Topic 1: Autonomic Nervous System
1/137
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
138 Terms
what processes does the ANS regulate:
SM contraction/relaxation
all exocrine + some endocrine secretions
heart rate
intermediary metabolism
what is the relationship between sympathetic and parasympathetic nervous systems and which predominates in what states?
opposing actions in some physiological systems
sympathetic NS activity increases in stress (flight/fight)
parasympathetic NS activity predoms during satiation and repose
What neurons are involved in ANS structure and what arrangment is it?
2 neurons arranged in series:
preganglionic
postganglionic
What is the anatomy of sympathetic and presympathetic neurons
sympathetic = SHORT pregang + LONG postgang neurons
parasympathetic = LONG PREgang + SHORT POSTgang
which neuronal cell bodies are located in the lateral horn of grey matter of thoracic and lumbar segments of the spinal cord
sympathetic preganglionic neurons
what is the arrangment of sympathetic neurons in the body
preganglionic neuronal cell bodies are located in lateral horn of grey matter of Thoracic and Lumbar segments of spinal cord
these connect to the prevertebral chain of sympathetic ganglia (contain cell bodies of postganglionic neurons)
postganglionic fibres reach peripheral destinations via branches of spinal nerves
fibres for pelvic and abdominal sites have cell bodies in prevertebral ganglia in abdominal cavity
What is the exception to the two neuron arrangment in the sympathetic NS
Adrenal medulla: innervation of adrenal medulla which releases catecholamines when stimulated and considered to be modified postgang sympathetic neuron
Adrenal Medulla: Modified postganglionic sympathetic neuron that releases catecholamines (epinephrine and norepinephrine) into the bloodstream.
what two outflows do parasympathetic preganglion neurons exit out of
cranial outflow originates in medullary region and innervates eye, lacrimal and salivary glands and organs in thoracic cavity
sacral outflow innervates pelvic and abdominal viscera via nerves called nervi erigentes
Where are most parasympathetic neurons located in?
in their target organs
What are the principal neurotransmitters?
Acetylcholine and Noradrenaline
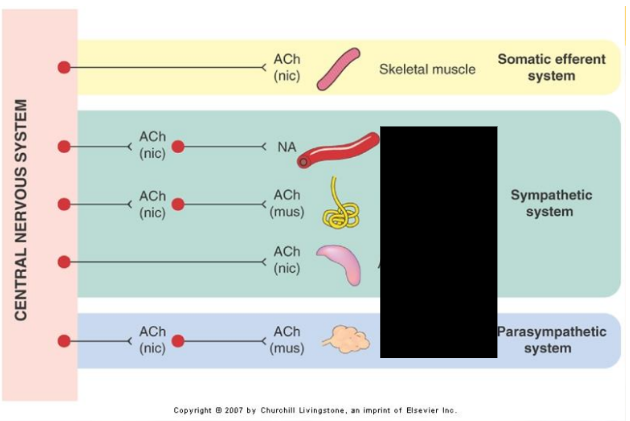
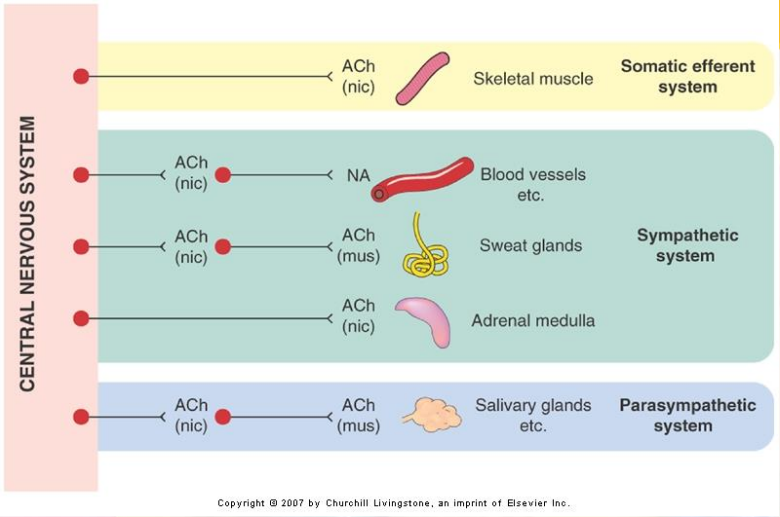
Preganglionic neurons are _______, and release ____ to act on ______ receptors
cholinergic (use ACh as primary transmitter)
acetylcholine
nicotinic
postganglionic parasympathetic neurons release _____ to act on ______ receptors
acetylcholine
muscarinic
postganglionic sympathetic neurons release _____ to act on __________ receptors
noradrenaline
alpha and beta adrenoreceptors
exceptionally, sympathetic neurons innervating ________, release _____ on _______ receptors instead
sweat glands
acetylcholine
muscarinic
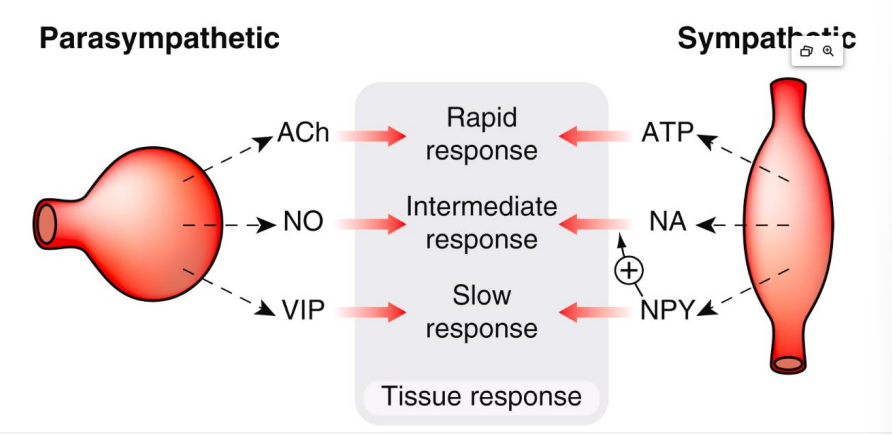
Can ANS receptors release more than 1 transmitter or modulator?
Yes, called cotransmission
What other neurotransmitters/modulators can ANS neurons cotransmit?
ATP, NO, VIP (Vasoactive Intestinal Polypeptide)
Do neurotransmitters/modulators act/are released the same or at the same time?
no there are different timeframes for action and different release patterns according to impulse patterns
