Block 3 Study Guide
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
101 Terms
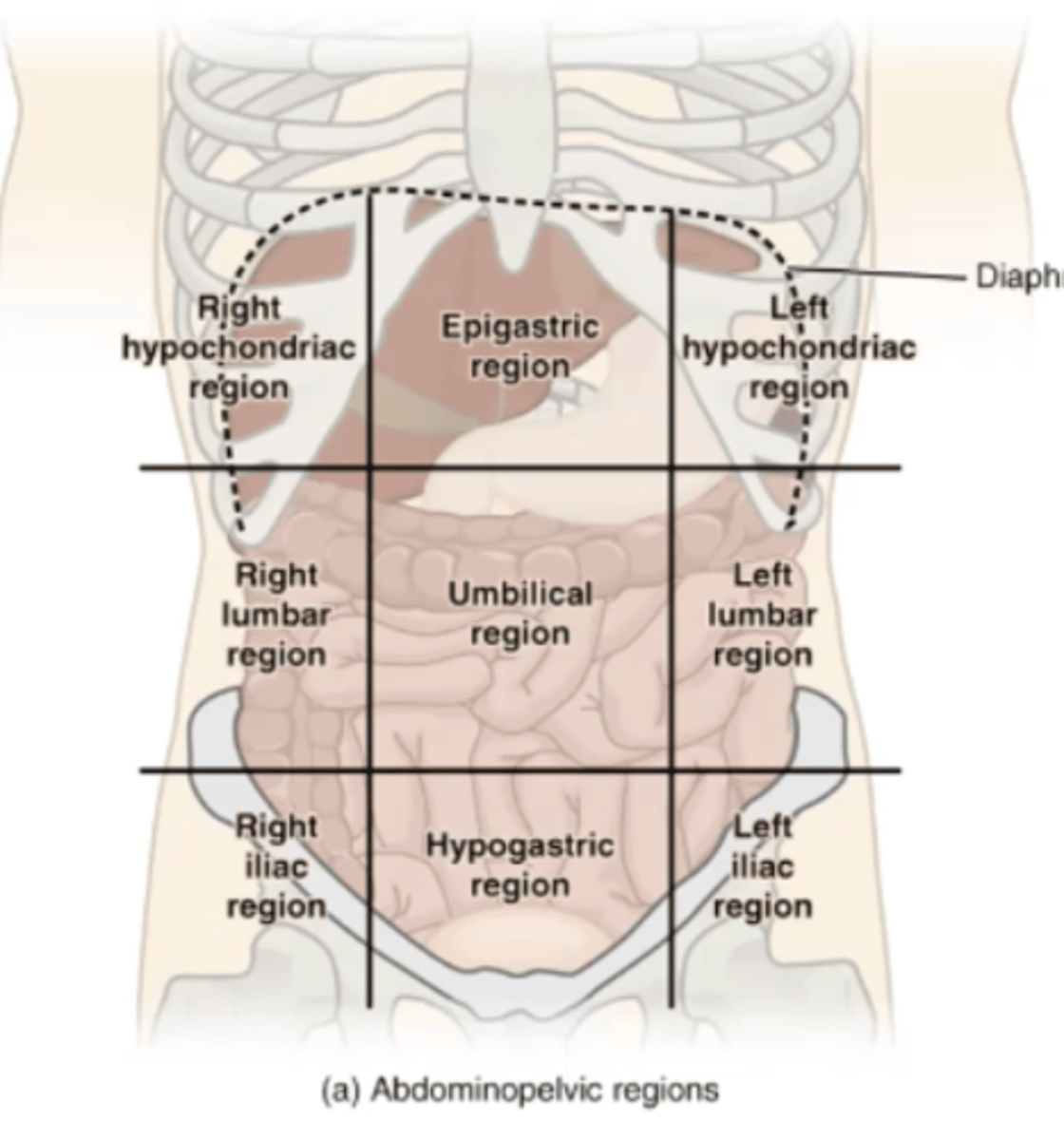
9 regions of the abdomen
Right hypochondriac, epigastric, left hypochondriac, right lumbar, umbilical, left lumbar, right iliac, hypogastric, left iliac
Lateral group muscles
External abdominal oblique, internal abdominal oblique, transverse abdominis
Medial group muscles
Rectus abdominis, pyramidalis
Innervation of lateral and medial group muscles
6 lower intercostal nerves and L1
Origin of inguinal ligament
External abdominal oblique
Origin, innervation, and clinical significance of cremaster muscle
Origin: internal abdominal oblique
Innervation: genital branch of genitofemoral nerve
Cremasteric reflex:
- Afferent limb : femoral branch of genitofemoral nerve. Efferent limb : genital branch of genitofemoral nerve.
