HEALTHSCI 2300A MIDTERM
1/70
Earn XP
Description and Tags
units 1-3
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
At approximately what vertebral level does the spinal cord end?
About the L1-L2 vertebral level.
What is the name for the end of the spinal cord?
The end of the spinal cord is called the conus medullaris.
What structure anchors the spinal cord to the coccyx and sacrum?
The filum terminale, which is an extension of the pia mater, which is responsible for anchoring the spinal cord to the coccyx and sacrum.
What is contained within the subarachnoid space?
The subarachnoid space contains cerebrospinal fluid (CSF).
Where are the cell bodies of sensory neurons clustered?
The cell bodies of sensory neurons cluster in the dorsal root ganglion, within the posterior/ dorsal root.
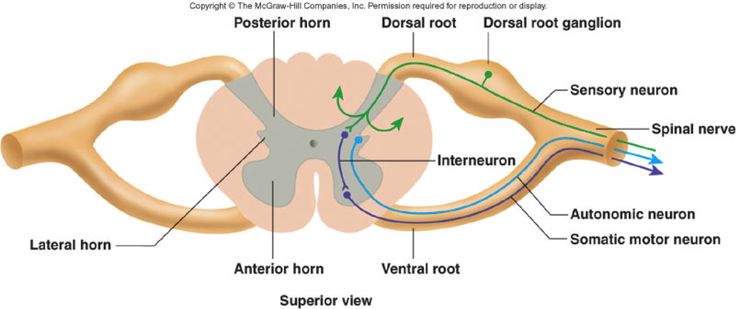
Where do the posterior/ dorsal rootlets enter the spinal cord?
Posterior/ dorsal rootlets enter the posterior horn of the gray matter.
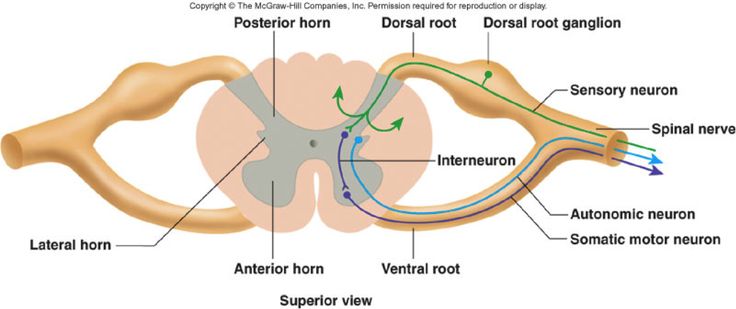
The anterior/ ventral rootlets are responsible for what function?
Anterior/ ventral rootlets are responsible for motor function.
What structure do the posterior and anterior roots combine to form?
The posterior and anterior roots combine to form the spinal nerve.
After exiting the intervertebral foramen, the spinal nerve splits into 2 rami. What are these rami?
The spinal nerve splits into the posterior/ dorsal ramus and the anterior/ ventral ramus.
What does the posterior/ dorsal ramus innervate?
The posterior/ dorsal ramus innervates the muscles and skin of the intrisic back.
Which spinal cord levels contribute neurons to the sympathetic trunk?
Sympathetic neurons at the spinal cord levels T1-L2 contribute to the sympathetic trunk.
What is the anatomical position?
Anatomical position is when a person stands upright, facing forward, with arms at their sides and palms facing up. Legs are parallel and feet are flat on the floor and facing forwards.
What plane splits the body into anterior and posterior sections?
The frontal (coronal) plane splits the body into anterior and posterior sections.
What plane splits the body into a left and right side?
The sagittal plane splits the body into right and left sides.
What is a transverse (horizontal or axial) plane?
A transverse plane cuts the body into upper and lower halves.
When referring to anatomical direction, what does proximal mean?
Proximal means closer to the trunk of the body.
When referring to anatomical direction, what does distal mean?
Distal means further away from the body of the trunk.
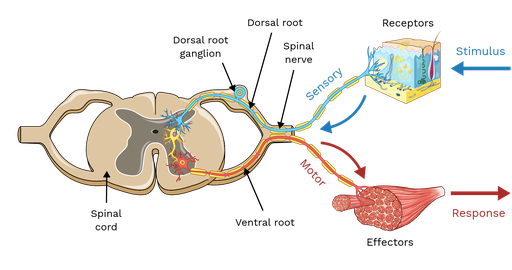
What are the two main skeletons of the body?
The two main skeletons are the axial and appendicular.
