Chapter 5 - Physical Foundations - Bones
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
Steady-state flows require _ gradients
Linear
Electrical capacitance application
Homeostasis (as it relates to flow)
steady supply of nutrients and removal of wastes
Steady state
no change in temperature, charge, concentration, pressure with time doesn’t usually happen in the body
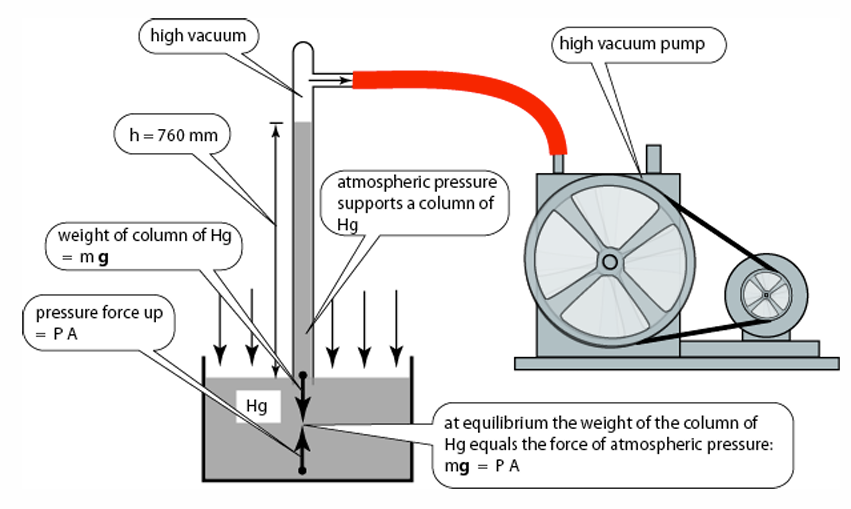
What drives fluid (including air) flow?
Pressure
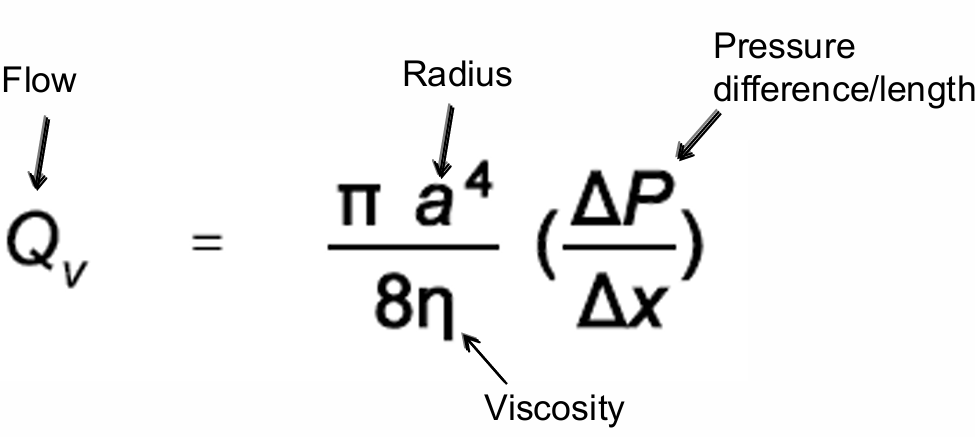
Poiseuille’s law governs
steady-state laminar flow in long narrow tubes
Laminar flow
Based on Reynold’s number
Flow through body often approximated as laminar
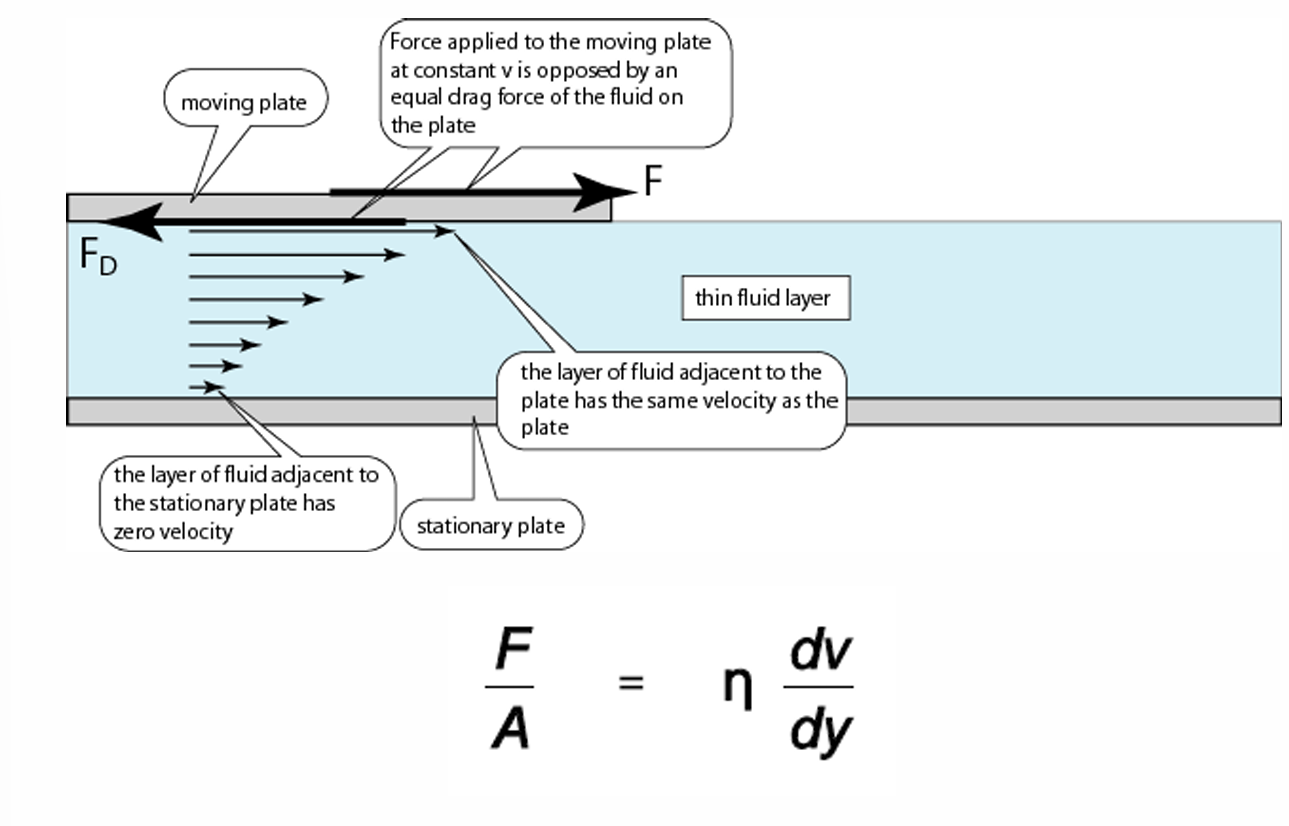
Viscosity
resistance of shear forces
(its the weird n in the equation)
Law of LaPlace
The larger the vessel radius, the larger the wall tension required to withstand a given internal fluid pressure
e.g: application trachea or food in esophagus
e.g: blood vessels cylindrical
e.g: bladder spherical
sphereical equation greater bc end on hot dogs break first (the sphereical part)
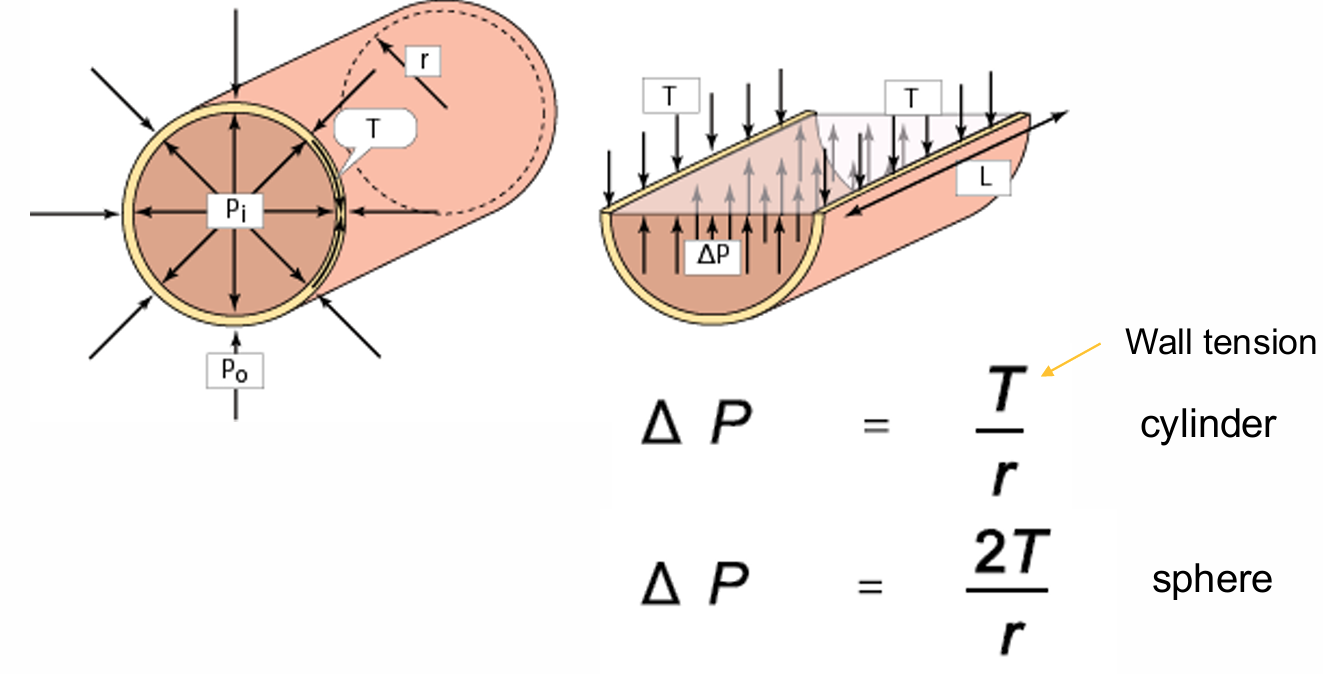
Law of LaPlace Equation break down
Pressure = (2 x Thickness x Tension)/Radius
Where
Pressure = The pressure inside the sphere
Thickness = Thickness of the sphere's wall
Tension = Tension within the sphere's wall
At a constant pressure, the tension in a filled sphere can be decreased by increasing the thickness of the wall
eg: calculating heart failure, wall thickness matters
Electrical forces between charged particles (when they repel vs attract)
Like charges repel, opposite charges attract
force very dependent on distance
in pic: q = charge, r = distance
