IPFC 1 - Thyroid disorders
1/182
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
183 Terms
Hypothyroidism
Syndrome due to thyroid hormone deficiency (thyroid hypofunction)
Sever Hypothyroidism is called
myxedema
Hyperthyroidism
Syndrome due to thyroid hormone excess (thyroid hyperfunction)
Sever Hyperthyroidism is called
Known as a thyroid storm when severe
Thyroid nodules may be ____________ or __________________
• May be unimodular or multinodular
• May be 'cold' or 'hot'
These are growths of cells on the thyroid (usually benign and can be hypo or hyperfunctioning)
Hypothalamic-Pituitary-Thyroid Axis
• Many neural inputs to the hypothalamus which stimulate secretion of TRH (thyroid releasing hormone)
• TRH then stimulates TSH (thyroid stimulating hormone) from anterior pituitary
• TSH then stimulates thyroid gland to synthesize and release of thyroid hormones (T3 and T4)
• Negative feedback loop (somatostatin, T3 and T4, and iodine inhibits)
• High levels of T3 and T4 block TSH and TRH secretion
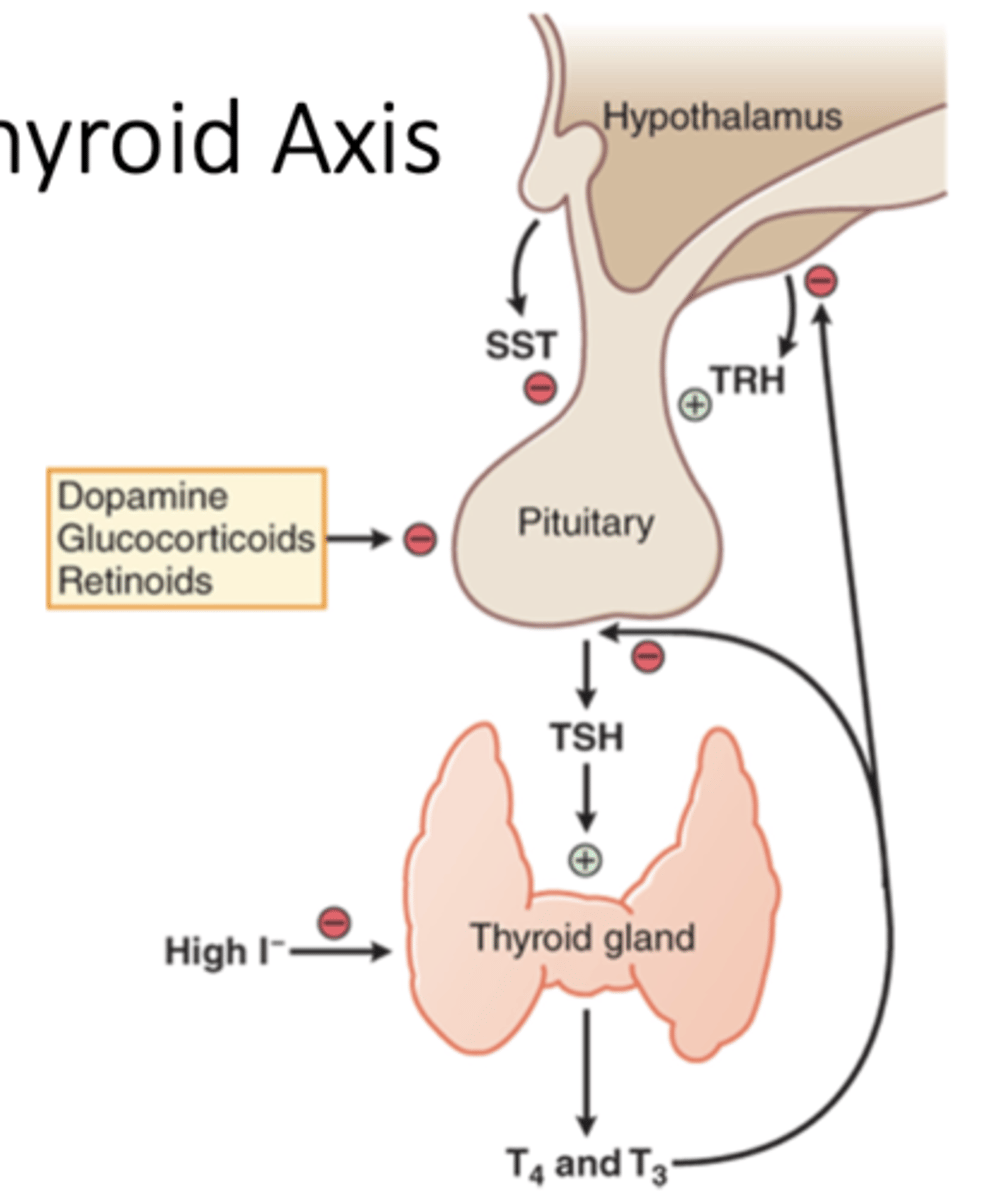
Other factors that influence thyroid hormone regulation
• Acute and chronic illness
• Starvation
• Medications
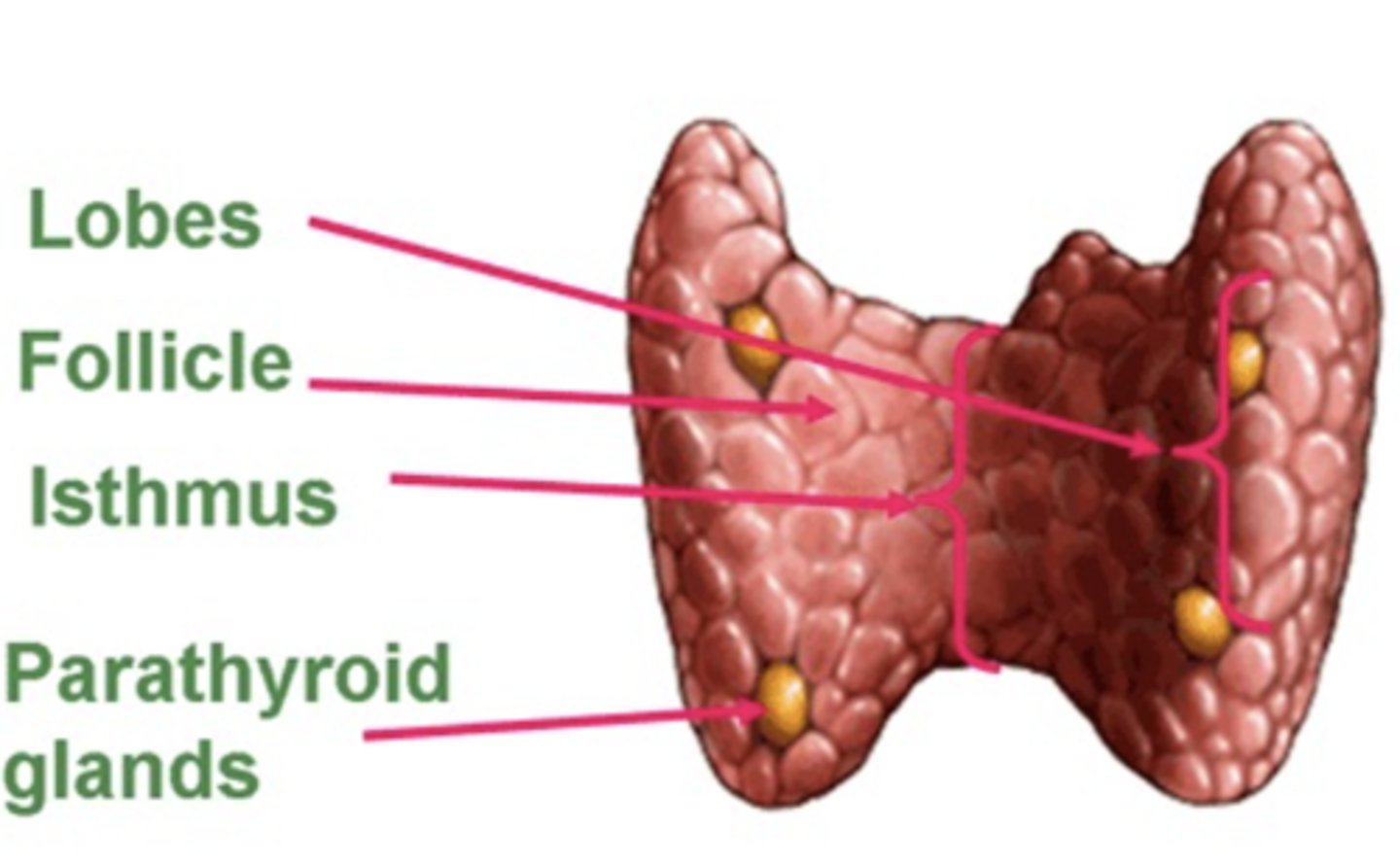
Thyroid gland
• Largest endocrine gland
• Two lateral lobes, 4 to 6cm in length
• Connected by isthmus (~5cm)
• Highly vascularized
