Wk 11 - Hypo/Hyperthermia and DCI/Barotrauma
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
Define Hypothermia?
Accidental and unintentional drop in core body temperature below 35 degrees, which can be defined as mild, moderate and severe.
What are the methods of heat loss from the body?
- Convection
- Radiation
- Evaporation
- Conduction
- Respiration
What is convection as a method of heat loss?
Body heat is lost to surrounding air
What is radiation as a method of heat loss?
Body heat is lost to nearby objects without physically touching them
What is evaporation as a method of heat loss?
Body heat causes perspiration which is lost from the body surface when changed from liquid to vapour
What is conduction as a method of heat loss?
Body heat is lost to nearby objects through direct physical contact
What is the ideal body temperature?
36 - 37 degrees
What are methods of the body to increase its temperature?
- Increased muscle tone
- increased basal metabolic rate
- Vasoconstriction
- Behaviour (put on jacket, drink warm tea)
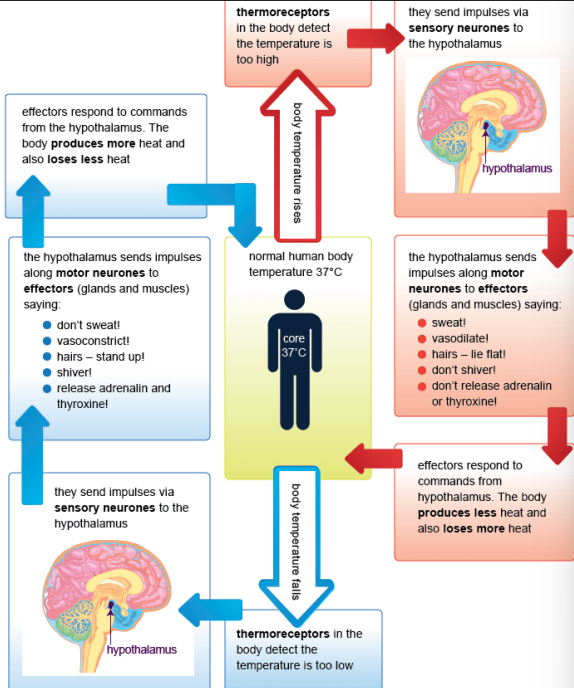
Temperature Regulation Diagram
How is heat loss different for paediatrics?
- Loose heat faster than adults
- Larger head-to-body ratio --> loose heat through head
- Less sufficient mechanisms of generating heat
- Infants cannot shiver
How is heat loss different for the elderly?
- Less likely to use heater --> money cost
- Reduced ability to generate body heat due to reduced mass
- Reduced ability to shiver
- Impaired mobility (can't get up to turn heater on etc.)
What are some specific conditions that can increase risk of hypothermia?
- Burns
- Spinal cord injury
- Stroke
- Diabetes
- Metabolic conditions
- Renal failure
- environmental exposure
- recreational activities (skiing, hiking etc.)
- entrapment
Which endocrine disorders can increase risk of hypothermia?
- Hypopituitarism
- Hypoadrenalism
- Hypothyroidism
How much heat loss does respiration account for?
10-30%
When would you be likely to see an Osbourne J wave on an ECG?
In patients with a body temperature of less than 24 degrees
What are the stages of hypothermia?
1. Normal - 36-37 degrees
2. Mild - 32-35 degrees
3. Moderate - 28-32 degrees
4. Severe - <28 degrees
How does the body decrease heat loss?
constriction of blood vessels in the skin
reduction in sweating
conscious behaviour such as putting on clothes, sheltering, etc
reduction of surface area by curling into a ball
How does the body increase heat production?
shivering
increase in voluntary activity
increased metabolic rate
What signs/symptoms would be present in mild hypothermia?
- Shivering (stops 32 degrees)
- Increased HR & RR
- Vasoconstriction (initial hypertension)
- Lethargy
- Ataxia
- Stiff joints
- Poor judgement
- Slurred speech
- Amnesia as temp drops more
- hyperglycemia due to decrease in insulin sensitivity and secretion
What signs/symptoms would be present in moderate hypothermia?
- Stopped shivering
- Pale
- Cyanosed lips/ears/nose
- Sleepy (stupor)
- Hard to obtain BP reading
- Cardiac arrhythmias
- Decreased HR, BP, RR
- eventually unconscious
- VF in bottom range
- Loss of muscle reflexes
What signs/symptoms may be present in severe hypothermia?
- Very low HR, BP, RR
- Acidosis (blood pH drop)
- Electrolyte imbalances
- Decreased cerebral blood flow
- Difficult to palpate pulse
- Non-reactive pupils
- cant spontaneously return to normal
- cerebral blood flow decreased by 66%
- hypotension
- pulmonary oedema
- osborn/j waves appear
- ventricular standstill, asystole at 18-20 degrees
- no response to pain at 26 degrees
What are other cold specific injuries?
- Frost bite
- Chilblains
- Trench foot
- Frost nip
What is frostbite?
When tissues freeze, affecting the peripheries (feet, toes, hands, fingers, ears, nose), and ice crystals form inside of the cells.
What is chilblains?
An abnormal vascular response characterised by itchy, red, painful, blistered skin.
What is trench foot?
Prolonged exposure to wet/cold environment causes flesh to become damaged
How to manage hypothermia?