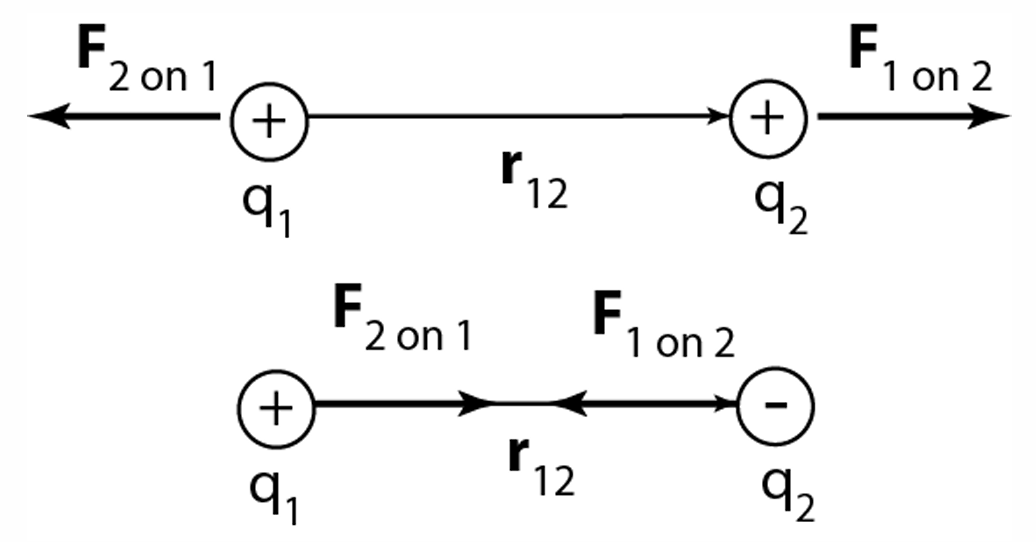
Coulomb’s Law
Separated charges in a vacuum experience a force on
one another described by Coulomb’s law
• Sign depends on the signs of point charges
• If space is some medium, add dielectric constant,
important thing charge and distance
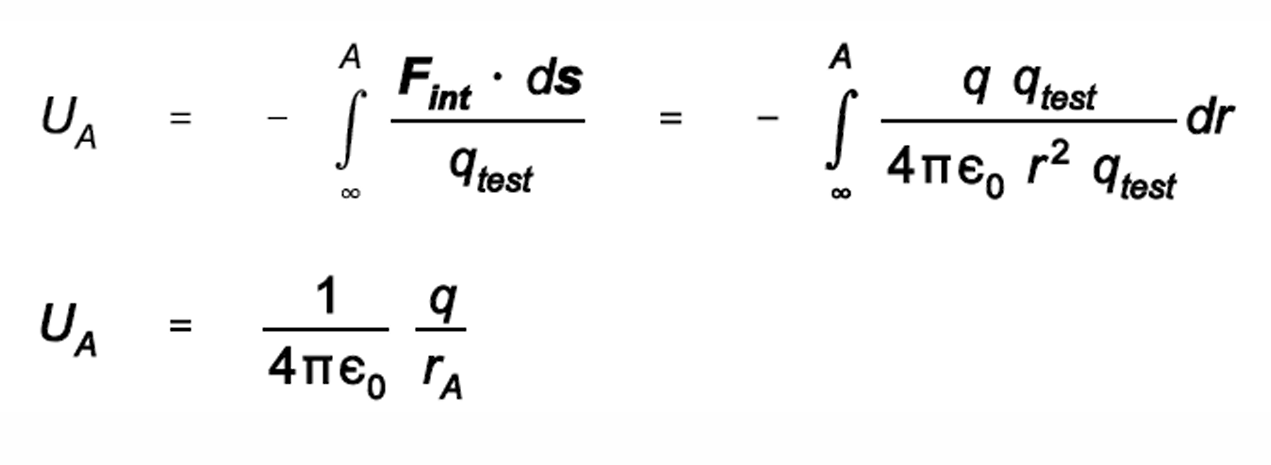
Electric potential
work necessary to move charge
Definition: Potential at a point in an electric field is defined as the work done in moving a unit positive charge from infinity to that point.
Potential surrounding a negative charge is negative, can get energy out of by bringing a positive charge toward it
Conclusion: A separation of charge produces an electric potential
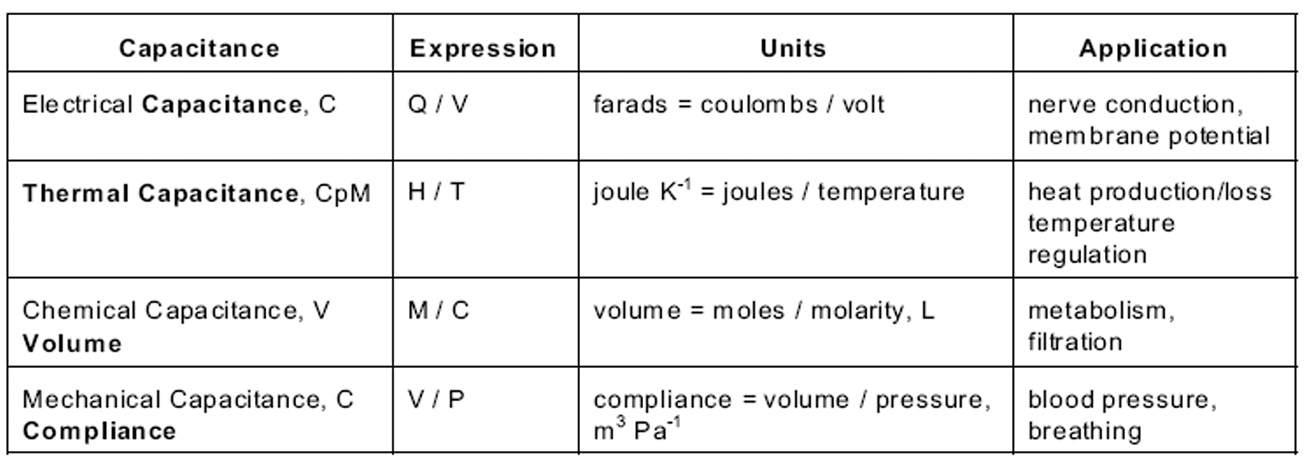
capacitance
the ability of a system to store electrical charge
dependent on area of plate and separation of plates
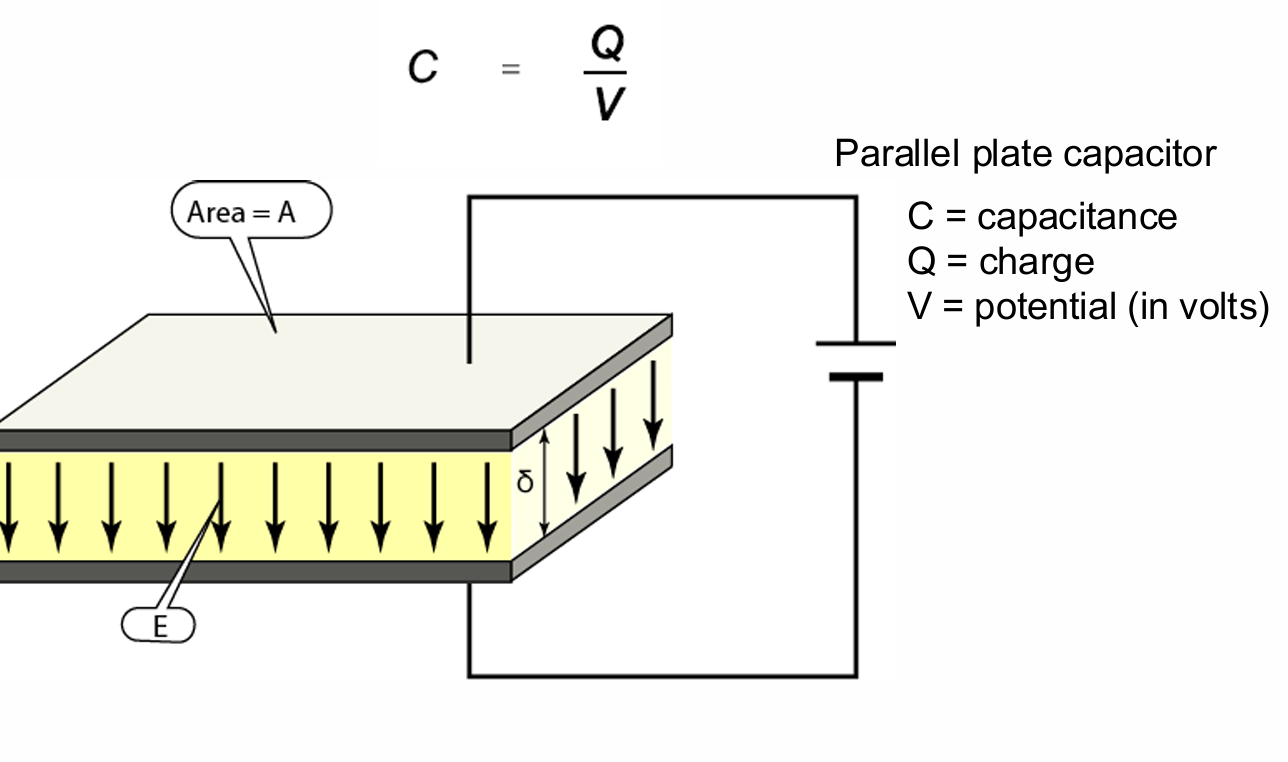
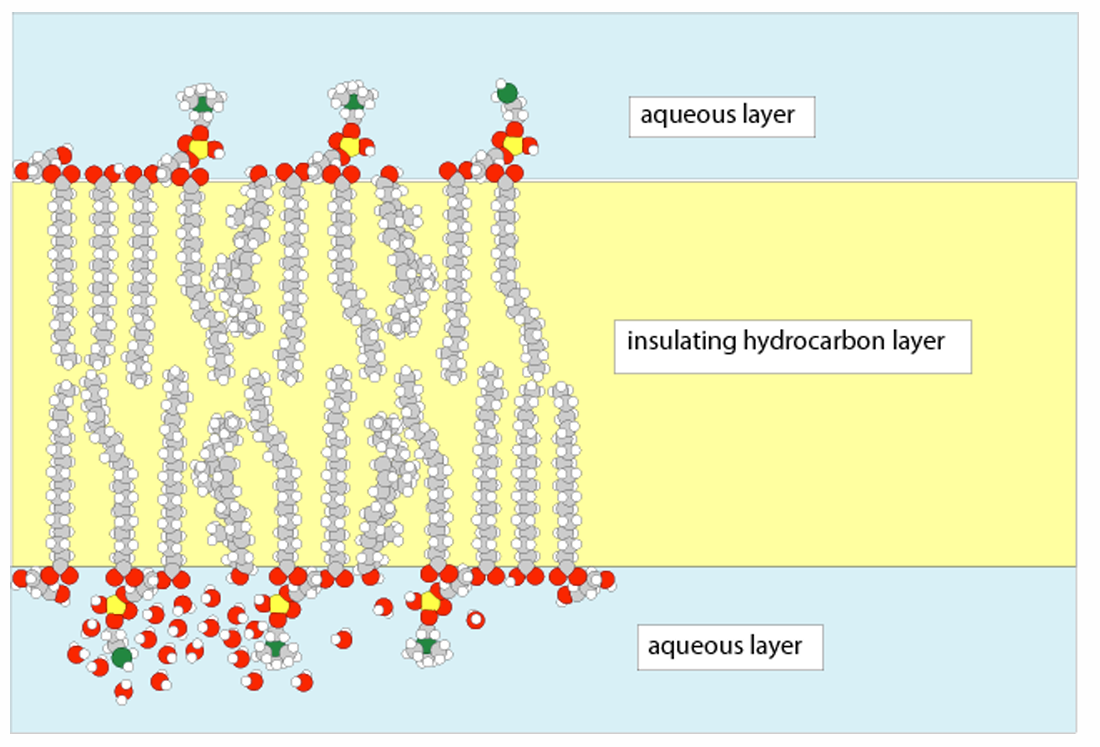
Biological membranes are essentially _
parallel plate capacitors
hydrocarbon layer important to separate charges and create potential
current
when there’s a net movement of solute and the solute as charge to it
ion channels
Have narrow, highly selective pores that can open and close
significantly faster than carrier protein
100 million ions/second can pass through one open channel, 105 times faster than the fastest carrier protein
Cannot be coupled to an energy source, only ion diffusion down the concentration gradient
Selective – permit some inorganic ions to pass, but not other; must shed associated water molecule
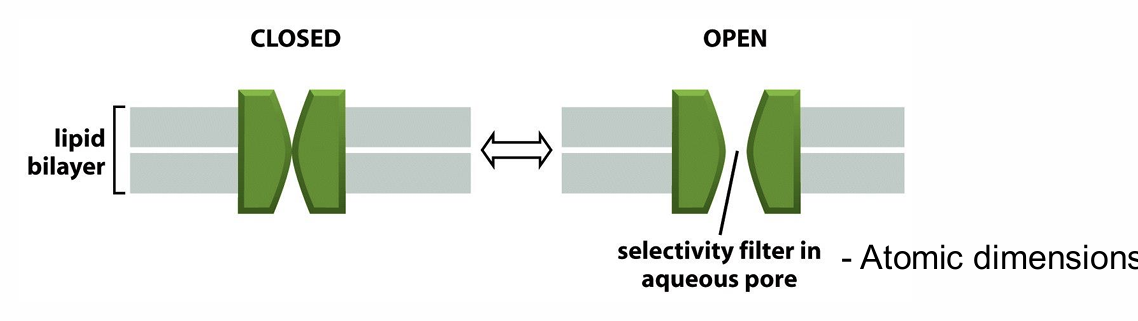
Selectivity filters
Protein structures in ion channels or aquaporins that allow only specific molecules through