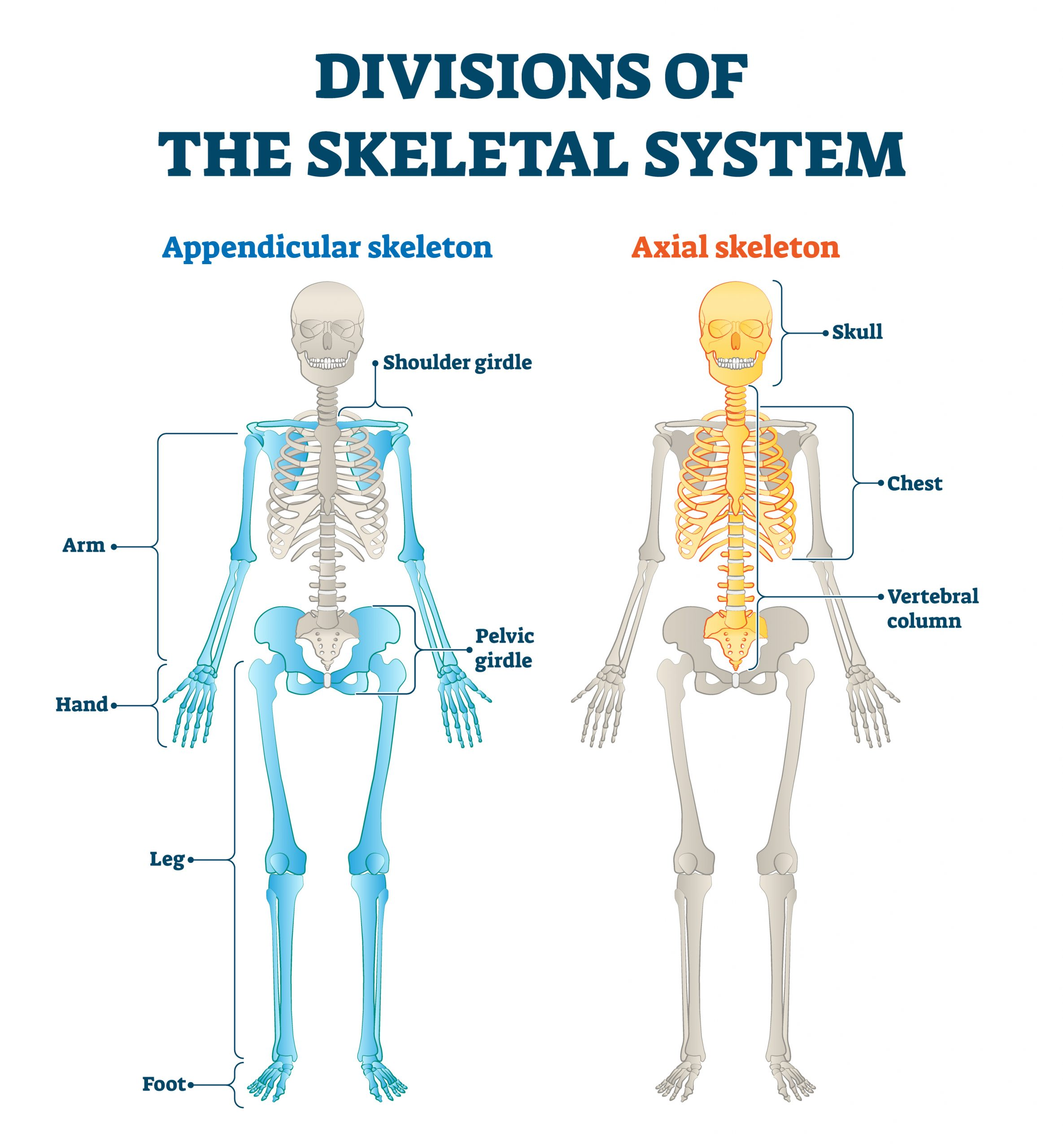
What does the axial skeleton consist of?
The axial skeleton consists of the skull, mandible, hyoid bone, vertebral column, ribs and sternum.
At what age does the epiphyseal plate typically close off in bone development?
The epiphyseal plate typically closes off as a person becomes an adult, approx 20 years old.
What are the 2 different types of bone tissue?
The two different types of bone tissue are cortical bone (compact bone) and trabecular bone (spongy bone).
What bone cells are responsible for bone production and bone absorption respectively?
Osteoblasts are responsible for bone production
Osteoclasts are responsible for bone absorption
Which type of bone fracture is more common in younger patients?
