Ch. 17: Physiology of the Kidneys
5.0(1)
Card Sorting
1/82
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
1
New cards
What does renal mean?
Pertaining to the kidneys
2
New cards
What is the main function of the renal system?
Regulation of extracellular fluid environment in the human body through urine formation
3
New cards
Name four other functions the renal system has:
1. Regulates blood volume
2. Eliminates organic waste products of metabolism
3. Regulates balance of electrolytes
4. With the respiratory system, maintains acid-base balance/pH of plasma
2. Eliminates organic waste products of metabolism
3. Regulates balance of electrolytes
4. With the respiratory system, maintains acid-base balance/pH of plasma
4
New cards
Name the structures within the renal system:
- Kidneys (2)
- Ureters (2)
- Urinary Bladder
- Urethra
- Ureters (2)
- Urinary Bladder
- Urethra
5
New cards
Kidney functions
- formation of urine
- water and electrolyte balance
- secretion of toxins and drugs into urine
- gluconeogenesis
- water and electrolyte balance
- secretion of toxins and drugs into urine
- gluconeogenesis
6
New cards
What is gluconeogensis?
Synthesis of glucose from AAs during prolonged fasting (also occurs in liver)
7
New cards
Ureters function
transfer of urine to bladder
8
New cards
Urinary Bladder function
storage and micturition
9
New cards
Urethra function
micturition
10
New cards
In the Female Renal System, what do the kidneys do?
Form a filtrate of the blood that's modified by reabsorption and secretion
11
New cards
Urine destined for ________ moves from the kidneys along the ______ to the _______.
excretion; ureters; bladder
*remember KIDNEYS -----> URETERS -----> BLADDER
*remember KIDNEYS -----> URETERS -----> BLADDER
12
New cards
Where is the urine excreted?
Through the urethra
13
New cards
What is the outer layer of the kidney called?
Renal Cortex
14
New cards
What is the renal cortex the site of?
Glomerular filtration and convoluted tubules
15
New cards
What is the inner layer of the kidney called?
Renal Medulla
16
New cards
What is the renal medulla the site of?
- Loops of Henle
- Drainage of collecting ducts into the renal pelvis and ureter
- Drainage of collecting ducts into the renal pelvis and ureter
17
New cards
What is Micturition?
Contractions of smooth muscle in ureter wall (another word for urination)
18
New cards
What does micturition cause?
Urine to move from ureter to bladder
19
New cards
Bladder walls are made up of what type of muscle?
Smooth muscle (detrusor muscle)
20
New cards
Contraction of detrusor muscles produces what?
Micturition
21
New cards
At the base of the bladder is the:
Internal urethral sphincter
22
New cards
Below the internal urethral sphincter is the:
external urethral sphincter
23
New cards
What does the external urethral sphincter do?
- Surrounds the urethra
- Contractions can prevent urination
- Contractions can prevent urination
24
New cards
What two things determine the contraction/relaxation of these muscles?
1. Neuronal input due to stretching of the bladder when it fills
2. Voluntary decision making
2. Voluntary decision making
25
New cards
How does blood enter and exit the the kidney?
- Enters through the renal artery
- Exits through the renal vein
- Exits through the renal vein
26
New cards
What is the Nephron?
The functional unit of the kidneys, consists of a renal corpuscle and tubule
27
New cards
What two things make up the renal corpuscle?
Glomerular capsule + Glomerulus
28
New cards
About how many nephrons are there in a kidney?
> 1,000,000
29
New cards
What does the branching of the renal artery lead to?
Afferent Arterioles
30
New cards
What do the afferent arterioles do?
Bring blood to the glomeruli
*Blood from renal artery ----> afferent arterioles ----> glomeruli*
*Blood from renal artery ----> afferent arterioles ----> glomeruli*
31
New cards
How much percent of plasma filters out of the glomerulus? And where does it filter out to?
20%; and into surrounding glomerular capsule & then into a tubule
32
New cards
Name the order of what occurs after the filtration of plasma
Plasma filtrates from glomerulus ----> glomerular capsule ----> tubule -----> collecting duct -----> renal pelvis -----> ureters
33
New cards
What does the remaining 80% blood do?
- Exits renal corpuscle through efferent arteriole to the peritubular capillaries
-The blood then drains into veins that exit kidney as the renal vein
-The blood then drains into veins that exit kidney as the renal vein
34
New cards
Name the order of what occurs to the 80% of blood
80% of blood in glomerulus -----> efferent arteriole ----> peritubular capillaries ----> renal veins
35
New cards
What does the glomerular/bowman's capsule do?