are ion channels continuously open?
no
gated
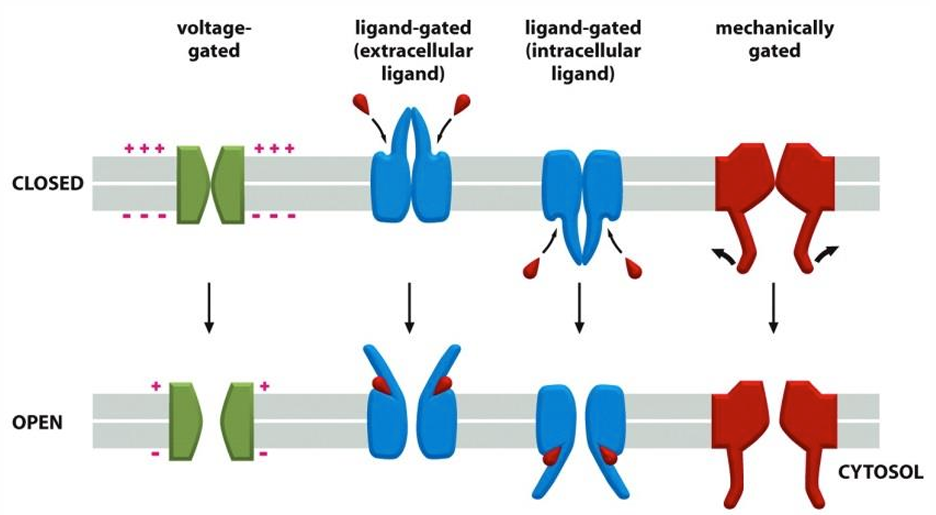
type of ion channel gates
Voltage gated
Mechanically gated
Ligand gated: Open in response to binding of a ligand
Mechanically-gated ion channels important facts
are also sensors for a number of other systems
Include touch, hearing and balance
Example: Mechanotransduction
Ion channels (specifically Ca2+) that respond to changes in substrate stiffness
Important in cardiovascular regulation/pathogenesis
Membrane potential
Arises when there is a difference in the electrical charge on each side of the membrane
Result from passive ion diffusion (animal cells)
In animal cells, Na+ - K+ pumps keep intracellular [Na+] low
K+ balances the negatively charged molecules
K+ can move freely in or out of cell in K+ leak channels or is pumped in by Na+ - K+ pumps
Membrane potential can be determined from the steepness of the K+ concentration gradient
what happens when no initial voltage gradient across the plasma
membrane (membrane potential = 0)
K+ is high inside of the cell and low outside of the cell
K+ will leave the cell through K+ leak channels, driven by concentration gradient
As K+ leaves, each ion leaves behind an unbalanced negative charge
A membrane potential is created
Efflux of K+ stops when the electrical driving force on K+ exactly balances the concentration gradient
Electrochemical gradient = 0
Resting membrane potential
equilibrium condition
Resting potential of animal cells varies between -20 mV and 120 mV
balance between chemical concentration force and electrical driving force
Use of Nernst equation
Can be used to calculate the theoretical resting membrane potential if we know the ratio of internal and external ion concentrations