Greenstick fractures are common in younger patients and don’t go all the way through the bone.
What are short bones responsible for? Vs what are long bones responsible for?
Short bones are responsible for support and stability.
Long bones are responsible for give us structure and limbs mobility.
What is the function of sesamoid bones and give an example
Sesamoid bones protect tendons and increase their efficiency. An example of a sesamoid bone is the patella in the knee.
Describe a syndesmosis joint and where one would be found in the body
A syndesmosis joint has thick connective tissue between two bones, preventing movement. An example of this joint is between the tibia and fibula in the lower leg.
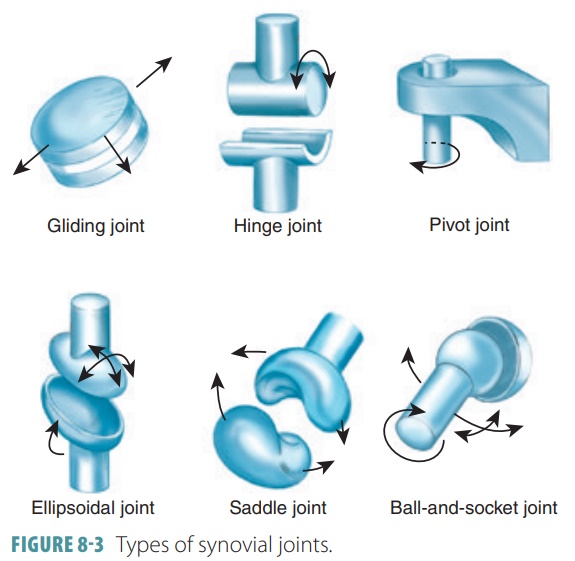
What distinguishes synovial joints from other joint types?
Synovial joints are distinguished by a joint cavity containing synovial fluid, which allows for a large range of motion.
What is the purpose of articular cartilage in a synovial joint?
Articular cartilage (AKA Hyaline cartilage) provides a smooth surface in a synovial joint, allowing for frictionless movement.
Besides articular cartilage, what other structures in a synovial joint help reduce friction?
Synovial fluid and bursae also help to reduce friction in the synovial joint.
What type of movement is allowed in a uniaxial joint and provide examples (2)
Uniaxial joints allow movement in one axis only. The pivot joint in the neck and hinge joints in the fingers are examples.
What are the 3 types of joints based on the amount of movement they allow?
The three types of joints from LEAST to MOST mobile are: solid joints, cartilaginous joints and synovial joints.
Describe the anatomical features and functions of the: cerebrum, cerebellum, brainstem and spinal cord
cerebrum: big area that holds cortical regions
cerebellum: extending off the brain stem, many functions
brainstem: midbrain, pons, and medulla oblongata (basal functions and pathways)
spinal cord: part of the central nervous system (CNS), different sections: cervical, thoracic and lumbar, sacral and coccygeal in lumbar section
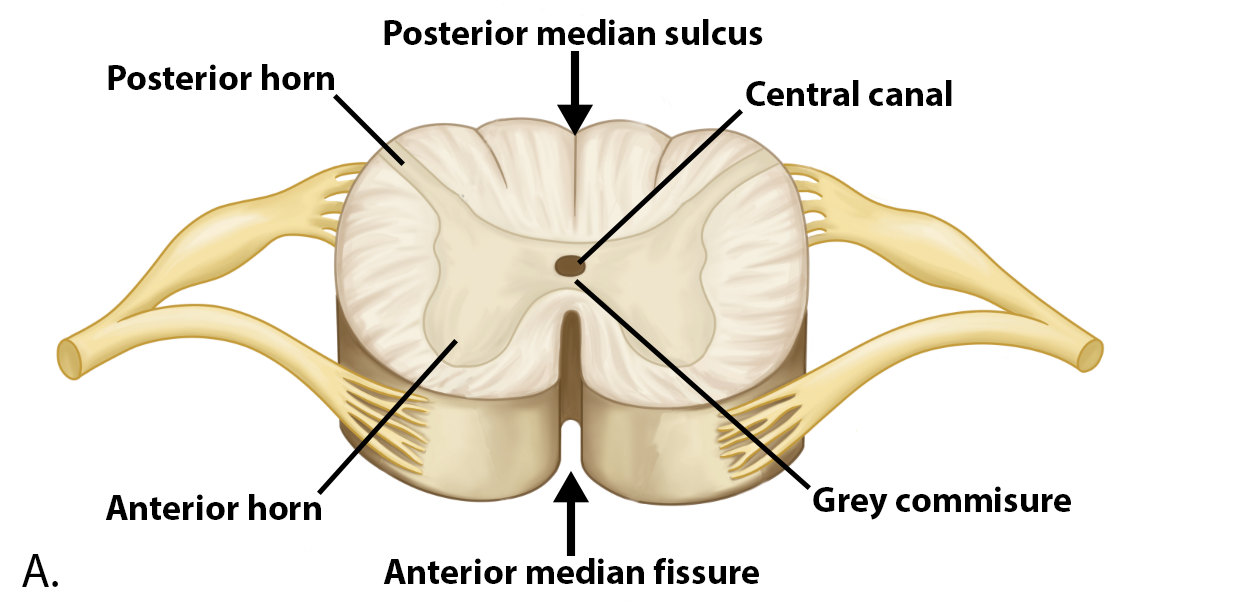
What is the difference between gray and white matter in the spinal cord?