- surrounds glomerulus
36
New cards
In the nephron, fluid filters from the ______ into the _____.
glomerulus; glomerular capsule
37
New cards
What does the proximal convoluted tubule do?
- Filtrates from glomerulus, enters its lumen
- Reabsorption of salt, water into peritubular capillaries that surround tubule
- Secretion of substances into filtrate
- Reabsorption of salt, water into peritubular capillaries that surround tubule
- Secretion of substances into filtrate
38
New cards
What does the collecting duct do?
- Distal convoluted tubule empties into it
- Duct drains into renal pelvis and then ureters
- Duct drains into renal pelvis and then ureters
39
New cards
Glomerula Filtration:
Appx 20% of plasma filters out of glomerulus (capillaries) into the glomerular capsule
40
New cards
How is the plasma filtered?
Filters through large pores in glomerular capillaries called fenestrae
41
New cards
Around _____ L of glomerular filtrate is produced each day, but urine ______ is only around _____ L per day.
180; excretion; 1-2
42
New cards
How much percent of the filtrate is excreted as urine?
1%
43
New cards
How much percent of the filtrate is reabsorbed to the vascular system? And why?
99%; to maintain blood volume and pressure
44
New cards
What is reabsorption?
Return of filtrate from tubules to peritubular capillaries by osmosis
45
New cards
Urine volume varies on what?
On fluid needs of body, so volume of fluid that's reabsorbed also varies
46
New cards
Where is salt and water in filtrate reabsorbed?
Proximal tubule or descending limb of loop henle
47
New cards
What does filtration refer to?
Movement of fluid/solutes from the glomerulus into the capsule and then into the tubules
*Glomerulus ---> Capsule ----> Tubules
*Glomerulus ---> Capsule ----> Tubules
48
New cards
What does reabsorption refer to?
Movement of materials from the tubules into peritubular capillaries
49
New cards
Which electrolyte is actively transported out of filtrate, and which one follows?
Na+ and Cl- follows passively by electrical attention
50
New cards
Due to _______, _______ follows salt into the peritubular capillaries
osmosis; water
51
New cards
If water wants to be reabsorbed into the bloodstream by osmosis what needs to happen to the ISF?
The ISF that surrounds the tubule must be hypertonic
52
New cards
Why is the fluid hypertonic?
B/c of the Countercurrent Multiplier System
53
New cards
What allows limbs to interact to create high osmotic pressure in the ISF?
Countercurrent flow in ascending and descending limbs in nephrons and close proximity of limbs
54
New cards
What occurs in the ASCENDING limb of the loop of Henle?
- Na+ is actively PUMPED into ISF
- Cl- follows Na+ bc of electrical attraction
- Not permeable to water so fluid in ascending limb becomes diluted
- NaCl accumulates in the ISF here, which increases the osmolarity of ISF
- Cl- follows Na+ bc of electrical attraction
- Not permeable to water so fluid in ascending limb becomes diluted
- NaCl accumulates in the ISF here, which increases the osmolarity of ISF
55
New cards
The countercurrent multiplier system does which of the following?
A) pumps CI- out of the tubule
B) secretes NaCl into the urine
C) allows water to diffuse out of the ascending limb
D) pumps Na+ out of the tubule
E absorbs water into the tubule
A) pumps CI- out of the tubule
B) secretes NaCl into the urine
C) allows water to diffuse out of the ascending limb
D) pumps Na+ out of the tubule
E absorbs water into the tubule
D) pumps Na+ out of the tubule
56
New cards
What occurs in the DESCENDING limb of the loop of Henle?
- permeable to water but not salt
- ISF is hypertonic compared to filtrate here, so water leaves descending limb by osmosis ---> ISF ----> capillaries
- hypertonic fluid then enters the ascending limb, where Na+ is actively pumped out and Cl- follows, creating diluted tubular fluid and more concentrated ISF
- ISF is hypertonic compared to filtrate here, so water leaves descending limb by osmosis ---> ISF ----> capillaries
- hypertonic fluid then enters the ascending limb, where Na+ is actively pumped out and Cl- follows, creating diluted tubular fluid and more concentrated ISF
57
New cards
What is the 3 steps within the Countercurrent Multiplier System in Tubule?