- NOT A PATHOLOGY
- Palpation of upper thigh contracts cremaster muscle, pulling testis up
- Patient with trauma/mass in testis will not have reflex
Location, contents, and importance of rectus sheath
is a strong wrapping made from the sideways belly muscles that cover the rectus abdominis (your six-pack muscle) from the front and back. It’s built from three muscle layers — external oblique in front, internal oblique split in the middle, and transversus abdominis inside — with a final inside lining called the transversalis fascia. This helps hold and protect the muscles and organs inside your belly.
Location: a fibrous compartment formed by the aponeuroses of the three flat abdominal muscles:
External oblique
Internal oblique
Transversus abdominis
It encloses the rectus abdominis muscle:
Anteriorly and posteriorly above the arcuate line
Only anteriorly below the arcuate line (posterior wall absent below this)
Contents:
- Rectus abdominis
- Inferior and superior epigastric vessels
- 5 lower intercostal nerves and subcostal nerve
Importance: compression and protection of abdominal viscera
Location and contents of inguinal canal for males and females
a short tunnel in the lower front belly with two openings — the deep ring (inside, in the fascia transversalis) and the superficial ring (outside, in the external oblique muscle). In boys, it carries the spermatic cord, and in girls, it carries the round ligament of the uterus and lymphatics. It’s an important spot in the body — and also a common place where hernias can happen!
- Lower anterior abdominal wall, just above the inguinal ligament
Runs obliquely from the deep inguinal ring to the superficial inguinal ring
Summary : Lower anterior abdominal wall, running from the deep to superficial inguinal rings
- Male contents: spermatic cord
- Female contents: round ligament of uterus and lymphatics
Cryptochordism
- Failure of testis to descend from abdominal cavity during embryonic development
- Infertility; testicular cancer
Hydrocele of the cord
when a tunnel (called the processus vaginalis) doesn’t close after the testicles move down into place. This lets fluid collect around the spermatic cord, making a soft bump. It usually shows up in baby boys or young kids and might go away on its own or need a small surgery to fix it.
- Process vaginalis fails to close after testis descend
- Fluid forms around spermatic cord
Contents of the spermatic cord
- Testicular arteries/veins
- Vas deferens
- Artery of vas deferens
- Pampiniform plexus
- Autonomic nerve fibers
- Gential branch of genitofemoral nerve
- Lymphatics
- Cremaster artery
- Cremater muscle
Direct inguinal hernia
This one goes directly through the belly wall, not through the whole inguinal canal. It’s like a shortcut!
- Does not pass through inguinal canal
- Occurs medially to epigastric vessels
- Occurs within Hesselbach's triangle
- Low risk of strangulation
- Almost always acquired
- Smaller in size; if palpated, it will be soft
- Middle aged men (over 40)
- Will sometimes require surgery
Indirect inguinal hernia (6)
This one takes the long path — it goes through the whole inguinal canal, just like how stuff normally travels in boys.
- Passes through inguinal canal
- Occurs laterally to epigastric vessels
- High risk of strangulation
- more commonly Congenital but can be acquired
- Larger in size
- Younger people
- Will always require surgery
Intraperitoneal organs
are located inside the peritoneal cavity and are completely covered by visceral peritoneum.
- Stomach
- Small intestine
- Spleen
- Liver
- Gallbladder
- Cecum w/ appendix
- Large intestine
Retroperitoneal organs
They’re not covered in visceral peritoneal because they aren’t inside the peritoneal cavity/sack.
- Kidneys
- Adrenal glands
- Uterine cervix
- Duodenum (descending, horizontal, and ascending)
- Ascending and descending colon
- Pancreas
- Upper 2/3 of rectum
Clinical significance of the lesser sac and epiploic foramen
our tummy has a secret little pocket called the lesser sac. To get into that pocket, there’s a small doorway called the epiploic foramen. Sometimes, part of your intestines (your belly tubes) can sneak into that pocket and get stuck — that’s bad and can hurt (because it is being stranged)! But doctors can also use that doorway to get to other important places in your belly. Surgeons can use the foramen to reach structures like the pancreas or posterior stomach. It also allows access to the cystic artery during gallbladder surgery.. They even go through it to find a special blood tube called the cystic artery when they need to fix or take out the gallbladder.
TLDR :
Sometimes, part of the intestine slips through this foramen and gets stuck — that’s called an internal hernia.
If it gets squeezed too hard and can’t get blood, the tissue can die — that’s called strangulation.
Surgeons have to be very careful here — they should operate from the opposite side so they don’t damage important stuff like the porta hepatis (a group of very important blood vessels and tubes).