gray matter looks like a butterfly in the middle, and white matter is on the outside of the spinal cord
neurons start within the gray matter, and axons leave through the periphery, creating the white matter
CSF goes through the central canal (v middle of the gray matter butterfly) → nourishes the spinal cord
Describe the locations and functions of the posterior horn, anterior horn and lateral horn
posterior horn → sensory input (thin butterfly top wing)
anterior horn → motor output (thick rounded butterfly bottom wing)
lateral horn → autonomic output (between posterior and anterior horn)
What are the layers of the spinal cord meninges and their functions?
spinal cord meninges (from most outer to inner layers)
dura mater: tough/ hard ‘mother’ → mother is protecting the most outer layer
arachnoid mater: ‘spider mother → ‘spider-web’ like projections where CSF is sitting, gives CSF stability
cerebrospinal fluid (CSF): within subarachnoid space
pia mater: ‘soft/ tender’ mother → layer which wraps directly onto the spinal cord
denticulate ligaments → looks like a shark tooth pointing out of the spinal cord, which anchors spinal cord to spinal column
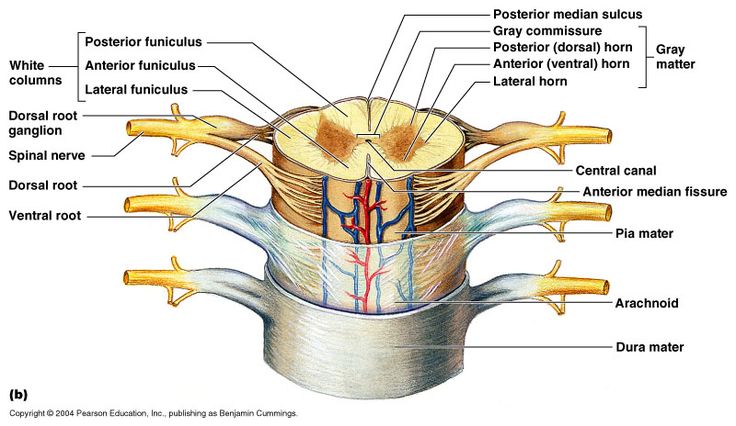
What are the spinal cord meninges spaces and applications?
subarachnoid space: between the arachnoid and pia mater
subdural space: between arachnoid and dura space (below the dura)
epidural spaces: outside of the dura mater
- ex. epidural, targeting the epidural space, to allow for slow diffusion or anesthetic
- ex. lumbar puncture, targeting subarachnoid space, for CSF sample or fast-acting spinal anesthesia
What are differences between dermatomes and nerve maps?
dermatomes: area of skin innervated by FIBERS from a SINGLE SPINAL NERVE
nerve map: area of skin innervated by a SINGLE PERIPHERAL NERVE
List the 6 cranial nerves and briefly describe their functions
12 pairs of nerves (bilateral)
general somatic → skeletal, muscle, skin
general visceral → blood vessels, glands, intraocular muscles
special somatic → vision, hearing
special visceral → taste, smell (chemical processes)
oculomotor nerve (CN III): pupillary constriction
facial nerve (CN VII): production of tears (lacrimal gland), production of saliva (sublingual and submandibular glands), production of mucus (nasal cavity and palate)
What is the difference between somatic and autonomic nervous systems?
