control of blood water potential
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
describe how urea is removed from the blood
hydrostatic pressure causes ultrafiltration at renal capsule through basement membrane enabled by small size urea molecule
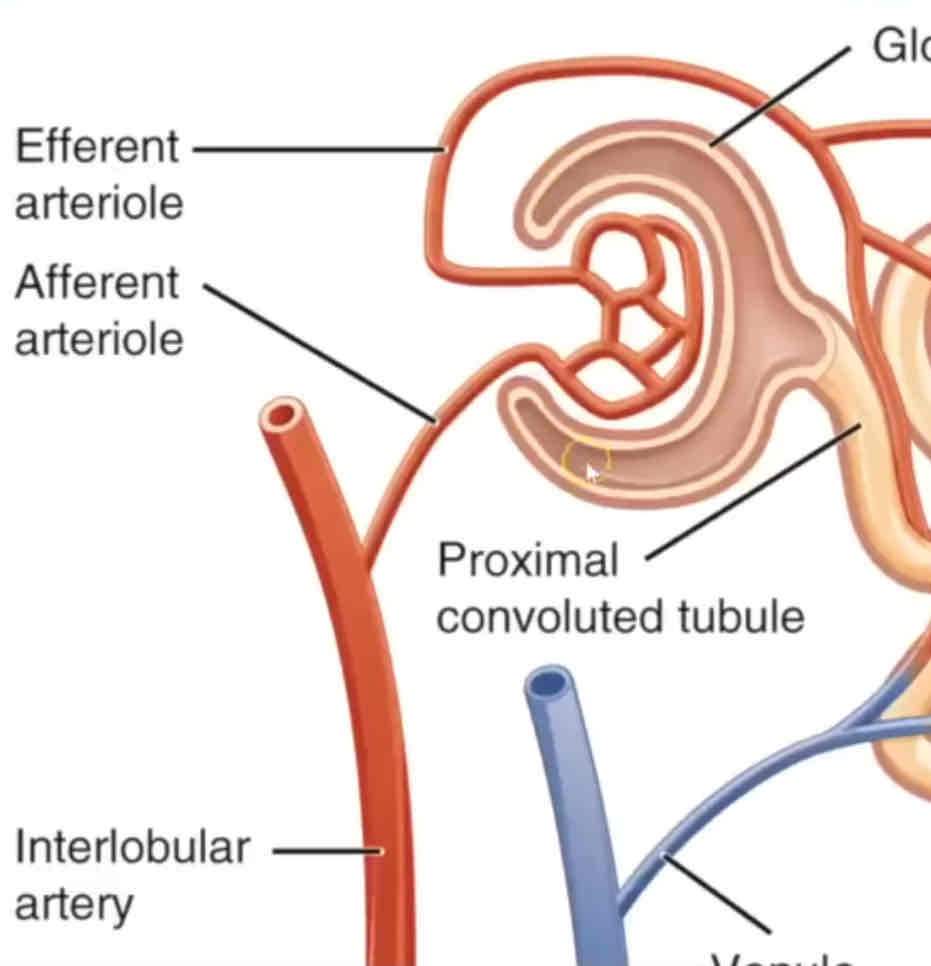
describe and explain what happens in ultrafiltraton
afferent arteriole narrows into efferent arteriole which increases hydrostatic pressure
causing ultrafiltration of small molecules: e.g. H2O, glucose and mineral ions are forced out through basement membrane into filtrate
filtrate passes out - through spaces between Podocytes and glomerular capillaries
RBCs and larger proteins can’t - too large so stay in the blood
glomerular filtrate
water, glucose, urea, fatty acids, etc. will be present
blood cells, platelets and proteins are not normally present in the filtrate
stages of osmoregulation
formation of glomerular filtrate at the Bowmans Capsule
reabsorption of glucose and water by the PCT
maintenance of gradient of Na+ by the loop of Henle (water reabsorption)
reabsorption of remaining water by the DCT and collecting ducts (role of ADH)
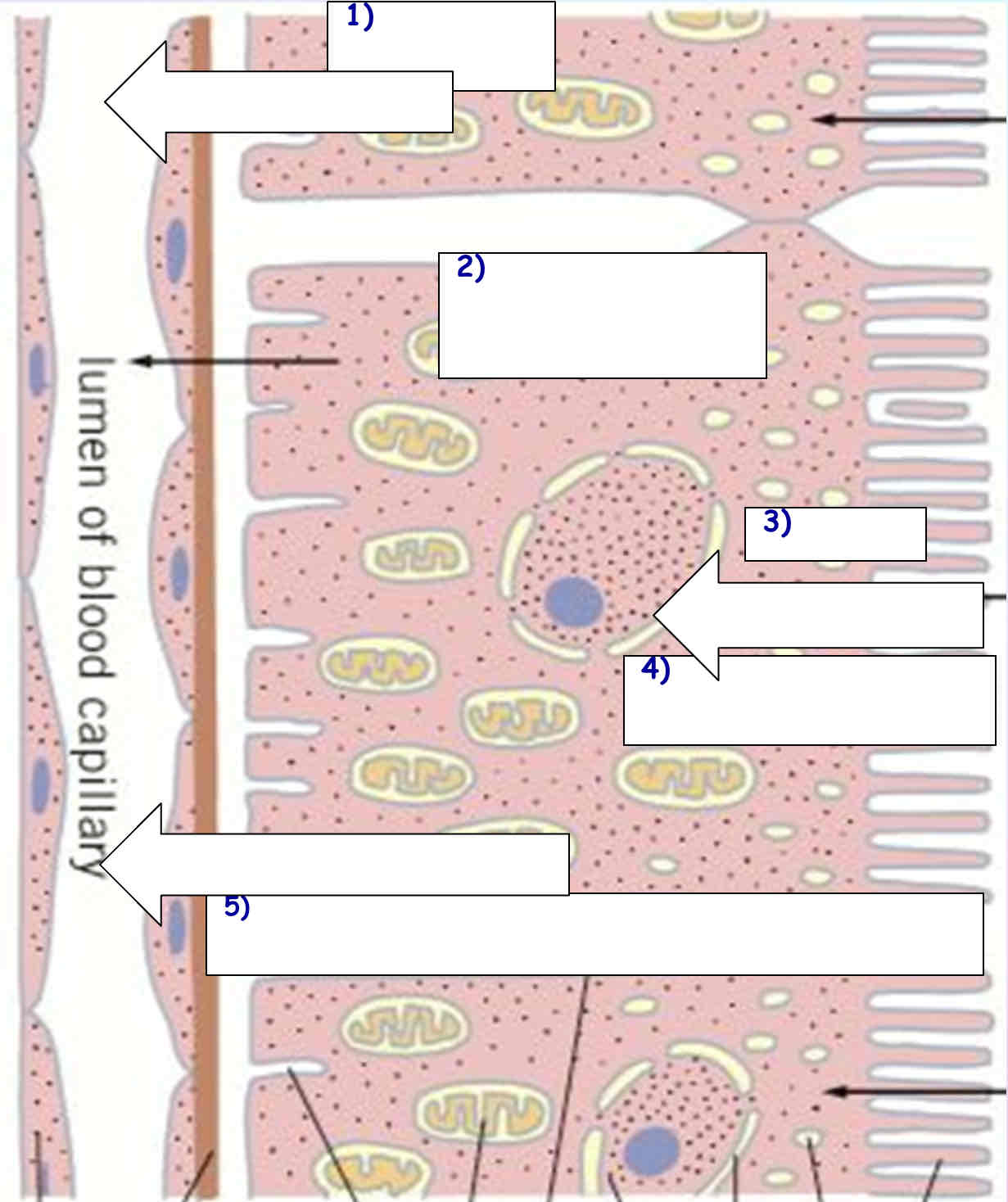
proximal convoluted tubule - reabsorption of glucose and water
1. Na+ actively transported out of cells lining proximal convoluted tubule into blood capillaries
2. this decreases the Na+ concentration in these cells
3. Na+ from lumen of proximal convoluted tubule enter down their concentration gradient through different co-transporter proteins, each bringing other molecules through, e.g. glucose, amino acids, chloride ions
4. these molecules then diffuse into the blood via facilitated diffusion, microvilli increase SA