This spot is also used in surgery to reach the cystic artery (a little artery that gives blood to the gallbladder).
- Site of internal herniation of part of intestine into lesser sac
- Surgery can be done from here to reach important structures on other side of body
- Cystic artery of the gallbladder can be reached through foramen
Importance of greater omentum
- Mesentery (double layer of peritoneum) that has grown away from the organ and falls down around them.
- “Abdominal policeman”
- Prevents visceral peritoneum from adhering to parietal peritoneum
- Mobility via peristaltic movements of internal viscera
- Contains fat, lymphocytes, and other immune cells
- Moves toward an inflamed/infected area
- Protects and insulates abdominal organs
Clinical significance of peritoneal spaces and compartments
Your belly has a thin, slippery covering on the inside called the peritoneum — like a plastic wrap around all your organs. Inside that space are pouches and compartments where things can move or collect.
The rectouterine pouch (Douglas pouch) in females and the rectovesical pouch in males are low points in the peritoneal cavity where fluid may collect, particularly in infection or inflammation.
Peritonitis is inflammation of the peritoneum, often caused by infection from perforated organs or injury (stab wound of a perforated appendicitis)
Ascites is abnormal fluid buildup in the peritoneal cavity, commonly associated with liver cirrhosis.
When liver breaks down drugs/alcohol, a by product of it H2O2 (hydrogen peroxide) which is toxic to living tissue → inflammation → fibroids → blocking of blood flow
Eventually leads to tissue irritation/infection
Paracentesis is a medical procedure to drain this fluid for relief or diagnosis.
Catheter to the side (maybe weekly drainage issue), put the catheter in, wait, go down, and then massage the patient’s tummy to get the fluid out
- Increase in fluid accumulation post-op
- Caused by improper movement of peritoneum
- Leads to tissue irritation/infection
Foregut structures (7) and blood supply
Structures:
- Esophagus
- Stomach
- Liver
- Pancreas
- Biliary system
- Gallbladder
- Duodenum (1st part)
Blood supply: celiac trunk
Midgut structures (5) and blood supply
Structures:
- Duodenum (2,3,4th parts)
- Jejunum
- Ileum
- Ascending colon
- Right 2/3 of transverse colon
Blood supply: superior mesenteric artery
Hindgut structures (5) and blood supply
Structures:
- Left 1/3 of transverse colon
- Descending colon
- Sigmoid colon
- Rectum
- Upper anal canal
Blood supply: inferior mesenteric artery
Innervations of foregut, midgut, and hindgut
Parasympathetic:
- Foregut to Midgut: Vagus nerve (CN X)
- Hindgut: Pelvic splanchnic nerves (S2, S3, S4)
Sympathetic:
- Spinal segments T5-L2
Blood supply and veinous drainage of esophagus
Blood supply:
- Cervical: inferior thyroid artery
- Thoracic: thoracic aorta/bronchial arteries
- Lower: left gastric artery/inferior phrenic artery
Drainage:
Inferior thyroid v. -> azygos v. -> hemiazygos v. -> gastric veins -> portal v.
Esophageal varices
- Swollen, varicose veins at the lower end of the esophagus
- Often seen in liver cirrhosis patients
- If ruptured, patient can bleed to death
Histology of esophagus
Mucosa, submucosa, muscularis, adventitia
GI tract epithelium
Stratified non-keratinized squamous epithelium:
- Mouth -> esophageal sphincter of stomach
- Lower anal canal -> external anal canal
Simple columnar epithelium:
- Stomach -> upper anal canal
Zenker's diverticulum
- Outpouching of the upper esophagus
- Dysphagia and halitosis
- Ulceration, bleeding, and inflammation
- Treated with surgery
Achalasia
- Failure of secretomotor/peristaltic function of esophagus
- Dilated proximal esophagus and aperistalsis (The upper (proximal) part of the esophagus gets stretched out (dilated) because food sits there and doesn’t move down. Aperistalsis = no normal squeezing waves to move food.)
- Dysphagia for solid and liquid (Most other swallowing problems cause trouble with solids first, then liquids later. But in achalasia, both are hard to swallow from the beginning.)
- Increased LES pressure (The lower esophageal sphincter (LES) stays tight and doesn’t relax, so food can’t get into the stomach easily. That's why the pressure is increased.)