somatic: general sensory, musculoskeletal movements and reflexes (motor)
autonomic: visceral afferents (sensory input FROM organs) and visceral efferents (motor output TO organs)
What is the difference between myotomes and dermatomes>
spinal nerve → muscle (myotome) → skin (dermatone)
myotome innervates similar groups of muscles to produce similar functions
dermatomes: area of skin innervated by fibres from a SINGLE SPINAL NERVE
Compare the parasympathetic to the sympathetic nervous system
parasympathetic nervous system (PSNS) : more chill functions, such as sleep and sexual activity → “rest and digest”, and “feed and breed”
sympathetic nervous system (SNS): “fight, flight or fright”
somatic: general sensory, musculoskeletal movements and reflexes (motor)
autonomic: visceral afferents (sensory input FROM organs) and visceral efferents (motor output TO organs)
What is the role of cranial nerves III, VII, IX and X?
oculomotor nerve (CN III): does a lot of muscle movement which moves our eyes
- but the parasympathetic function of this nerve, does constriction and dilation of the pupil
facial nerve (CN VII): motor fibres to muscles of facial expression
- but the parasympathetic function of this nerve, is for lacrimal glands and mucosa of nose and palate
glossopharyngeal nerve (CN IX): general and special sensory to posterior 1/3 of tongue and motor of pharyngeal muscles
vagus nerve (CN X): does the majority of parasympathetic sensation for the body
What are the 3 types of muscle tissue and their key characteristics?
skeletal muscle: striated muscles w myosin and actin
- under voluntary control
cardiac muscle: found in the heart, striated muscle
- involuntary control
smooth muscle: found in viscera, blood vessels, skin; not striated
- involuntary control
What are the 4 basic properties of muscle?
contractility → contraction (shortening) produces force; skeletal muscles attached to bone via tendons, so contraction (shortening) produces movement
extensibility → can stretch/ lengthen (to an extent) without damage
elasticity → returns to its original length after contracting (shortening) or extension (lengthening)
greatest elasticity is found in smooth muscle
electrical excitability → electrical signals (ie heart) and chemical signals (ie neuromuscular cleft)
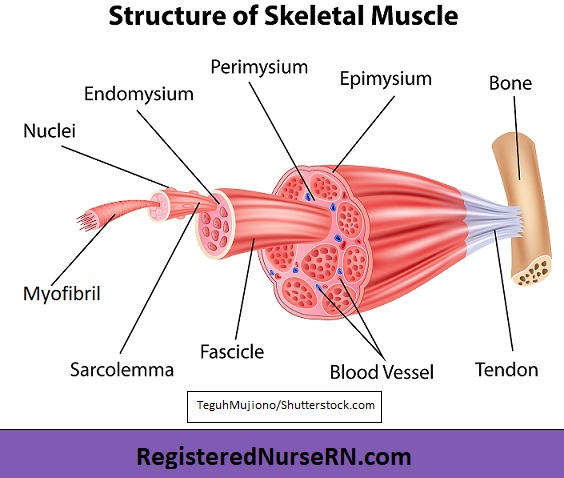
What is the structure of skeletal muscle, from sarcomere to the whole muscle
myofibril (repeating units of sarcomeres), come together to form a muscle fibre
muscle fibre: muscle cell, bundles of myofibrils
- wrapped in perimysium (fibrous tissue)
group of perimysium becomes a fascicle (bundle of muscle fibres)
fascicles grouped together within an epimysium becomes a muscle
muscle is attached to a tendon (anchors muscle to bone)
Differentiate between the following types of muscle contraction: phasic, concentric and eccentric contraction.
phasic contraction: muscle contracts but does not shorten (no movement)
concentric contraction: muscle shortens (myosin contracts) during contraction (ie curling biceps w weights)
eccentric contraction: muscle lengthens (myosin lengthens) during contraction (ie placing a weight down after curling biceps)
Define the roles of agonists, antagonists and synergists in muscle movement
agonists: primary driver of movement (concentric)
antagonists: controls, slows or resists the antagonist (eccentric)
synergist: additional muscles that assist the agonist (concentric)
What are the 3 grades of muscle strains?
grade 1: stretching or slight tearing of a tendon
- usually rest will heal this effectively
grade 2: incomplete tear; when muscle heals won’t heal super well as scar tissue goes over the tear
grade 3: complete tear of the muscle belly
- doesn’t necessarily always require surgery
sTrain= tendons, sPrains= ligaments
What is the PRICE protocol
P → protection
R → rest
I → ice
C → compression
E → elevate
and in the grade 3 sprains, SURGERY!! but grade 3 strains may not require surgery
sTrain= tendons, sPrains= ligaments
What are the functions of the musculoskeletal system?