in a healthy person you shouldn't be able to feel it
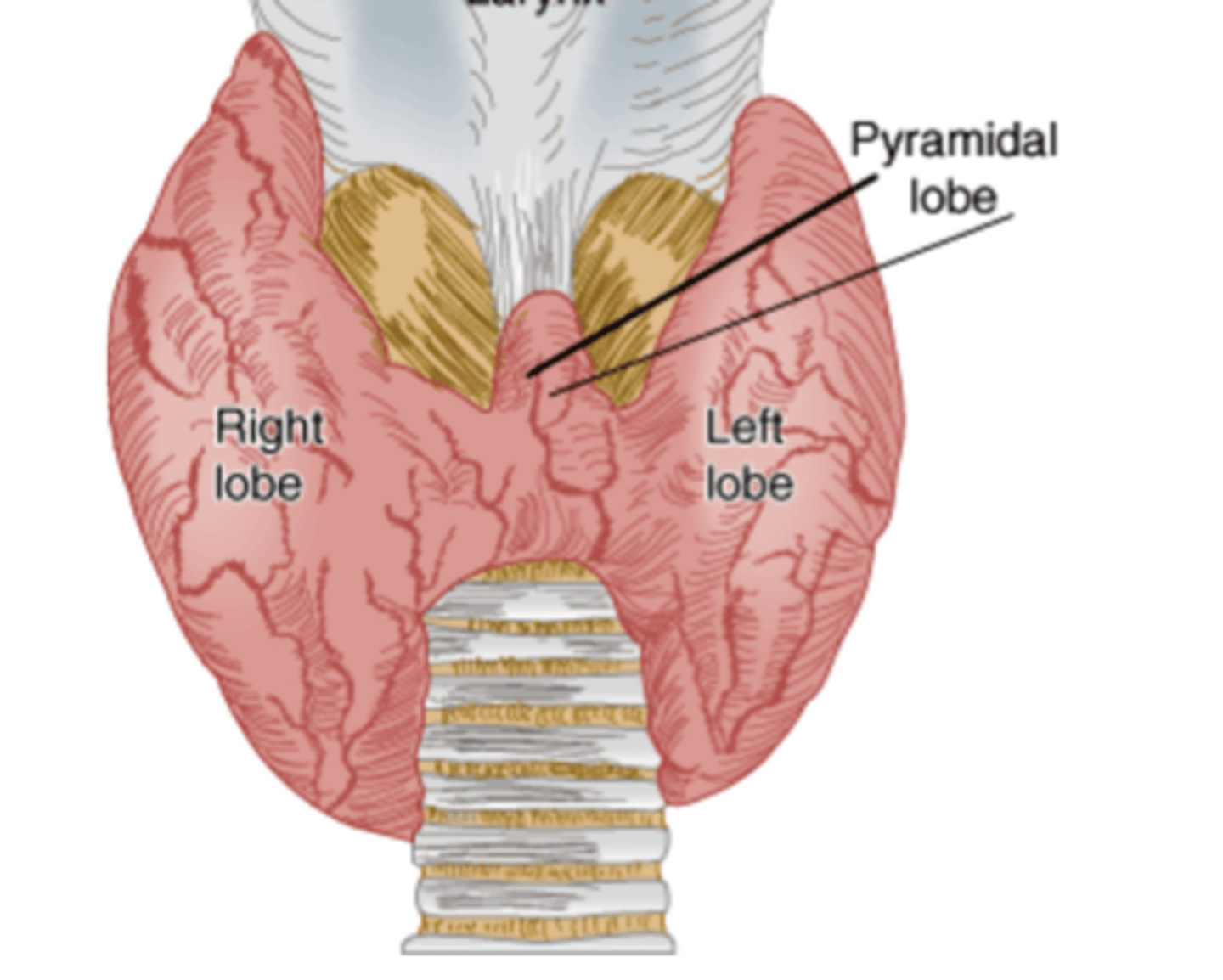
Which nerves pass under the thyroid?
Laryngeal nerves
- potential risk in hyperthyroidism surgery
Which thyroid hormone is more potent and active?
T3 (more than T4)
T/F Almost all T4 and T3 in plasma is free and unbound in the blood
False! almost all is protein bound
What proteins bind T3 and T4 in the plasma
• Thyroxine-binding globulin (TBG) (~70%)
• Albumin (~15%)
• Thyroid-binding pre-albumin (TBPA) (
T/F: T4 has a longer half-life vs T3
True, (7 days vs. ~1.5 days)
T/F Thyroid gland produces more T3 vs T4
False! more T4 (80mcg) than T3 (30-40mcg)
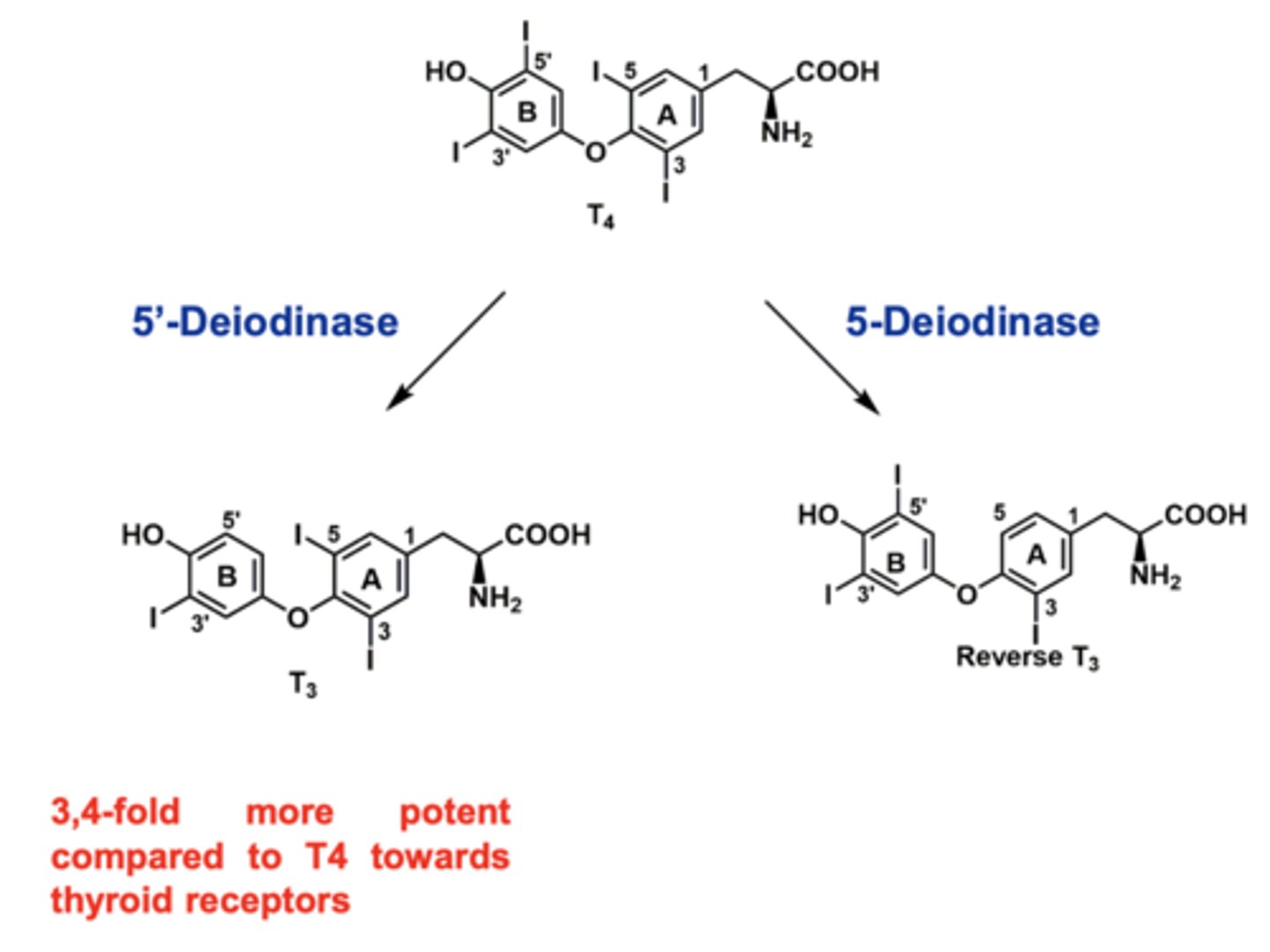
T4 is converted to T3 primarily in the _____________________
peripheral tissues
• ~ 35 to 40% of secreted T4 is converted to T3 via peripheral deiodination
• ~ 45% of secreted T4 is converted to inactive reverse T3
_____ IS THE MOST ACCURATE INDICATOR OF EUTHYROIDISM!
TSH
within the normal range will tell you if there is normal thyroid functioning
- high leveels of T3 and T4 in the body will not release much TSH, where if there is not enough, it will secrete a lot of TSH
Low TSH indicates...
hyperthyroidism
High TSH indicates...
Hypothyroidism
What are the most reliable tests for assessing thyroid hormone concentrations?
Free T4 and Free T3
Thyroid gland autoantibodies indicate...
