6/7/8- MHC and Antigens
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
Major histocompatibility complex (also known as HLA)
•Tightly linked cluster of 40-50 genes on chromosome 6 that encode a number of proteins
•Organised into regions that encode different classes of molecules (1-3)
•Associated with recognition of antigens and self/non-self recognition
•Play a role in transplantation acceptance
Naming the molecules
•HLA-A, HLA-B and HLA-C encode for MHC class 1
•HLA-G encodes for a non-classical type 1 molecule that protects the foetus
•HLA-DP, HLA-DQ and HLA-DR encode for class 2
•Class 3 not directly involved in antigen presentation- encode for serum proteins, complement proteins cytokines e.g. tumor necrosis factor
Two key properties of MHC
•Polygeneic- several genes within each class, each person posesses a different range of MHC molecules with different properties
•Polymorphic- multiple variants of each gene, different alleles within population, molecules have a broad specificity
•Every cell in the individual expresses the same set of MHC molecules
Functions of MHC
•Encode for cell surface glycoproteins, play a role in antigen presentation and T cell activation
•Class 1 presents on all nucleated cells
•Class 2 presents only on antigen presenting cells (B cells, macrophages, dendritic cells)
•Will result in killing of virally infected cell (cytotoxic), macrophage activation to kill bacteria (helper), B cell production of antibody (helper)
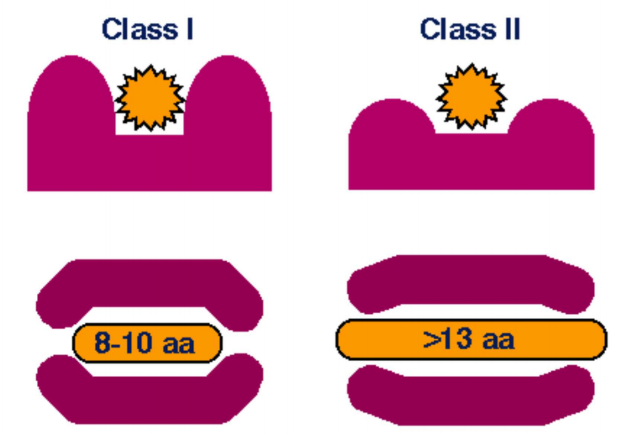
MHC class 1 structure
•Necessary for activation of cytotoxic T cells
•Heavy alpha chain with 3 domains- a1, a2, a3
•Light B2 microglobulin associated chain
•Antigenic peptides between 8-10 amino acids bind to the a1 and a1 domains

Class 2 structure
•Present antigens to helper T cells
•Two polypeptide chains- alpha and beta
•Peptide groove created within a1 and B1 domains
•Bind antigenic peptide of >13 amino acids
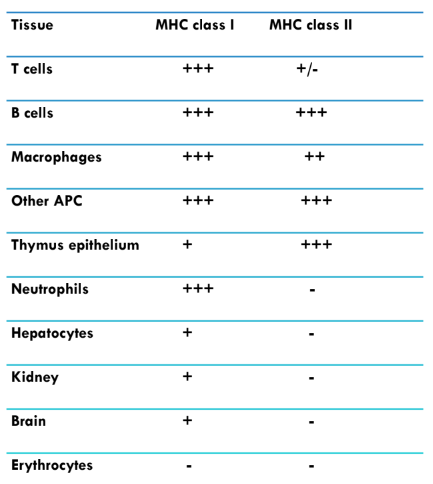
Expression of MHC molecules on cells
Anchoring of peptides within groove
•Class 1- peptide is bound (encased) at both ends to specific anchor residues, presents internal peptides e.g. derived from viruses
•Class 2- ends of peptide are unbound, side chains of peptide interact with anchor residues found in pockets along MHC molecule, presents external peptides e.g. derived from bacteria
MHC class 3 genes
• Encode soluble serum proteins, some complement proteins
• Tumour necrosis factor a and B
• Not involved in activation of T cells or transplatation
MHC gene diversity
• Individual alleles vary in their ability to present antigens from particular infections, may lead to more or less favorable outcome e.g. HIV
• Heterozygote advantage- individuals heterozygous for MHC alleles are more likely to have protective alleles
• Rare allele advantage- new infection may evolve to evade MHC alleles prevalent in a population, those with rare alleles are more likely to survive
• Diversity causes problems in transplantation- donor and recipient need to be as similar as possible
Where can antigens come from and what is an epitope
• Bacteria, infected cells, pollen
• Region on an antigen that triggers response in B or T lymphocytes
Immunogenicity vs antigenicity
• Immunogenicity- ability to induce B or T cell response
• Antigenicity- ability to combine specifically with the products of a B or T cell response e.g. antibodies or cell surface receptors
Four factors that determine immunogenicity
• Foreignness- any molecule that immature lymphocytes are not exposed to during development is later recognised as foreign
• Molecular size- best immunogens have size approaching 100k daltons, poor less than 10k
• Chemical composition- homopolymers tend to lack immunogenicity regardless of size, copolymers (different units) of sufficient size are immunogenic,also enhanced by aromatic amino acids
• Ability of immunogen to be processed and presented by an MHC molecule- large insoluble macromolecules are more immunogenic than small soluble ones are they are easier to phagocytose and process
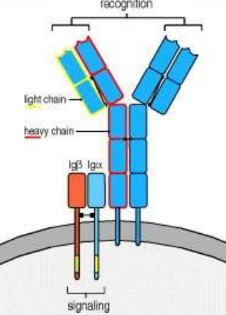
B cell receptors
• Membrane bound immunoglobulin binds antigen but cannot generate signal
• Iga and IgB are transmembrane antigen associated nonspecific signalling molecules
• Each have single immunoreceptor tyrosine based activation motif (ITAM) in cytosolic tails