Barret's esophagus
- Cells in the epithelial tissue of the esophagus are damaged by chronic acid exposure
- Can lead to cancer
Importance of stomach rugae and oblique muscle layer
Stomach rugae: expansion of stomach
Oblique muscle layer: churning of stomach
Gastric pit
- Narrow channels extending into the wall of the stomach
- Mucosa cells
Gastric gland
- Bottom of gastric pits between rugae
- Secrete gastric juices
Cells found in gastric glands
Parietal cells:
- Produce HCl and intrinsic factor
- Pepsin formation and B-12 absorption
Chief cells:
- Produce pepsinogen
- Activated by HCl to form pepsin
G cells:
- Produce gastrin
- Stimulates parietal cells
Blood supply, drainage, and innervation of stomach
Blood supply:
- Left gastric artery
- Common hepatic artery
- Splenic artery
Drainage: portal vein
Parasympathetic Innervation: Vagus nerve (CN X)
Sympathetic innervation: splanchnic nerves
Gastric ulcers
- Open sores in the lining of the stomach
- Pain increased by eating
- No acid, no ulcer
Vagotomy
- Cutting of certain branches of the vagus nerve
- Reduce the amount of gastric acid produced and thus reduce the recurrence of ulcers
Hemigastrectomy
- Removal of part of the stomach
- Pylorus and antrum
- Removes gastric glands containing parietal and G cells
Sliding hiatal hernia
- Abdominal esophagus and stomach cardia slide up through esophageal hiatus
- Regurgitation and heartburn
Paraesophageal hiatal hernia
- Fundus and peritoneum passes through esophageal hiatus
- No regurgitation
Fundoplication
Fundus of stomach is wrapped around the lower esophagus and anchored to diaphragm to prevent reflux
Hypertrophic plyloric stenosis
Significance:
- Hypertrophy of circular muscles in pyloric sphincter
- Narrows pyloric lumen, obstructing food passage
- Projectile, non-bilious vomiting after feeding
Treatment:
- Longitudinal pyloromyotomy, leaving mucosa intact
- removal of longitudinal pyloric sphincter muscle
Functions of duodenum (4)
1.) Regulates stomach and gallbladder emptying
2.) Secretin secretion
3.) Cholecystokinin secretion
4.) Enterogastrone secretion
Parts of duodenum
Superior, descending, inferior, ascending
Superior duodenum
- 5 cm long, T12-L1
- Anterior to portal vein and common bile duct
- Duodenal gap: site of ulcer
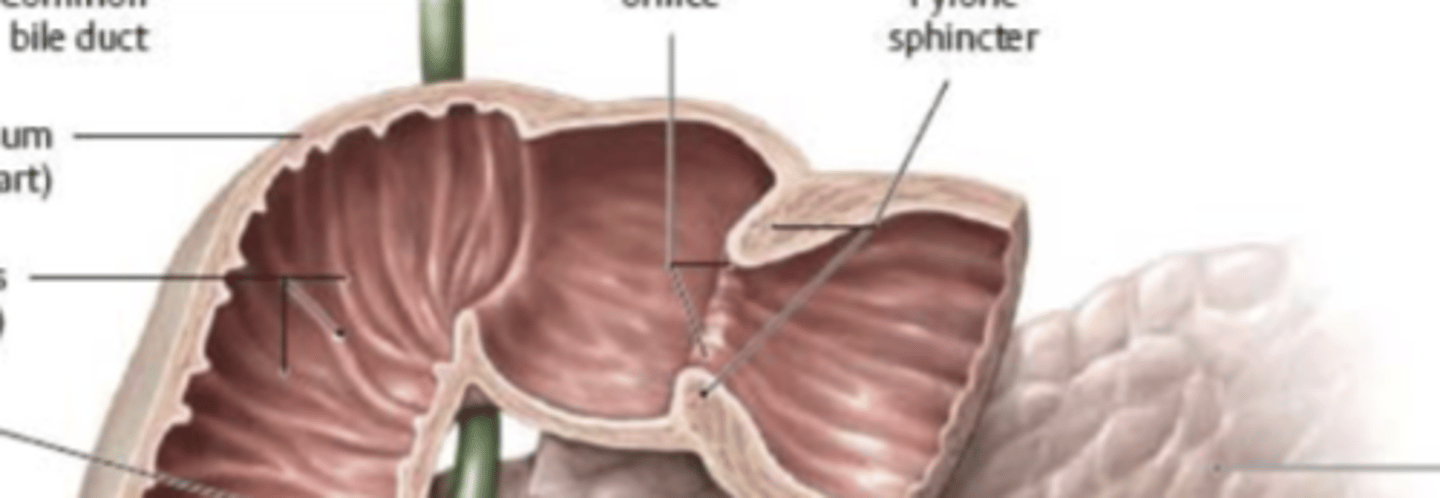
Descending duodenum
- 7.5 cm long, L1-L3
- Contains major/minor duodenal papillas
- Ampulla of Vater within major duodenal papilla
Inferior duodenum
- 10 cm long, L3
- Anterior to IVC and abdominal aorta
- Crossed anteriorly by superior mesenteric a./v.