skeletal movement
maintaining posture and position
opening and closing of orifices
maintaining of homeostasis (burning fat and carbs during exercise or for body heat)
Describe the different types of bone fractures
epiphysial fracture: fracture that occurs right at the epiphysial plate
- more common in younger patients
spiral fracture: twisting foot → fracture is due to rotational movement
- more common in younger and mature adult patients
depressed fracture: whacked in the head w a hammer, occur on bones that are flatter or rounded (punching in a piece of bone)
- more common in mature adult patients
compression fracture: pressure compressed through the vertebrae
What are the main types of joints?
fibrous joints:
syndesmosis joints: thick connective tissue between two bones so no movement occurs (found in femur bone)
suture joints: at birth, we have a squishy skull, and as we grow they slowly fuse together
gomphosis: connective tissue between teeth and jaw bones (gums) which prevents teeth from coming out
cartilaginous joints:
symphysis: fibrocartilage, some movement that can occur within the cervical spine to allow some movement
synchondrosis: hyaline cartilage, sinking of bone into cartilage
Explain the classification of synovial joints based on their axes of movement
bursae, allows for things to roll over one another
synovial sheaths: allow for fine movement
- classification of synovial joints
uniaxial joints: only move in one axis
- ie pivot joints (neck and head), hinge joints (fingers)
biaxial joints: can move in 2 axes
- planar (gliding), saddle joint (in thumb), condyloid joint
multiaxial joints: can move in multiple axes
- ball and socket joint (shoulder)
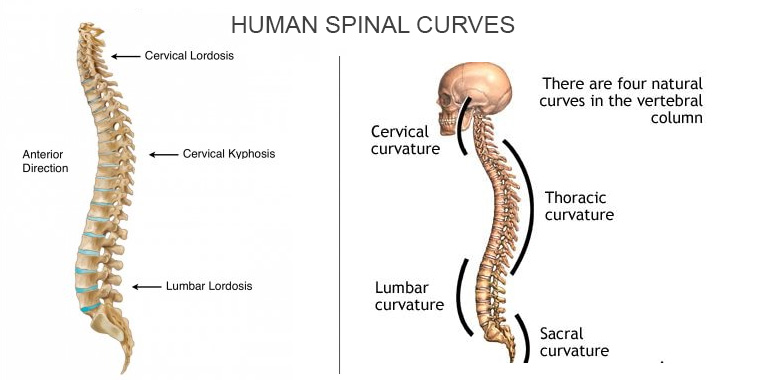
Describe the regions and curves of the spinal column
cervical (7) → up in the neck
thoracic (12) → in the thorax
lumbar (5) → in the abdomen
lumbar lordosis: opposite concave structure to keep our structure up (C shape)
thoracic kyphosis: allows us hold our lungs upright (opposite C shape)
cervical lordosis: allow to keep our head in balance (opposite shape)
between them, we have zygapophyseal joints (synovial), allow the movement of the trunk
Describe the features between the atlas, axis, sacrum and coccyx
atlas: C1, first vertebral piece, so articulates w the skull and thus has superior articular facets, which sits on the atlanto-occipital joint to allow for nodding back and forth
axis: CII, dens (a tooth shape going up) to articulate w C1, this allows for rotational movements of the neck (due to atlanto-axial joints)
sacrum (and coccyx) has sacral promontory (point), where the pelvis starts and goes into the pelvic bowl, sacral hiatus an opening where the nerves that ran through the spine come out
Describe the “dinner fork deformity” and why it occurs
distal radius fracture → dinner-fork deformity (looks like a fork placed upside down) is common, as the larger base of the radius is more prone to breakage
What is the role of the interosseous membrane in the forearm?
interosseous membrane: thick ligament that stabilizes the forearm and forces radius and ulna to work together
helps to share the force applied between the radius and ulna (effective transfer force) so we don’t end up w breaks
Name the 8 carpal bones and their respective rows. What mnemonic can be used to remember their order?
first proximal row of the carpals (thumb to the pinky): scaphoid, lunate, triquetrum, pisiform
second distal row of the carpals (pinky to thumb): hamate, capitate, trapezoid, trapezium
use pneumonic: so long to pinky, here comes the thumb
What carpal bone doesn’t directly articulate w distal ulnar end and what structure fills the space instead?