The actual value is slightly off, cell is permeable to more than K+ and Cl
physiological significance of membrane potiental and ion movement
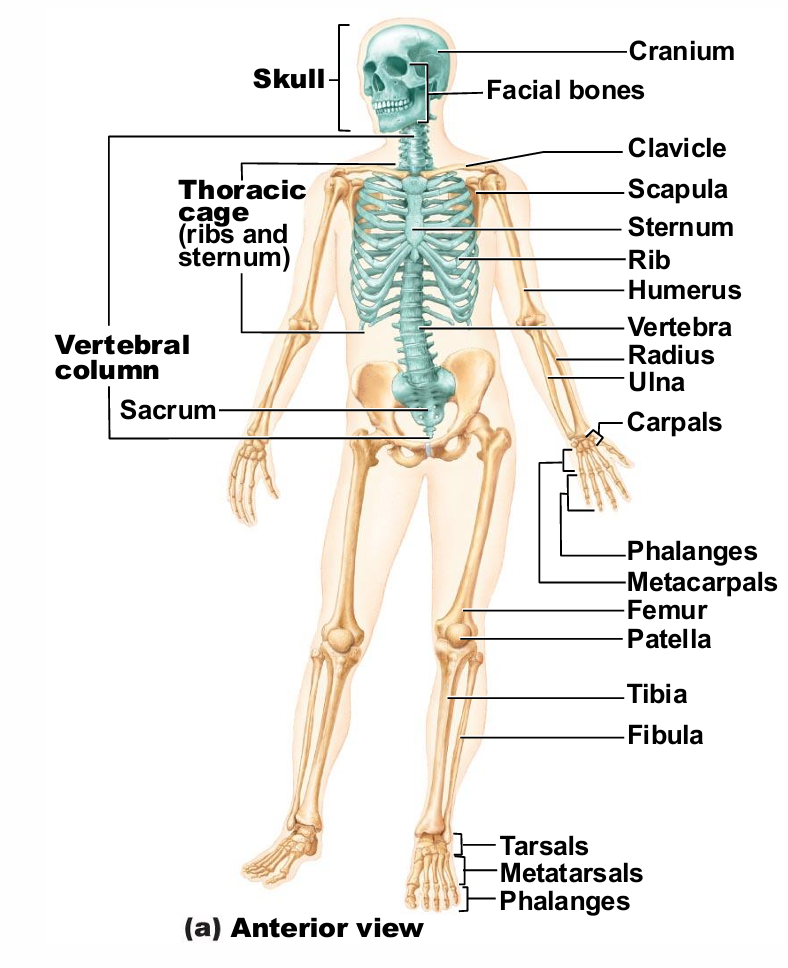
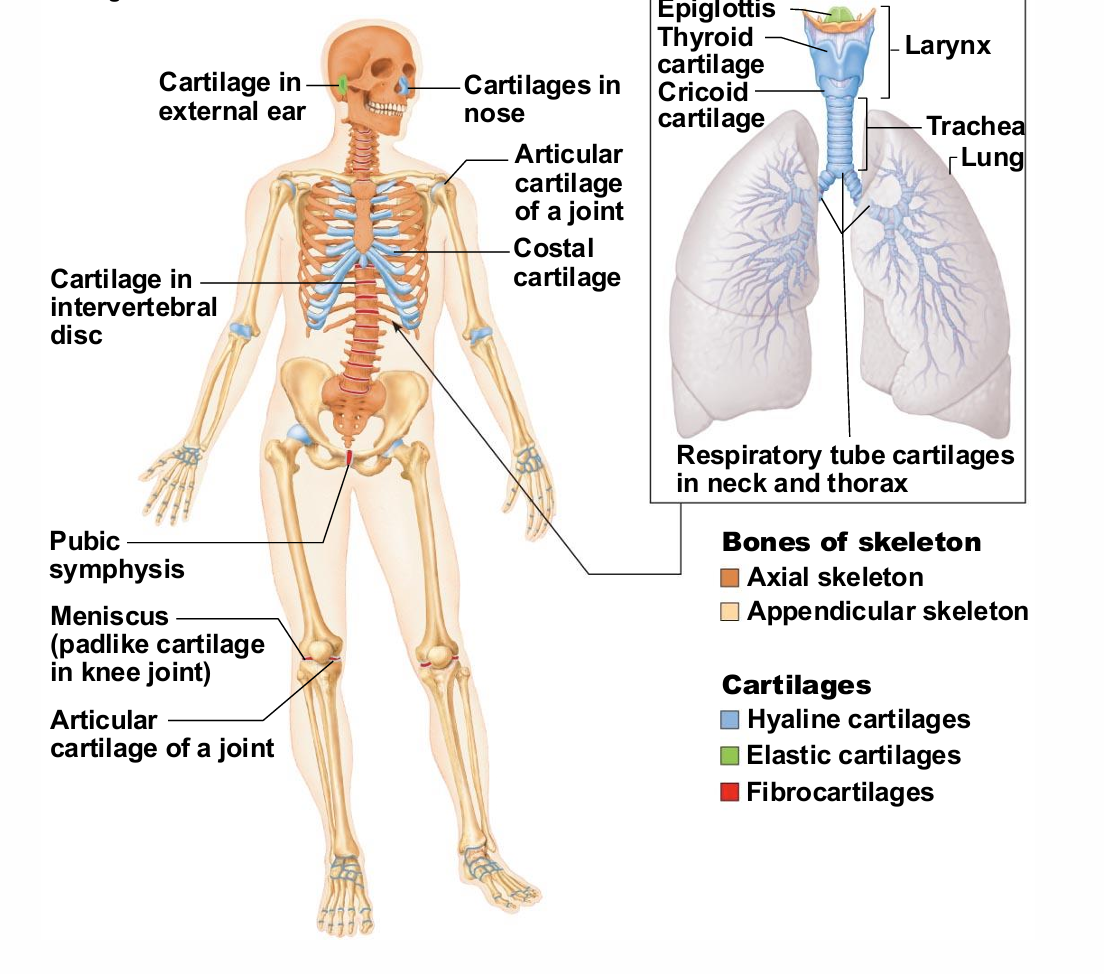
Skeletal sytem composed of
bones
cartilages
joints
ligaments
connect bone to bone
skeletal system _% of body mass
20
how many named bones in skeleton
206
Classification of bones (2 groups)
Axial skeleton
Long axis of body
Skull, vertebral column, rib cage
Appendicular skeleton
Bones of upper and lower limbs
Girdles attaching limbs to axial skeleton
The Axial Skeleton
Consists of 80 bones
Three major regions
Skull
Vertebral column
Thoracic cage
Skeletal Cartilage
all types of skeletal cartilages contain _
chondrocytes in lacunae and extracellular matrix
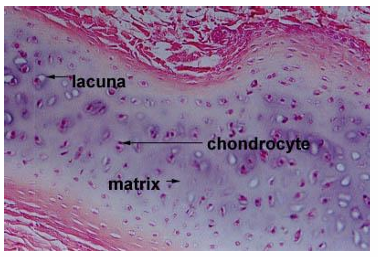
types of skeletal cartilage
hyaline cartilage
elastic cartilage
fibrocartilage
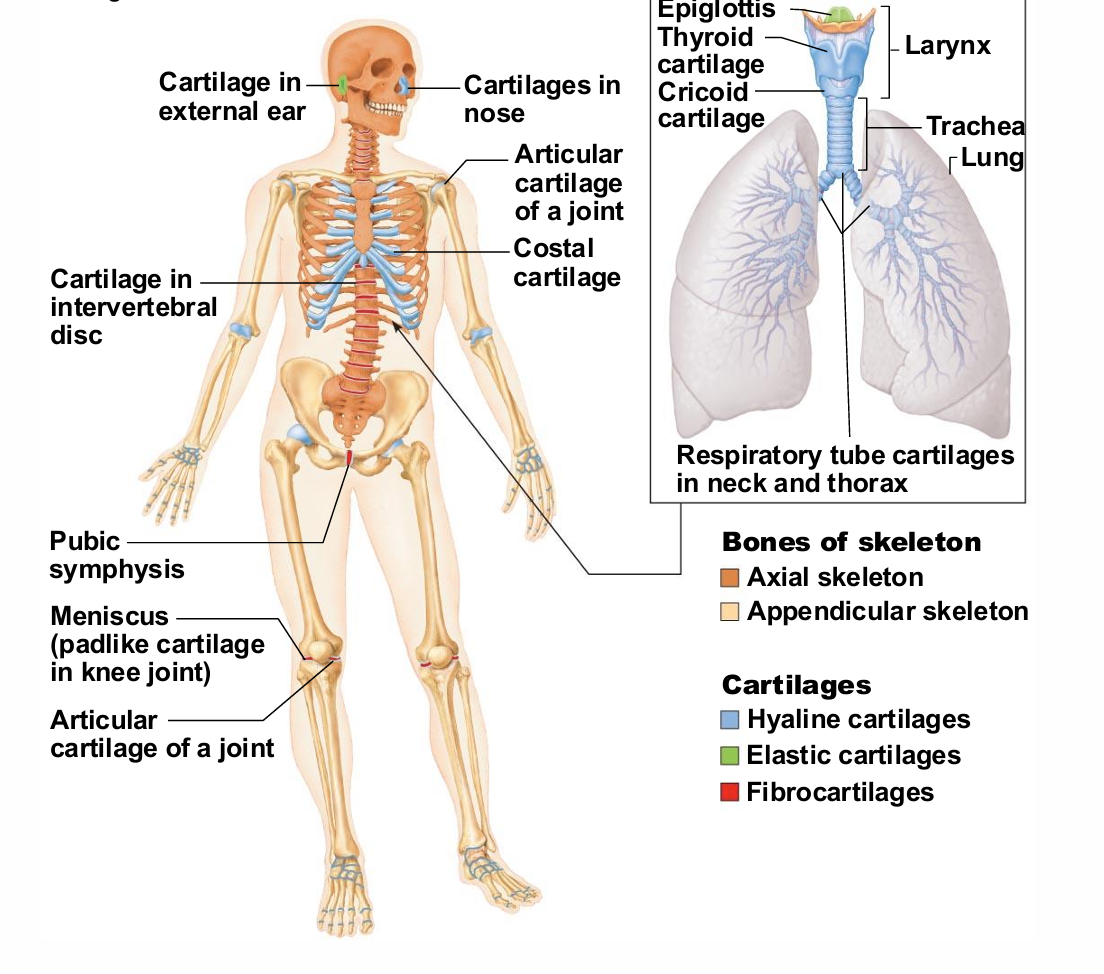
Hyaline cartilage
Provides support, flexibility, and resilience
transfers of stresses
Most abundant type
mainly found at articulated surfaces
Articular, costal, respiratory, nasal cartilage
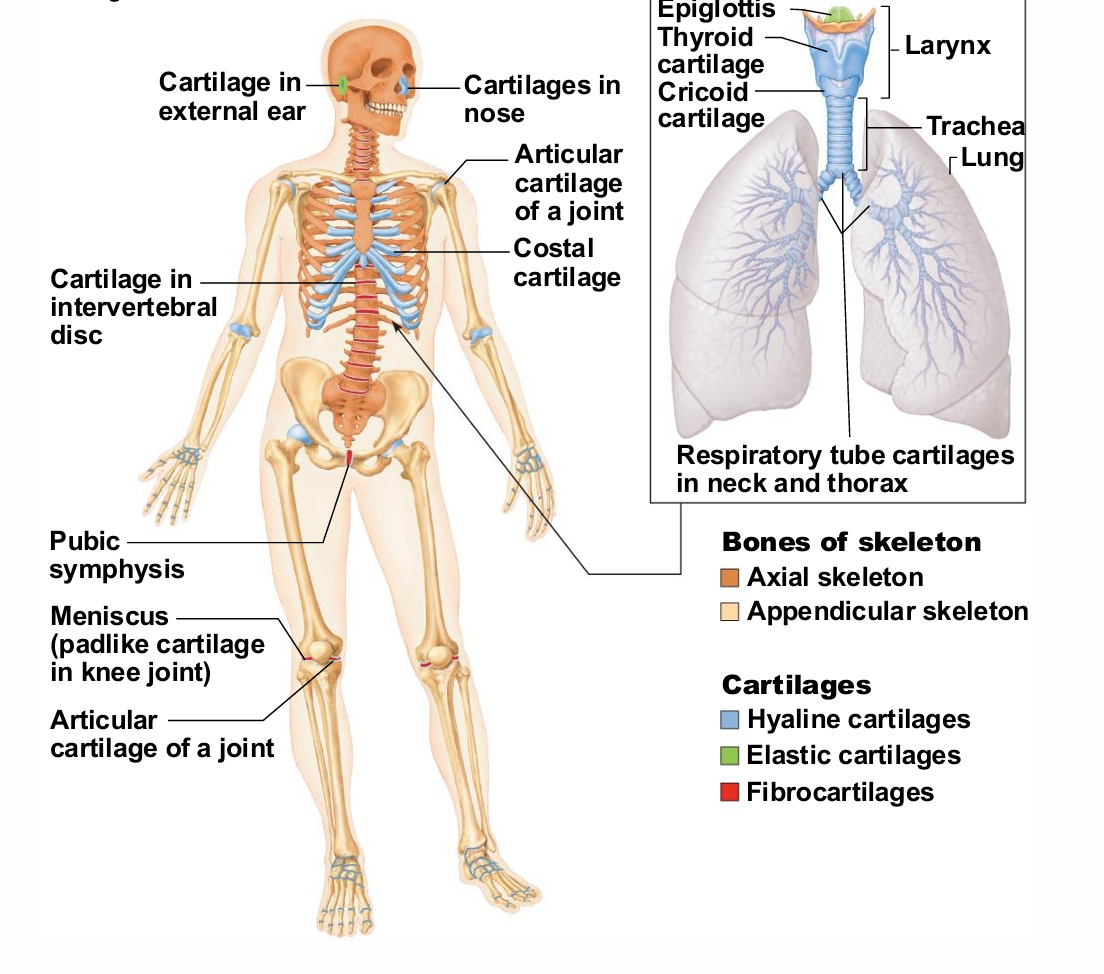
Elastic cartilage
has high concentration of elastane
Similar to hyaline cartilage, but contains elastic fibers
External ear and epiglottis
much less than the amount of hyaline cartilage
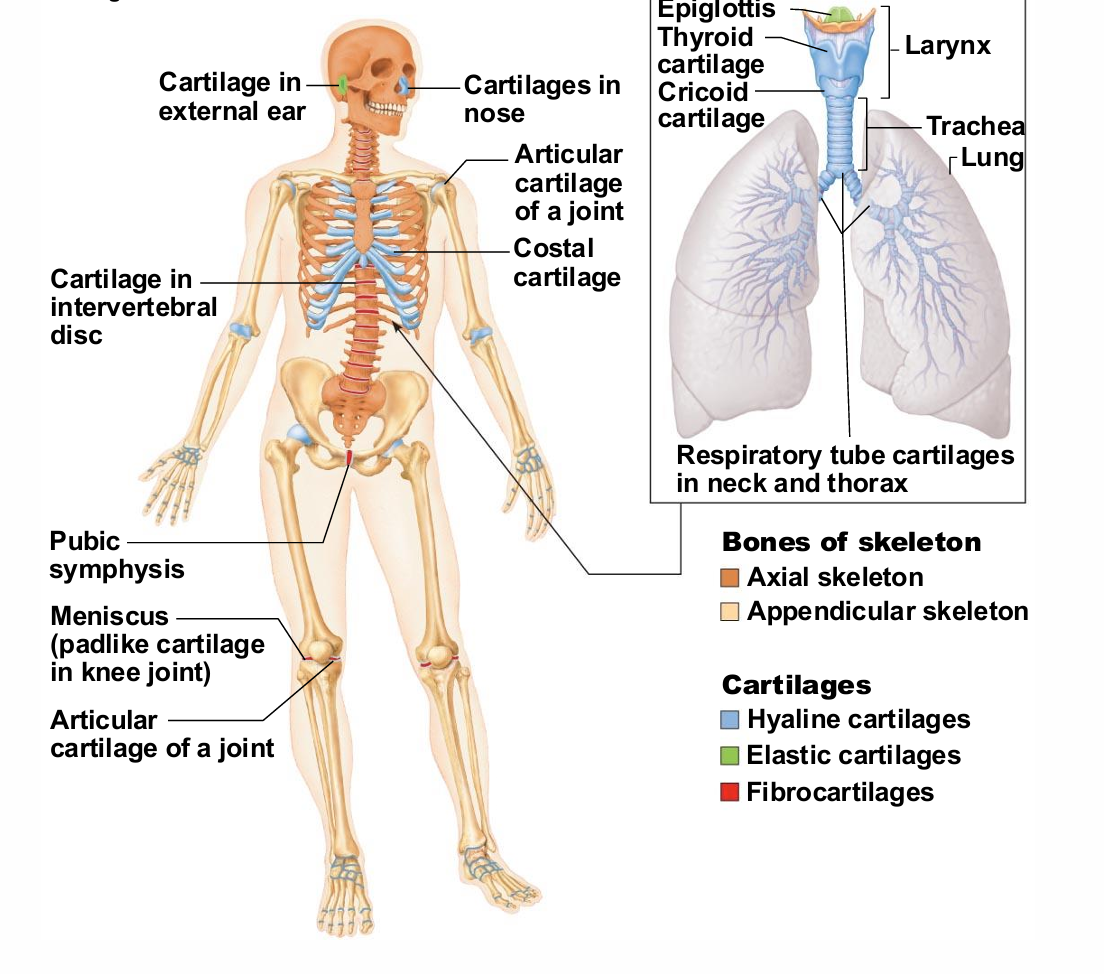
Fibrocartilage
Thick collagen fibers—has great tensile strength
Menisci of knee; vertebral discs
weight barring areas
Growth of Cartilage
Appositional growth
Interstitial growth
can become calcified
Appositional growth
