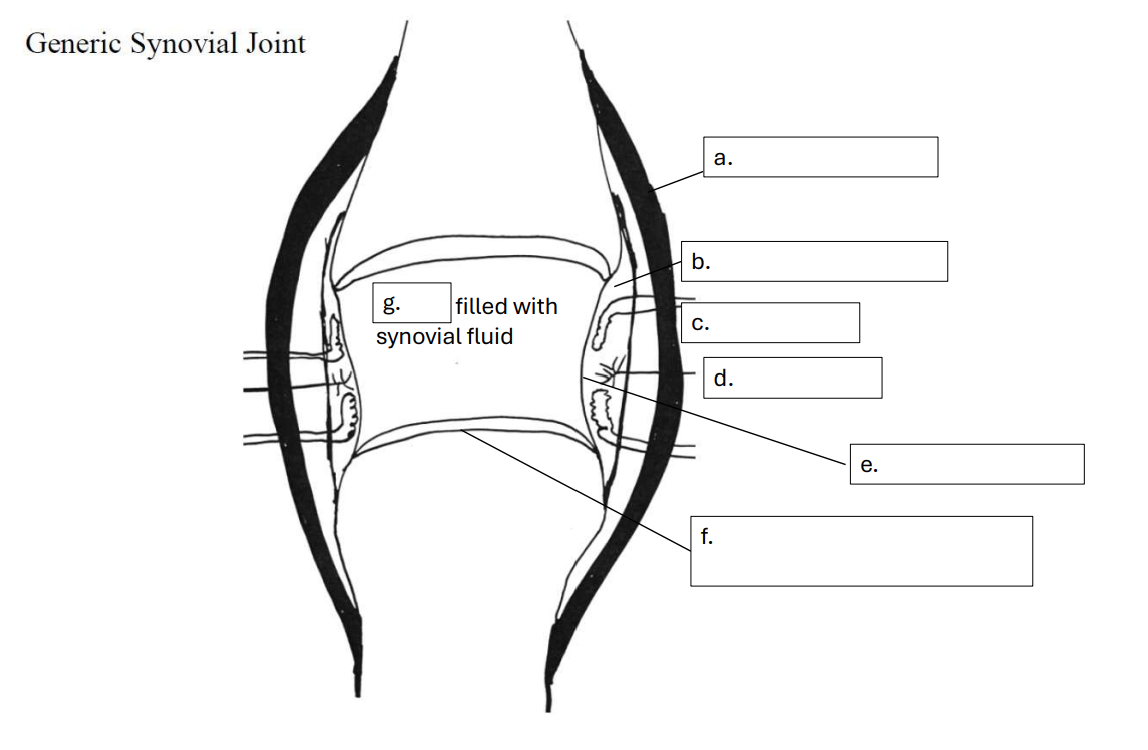
bursae
g
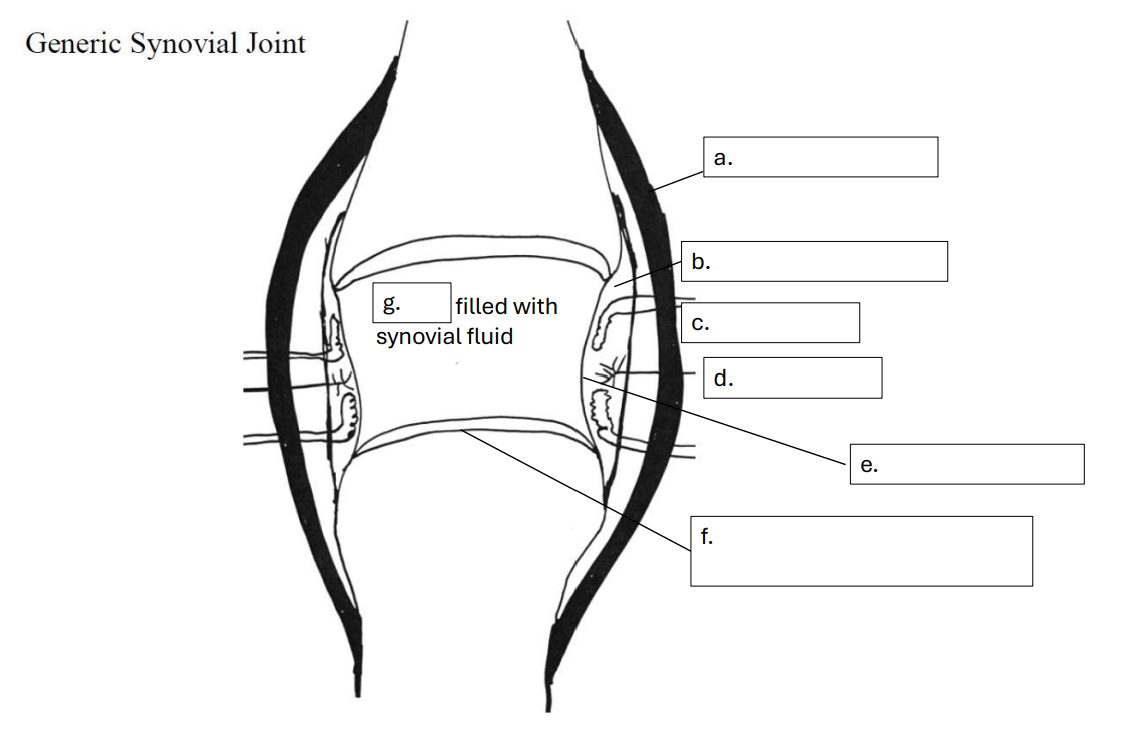
problems of not having blood vessels in articular cartilage
• Articular cartilage is squish material
• Compressed: water flows out
• Unloaded: absorb the water again.