ulnar distal end doesn’t articulate w the carpal ends, this is where ulnocarpal disc (AKA articular disc) is found
What is the common origin of the superficial anterior forearm muscles? List three of these muscles and their functions
flexor carpi radialis m.: origin: CFO, insertion: 2nd metacarpal, median n innervation
flexor carpi ulnaris m: origin: CFO, insertion: 5th metacarpal, ulnar n innervation
palmaris longus m: origin: CFO, insertion: palmar aponeurosis, median n innervation
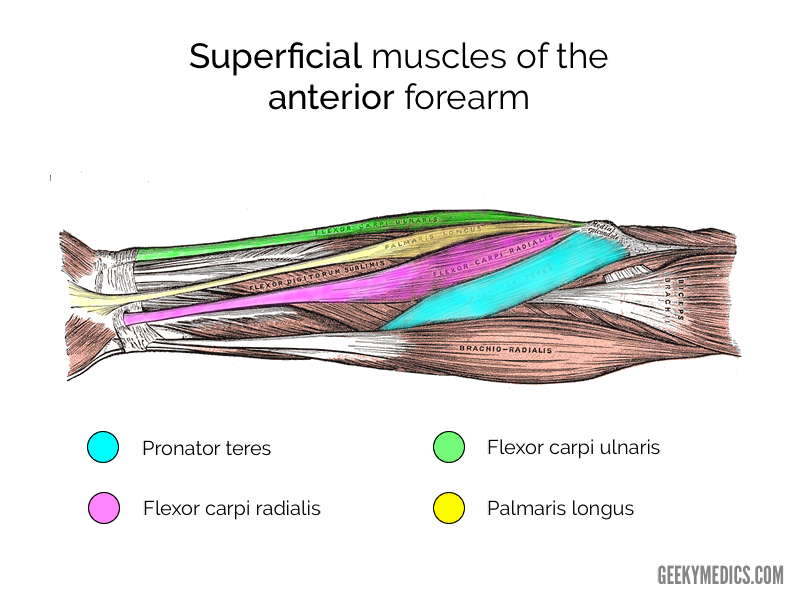
Which nerve innervates most of the anterior forearm muscles? Which nerve innervates all of the posterior forearm muscles?
anterior forearm muscles: median nerve (and some ulnar nerve)
posterior forearm muscles: radial nerve
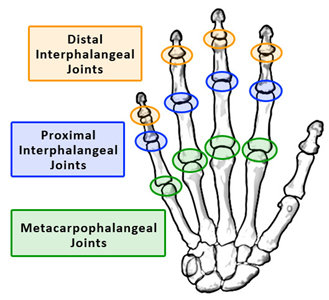
What type of joint is the metacarpophalangeal (MCP) joint? What movements are possible at this joint?
metacarpophalangeal joints are condyloid joints (have a lot more range of motion, first knuckle)
flexion and extension (anterior and posterior movement respectively)
What are the three muscles of the thenar eminence, and what are their actions and their innervation?
thenar eminence: muscles at the base of the thumb (meaty part of your hand) and are made up of the AFO
AFO consists of:
Abductor pollicis brevis m: origin: carpals, insertion: proximal phalanx
flexor pollicis brevis m: origin: carpals, insertion: proximal phalanx
opponens pollicis m: origin: carpals, insertion: 1st metacarpal
innervation from median nerve (recurrent) and deep branch of ulnar nerve
What are the three muscles of the hypothenar eminence, and what are their actions and their innervation?