Cells secrete matrix against external face of existing cartilage
building outward
Interstitial growth
Chondrocytes divide and secrete new matrix, expanding cartilage from within - more to come
growing from center
Calcification of cartilage
Occurs during normal bone growth
Hardens, but calcified cartilage is not bone
not the same absorbance/dissipation of energy
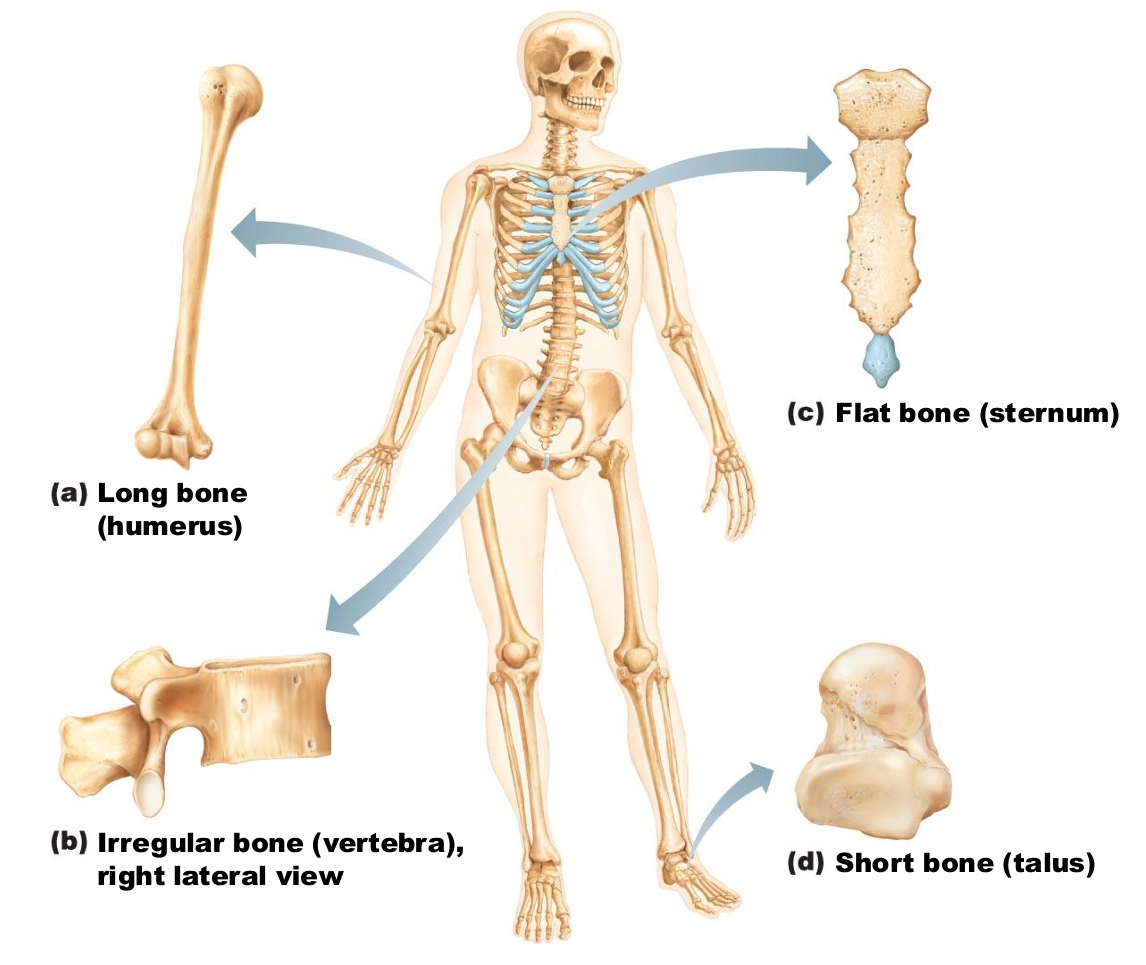
Classification of Bones by Shape
Long bones
Short bones
Flat bones
Irregular bones
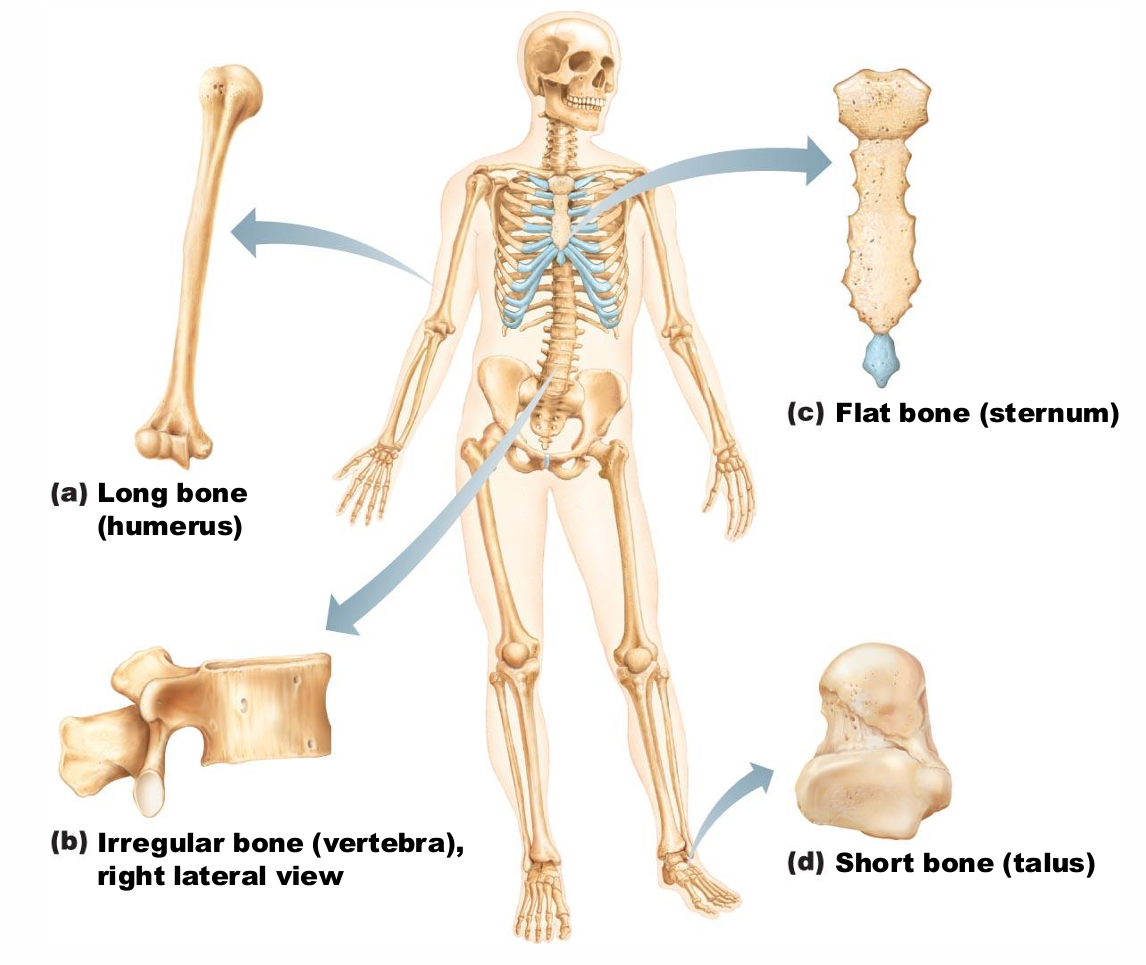
Long bones
Longer than they are wide
Limb, wrist, ankle bones
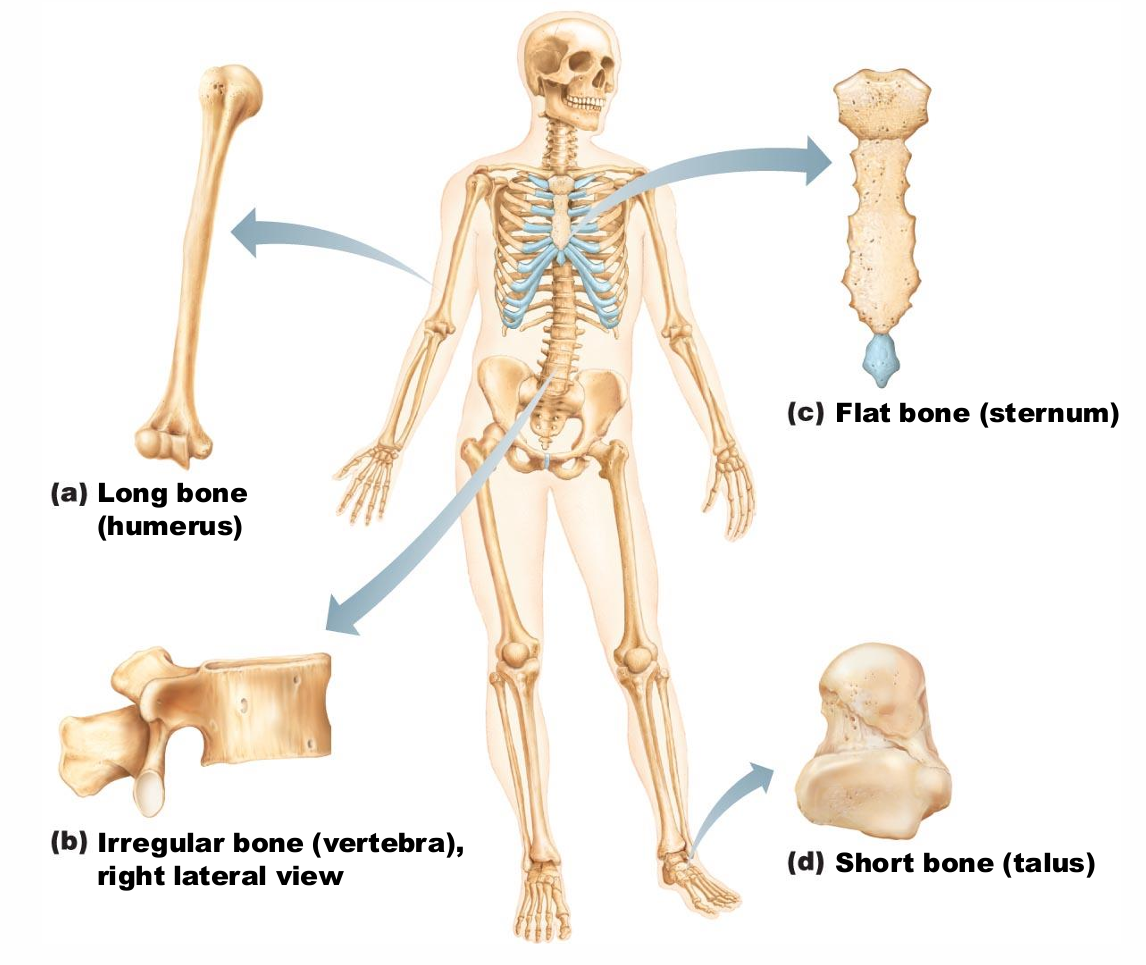
Short bones
Cube-shaped bones (in wrist and ankle)
sesamoid bones (within tendons, e.g., Patella)
Vary in size and number in different individuals
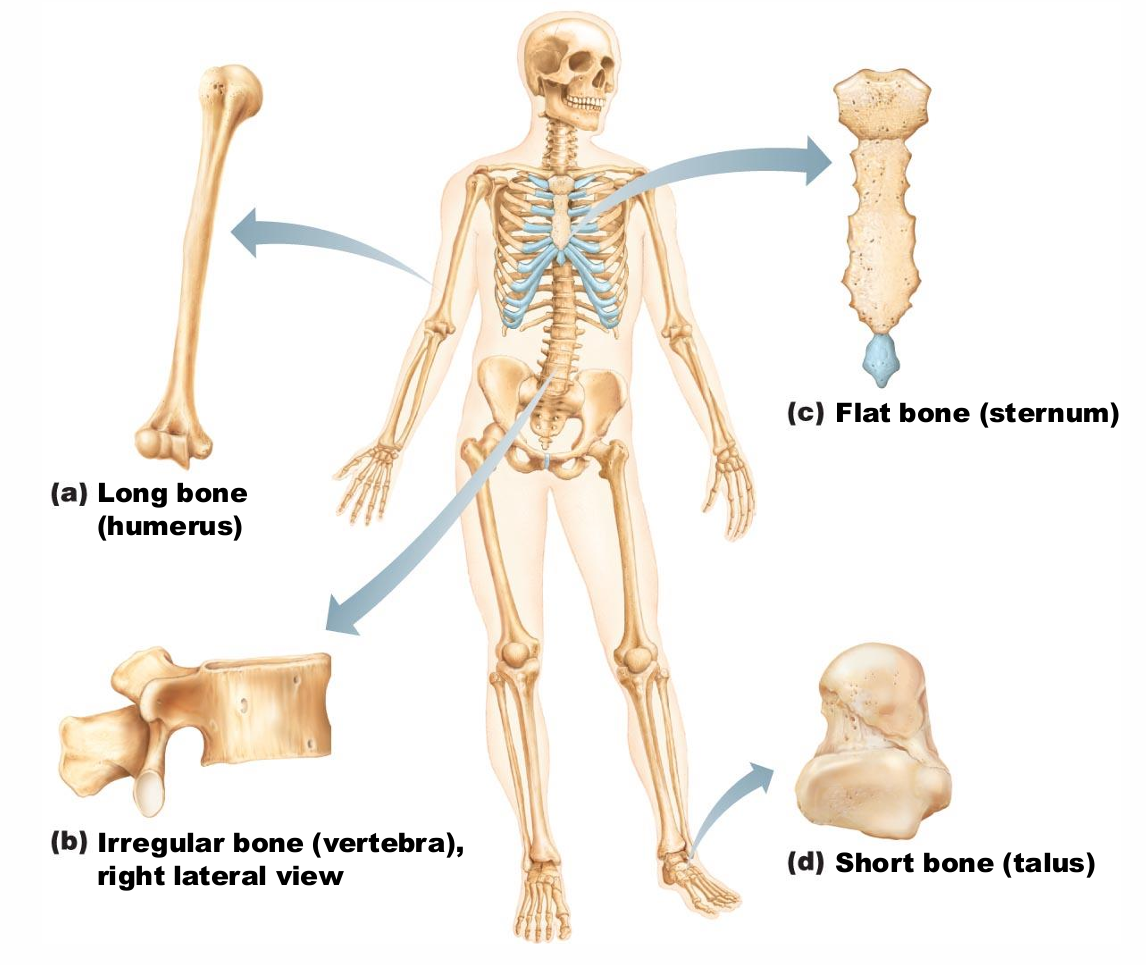
Flat bones
Thin, flat, slightly curved
Sternum, scapulae, ribs, most skull bones
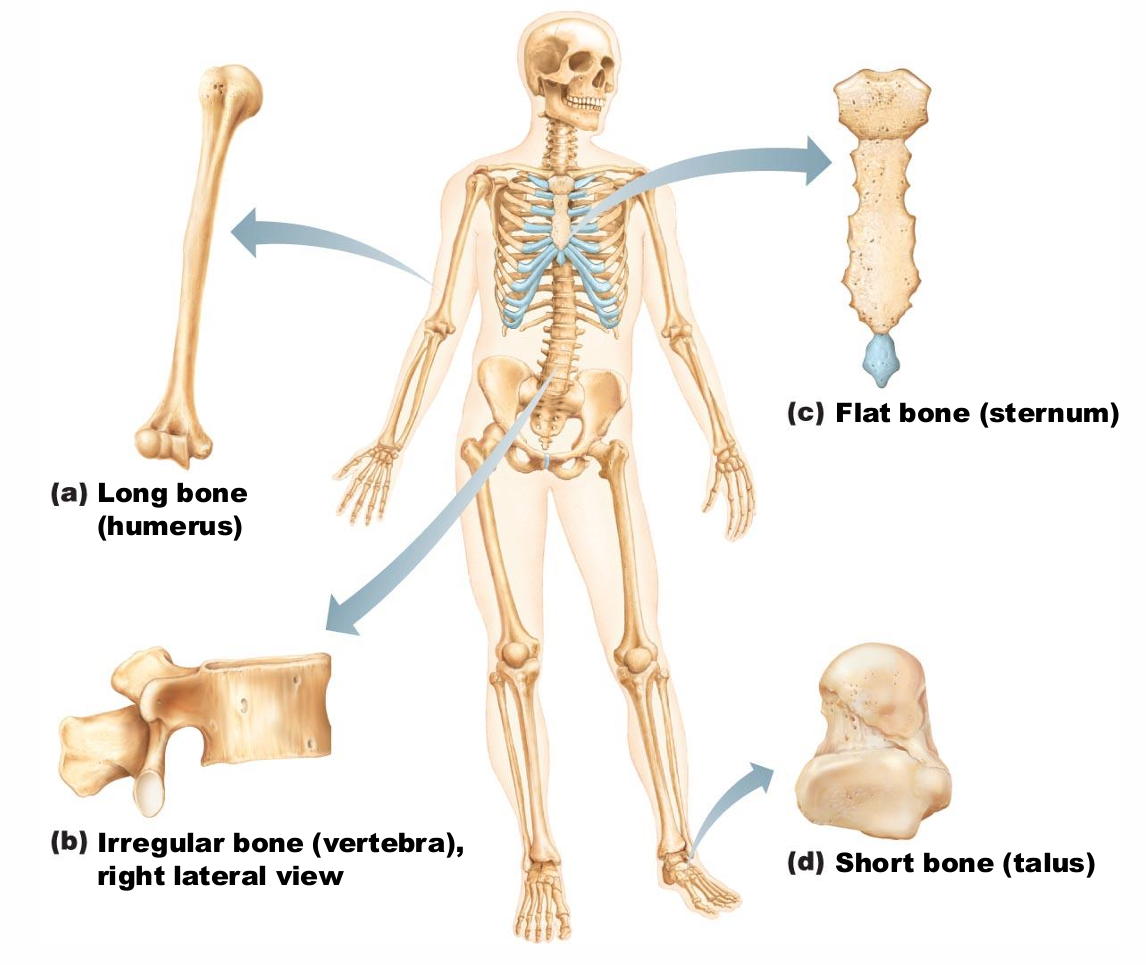
Irregular bones
Complicated shapes
doesn’t fit into other catorgories
Vertebrae, coxal bones
Functions of Bones
Support
Protection
Movement
Mineral and growth factor storage
Blood cell formation
Triglyceride (fat) storage
Hormone production
Bones provide support for _
body and soft organs
Bones provide protection for _
brain, spinal cord, and vital organs
Bones provide movement via _
Levers for muscle action
Mineral and growth factor storage function of bone
Calcium and phosphorus, and growth factors reservoir
mineral matrix storage
hematopoiesis takes place in_
red marrow cavities of certain bones
Triglyceride (fat) storage in bone cavities importance
energy source
Hormone production in bones
Osteocalcin
Regulates bone formation