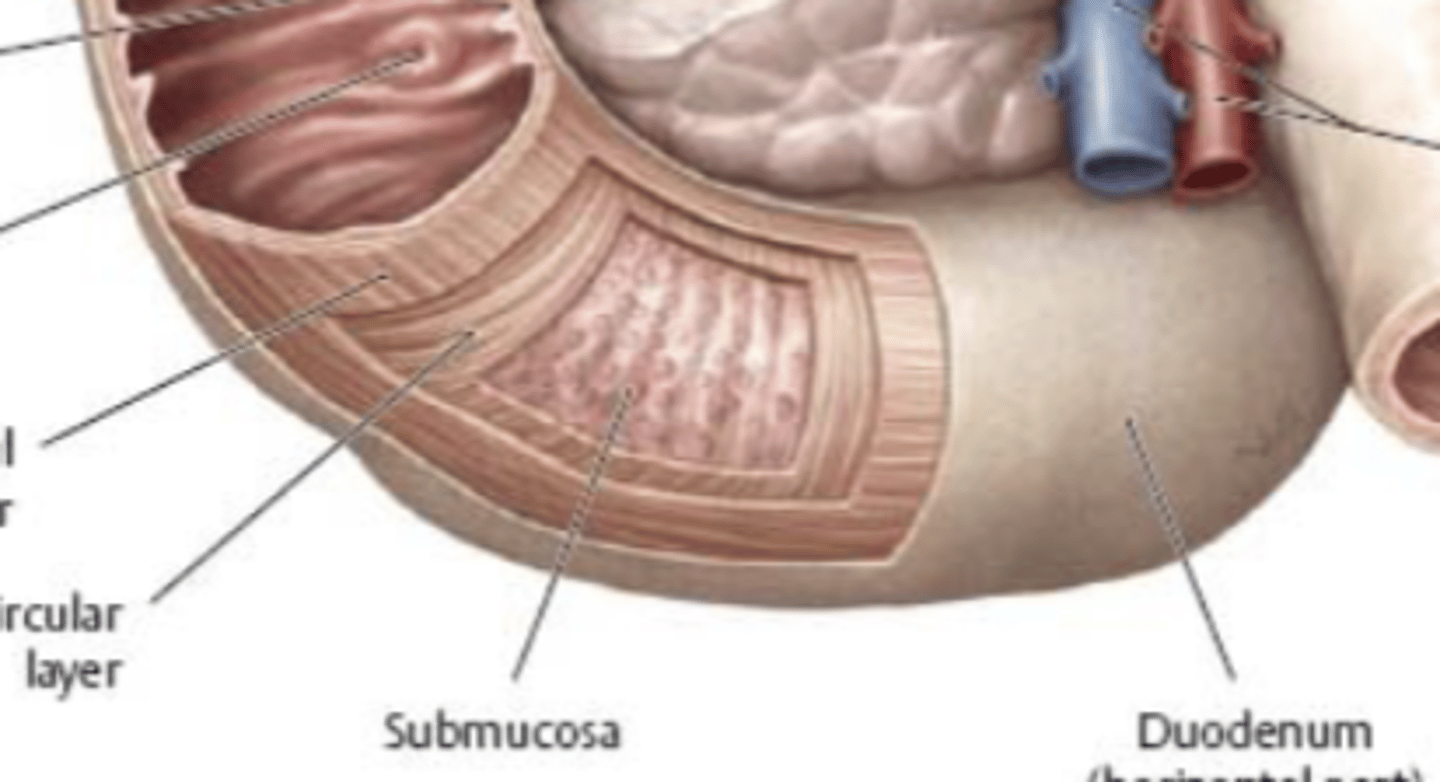
Ascending duodenum
- 2.5 cm long
- Across midline to duodenojejunal flexure at L1-L2
Innervation of digestive tract
- Sympathetic and parasympathetic
- Submucosal plexus of Meissner: secretomotor
- Myenteric plexus of Auerbach: peristaltic movement
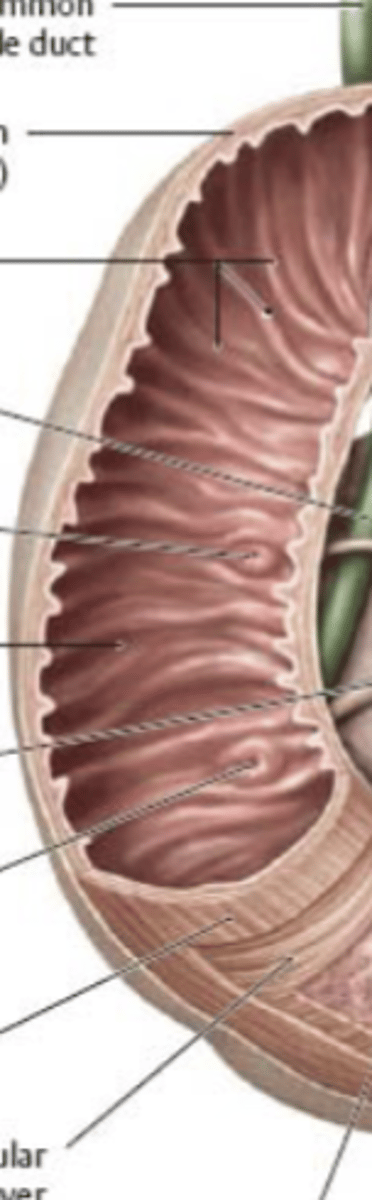
Function of jejunum and ileum
Absorption of digested food
Jejunum: folate absorption
Ileum: B12 absorption
Blood supply, drainage, and innervation of the small intestine
Blood supply: superior mesenteric artery
Drainage: superior mesenteric vein
Parasympathetic: vagus nerve (CN X); peristalsis and glandular secretion
Sympathetic: splanchnic nerves; inhibition of PNS function
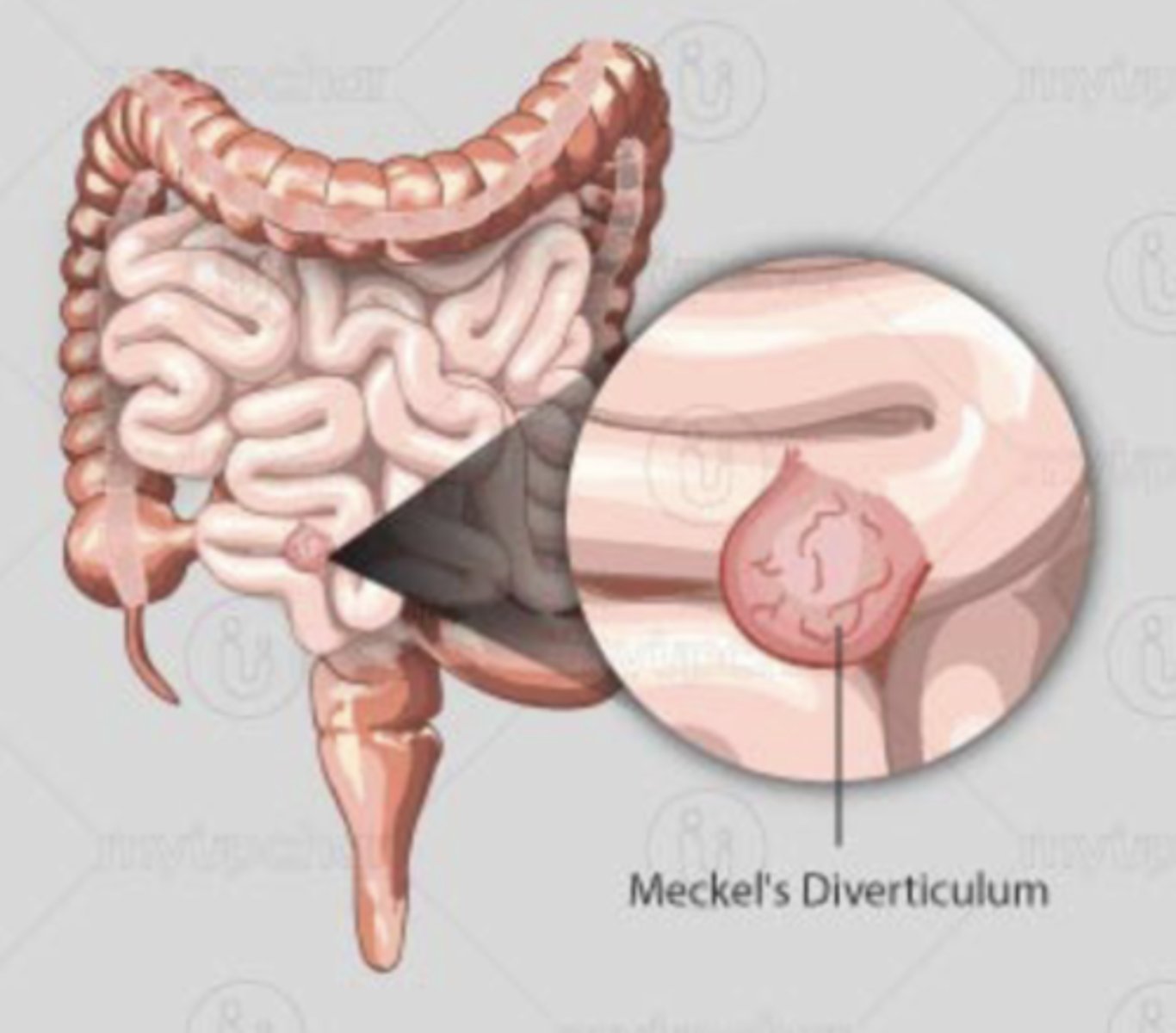
Meckel's diverticulum
- Outpouching of ileum 50-75 cm of ileocecal valve
- Congenital disorder resulting from persistence of embryonic vitelline duct
- Mimics pain of appendicitis
- Rule of 2's: 2% of children, 2 years of age, 2 feet from ileocecal valve, 2 types of mucosa
Location and function of appendix
Location: posteromedial portion of cecum
Function: houses extra e. coli
Appendicitis
- Inflammation of the appendix
- Caused by fecal matter/bacteria entering appendix
- Treated by appendectomy at McBurney's point
McBurney's point
- Point on lower right side of abdomen
- ~2/3 of the way between umbilicus and right anterior superior iliac spine
Blood supply and drainage of colon
Blood supply:
- Superior mesenteric a.
- Inferior mesenteric v.
Drainage:
- Colic v. -> superior mesenteric v. -> portal v.
Significance of the pectinate line of the anal canal
- Junction between the internal and external canal
- Transition between epithelium and innervation
- Simple columnar -> non-keratinized stratified squamous epithelium
- pelvic splanchnic nerves -> pudendal nerve
Blood supply, veinous drainage, and innervation of rectum and anus
Blood supply:
- Superior rectal artery
- Middle rectal artery
- Inferior rectal artery
Drainage:
- Superior rectal v. -> inferior mesenteric v. -> portal v.
- Middle and inferior rectal v. -> internal iliac v.
Parasympathetic innervation: pudendal nerve
Sympathetic innervation: pelvic splanchnic nerves
Clinical significance of portocaval anastomosis