hypothenar eminence: muscles at the base of the pinky and are made up of the AFO
the AFO consists of:
abductor digiti minimi m: origin: carpals, insertion: proximal phalanx
flexor digiti minimi m: origin: carpals, insertion: proximal phalanx
opponens digiti minimi m: origin: carpals, insertion; 5th metacarpal
all are innervated by the deep branch of the ulnar nerve (C8-T1)
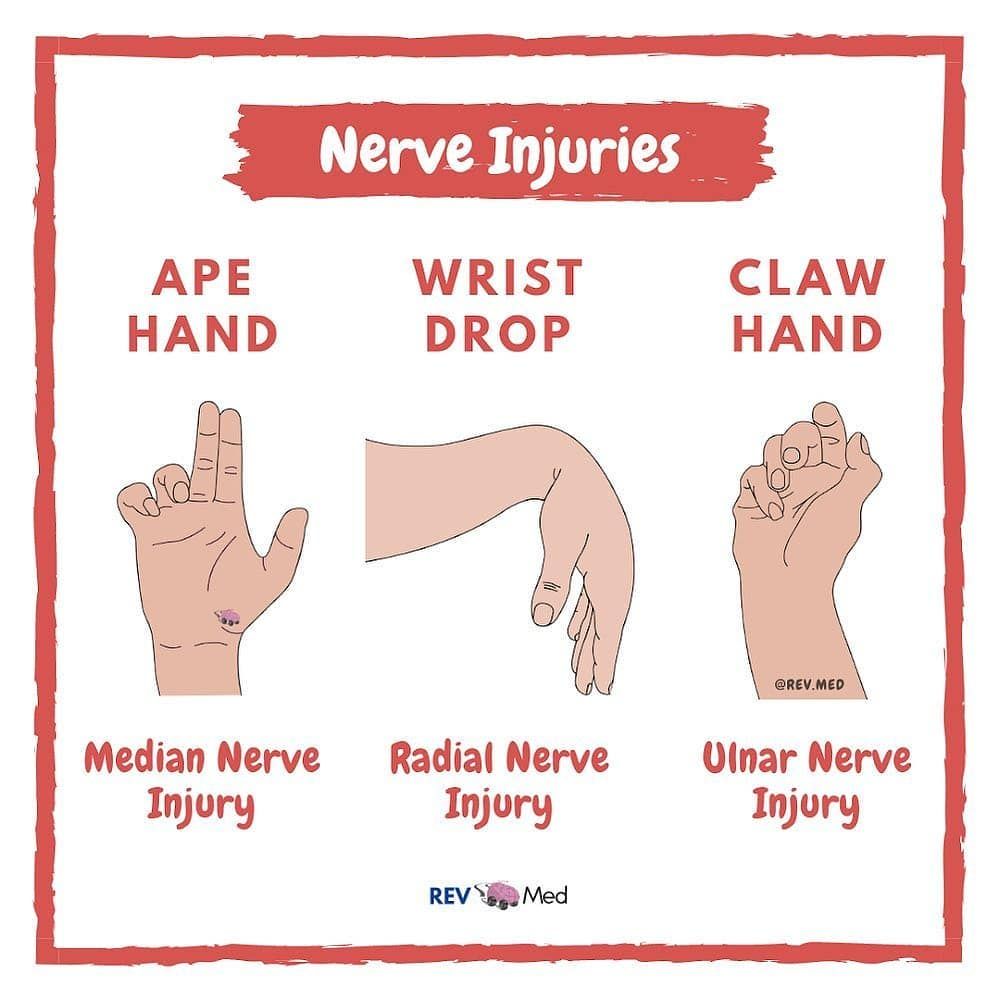
What is claw hand, and what nerve injury is it associated with?
claw hand signifies ulnar nerve injury at the wrist (deep branch ulnar nerve injury)
What is ape hand, and what nerve injury causes it?
injury to the recurrent branch of the median nerve (AKA “million-dollar nerve”) will result in ape hand
The brachial plexus has a specific branching pattern that can be remembered with the mnemonic "Really Thirsty? Drink Cold Beer!"
Roots: C5, C6, C7, C8, T1
Trunks: Roots merge to form superior, middle, and inferior trunks.
Divisions: Each trunk divides into anterior and posterior divisions.
Cords: Divisions combine to form lateral, posterior, and medial cords, named in relation to the axillary artery.
Branches: Cords give rise to the major terminal branches of the brachial plexus, including the musculocutaneous, axillary, radial, median, and ulnar nerves.
Explain the difference between a dermatome and a nerve map.
nerve maps are regions that the nerve is responsible for
dermatomes are based on embryology → arms and legs stretched out the dermatomes they emerged from
we know that nerves can carry through multiple spinal levels, therefore one nerve can affect multiple dermatomes
and multiple different nerves can affect the same dermatome
Describe the location and function of the bicipital aponeurosis
the bicipital aponeurosis is a broad, flat sheet of tendon that originates from the distal tendon of the biceps brachii muscle
It fans out medially and inserts into the deep fascia of the forearm and it serves to protect the underlying structures in the cubital fossa, including the brachial artery and median nerve
Explain the concept of compartment syndrome, including its causes and potential consequences.
Compartment syndrome occurs when pressure within a muscle compartment, bounded by fascia, increases to the point that it compresses blood vessels and nerves.
This can be caused by trauma, bleeding, or swelling within the compartment. If left untreated, compartment syndrome can lead to muscle and nerve damage, and in severe cases, may require a fasciotomy to relieve the pressure.
Differentiate between the functions of the superficial and deep branches of the radial nerve.
The superficial branch of the radial nerve is purely sensory, providing cutaneous innervation to the dorsum of the hand.
In contrast, the deep branch of the radial nerve, which becomes the posterior interosseous nerve, is primarily motor, innervating the muscles of the posterior forearm