Protects against obesity, glucose intolerance, diabetes mellitus
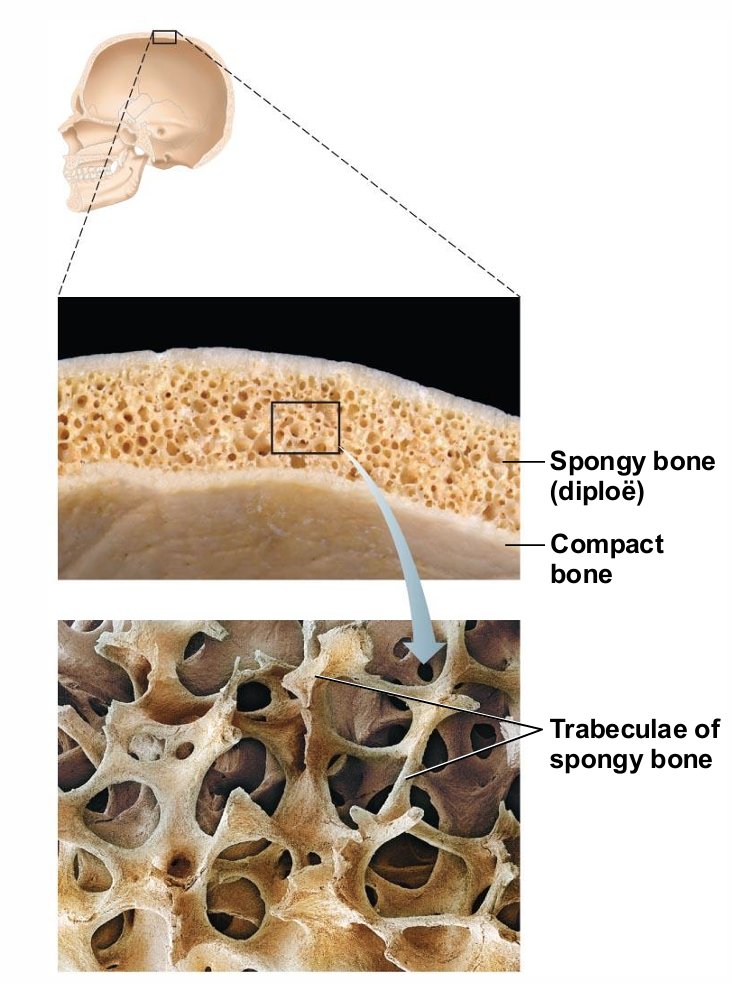
Bone textures (other way to classify)
Compact/Cortical
Dense outer layer; smooth and solid
Spongy/Trabecular
Honeycomb of flat pieces of bon
Structure of Short, Irregular, and Flat Bones
Thin plates of spongy bone covered by compact bone
very very thin is flat bones
Plates sandwiched between connective tissue membranes
Periosteum (outer layer) and endosteum
No shaft or epiphyses
different from long bones
Bone marrow throughout spongy bone; no marrow cavity
Hyaline cartilage covers articular surfaces
Structure of typical long bones
Diaphysis
long shaft section
Epiphyses
two ends
Diaphysis
part of long bone
Tubular shaft forms long axis
Compact bone surrounding medullary cavity
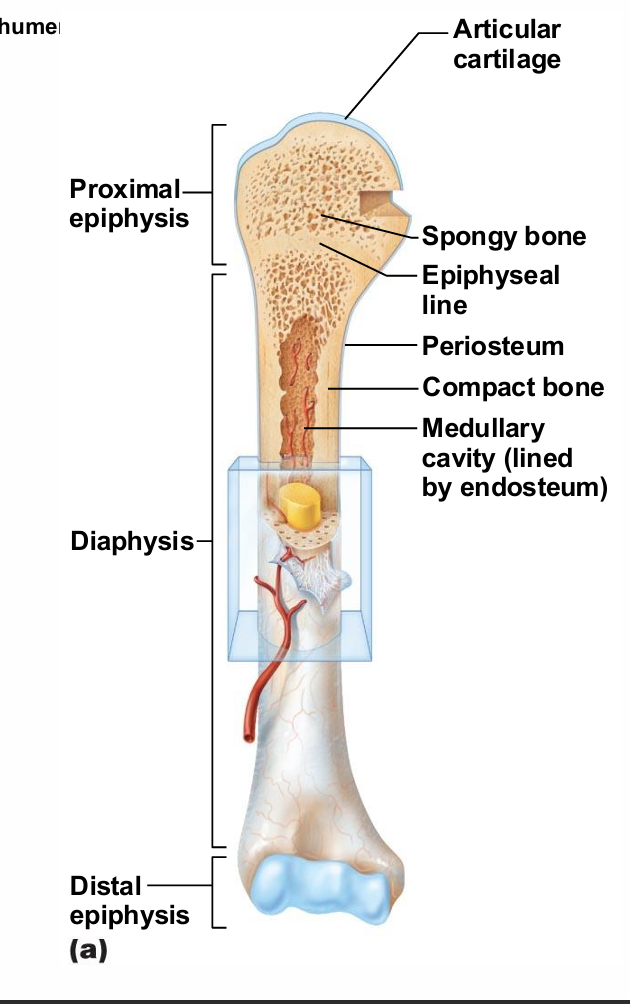
Epiphyses
part of long bone
Bone ends
External compact bone; internal spongy bone
Articular cartilage covers articular surfaces
Between is epiphyseal line
Remnant of childhood bone growth at epiphyseal plate
growth plate, calcifies when down growing
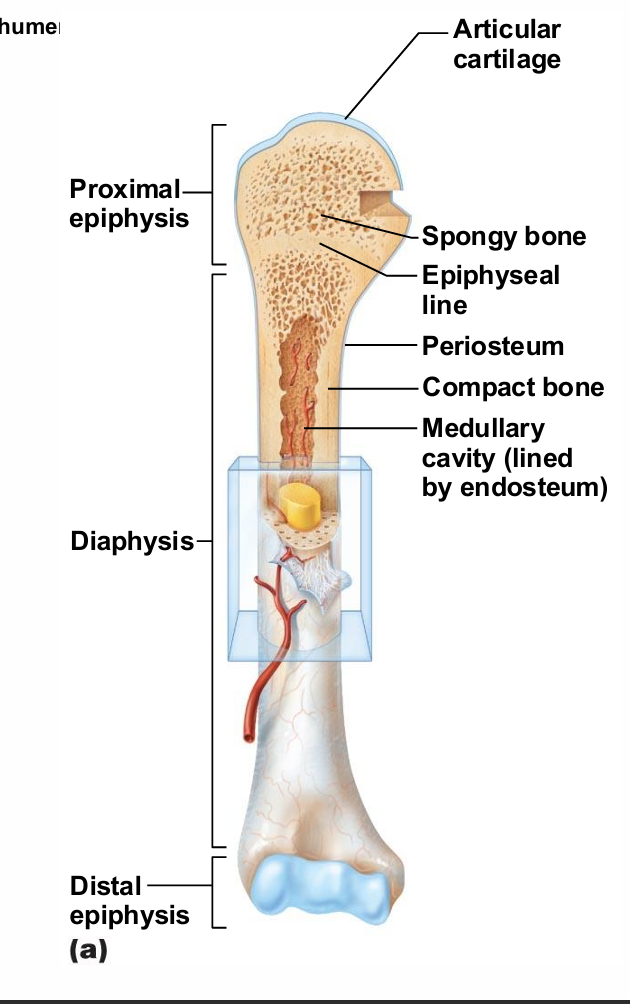
Red marrow
Found within trabecular cavities of spongy bone and diploë of flat bones (e.g., sternum)
Adult long bones have little red marrow
found in ends of long bones
have tons when born but converts to yellow
Heads of femur and humerus only
Red marrow in diploë and some irregular bones is most active
Yellow marrow can convert to red, if necessary
usually in diseased states
differences in Hematopoietic tissues in bones
Red vs. Yellow marrow
Main difference:
Red bone marrow produces red blood cells, white blood cells, and platelets (color from hemoglobin in red blood cells)