The presence of these autoantibodies shows that the thyroid is attacking the main processes of the body
What are the thyroid gland autoantibodies
The presence of these autoantibodies shows that the thyroid is attacking the main processes of the body
Thyroglobulin antibodies (TgAb) and Thyroid peroxidase antibodies (TPOAb)
Thyroid stimulating immunoglobulin (TSI) and Thyroid receptor stimulating antibodies (TRAb)
Which autoantibodies are found in those with Grave's disease
Thyroid stimulating immunoglobulin (TSI)
Thyroid receptor stimulating antibodies (TRAb)
Thyroid follicle
functional unit of the thyroid gland that secrete T4 and T3
- contain a protein filled colloid (containing thyroglobulin that becomes T4 and T3)
- C cells (parafollicular cells) release calcitonin
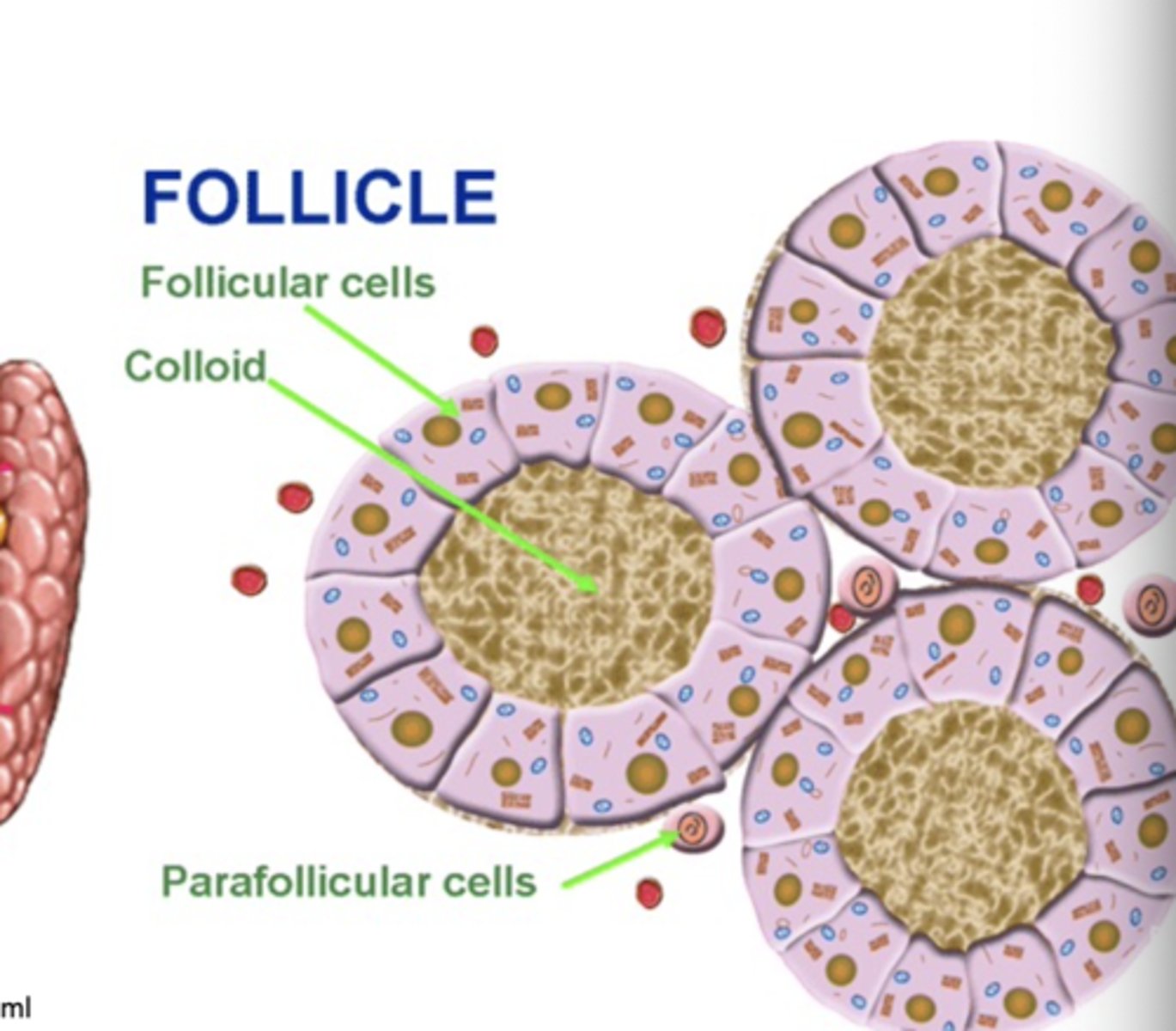
Parathyroid gland
releases parathyroid hormone in response to low calcium levels to increase serum calcium
What is the majority of thyroid hormone produced?
T4 turns into T3, and also rT3
only T3 is active, exerting effects on target organs and tissues
Measure of FT4 circulating hormone
Direct measurement of free T4
Measure of FT4I circulating hormone
Calculated free T4 index
Measure of TT4 circulating hormone
Total free and bound T4
Measure of TT3 circulating hormone
Total free and bound T3
Measure of FT3 circulating hormone
Direct measurement of free T3
Measure of FT3I circulating hormone
Calculated free T3 index
Tests of autoimmunity: TgAb
Thyroglobulin autoantibodies
Tests of autoimmunity: TPOAb / TPA
Thyroid peroxidase antibodies
Tests of autoimmunity: TSI
Thyroid stimulating antibody
Tests of autoimmunity: TRAb
Thyroid receptor antibody
Why do we use T4 to treat thyroid conditions? (I.e. synthroid)
longer half life
Tests of thyroid gland function
RAIU (radioactive iodine uptake)
Scan
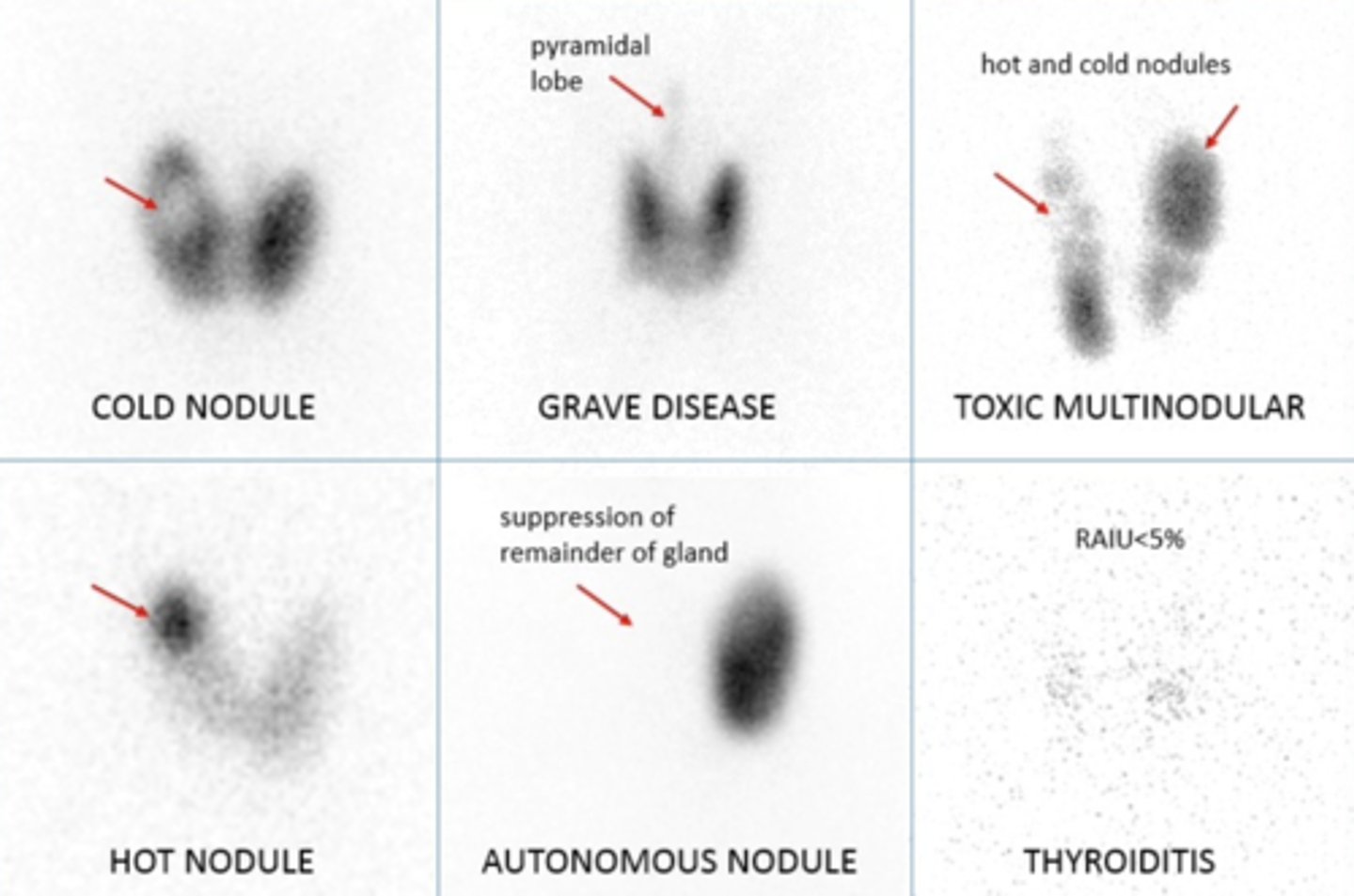
Tests of thyroid gland function: RAIU (radioactive iodine uptake)
Gland’s use of iodine after trace dose of radioactive iodine (indirect measure of hormone synthesis)
4-hr normal is 10 to 15% 24-hr normal is 20 to 30%
Thyroid Scan
Gland size, shape, and tissue activity (identifies hypermetabolic [hot] or hypometabolic [cold] areas)
Thyroglobulin test is used for..
Measuring colloid protein of normal thyroid gland
- rarely used, only for certain types of thyroid cancer
What do nodule scans look like with varying conditions?
darker indicates more thyroid hormone
Factors that can affect thyroid function tests in euthyroid patients
- ↑ TBG binding capacity
- ↓ TBG binding capacity / displacement T4 from binding sites
- ↓ peripheral T4 to T3 conversion
- ↓ pituitary and peripheral T4 to T3
- ↑ T4 clearance by enzyme induction / increase fecal loss
- ↑ /↓ TSH secretion
Increase TBG binding capacity will have what effect on lab values?
↑ TT4 ↑ TT3, everything else normal
What can cause increased TBG binding capacity
Estrogens, tamoxifen, raloxifene
Oral contraceptives
Heroin, Methadone
Clofibrate
Active hepatitis
Genetic increase in TBG
Decrease peripheral T4 to T3 conversion will have what effect on lab values?
↓ TT3 only
What can cause decrease peripheral T4 to T3 conversion?