Where are nicotinic receptors located?
located in:
autonomic ganglia
neuromuscular junction
adrenal medulla
CNS
receptors located in the: autonomic ganglia, neuromuscular junction, adrenal medulla, CNS are…?
nicotinic receptors
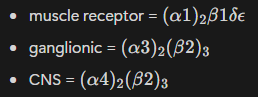
what are the three main nicotinic receptor subclasses?
CNS
muscle
ganglionic
what time of receptors are nicotinic receptors?
ligand gated ion channels with similar molecular structure but behave differently pharmacologically
What is the mechanism of nicotinic receptors?
nicotinic receptors are coupled to cation channels and mediate fast excitatory synaptic transmission
Binding of ACh opens cation channels, allowing Na+ and K+ to flow, causing rapid excitation.
How many nicotinic receptor subtypes are there and what structure are they?
Five subunits forming receptor-channel complex in pentameric structures
α, Β, γ, δ, ε
Where are muscarinic receptors located?
Located in:
SM
cardiac muscle
glands in periphery
CNS (motor control, memory)
receptors located in the: SM, cardiac muscle, glands in periphery, CNS (motor control, memory) are…?
muscarinic receptors
What type of receptors are muscarinic receptors?
G-protein coupled receptors
What is the mechanism of muscarinic receptors?
cause activation of phospholipase C, inhibition of adenylyl cyclase, activation of K+- channels or inhibition of Ca2+
Binding of ACh activates intracellular signaling pathways (e.g., activating phospholipase C, inhibiting adenylyl cyclase, or affecting ion channels).
What two components make up Acetylcholine?
Choline and Acetyl from Acetyl-CoA
How is ACh synthesised then released?
choline taken up into nerve terminal via membrane transporter
free choline is acetylated by cytosolic enzyme Choline Acetyltransferase (CAT) which transfers acetyl group from acetyl-CoA
ACh is pumpted from cytosol via transport proteins and packaged into synaptic vesicles
ACh is released via exocytosis which is triggered by Ca2+ entry into nerve terminal
ACh diffuses across synaptic cleft to combine with receptors on postsynaptic membrane
What happens to ACh after being released
some released ACh is hydrolysed by acetylcholinesterases bound to BM of nerve termine
others bind to receptors for ~2ms and then dissociate and is rapidly hydrolysed to prevent binding to another receptor
then recycled
What is the concentration of choline in the plasma vs near the nerve terminal?
in plasma = 10µM
near nerve terminal = 1mM
How can drugs affect ACh release?
inhibit synthesis:
hemicholinium - blocks choline carrier
inhibit storage:
venomous red back spider - disrupts synaptic vesicles and depletes nerve endings of ACh
Compete with Ca2+ entry:
Mg2+ ions, aminoglycosides
Block active transport of ACh into vesicles:
vesamicol
Inhibit ACh release:
botulinum toxin from Clostridium botulinum (anaerobic bacteria) - cleaves proteins involved in exocytosis in nerve membrane progressive parasympathetic and motor paralysis
dry mouth, blurred vision, difficulty swallowing, respiratory paralysis
What drug can inhibit ACh synthesis?
hemicholinium - blocks choline carrier
What drug can inhibit ACh storage?
venomous red back spider - disrupts synaptic vesicles and depletes nerve endings of ACh
What drug competes with Ca2+ entry into nerve terminal?