Provides alternate routes of blood circulation in case of blockage in liver or portal vein
Internal hemorrhoids (Piles)
- Prolapse of rectal mucosa containing superior rectal veins
- Occur above pectinate line
- Painless bleeding
External hemorrhoids
- Blood clots in inferior rectal veins
- Occur below pectinate line
- Painful bleeding
Hirschsprung's disease
- Conginetal megacolon
- Common in those w/ down syndrome/Chaga's
- Deficiency of ganglion cells in submucosal and myenteric plexuses
- Loss of secretomotor/peristaltic function
- Causes dilated bowels
- Leads to prolapse of rectum or cancer
Functions of the liver
- Bile production
- Carbohydrate and protein metabolism
- Storage of glycogen
- Vitamin and protein production
- Detoxification
Glisson's triad (portal triad)
Branches of portal vein, hepatic artery and bile duct
Disse's space
- Space between the vessel wall of the sinusoids and the surface of the liver cell
- Blood plasma passes through
- Ito cells lie here
Ito cells
- Found in Disse's space
- Fat storage cells
- Accumulate vitamin A
Hepatocytes
- Liver cells
- Detoxify blood
- Produce bile
Clinical significance of liver cirrhosis
- Compromised blood flow of the liver
- Necrosis -> fibrosis
- Caused by alcohol/drug use, lifestyle
Development, diagnosis, and treatment of gallstones
Development:
- Imbalance in bile cholesterol and salt concentration
- Precipitation of either forms gallstone
Diagnosis: 5 F's
- Female
- Fertile
- Forty-fifty
- Full-figured
- Fair
Treatment: cholecystectomy
Secondary condition of gallstones
Cholecystitis
Endocrine functions of pancreas
- Alpha cells: glucagon
- Beta cells: insulin
- Delta cells: somatostatin
Exocrine functions of pancreas
- Acinar cells: sodium bicarbonate, amylase, and lipase
- S cells: secretin (stimulate sodium bicarbonate production)
- I cells: CCK (stimulate enzyme production)
Clinical significance of pancreatitis
- Inflammation of the pancreas
- Caused by blockage of ampulla of vater
- Severe left abdominal pain radiating into back
- Can lead to cancer
Clinical significance of cystic fibrosis
- Congenital defect of chloride channels
- Affects respiratory system and GI tract
- Mucus/gastric juices are thick and pasty
- Blocks lamela
Functions of the spleen