PTU
Propranolol
Glucocorticoids
Decrease TBG binding capacity / displacement T4 from binding sites will have what effect on lab values?
↓ TT4, ↓ TT3
What can cause decrease TBG binding capacity / displacement T4 from binding sites?
Androgens
Salicylates (high dose ASA)
High-dose furosemide
Danazol
Glucocorticoids
Nephrotic syndrome
Cirrhosis/hepatic failure
Decreased pituitary and peripheral T4 to T3 can show in euthyroid patients
What will the tests show and what can cause this?
↑ TT4
↓ TT3
↑ TSH (transient) ↑ FT4I
Amiodarone can cause it
Increase T4 clearance by enzyme induction / increase fecal loss can show in euthyroid patients
What will the tests show and what can cause this?
↓ TT4
↓ FT4I
Normal or ↑ TSH
Normal or ↓ FT4
Normal or ↓ TT3
Certain drugs can cause it
Phenytoin
Phenobarbital
Carbamazepine
Rifampin
Bexarotene
Cholestyramine Colestipol
What drugs can cause ↓ TSH secretion
Dopamine, Levodopa Bromocriptine, cabergoline, pramipexole Glucocorticoids
Octreotide, Metformin
What drugs can cause ↑ TSH secretion
Metoclopramide
Domperidone
T/F Thyroid function tests may be abnormal in the context of absence of thyroid disease (euthyroidism)
True
"Euthyroid sick syndrome"
• Occurs in 37 to 70% of chronically ill or hospitalized patients
• Sicker the patient, the more extensive the thyroid function test abnormalities
• No actual thyroid disease
• Commonly triggered by serious systemic illness, starvation, infections, sepsis, acute psychosis
Altered TBG levels can be caused by:
Acute hepatitis, pregnancy, drugs (estrogens, oral contraceptives, tamoxifen, raloxifene, heroin, or methadone)
T4 is considered a "________________"
pro-hormone
T3 has significantly greater biological activity such that it is considered the active thyroid hormone, and T4 is the “pro-hormone”
Where does most T3 come from
Most T3 is converted from T4 within the target tissues by 5’-deiodinase enzymes
Thyroid hormone receptors
Inside the cell, so the hormone has to enter and find the receptor
• Two subtypes, alpha and beta, each with different isoforms
Hyperthyroidism symptoms
Increase in metabolic rate and oxygen consumption in all target tissues
Increased respiratory rate, heart rate
Increased body temperature
Increased catabolism of all fuels (carbs, fat, protein)
Circulating thyroid hormones are mainly bound to ___________________ and other proteins as well (99%+)
thyroxine-binding globulin (TBG)
Only unbound hormone is free to diffuse into target cells
How does T3 interact with the hormone receptor?
Inactive: the unliganded T3 receptor dimer bound to the thyroid hormone response element (TRE) along with corepressors acts as a suppressor of gene transcription.
Active:
- T3 and T4 circulate bound to thyroid-binding proteins (TBPs).
- The free hormones are transported into the cell by a specific transport system.
- Within the cytoplasm, T4 is converted to T3 by 5'- deiodinase; T3 then moves into the nucleus.
- T3 then binds to ligand-binding domain of the thyroid receptor (TR) monomer promoting distribution of TR homodimer and heterodimerization with retinoid X receptor (RXR) on the TRE, displacement of corepressors, and binding of coactivators.
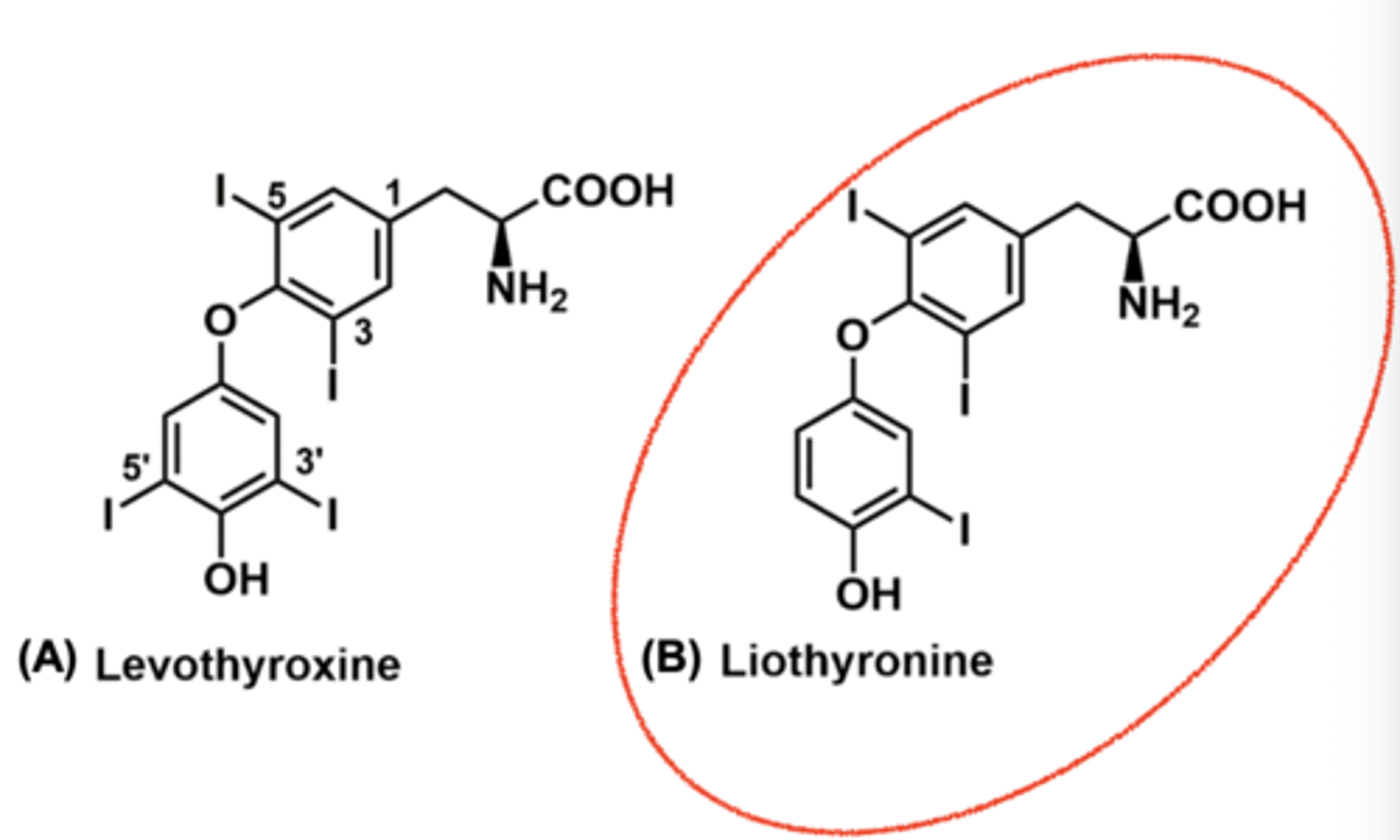
Low thyroid hormone treatment
• Management consists of hormone replacement
Options include
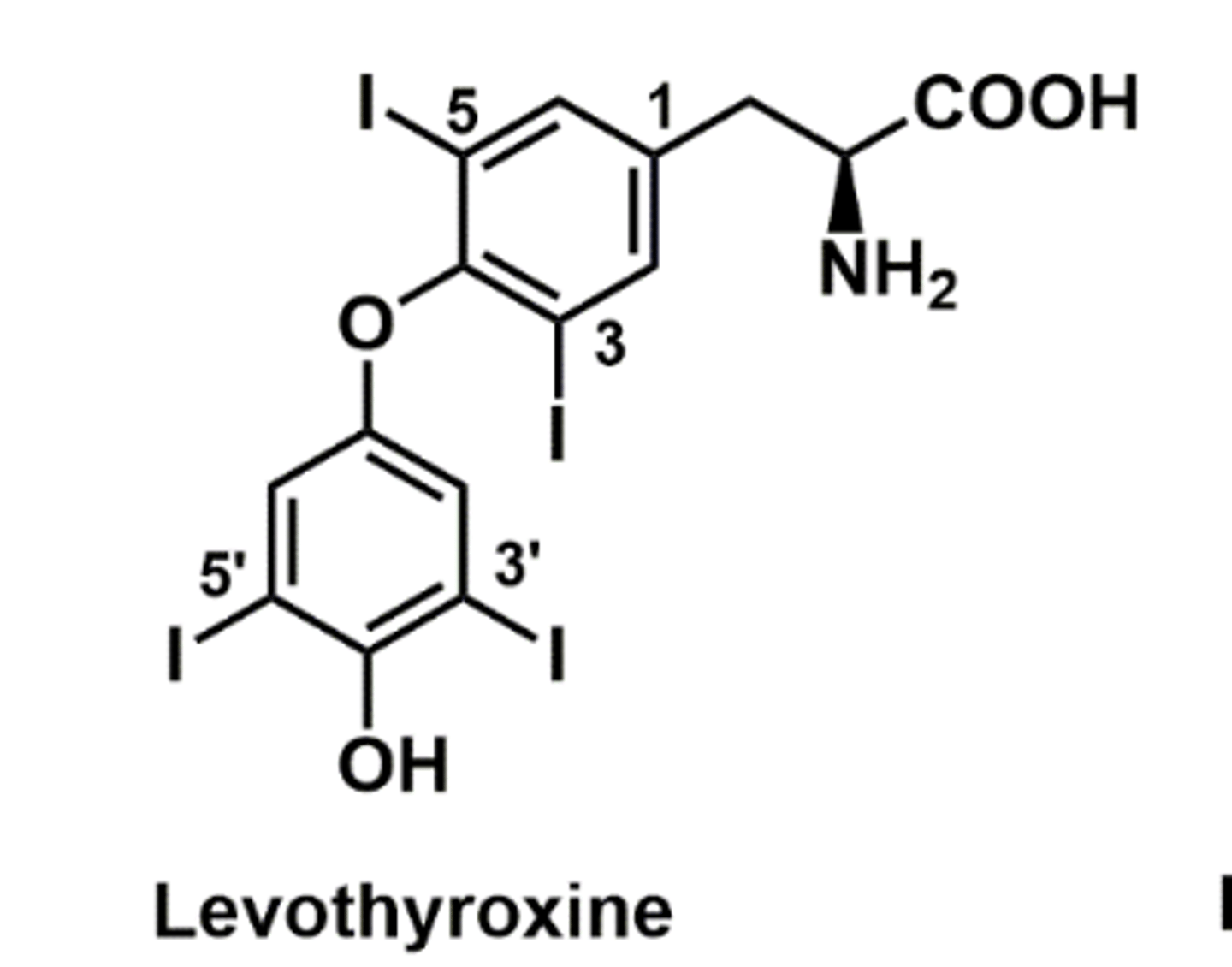
• Levothyroxine – L-T4
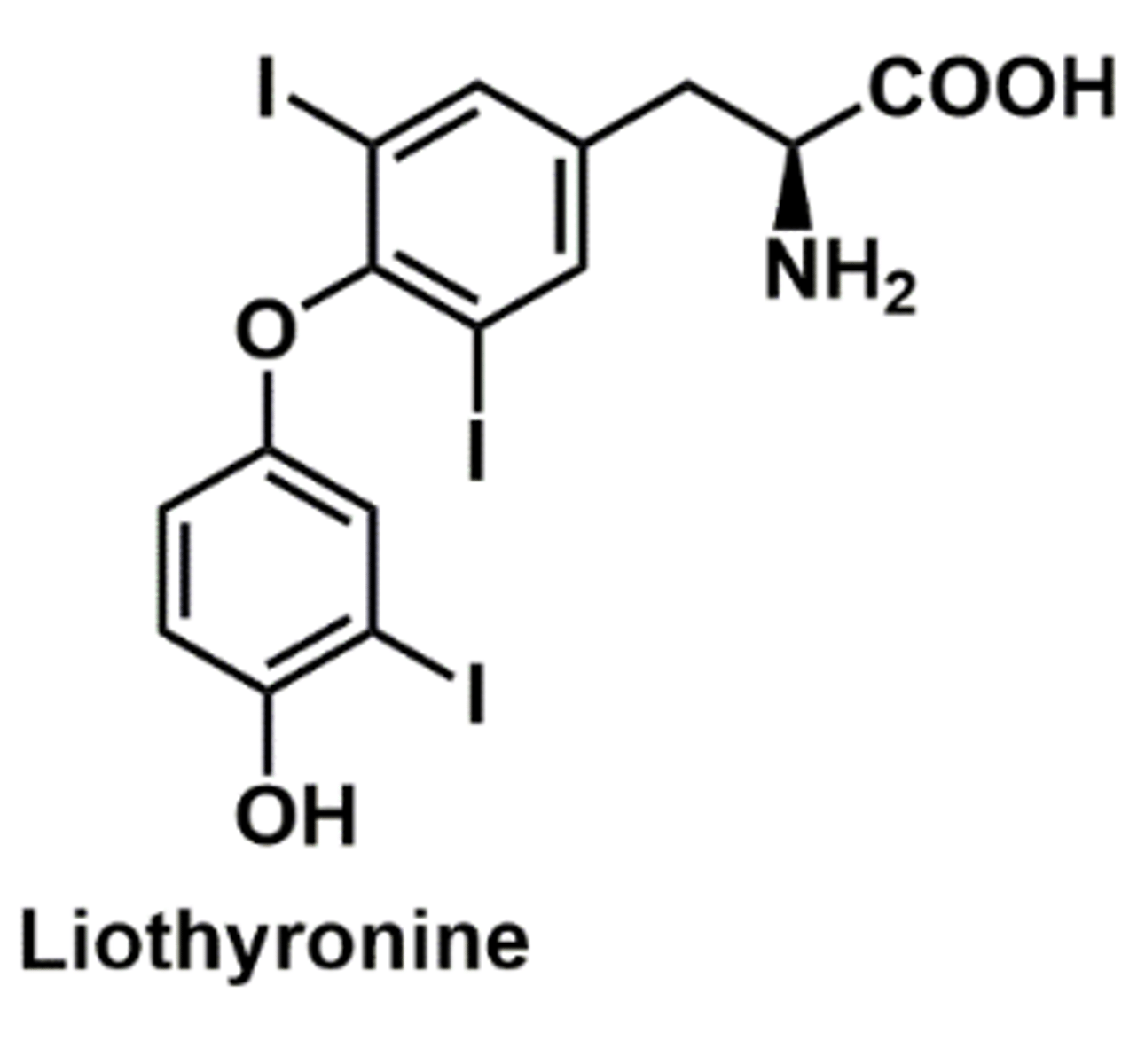
• Liothyronine - L-T3
• Liotrix – 4:1 combination of T4:T3
• (dessicated animal thyroid not used often)
Levothyroxine info
• First-line drug for hypothyroidism
Stable, long half-life (~ 7 days)
• Results in a stable pool of T4 and allows the target tissue to convert to T3 as necessary
Dosage adjusted upwards incrementally every 4-6 weeks
Levothyroxine - drug interactions