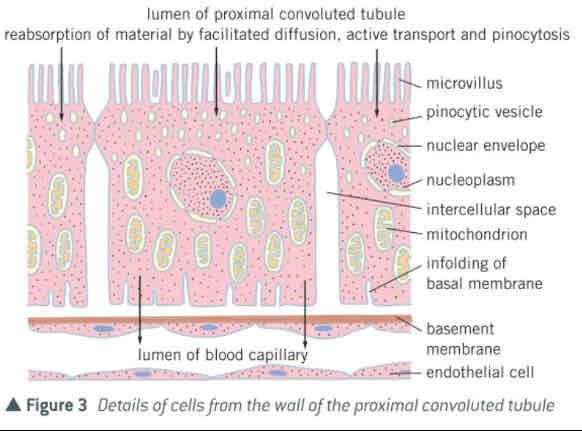
how is the proximal convoluted tubule adapted?
by having cells that have:
- microvilli - large SA to reabsorb substances from filtrate
- carrier proteins in membrane for active transport
- mitochondria - high density to provide ATP for active transport
describe the processes involved in the absorption of the products of polypeptide digestion
amino acids are absorbed down their conc gradient from the lumen into the blood by facilitated diffusion
Na+ removed from epithelial cell by active transport using the sodium-potassium pump into blood
maintains low conc of Na+ in epithelial cell (maintaining Na+ conc gradient between lumen and epithelial cell)
amino acid moves into epithelial cell with Na+ via carrier protein in co-transport
amino acid then moves into blood by facilitated diffusion
explain how a lack of insulin affects reabsorption of glucose in the kidneys of a person who does not secrete insulin
1. high concentration of glucose in blood
2. high concentration in filtrate
3. reabsorbed by facilitated diffusion
4. requires carriers
5. these are working at maximum rate
6. not all glucose is reabsorbed
explain how urea is concentrated in the filtrate
reabsorption of water by osmosis
at the proximal convoluted tubule
at the distal convoluted tubule
active transport of ions creates gradient
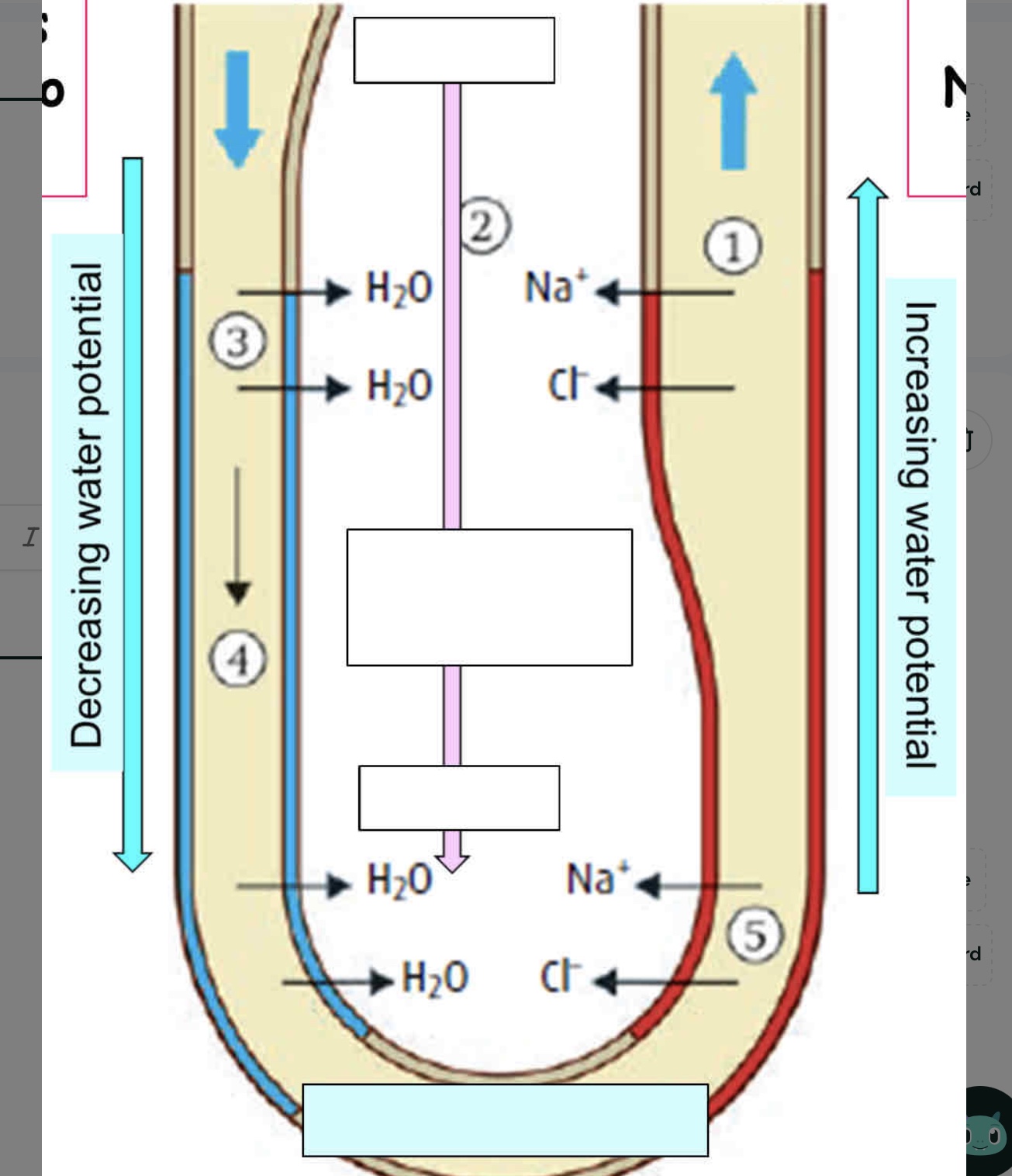
the loop of Henle
descending limb: narrow, thin walls and very permeable to water
ascending limb: wide, thick walls, not permeable to water and more permeable to salts, e.g. Na+
function:
- creates a high concentration of Na+ and chloride ions in the tissue fluid of the medulla