- Remove patient from cold environment
- Remove wet clothing
- Provided warm drinks
- Protect against further heat loss
- Avoid rough handling
- Utilise heat blankets
- Provide fluid warming (if accessible)
- ECMO (HEMS)
How is a thermal wrap achieved?
Heat packs on neck, armpits & groin, wrap in foil & blanket
What are the considerations for a hypothermic cardiac arrest?
If the patient temperature is <30 degrees, double the interval for adrenaline (now every 8 minutes) and amiodarone
What is hyperthermia?
A rise in body temperature above the hypothalamic set point when heat-dissipating mechanisms are impaired or overwhelmed by external or internal heat production.
What are the 2 types of heat stroke?
1. Classic
2. External
What is classic hyperthermia?
Occurs during high environmental temperatures, often affecting elderly in a heat wave, for example.
What is external hyperthermia?
Occurs during strenuous physical activity in high environmental temperatures and/or high humidity. Usually affecting young, healthy adults.
What is malignant hyperthermia?
A pharmaco-genetic disorder, manifesting as a hyper-metabolic response, usually due to inhalation agents used for anaesthesia
What is Boyle's Law?
At a constant temperature, the volume of a given mass of gas varies inversely with the absolute pressure. When the pressure is doubled, the volume is halved.)
What is Dalton's Law?
In a mixture of gases, each constituent gas exerts a partial pressure in proportion to its percentage of the mixture. (At depth partial pressures of gas increase but the percentages of the gas remain the same.)
What is Henry's Law?
The amount of gas that dissolves in a liquid is proportional to the partial pressure of the gas in contact with the liquid. (More gas will be dissolved into a liquid at high pressure & less gas can be dissolved when the pressure is decreased.)
What is CAGE (Cerebral arterial gas embolus)
When micro-bubbles come out of a solution due to deep pressure being dissolved into the bloodstream from rapidly advancing to the surface, causing a gas embolism. This can travel into the pulmonary circulation and then into the brain
What is AGE (arterial gas embolus)?
Results from an embolus travelling the arteries and causing tissue to become damaged and blocks blood flow to smaller vessels.
What is decompression illness?
Results from bubbles growing in the tissue causing local damage, which can lead to a variety of symptoms from joint pain and swelling, to paralysis and even to death.
Signs/Symptoms of decompression illness?
- Fatigue
- Itchy skin
- pain in joints
- Dizziness
- Vertigo
- Numbness
- Tingling
- Paralysis
- Muscle weakness
- Confusion
- Unconsciousness
How long after diving can decompression illness occur?
Up to 24hrs later
Treatment for decompression illness
- Position patient supine or lateral
- Provide hi-flow O2
- Normal saline IV
- transport to a recompression facility (hyperbaric chamber --> Alfred hospital)
What is TXA (Tranexamic Acid)?
AKA Cyklokapron, TXA Lupin, APO-TXA
An anti-fibrinolytic/anti-haemorrhagic medication which inhibits the lysine-receptor in plasminogen, preventing activation of plasminogen into plasmin. Sythetic, competitive inhibitor.
How does TXA work?
It disrupts plasminogen being activated by plasmin by tissue plasminogen activator, and so fibrin isnt broken down (clots remain)
What is the clotting cascade (simplified)?
1. Damage blood vessel releases clotting factors
2. Clotting factors turns prothrombin into thrombin
3. At the same time, platelets are getting 'sticky' and creating a plug at the wound site
4. thrombin reacts with fibrinogen to create fibrin
5. fibrin is a protein strand that weaves in and out of the platelet plug, stabilising it and creating the 'clot'
What is fibrinolysis?
- Once a clot is formed and done its job, the body will break it down to stop it from getting bigger.
- Plasminogen is activated into plasmin by tissue plasminogen activator (TXA will interrupt this step)
- Plasmin snips at the fibrin mesh of a clot, causing it to break down and its components are absorbed into the body
What is plasminogen?
- Circulates around the body in a closed an inactive state
- When it binds to a clot, it opens and waits to be activated
- While open, it will be activated by certain proteins (plasminogen tissue activator) binding to the lysine receptor sites
How does TXA work?
- TXA binds to the lysine receptor sites on the open plasminogen, but doesn't activate it
- This prevents plasminogen from activating into plasmin, therefore inhibiting fibrinolysis
- Thus stopping clot breakdown and reducing bleeding
What are the indications for TXA?
- Severe postpartum haemorrhage
- Severely injured patients at risk of acute traumatic coagulopathy
What is a COAST score?
Assesses a patients risk of coagulopathy in severe trauma, thus indicating the need for TXA. A score >3 is indicative for TXA
What does a COAST score assess?
- entrapment
- Systolic BP
- temperature
- Major chest injury needed decompression
- Abdominal/pelvic injury
When would you give TXA to the patient?
After EVERYTHING else --> basically when patient is loaded and on the move to the hospital
Contraindications for TXA?
- Injury occurred >2hours prior to administration
Possible adverse effects of TXA?
- Seizure
- Hypotension
- Dizziness
- Nausea
- Vomiting
- Diarrhoea
How is TXA administered?
- 1 gram of TXA into 100ml of dextrose 5% or normal saline, over 10 minutes (3 drops per second)
- 2 x 5ml injection to upper lateral thigh
Can a paediatric be given TXA?
No
TXA dose
1g/10mL, seperated into 2×5mL
How is TXA infused?
Add 1g of TXA into 100mL of dextrose or Normal Saline, and infuse over 10min.