Estrogen
• Increases TBG levels, further reducing free T4
• Agents that interfere with absorption
Cholesterol lowering drugs, phosphates, iron, calcium, agents that reduce HCl secretion
Liothyronine
• Salt of triiodothyronine (T3)
• More potent and higher bioavailability
• Used when more rapid onset of action is needed
• Short half-life (~1 day), therefore not desirable for chronic replacement therapy
• Also does not change T4 levels
• May be more difficult to monitor, more adverse
cardiac effects, more expensive
Strategies of reducing thyroid hormone activity (for hyperthyroidism)
• Interference with thyroid hormone production
• e.g. thoiamides, iodides
• Blockage of thyroid hormone release
• e.g. iodides
• Destruction of the thyroid gland
• e.g. radioactive iodine, surgery
• Blockage of thyroid hormone effects at target tissues (in development)
• Supportive care for symptom management
• e.g. β-blockers
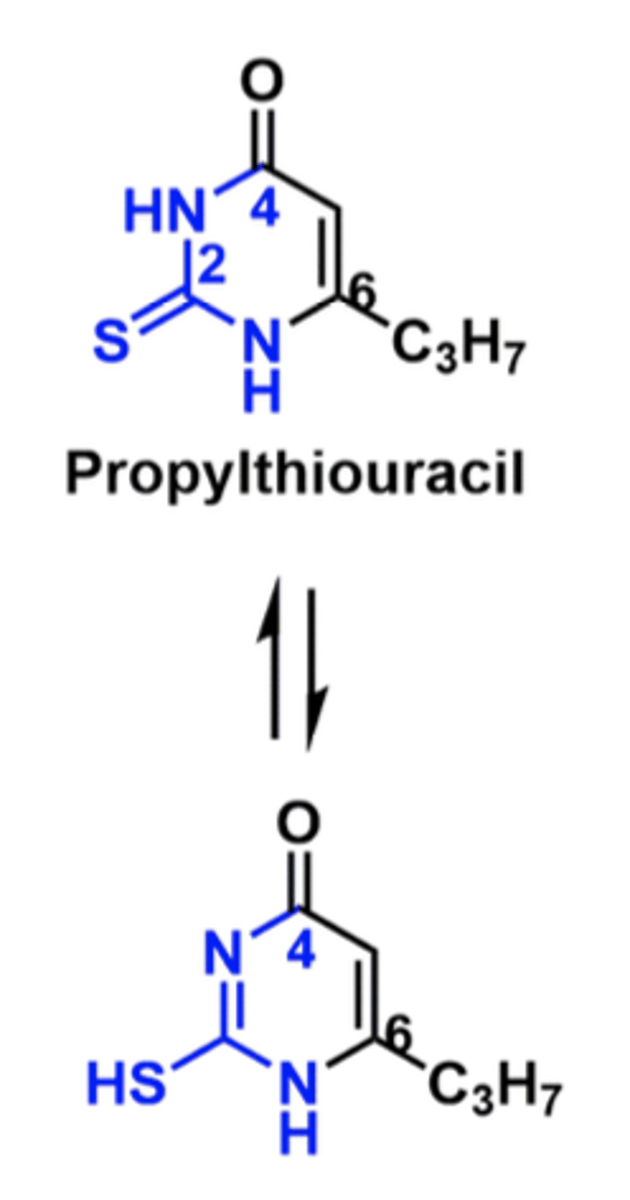
Thioamides MOA
Inhibition of thyroid peroxidase
• Iodine incorporation into tyrosyl residues of thyroglobulin is inhibited, as is coupling of these iodotyrosyl residues to form iodothyronines
• Does not affect thyroid hormone storage or release, therefore onset of action may be 3-4 weeks (because you have storage of hormone still)
Secondary mechanism: Propylthiouracil, but not methimazole, also inhibits peripheral deiodination (T4 to T3 conversion)
Thioamides Pharmacokinetics
• Propylthiouracil has a bioavailibility of up to
80% (GOOD)
• Accumulates in the thyroid gland (GOOD)
• Metabolized to glucuronide conjugate and excreted
• Both thioamides have short serum half-lives but long functional half-lives due to accumulation in the thyroid gland
PTU and Methimazole toxicity
• Cross-sensitivity of about 50% between methimazole and PTU
- Itchy rash, fever, arthralgia, benign, transient leukopenia
- Rare: jaundice, agranulocytosis; liver failure (only PTU)
"Wolff-Chaikoff" effect of Iodides
• High doses of iodide cause acute inhibition of the synthesis of iodotyrosines and iodothyronines
• Paradoxical effect; an autoregulatory phenomenon to prevent excess thyroid hormone production
• Iodides inhibit their own transport, synthesis of thyroid hormones, and release of thyroid hormone
Iodides onset
Requires high circulating levels of iodide
- Quick onset, but effect is transient (~ 3 weeks), followed by resumption of normal organification
PTU vs. Methimazole
• PTU may be better in severe states since it also inhibits peripheral deiodination (T4 to T3 conversion)
• Methimazole often is drug of choice due to its longer half-life and less frequent dosing
• PTU is preferred in the first trimester of pregnancy due to concerns with methimazole
Radioactive iodine treatment
• Sodium-131 Iodide is used to destroy thyroid tissue
• Used for hyperthyroidism, thyroid cancer
• Administered orally, absorbed rapidly
• It accumulates in the thyroid and emits β– and γ- radiation which can pass through 0.4-2 mm of human tissue and destroy the tissue
• Is a teratogen that crosses the placenta, excreted in breastmilk
• Other iodine isotopes are used for scanning purposes
Potassium iodide
• High levels of iodine-131 are produced as a nuclear fission by- product, released after nuclear detonations or uncontrolled reactions
• Non-radioactive iodine can be taken immediately before or within 3-4 hours of exposure to radioactive iodine to compete for uptake into the thyroid
β-blockers
• Thyroid hormone enhances sympathetic activation of the CV system
• Hyperthyroidism causes tachycardia, palpitations, arrhythmia
• β-blockers such as propranolol are used to treat cardiovascular symptoms by antagonizing the sympathetic effects of thyrotoxicosis
• Reduce tachycardia, tremor, palpitations, anxiety, etc.