- this allows water to be reabsorbed from the contents of the nephron as the pass through collecting duct
survival advantage:
- very concentrated urine can be produced
- conserves water and prevents dehydration
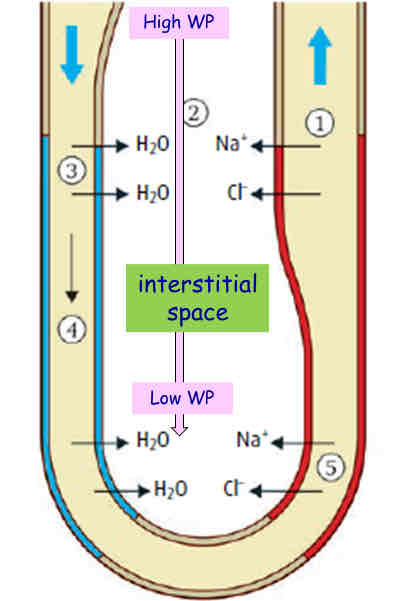
explain the role of the loop of Henle in the absorption of water from the filtrate
1. Na+ and Cl- are actively transported out of ascending limb
2. this decreases water potential in tissue fluid (interstitial region)
3. water can’t leave ascending limb (it’s impermeable to water)
4. water can leave filtrate in the descending limb by osmosis into interstitial space
5. water absorbed into blood capillaries by osmosis
6. water leaves collecting duct
7. (add from notes)
interstitial space
highest water potential (at top) by cortex
counter-current system
solute conc at any part of the ascending tubule is lower than that in the descending limb
causes a build up of salt conc in the surrounding tissues
water moves out by osmosis
counter current multiplier
- active transport of Na+ and Cl- in the epithelial cells of ascending loop of Henle (out of the filtrate and into the surrounding tissue)
- Na+ and Cl- transported against conc gradient
- this creates and maintains a wp gradient, so water moves out of the collecting duct by osmosis
- the water can then be reabsorbed back into the blood
explain how the loop of Henle maintains the gradient of ions which allows water to be absorbed from filtrate in the collecting duct
epithelial cell of tubule cells carry out active transport
transport Na+ out of filtrate against conc gradient into tissue fluid
maintains wp gradient for water reabsorption
countercurrent multiplier
collecting duct