Yellow bone marrow produces fat cells, cartilage, and bones (color from fat cells)
Both have lots of blood vessels and capillaries
At birth, all bone marrow is red
In adults, red marrow is mainly in the flat bones and the proximal ends of the long bones
Major cell types of bone
Osteogenic cells
Osteoblasts
Osteocytes
Bone lining cells
Osteoclasts
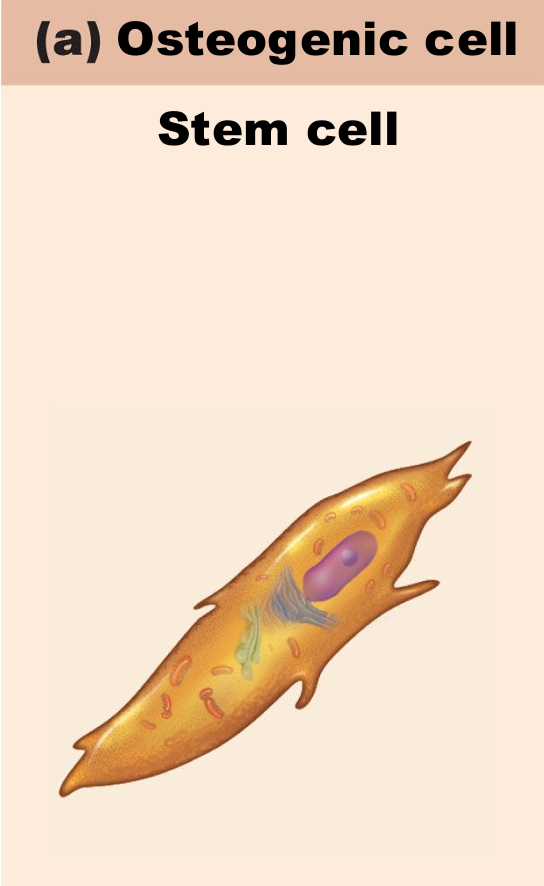
Osteogenic Cells
Also called osteoprogenitor cells
Mitotically active stem cells in periosteum and endosteum
When stimulated differentiate into osteoblasts or bone lining cells
Some persist as osteogenic cells
pic
pretty small
not doing much in tissue, but ready
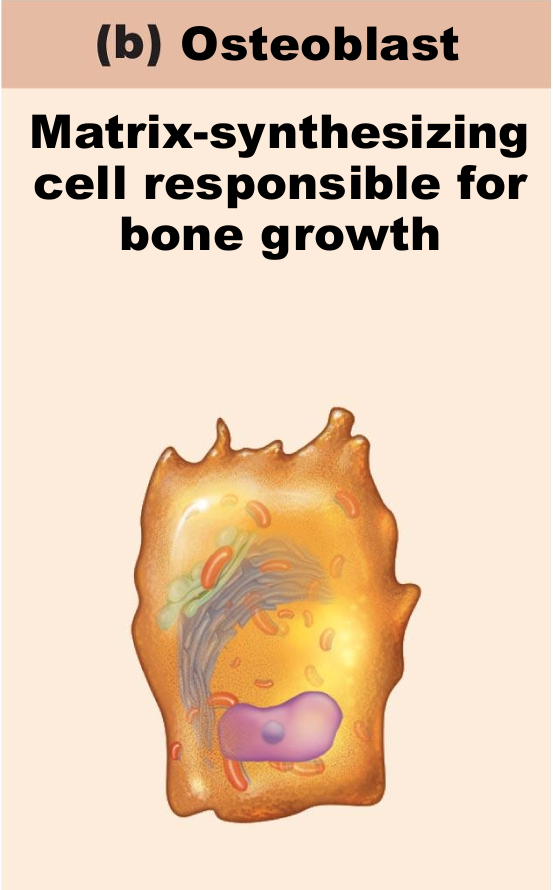
Osteoblasts
Bone-forming cells
Secrete unmineralized bone matrix or osteoid
Includes collagen and calcium-binding proteins
Collagen = 90% of bone protein
Osteogenic cells become osteoblasts
pic
much larger than osteogenic cells
have lots of proteins
able to synthesize
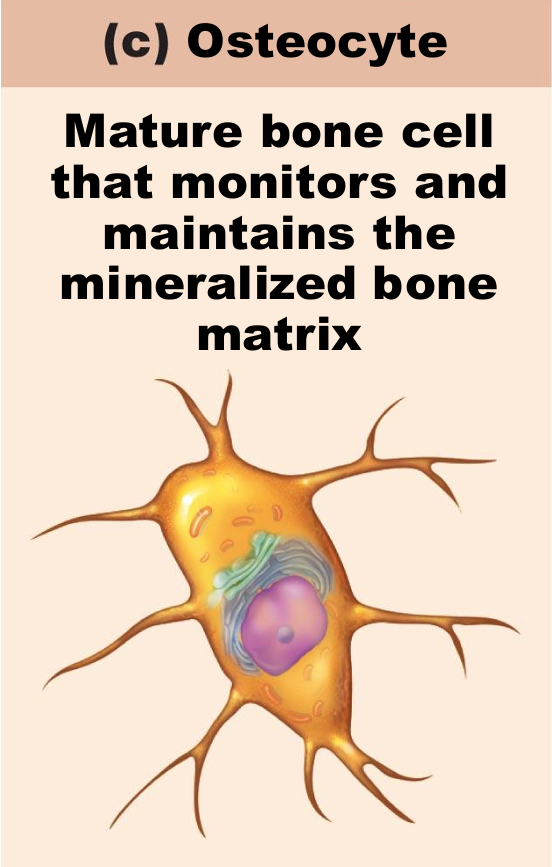
Osteocytes
Mature bone cells in lacunae
Monitor and maintain bone matrix
Act as stress or strain sensors
Respond to and communicate mechanical stimuli to osteoblasts and osteoclasts (cells that destroy bone) so bone remodeling can occur
lots of mechanically activated sensors
Wolf’s law, its there cell that sense the stress to tell osteoblasts to build more
pics:
needs to sense and communicate hence the protrusions
Bone lining cells
Flat cells on bone surfaces believed to help maintain matrix
On external bone surface called periosteal cells
Lining internal surfaces called endosteal cells
Do not fulling understand, think they help with bone maintenance
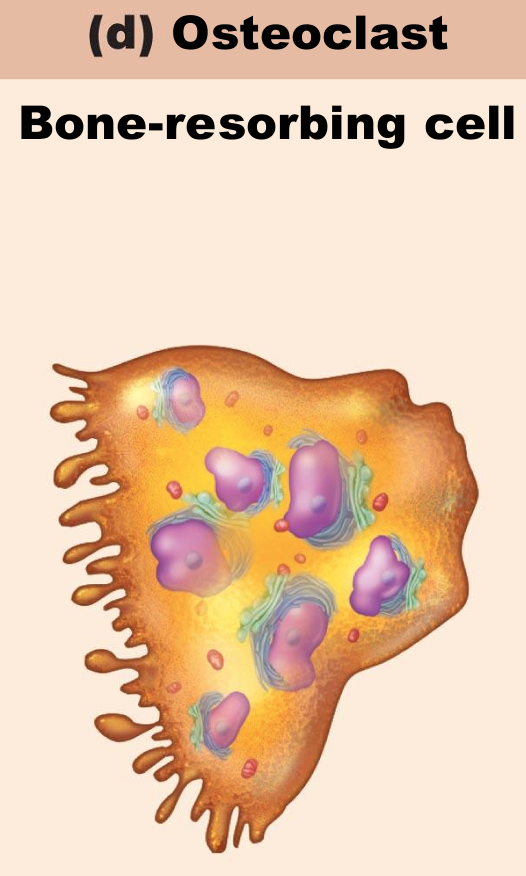
Osteoclasts