Other adjunctive treatments
- Non-dihydropyridine type calcium channel blockers, second line to beta- blockers
Corticosteroids MOA
• blocks some T4 to T3 conversion
• used during thyroid storm
What may added to thiamine therapy in Grave's disease
Immunosuppressants such as rituximab
Other anions used for hypothyroidism
perchlorate (Cl04-), pertechnetate (TcO4-), and thiocyanate (SCN-), as well as nitrate can compete with iodide for transport into the thyroid
Hypothyroidism leads to...
goiter, cretinism, myxedema, Hashimoto's disease
Hyperthyroidism leads to...
Grave's disease, generalized resistance to thyroid hormone (GRTH)
-Thyroid cancer
Risk factors for thyroid dysfunction
Congenital (birth) defects, radiation/radioactive iodine treatment, drug-induced, viral infections, female sex, surgical removal
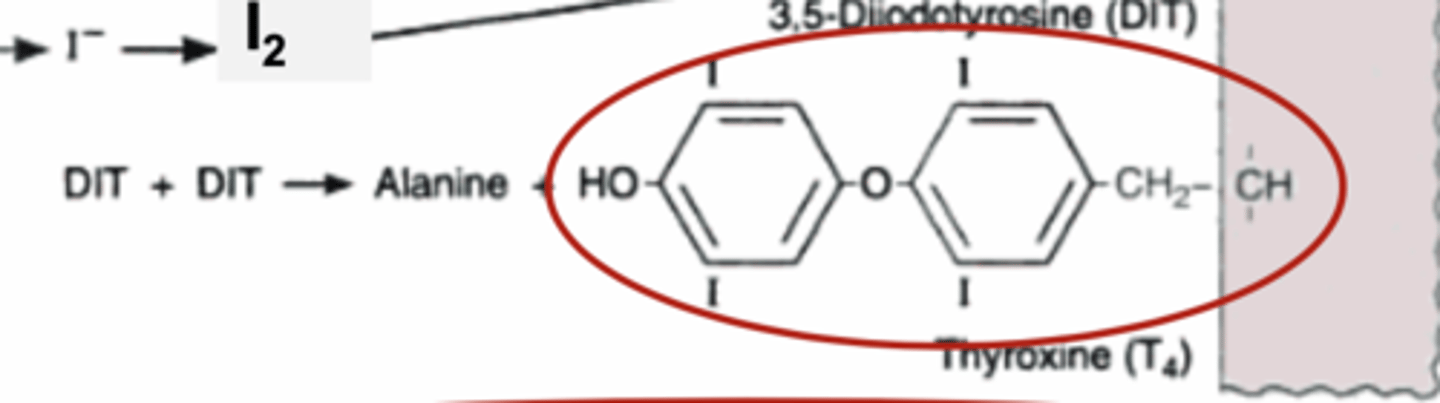
T4 structure
Pharmacotherapy classes to treat thyroid dysfunction
1. Thyroid replacement therapy:
Natural THs, synthetic THs (levothyroxine, liothyronine, dextrothyroxine, liotix)
2. Antithyroid drugs:
Sodium iodide, thionamides (methimazole, propylthiouracil), Lugol's solution (potassium iodide KI and iodine I2, 2:1)
3. Thyroid Imaging agents:
Radioiodine (131I, 125I), perchlorate (ClO4-/pertechnetate (TcO4-)
4. Beta blockers:
Propranolol, atenolol, metoprolol (to treat the symptoms of hyperthyroidism)
5. Other: Corticosteroids (prednisone)
T/F rT3 has NO pharmacologic activity
True
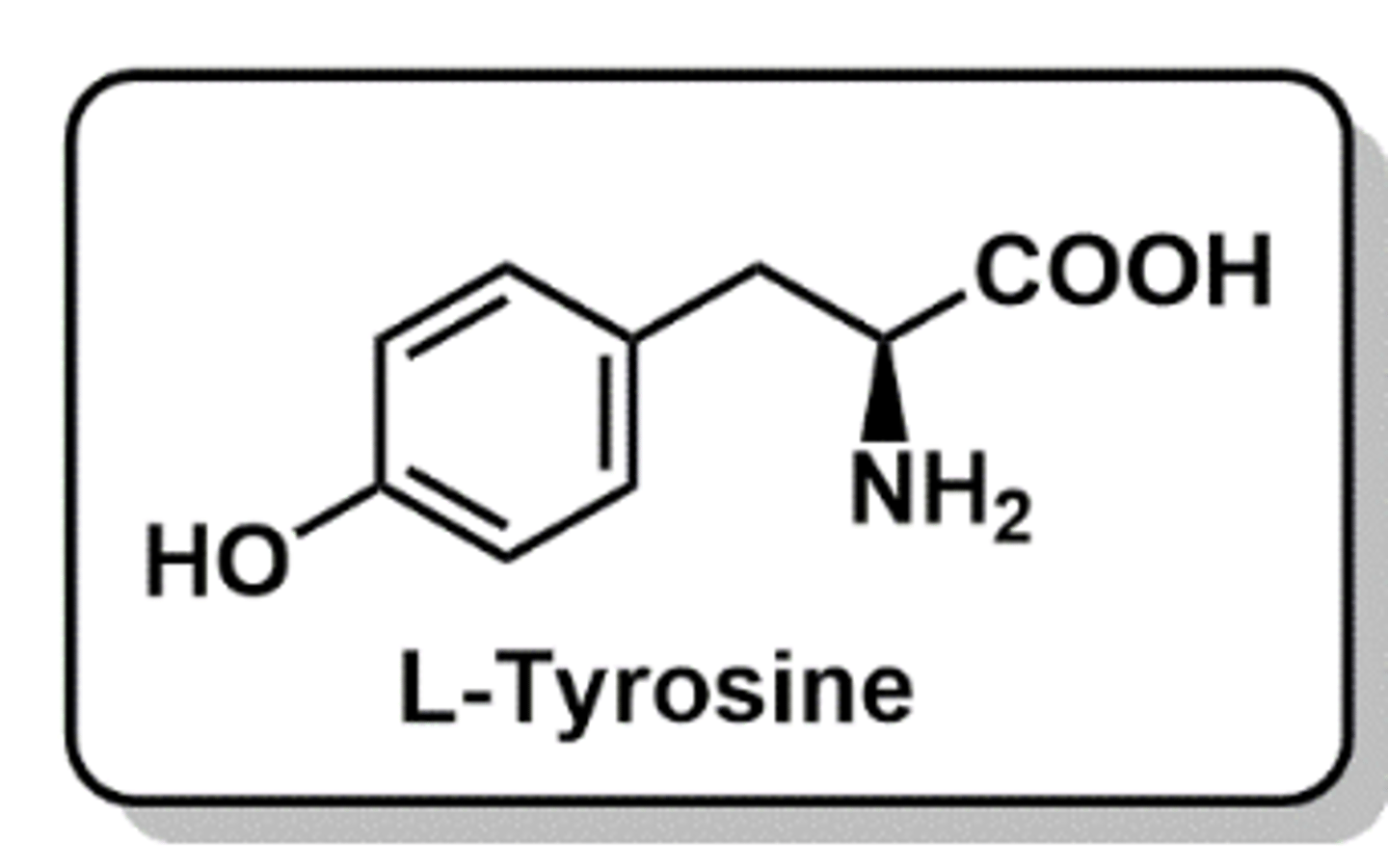
Synthetic thyroid hormones
- Derived from the amino acid L-tyrosine
- Levothyroxine has a long in vivo half-life
- Liotrix is a mixture of sodium salts of T4 and T3 in a ratio of 4:1
- Used to treat hypothyroidism
- Given either orally or through IV
- LIGHT SENSITIVE because of the C-I bonds
Levothyroxine, Liothyronine, L-tyrosine
Levothyroxine structure
T4
2 iodines at C3' and C5'
Liothyronine structure
T3
missing one iodine
L-tyrosine
Does Levothyroxine or Liothyronine have a faster onset of action? Why?