• Through loading and unloading - the water that once flows out brings nutrition and oxygens and be absorbed to the cartilage.
Main Structure of Articular Cartilage
1. Cells – Chondrocytes (<10% volume)
2. Fibers – Collagen (10-30% of weight, % increase with age)
3. Proteoglycan (3-10%)
4. Water (60-90%)
Diarthroses/Synovial
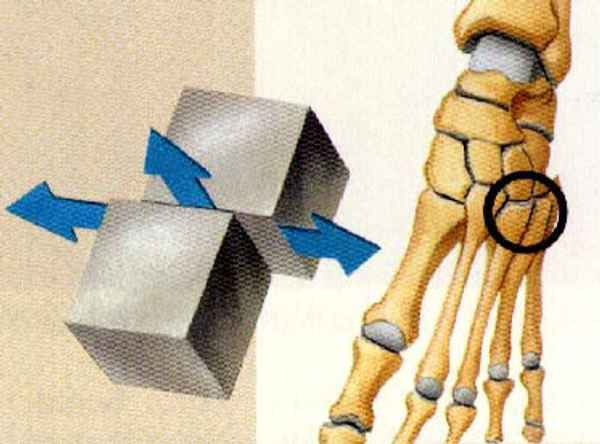
gliding
hinge
pivot
condyloid
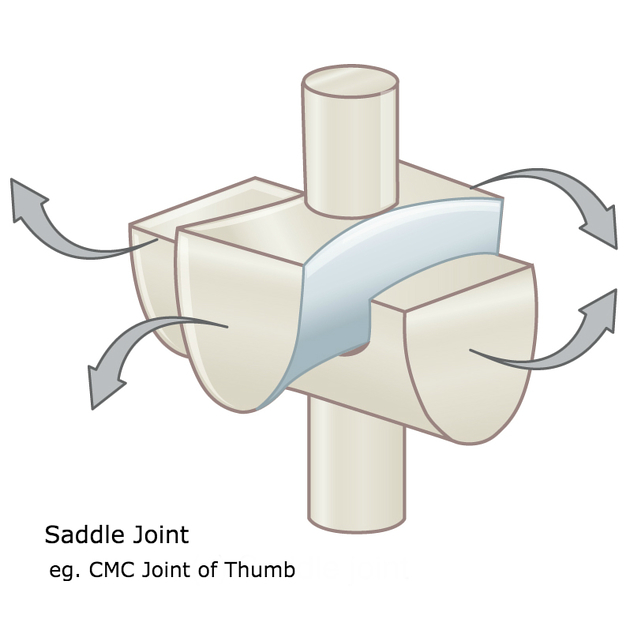
saddle
ball and socket
translations and rotations possible of synovial joint
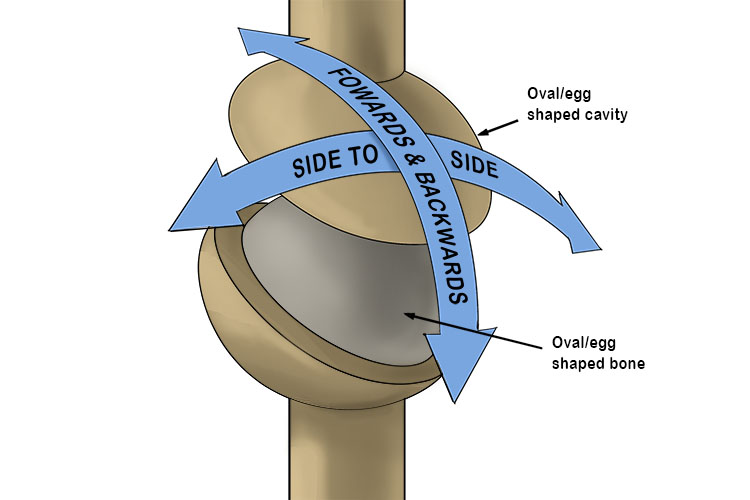
saddle joint
gliding joint
condyloid joint