- Destroys defective RBCs
- Hemoglobin storage
- Maturation of RBCs by removing Howell-Jolly bodies
Functions of the kidney
- Urine production
- Electrolyte balance
- Water balance
- pH balance
Function and parts of a nephron
- Functional unit of the kidney,
- Glomerulus, renal tubule, and collecting tubule
Juxtaglomerular complex
Specialized cells that secrete renin when glomerular blood pressure decreases
Renin-angiotensin-aldosterone system
- Hormone cascade pathway that helps regulate blood pressure and blood volume
- Detects when blood pressure is low
- Raises blood pressure
- Renin --> angiotensin I --> angiotensin II --> aldosterone
Blood supply and drainage of kidney
Blood supply:
- Abdominal aorta
- Renal arteries
Drainage: renal veins
Layers of the adrenal cortex
1. )Zona glomerulosa
- Produces mineralocorticoids
- Regulates electrolyte and fluid homeostasis
2.) Zona fasciculata
- Produces glucocorticoids
- Regulates macronutrient metabolism
3.) Zona reticularis
- Produces epinephrine and norepinephrine
- Regulated by sympathetic nervous system
Nerves of the lumbar plexus
1.) Iliohypogastric
2.) Ilioinguinal
3.) Genitofemoral
4.) Lateral femoral cutaneous
5.) Femoral
6.) Obturator
7.) Short, direct muscular branches
Characteristics of male pelvis
Sacrum: narrow, longer, sacral promontory more ventral
Coccyx: less movable, curves ventrally
Greater sciatic notch: narrow and deep
Pelvic inlet: narrower, heart shaped
Pelvic outlet: narrower, ischial tuberosities longer, sharper, and point more medial
Characteristics of female pelvis
Sacrum: wider, shorter, sacral curvature is accentuated
Coccyx: more movable, straighter
Greater sciatic notch: wide and shallow
Pelvic inlet: wider, oval from side to side
Pelvic outlet: wider, ischial tuberosities shorter, further apart, and everted
Pelvic wall muscles
Piriformis and obturator internus
Leiomyomas (fibroids)
- Most common uterine tumors
- Estrogen sensitive muscle tumors
- During pregnancy, enlarge and obstruct delivery
Endometriosis
- Endometrial growth that occurs outside of uterus
- Under estrogen influence so it can grow and break down cyclically
- 5-10% of all women; 30-50% infertility patients
- Caused by genetics, menstrual backflow, lymphatic or vascular spread