The more ionized one is water soluble so it cannot cross over as easily and bind - This is levothyroxine
Liothyronine is missing the one iodine so it is much less ionized and can more easily cross over and bind TBG - giving it a faster onset of action
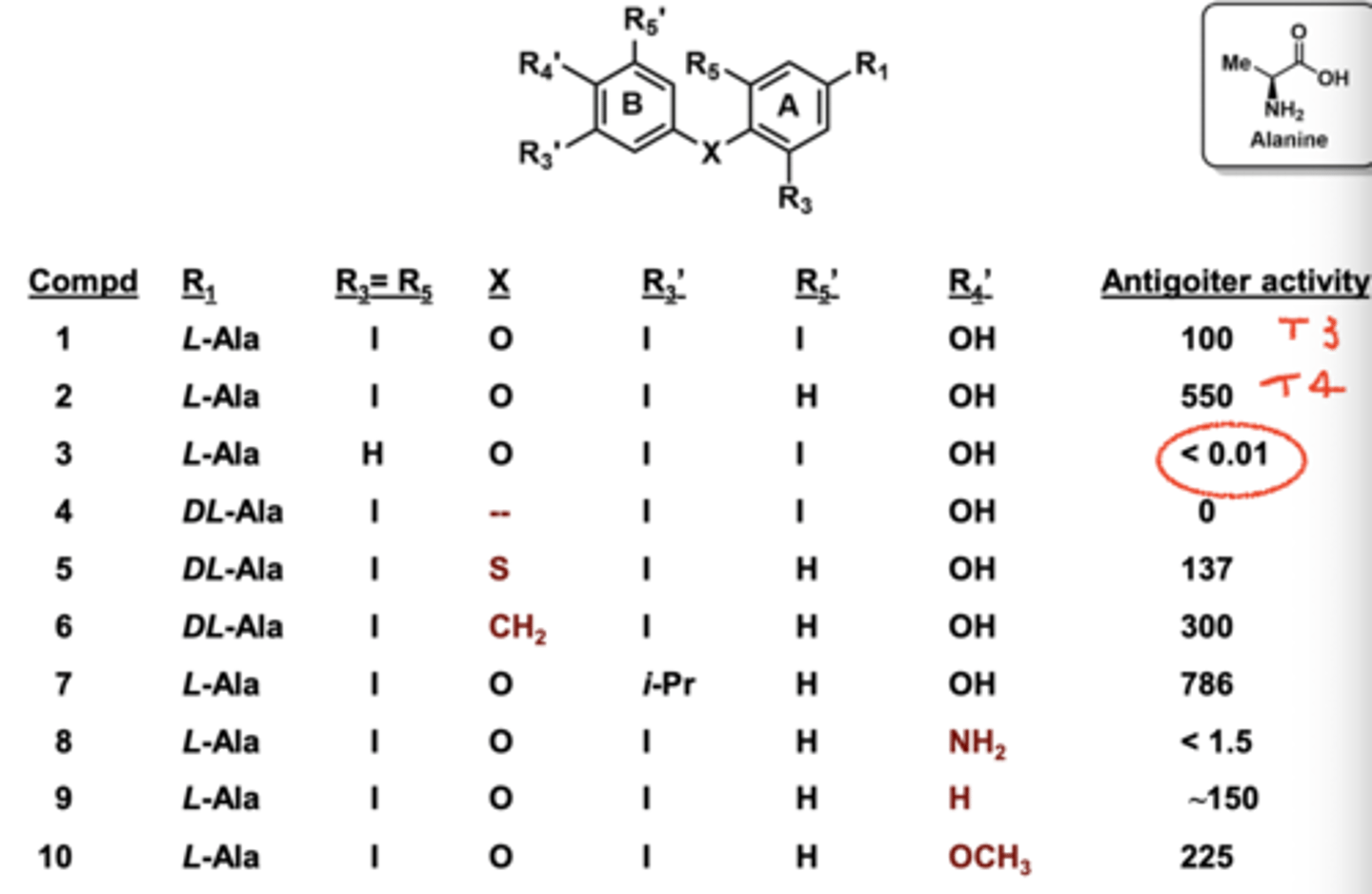
What happens if the R3 and R5 Iodines are replaced with hydrogen?
Complete loss of activity
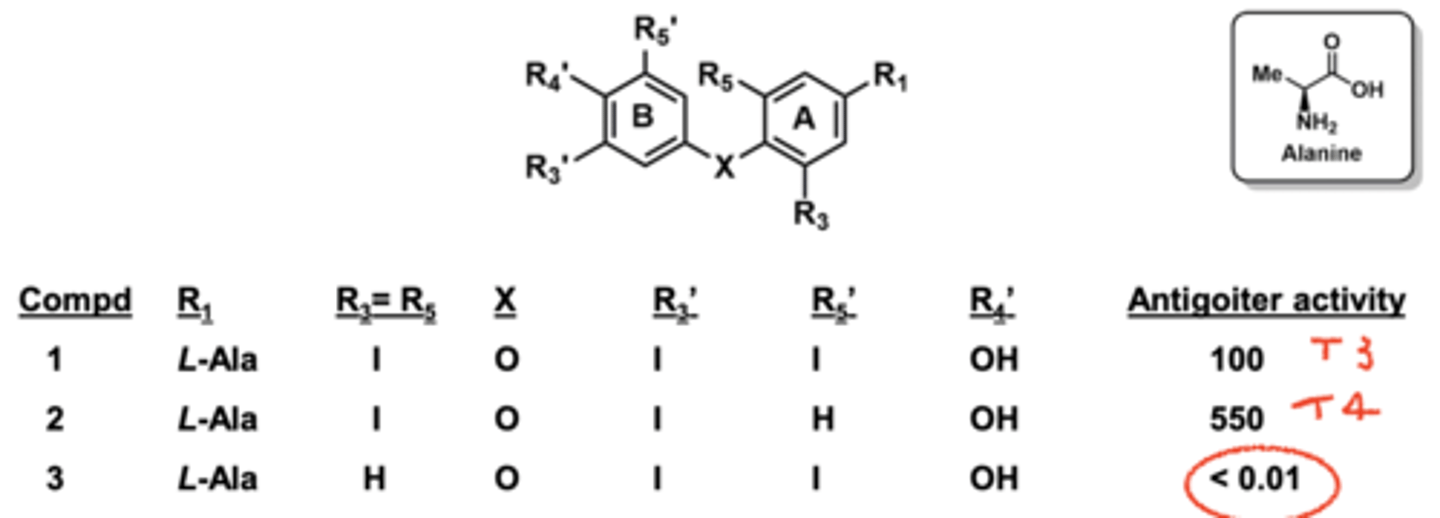
Why not use the structure of i-Pr if it had the highest activity?