Mg2+ ions and aminoglycosides
what drug blocks the active transport of ACh into vesicles?
vesamicol
what drug inhibits ACh release?
botulinum toxin from Clostridium botulinum - cleaves proteins involved in exocytosis in nerve membrane progressive parasympathetic and motor paralysis
What are the uses of botulinum toxin A?
skeletal muscle spasm, overactive bladder
what does botulinum toxin A cause?
causes flaccid paralysis of skeletal muscle
diminished activity of parasympathetic and sympathetic cholinergic nerves
How long does inhibition last for and what side effect may occur from botulinum toxin A?
lasts several weeks to 3-4 months
immunoresistance may occur
what drugs are parasympathomimetic drugs?
muscarinic receptor AGONISTS
Drugs that mimic the effects of ACh at muscarinic receptors.
What chemical groups do muscarinic receptor agonists have?
quarternary ammonium group (+ve charge)
ester group (partial -ve charge)
What organs do muscarinic receptor agonists affect?
eye
exocrine glands
cardiovascular
smooth muscle
there are central effects as well
how do muscarinic receptor agonists affect the eye?
cause contraction of:
constrictor pupillae (pupil constriction)
ciliary muscle (accomodation for near vision)
how do muscarinic receptor agonists affect the exocrine glands?
stimulation of exocrine glands w increases in sweating, lacrimation, salivation and bronchial secretions
stimulate HCl prod in stomach
how do muscarinic receptor agonists affect the cardiovascular system?
cardiac slowing (negative chonotropic effect, M2)
decreased CO
reduced force of contraction (negative inotropic effect)
vasodilation (NO mediated effect, M3)
how do muscarinic receptor agonists affect smooth muscle?
contraction of SM in:
Lung (bronchoconstriction)
GI tract (increased peristalsis)
bladder (during micturition)
what central effects do muscarinic receptor agonists have?
tremor
hypothermia
increased locomotor activity
improved cognition
what drugs cause side effects such as:
abdominal discomfort - vomiting, diarrhoea, intestinal cramps
bradycardia, hypotension, flushing
salivation, sweating
tremor, improved cognition
muscarinic receptor agonists
what drug interations do muscarinic receptor agonists have?
other muscarinic agonists
anticholinesterase medications
ganglion blocking drugs
What are some contraindications for muscarinic receptor agonists?
hypersensitivity, parkinsons disease, asthma, epilepsy, vagotonia, hypotension, severe bradycardia
coronary artery disease
GI obstruction
urinary obstruction
hyperthyroidism
peptic ulcer
what two cholinesterases are there
acetylcholinesterases
butyrylcholinesterases
Acetylcholinesterases are _____ cholinesterases and butyrylcholinesterases are ______
true
pseudocholinesterase
where are acetylcholinesterases found/located?
located in BM of synaptic cleft
found in cholinergic nerve terminals and RBCs
serine hydrolases have two distinct regions/sites. What are they>
anionic site (glutamade residue) - binds choline moiety
esteratic site (histidine and serine) - catalytic
where are acetylcholinesterases found/located?
found in tissues of liver, skin, brain and GI smooth muscle
plasma
which cholinesterase demonstrates narrow substrate specificity (primary ACh)
acetylcholinesterases
which cholinesterases exert broad substrate specificity
butyrylcholinesterases
What is a short acting anticholinesterase and how long does it last?
Edrophonium - 2 min duration
What is a medium duration anticholinesterase and how long does it last for?
Neostigmine and Physostigmine - 3 hour duration
What anticholinesterases are irreversible?
organophosphates
what are some examples of irreversible anticholinesterases?
nsecticides - parathion
therapeutic uses - ecothiopate
chemical warfare - sarin
common drug for poisons and suicide
What drug can reactivate cholinesterases?