• Activate immune response by cell signalling after ligand binds to antibody
T cell receptors
• T cell receptors are made from an alpha beta heterodimer
• Antigens are presented to T cells by MHC molecules, whole complex binds to receptors, cannot initiate signalling
• Cell also contains associated CD3 complexes made up of polypeptides
• Acitvate T cells after ligans binds to receptor

Clonal selection theory
• Aims to explain diversity of antibodies formed during the initiation of the immune response
• States that in a pre-existing group of lymphocytes a specific antigen activates only its antigen specific cell to multiply and produce identical clones
• Lymphocytes circulate in blood and lymph and await their specific antigen
• Only recognise epitope that fits receptor, activation occurs in secondary lymphoid organs
• Once activated, produce clones with same epitopes
Immature lymphocytes
• Have not encountered antigen and lack fully developed antigen specific receptors
• Found in primary lymphoid organs
Naive lymphocytes
• Fully developed antigen receptors but have not encountered antigen
• Found in secondary lymphoid organs
• As they move around they interact with many dendritic cells and stop when the encounter antigen for which they express specific receptors
• This activation induces several responses in T cells- cytokine secretion, proliferation (clonal expansion), differenciation into effector and memory lymphocytes
Effector cells
• Activated helper and cytotoxic T cells, antibody secreting B cells
• Recognise antigens in lymphoid organs or peripheral non-lymphoid tissues and are activated to perform specific functions to eliminate microbes and prevent tissue damage
• CD4+ effector cells activate macrophages, B cells, inflammatory response
• CD8+ cells activate macrophages, kill infected cells
Memory lymphocytes
• Progeny of activated lymphocytes responsible for rapid secondary response if antigen is encountered again, will generate new effector cells
• Present in lymph circulation and are abundant in mucosal tissue, skin and lymphoid organs
• T cell response declines (apoptosis) after antigen is eliminated by effector cells to maintain state of equilibrium and homeostasis
Adjuvants
• Substances that enhance the immunogenicuty of an antigen when mixed with it and injected during vaccination
• Prolong antigen persistance at certain sites
• Result in increase in local inflammation and granuloma formation- dense, macrophage rich mass of cells
• Stimulate lymphocyte production non-specifically
Superantigens
• Class of antigens that results in excessive activation of the immune system by polyclonal T cell activation and massive cytokine release
• Do not bind to TCR but common structures on T cells (non-specific)
• Present on bacteria e.g. staphylococcal enterotoxins (SEs) and toxic shock syndrome toxin 1
• One in five T cells can be activated by superantigen which can lead to shock and death
Types and function of antigen presenting cells
• Process and present antigen to T cells to activate them
• Include dendritic cells, macrophages and B cells
• Capture the antigens and transport them to secondary lymphoid organs
• Provide primary signal- TCR binds to antigen-MHC complex
• Secondary signal- co-stimulatory molecules bind to receptors like CD28 on the T cell, required for activation
Antigen processing and presentation for extracellular antigens
• Derived from bacteria, foreign cells, toxins
• Usually dendritic cells detect entry of those materials and phagosytose them and package into vesicles
•Vesicles fuse with lysosomes to form phagolysosomes which fuses with vesicle containing MHC class 2 molecule
• Phagolysosome degraded by enzymes into peptides that fuse with the binding groove of MHC2
• This comples is transported to cell surface for display and is recognised by CD4+ cells (helper)
Antigen presentation pathway for intracellular antigens
• Pathogens e.g. viruses enter cell, cytoplasmic peptides derived from virus are tagged by the cell with a small molecule called ubiquitin
• The ubiquitin is recognised by the proteasome which digests the viral proteins into smaller peptides
• These are then transported to the endoplasmic reticulum by TAP (transporter associated with antigen processing) where they bind to MHC1 molecules
• This complex is displayed on the cell surface and recognised by CD8+ cells (cytotoxic)