1) Extrusion of NaCl from ascending limb makes ISF more concentrated. Na+ is pumped out, Cl- follows due to electrical attraction
2) In descending limb, water diffuses out by osmosis and enteres capillaries. This increases osmolarity of tubular fluid and decreases its volume as the fluid descends
3) Fluid at the bend of the loop has a high osmolarity, 1200 mOsm. The saltiness of the ISF is multiplied here b/c of the lack of permeability to water
2) In descending limb, water diffuses out by osmosis and enteres capillaries. This increases osmolarity of tubular fluid and decreases its volume as the fluid descends
3) Fluid at the bend of the loop has a high osmolarity, 1200 mOsm. The saltiness of the ISF is multiplied here b/c of the lack of permeability to water
58
New cards
Fluid that enters the collecting duct is _____. What does this conclude?
hypotonic; ISF surrounding collecting duct is hypertonic
59
New cards
What is the collecting duct permeable to and not permeable to? What does this cause water to do?
Permeable to water but not salt so water diffuses out of duct into hypertonic ISF by osmosis
60
New cards
What causes ADH secretion to increase?
Plasma osmolarity increasing
61
New cards
Why must both plasma osmolarity and ADH secretion increase?
To increase permeability of collecting duct to water
62
New cards
What is the action of osmoreceptors in ADH secretion?
Senses changes in water intake that alters plasma osmolarity
63
New cards
Release of _____ is altered to affect water _______ in the kidneys. What does this affect?
- ADH; Reabsorption
- It affects the volume of urine excretion to maintain blood volume
- It affects the volume of urine excretion to maintain blood volume
64
New cards
What is renal plasma clearance?
Volume of plasma that's "cleared" of a substance by kidneys per unit time
65
New cards
How are substances from the plasma removed?
By filtration from glomerulus, or secretion into filtrate
66
New cards
What is secretion?
Movement of substances from the peritubular capillaries into the tubular fluid for excretion in the urine
67
New cards
During Renal Plasma Clearance what occurs to the filtered glucose and AAs?
They're completely reabsorbed in the proximal tubule by active transport
68
New cards
What happens when the concentration of glucose exceeds the capacity of the transporters?
The excess glucose is exerted in the urine = glucosuria
69
New cards
When there is excess glucose in the urine, this is called glucosuria.
A)True
B) False
A)True
B) False
A)True
70
New cards
When is filtered Na+ and K+ reabsorbed?
In early part of nephron
71
New cards
What do the concentrations of Na+ and K+ in the urine excreted depend on?
Physiological needs/homeostasis and are adjusted late in the nephron
72
New cards
What do decrease plasma [Na+] activate?
Renin-angiotensin-aldoesterone system
73
New cards
Name some results in secretion of aldosterone (adrenal cortex)
- Stimulates Na+ reabsorption to increase plasma
- Causes passive reabsorption of Cl-
- Water follows by osmosis to increase blood volume
- Causes passive reabsorption of Cl-
- Water follows by osmosis to increase blood volume
74
New cards
What is the main function of ADH in regards to homeostasis of Plasma Na+
Regulates water reabsorption to regulate urine volume and blood volume
75
New cards
What does the Renin-angiotensin-aldoesterone system do?
Stimulates secretion of aldosterone when Na+ intake is low
76
New cards
What does aldosterone do?
Stimulates Na+ reabsorption in the cortical collecting ducts
77
New cards
How is Potassium filtered?
From the glomerulus, some is reabsorbed
78
New cards
What does aldosterone do when [K+] is high?
Stimulates potassium secretion
79
New cards
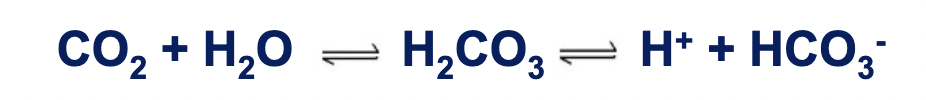
What's the equation for Renal Control of Acid/Base Balance?
CO2 + H20 -----> H2CO3 -------> H+ + HCO3-
80
New cards
How do kidneys regulate blood pH?
By excreting H+ in the urine and by reabsorbing bicarbonate
81
New cards
Why is urine slightly acidic?
Almost all of the filtered bicarbonate is reabsorbed in tubules and H+ is excreted
82
New cards
What occurs in acidosis?
- Increase plasma [H+] and more in filtrate
- Bicarbonate is synthesized in proximal tubule cells to compensate
- Bicarbonate enters blood
- Bicarbonate is synthesized in proximal tubule cells to compensate
- Bicarbonate enters blood
83
New cards
What occurs in alkalosis?
- Decreased plasma [H+] and less in filtrate
- Less bicarbonate is reabsorbed to compensate
- Less bicarbonate is reabsorbed to compensate