the last chance to reabsorb the water
here the amount of water reabsorbed in to the blood can be controlled
the duct then flows into the renal pelvis, down the ureter and into the bladder
anti-diuretic hormone
- if dehydrated the wp of blood decreases and gets too low
- detected by osmoreceptors in the hypothalamus
- water moves from osmoreceptor into blood by osmosis (osmoreceptor decrease in volume)
- causes posterior pituitary gland to secrete more ADH
role of ADH:
- ADH is passed in the blood to the kidneys, where it binds to a cell surface receptor
- this activates phosphorylase
- phosphorylase causes vesicles containing aquaporins (water channel proteins) to bind with cell surface membrane of collecting duct
- increases the permeability of membrane to water and therefore allows more water to be reabsorbed
- when wp too high, less ADH released meaning fewer aquaporins are fused with the cell membrane
blood water potential too high
how:
- drink lots of water
- insufficient ions
what happens:
- detected by osmoreceptors in the hypothalamus
- less ADH secreted from posterior pituitary gland
- decreases permeability of collecting duct and distal convoluted tubule to water and urea
- more water leaves the body (less is reabsorbed back into the blood - dilute urine)
- osmoregulation → normal blood wp
blood water potential too low
how:
- don’t drink enough water
- sweat too much
- take in lots of ions, e.g. NaCl
what happens:
- detected by osmoreceptors in the hypothalamus
- more ADH secreted from posterior pituitary gland
- increases water permeability of collecting duct and distal convoluted tubule (inserts aquaporins)
- less water leaves the body, more is reabsorbed back into the blood