Because it had poor pharmacokinetics
What R5 position causes weak binding affinity
Iodine (H is better)
5'-Deiodinase vs 5-Deiodinase
5' produces T3
5 produces rT3
Thionamides (propylthiouracil) structure
pharmacophore
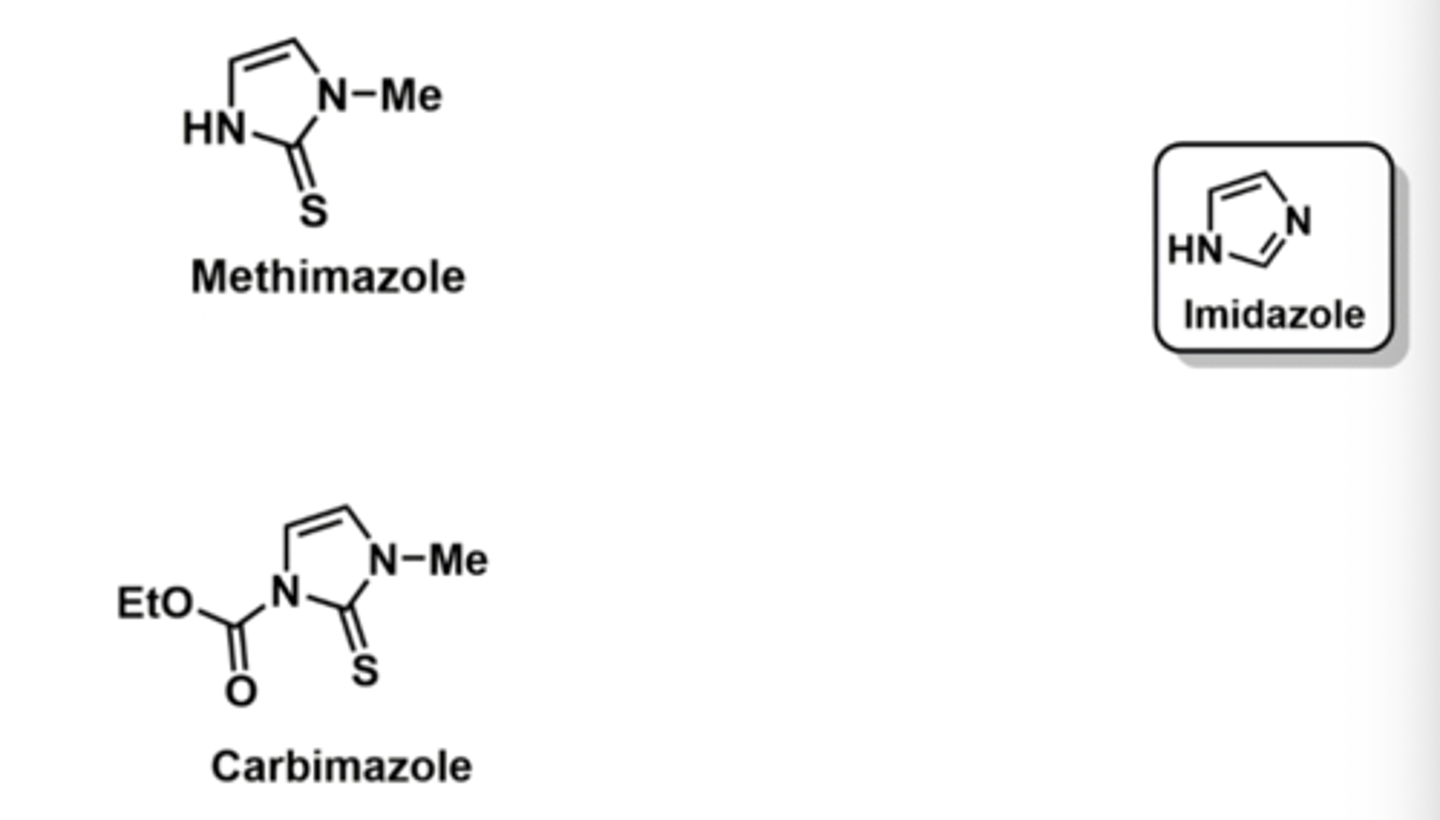
Methimazole vs carbimazole
- Methimazole is derived from imidazole
- Inhibits TPO
- Route of adm: Oral
- Used to treat hyperthyroidism
carbimazole is the prodrug so methimazole is the active form
Hypothyroidism symptoms
Weakness, fatigue, lethargy, tiredness
Cold intolerance
Headache
Loss of taste/smell
Hoarseness
No sweating
Modest weight gain
Muscle cramps, aches, pains
Dyspnea
Slow speech
Constipation
Menorrhagia
Galactorrhea
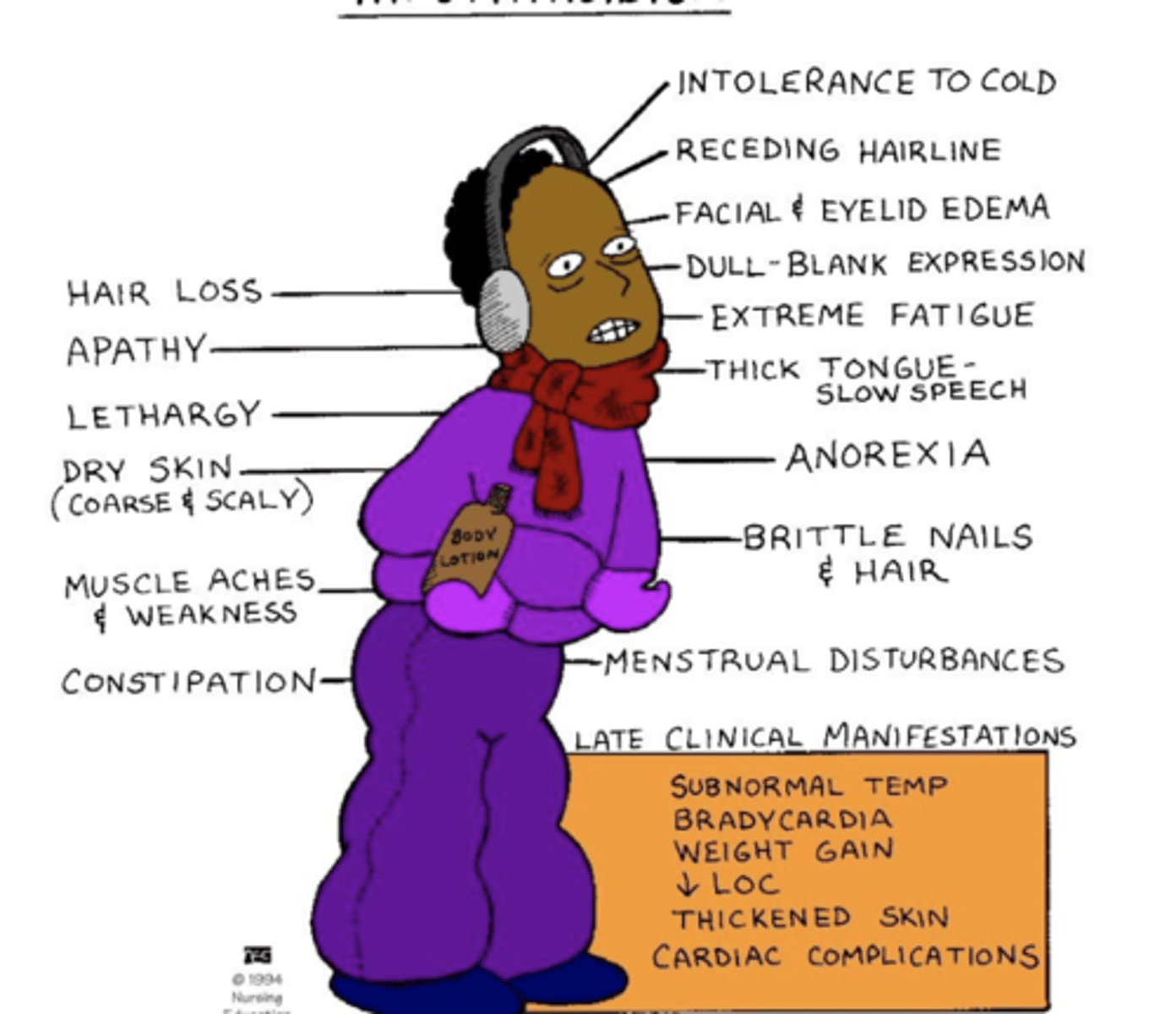
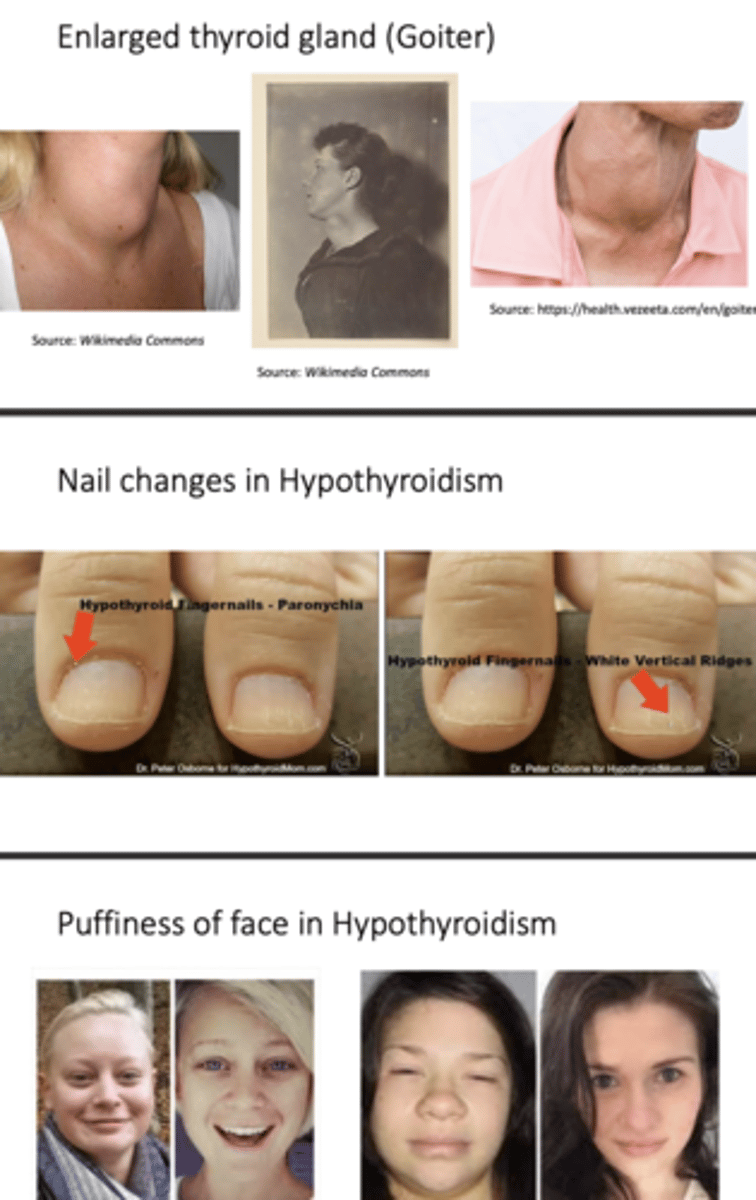
Hypothyroidism physical manifestations
Thin brittle nails
Thinning of skin
Pallor
Puffiness of face, eyelids
Thinning of outer eyebrows
Thickening of tongue
Peripheral edema
Pleural/peritoneal/pericaridal effusions
Decreased deep tendon reflexes
Myxedema heart
Bradycardia
Hypertension
Goiter
Hypothyroidism: Prevalence and types
• Prevalence of 1.4 to 2% in women and 0.1 to 0.2% in men
• higher in those over 60 (6% in women and 2.5% in men)
Primary hypothyroidism
• problem with thyroid gland (thyroid destruction or thyroid deficiency)
Secondary hypothyroidism
• problem with hypothalamus or pituitary
• TSH or TRH deficiency
How is hypothyroidism diagnosed
Diagnosed by laboratory testing plus symptoms
• TSH level
- Main indicator of thyroid function
- If high, suggests possible hypothyroidism
- Generally sufficient to diagnose primary hypothyroidism, but FT4 often measured as well
- If low, need free T4 to distinguish between primary hyperthyroidism and secondary hypothyroidism
• Autoantibody titers
• Helpful to determine etiology