Parts of the menstrual cycle
- Desquamation and regeneration
- Follicular/proliferative phase
- Luteal/secretory phase
Desquamation and regeneration
-1st-4th day
-Disappearance of progesterone and increase in estrogen
-Superficial portion of endometrium is shed
-Eventually, epithelium and connective tissue of functional layer regenerate basal layer
Follicular/proliferative phase
- Menses (5 days) + Proliferative phase (9 days)
- After menses, there is a gradual increase in GnRH release and subsequent gonadotropins
- Estradiol concentration increases with follicular development
- Proliferation refers to the increase in thickness of the endometrium immediately following menses
Luteal/secretory phase
- 11-14th day, ovulation occurs at end of follicular phase
- Progesterone and estradiol increase dramatically, both secreted from the corpus luteum
- Endometrium reaches maximal thickness, providing optimal environment for embryo
- If no established pregnancy, luteal phase ends with menses
Four parts of male urethra
Pre-prostatic, prostatic, membranous and spongy parts
Prostatic urethra
- Surrounded by prostate
- 4cm long
- Exit point for ejaculatory duct
- Urethral crest w/ urethral sinuses
Membranous urethra
- Between the prostate and the penis
- Cowper's glands posterolaterally
- Most vulnerable
Spongy urethra
- Runs through penis; opens at external urethral orifice
- 15-16cm long
Location and importance of epidydimis
Location: posterior surface of testes
Importance: maturation and storage of sperm
Location and importance of vas deferens
Location: runs through inguinal canal to seminal vesicle
Importance: passage of sperm to urethra
Location and importance of seminal vesicle
Location: between rectum and fundus of bladder, superior to prostate
Importance: produces an alkaline fluid that helps to form semen
Location and importance of prostate
Location: posterior to pubic symphysis
Importance: works with seminal vesicle to produce sperm
Erection
- Erectile tissue fills with blood, causing penis to enlarge and become rigid
- Corpus cavernosum and spongiosum
Seminal emission
- Stimulation of penis causes vas deferens and seminal vesicle to deliver constituents to prostatic urethra
- Produces seminal fluid for ejaculation