- increase collecting duct permeability to urea, urea leaves, decreases wp around duct, water leaves duct
- osmoregulation → normal blood wp
why does the cell volume of an osmoreceptor decrease when a person is dehydrated?
wp of blood will decrease
water moves from osmoreceptor into blood by osmosis
how does the secretion of ADH affect urine produced by the kidneys
permeability of membrane to water is increased
more water absorbed from collecting duct permeability to
smaller volume of urine
urine becomes more concentrated
how does ADH increase the movement of water from the lumen of the collecting duct into the blood?
ADH causes vesicles containing aquaporins to be inserted into membrane
water enters cell through aquaporins by osmosis down a wp gradient from cell to capillary via interstitial fluid
which hormone causes the decrease in the water content in the distal convoluted tubule?
ADH
explain how the structure of protein molecules allows them to form channels through which only water molecules can pass
each protein has a specific tertiary structure which gives a specific shape to inside of channel
explain how the cells of the collecting duct are able to absorb water from the filtrate through the protein channels in their plasma membrane
more negative wp inside tubule cells
water enters by osmosis
distal convoluted tubule
in the distal convoluted tubule Na+ are actively pumped out of nephron into blood
reabsorption of water from the collecting duct
tissue fluid deep in the medulla as a very low wp
water moves down the collecting duct and the wp gradient decreases further into the medulla
water enters the blood by osmosis and is conserved