Pralidoxime
How does pralidoxime reactivate cholinesterases ?
brings oxime grp close to phosphorylated esteratic site
attracts phophate grp from serine hydroxyl grp
What effects do anticholinesterases have in autonomic cholinergic synapses?
increased ACh @ nerve terminals
increased secretions
increased peristaltic activity
bronchoconstriction
bradycardia and hypotension
pupillary constriction
fixation of accommodation for near vision
decreased intraocular pressure
What are some clinical uses of anticholinesterases?
anaesthesia: neostigmine reverses effects of non-depolarising neuromuscular blocking drugs
glaucoma: ecothiopate
alzheimers: tacrine, donepezil, galantamine, rivastigmine
myasthenia gravis: neostigmine
What type of drugs can be used for anaesthesia, glaucoma, alzheimers and myasthenia gravis
anticholinesterases
What chemical groups are muscarinic receptor antagonists composed of?
ester and basic groups
tertiary ammonium compounds
quarternary ammonium compounds
what organs do muscarinic receptor antagonists affect?
exocrine secretions
heart rate
eye
GI tract
SM
CNS
What effect does muscarinic receptor antagonists have on exocrine secretions?
decreased secretions of salivary, lacrimal, bronchial, and sweat glands
What effect does muscarinic receptor antagonists have on heart rate
tachycardia
What effect does muscarinic receptor antagonists have on the eye
pupil dilation (mydriasis)
paralysis of accommodation (cycloplegia)
What effect does muscarinic receptor antagonists have on the GI tract
inhibition of GI motility
What effect does muscarinic receptor antagonists have on SM
relaxation of bronchial, biliary and urinary SM
What effect does muscarinic receptor antagonists have on CNS
antiemetic effects and treating motion sickness - hyoscine
reduce involuntary movement's in parkinson’s disease by inhibiting extrapyramidal system
reduced cognition/arousal
Muscarinic antagonists have clinical uses for:
sinus bradycardia
ophthalmic - dilate pupil
prevention of motion sickness
parkinsonism
asthma
anaesthetic premedication
GI endoscopy antispasmotic - IBS, colonic diverticular disease
Peptic ulcer - reduce acid secretion via M$_3$ receptors
What are some contraindications for muscarinic receptor antagonists?
hypersensitivity
myasthenia gravis
severe cardiac disease
GI obstructive disease
narrow-angle glaucoma
acute haemorrhage
prostatic hypertrophy
urinary retention
pyloric obstruction
ulcerative colitis
toxaemia
febrile condition
What is an example of ganglionic nicotinic receptor agonists?
dimethylphenylpiperazinium (DMPP) - no therapeutic value
nicotine is provided in (DMPP) - no therapeutic value
nicotine is provided in patches and gum for relief from cigarette smoking
What is an example of ganglionic nicotinic receptor antagonists/ganglion blocking drugs?
hexamethonium, nicotine (high doses)
What do ganglion blocking drugs/nicotinic receptor antagonists do?
interfere w ACh release
prolonged depolarisation causing desensitisation
Which neurons contain large dense cored vesicles:
Noradrenergic neurons
Where are noradrenergic neurons located:
heart
spleen
vas deferens
blood vessels
Noradrenergic transmission: The process by which ______is released from ______ neurons and acts on ________.
Norepinephrine/Noradrenaline
sympathetic
adrenoceptors
which neurons are postganglionic sympathetic neurons?
Noradrenergic Neurons
What are catecholamines?
Compounds with a catechol nucleus and an amine side group.
catecholamine examples?
noradrenaline (NA)
adrenaline (A)
Dopamine (DA)
Isoprenaline (ISO)
the metabolic precursor for noradrenaline and adrenaline is ______
L-tyrosine
L-tyrosine is the metabolic precursor for ______and ______
noradrenaline and adrenaline
NA is mostly stored in:
nerve terminals or chomaffin cells is contained in vesicles???
how do the cytoplasmic concentrations of NA remain low?
via transport mechanism in vesicular membranes
a transport mechanism in vesicular membranes ensures:
that cytoplasmic concentrations of NA remain low
Storage vesicles for NA also include/contain:
ATP (4 molecules per molecule of NA)
chromagranin A
increased cytoplasmic levels of ____ promotes the fusion and discharge of NA synaptic vesicles
calcium
Can NA regulate its own release? if so, then how?
Yes, through auto-inhibitory feedback mechanism which operates through alpha 2-adrenoreceptors which inhibit adenylyl cyclase and prevent opening of Ca2+ channels
Reuptake of NA by nerve terminals and other cells is responsible for:
The termination of NA transmission
The termination of NA transmission occurs via:
Reuptake of NA by nerve terminals and other cells
What 2 main mechanisms are responsible for reuptake of NA
neuronal (NET) and extraneuronal (EMT) transport systems.
What is the difference between neuronal (NET) and extraneuronal (EMT) reuptake?
Neuronal (NET): Reuptake into nerve terminals, then repackaged into vesicles or metabolized.
Extraneuronal (EMT): Uptake into non-neuronal cells (e.g., smooth muscle cells, cardiac muscle, endothelium), and metabolized by COMT.