Derived from hematopoietic stem cells that become macrophages
not from bone percussors
relative of macrophage…phagocytosis
Giant, multinucleate cells for bone resorption
When active rest in resorption bay and have ruffled border
Not constantly active
Ruffled border increases surface area for enzyme degradation of bone and seals off area from surrounding matrix
Compact Bone - microscopic anatomy
Also called lamellar bone
Osteon or Haversian system
Structural unit of compact bone
Elongated cylinder parallel to long axis of bone (Diaphysis)
concentric
Hollow tubes of bone matrix called lamellae
Collagen fibers in adjacent rings run in different directions
Withstands stress – resist twisting
hollow center allows for integration and vascularization
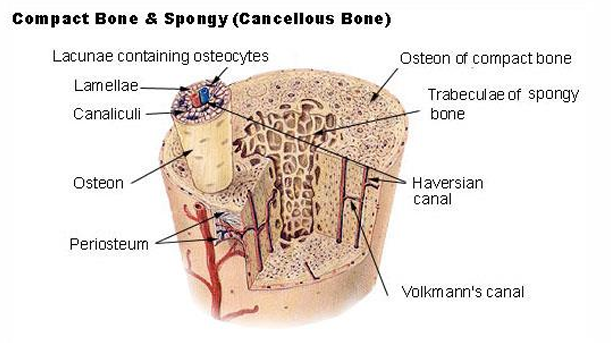
Canaliculi Formation
Osteoblasts secreting bone matrix maintain contact with each other and osteocytes via gap junctions
When matrix hardens and cells are trapped the canaliculi form
Allows communication
Permit nutrients and wastes to be relayed from one osteocyte to another throughout osteon
Lamellae types
Interstitial lamellae
Circumferential lamellae
Interstitial lamellae
Incomplete lamellae not part of complete osteon
Fill gaps between forming osteons
Remnants of osteons cut by bone remodeling
Circumferential lamellae
Just deep to periosteum
Superficial to endosteum
Extend around entire surface of diaphysis
Resist twisting of long bone
Microscopic Anatomy of Bone: Spongy Bone
Appears poorly organized
Trabeculae
Align along lines of stress to help resist it
No osteons
Contain irregularly arranged lamellae and osteocytes interconnected by canaliculi
Capillaries in endosteum supply nutrients