~sexuality
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
sexuality
state of mind that represents how individuals feel about themselves, relate to others, establish relationships, and express themselves
as an occupation, it is highly personal and involves one’s sexual values, beliefs, sexual expression, and how one engages in sex, which varies from person to person
intimacy
a close, personal, trusting relationship with another person or group of people, which include giving and receiving support and affection
self-intimacy
related to being aware of and connection to one’s authentic, inner self, and may include our self concept, worth, and compassion for others
sexual pleasure
the physical and/or psychological satisfaction and enjoyment derived from shared or solitary behaviors, as well as partnered or multiple partners; consists of solitary behaviors as well as partnered or multiple partners
solitary: masturbation and fantasy
partnered: kissing, touching, oral sex, penetration (vaginal or anal), spicy sex (sex toys, explicit material, group sex, swinging)
sexual self-view
how you see yourself as a sexual being
sexual preference
sexual expression
gender identity
sexual orientation
self esteem
body image
sexual education
sexual health
fundamental to the overall health and well-being of individuals, couples, and families, and to the social and economic development of communities and countries; when viewed affirmatively, requires a positive ad respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence
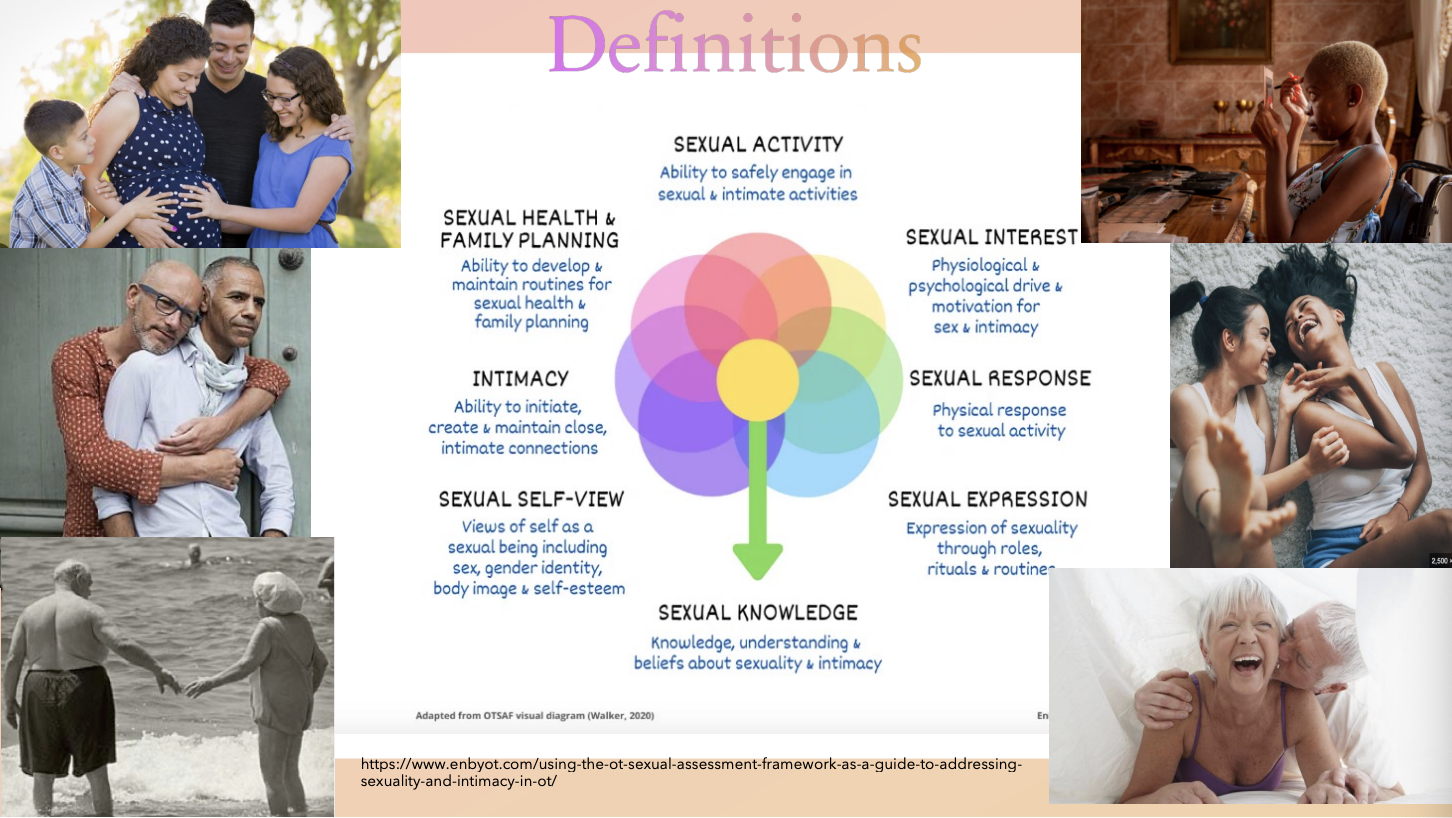
definitions:
sexual activity
sexual interest
sexual response
sexual expression
sexual knowledge
sexual self-view
intimacy
sexual health and family planning
bias
e.g., ageism, homophobia, transphobia, etc.
implicit (unconscious bias)
explicit (conscious bias)
internalized bias
the truth
a significant proportion of older adults are sexually active
wide variety of sexual activities
this proportion decreases with age
this decline is more pronounced among women
why do most healthcare practitioners often ignore sexuality in their practice?
inadequate knowledge
another team member will address it
feeling uncomfortable talking about it
may think it is expressing interest
may be complicated when sexuality differs from own
religious
societal attitudes
myths of sexuality and people with disabilities
limited resources
sexuality and OT
domain: occupations
Occupational Therapy Practice Framework: Domain and Process 4th Edition (AOTA, 2020)
activities of daily living (ADL): sexual activity
“engaging in broad possibilities for sexual expression and experiences with others (e.g., hugging, kissing, foreplay, masturbation, oral sex, intercourse)
health management
social and emotional health promotion and maintenance
“identifying personal strengths and assets, managing emotions, expressing needs effectively, seeking occupations, and social engagement to support health and wellness, developing self-identity, making choices to improve quality of life participation”
personal care device management
“procuring, using, cleaning and maintaining personal care devices, including…contraception and sexual devices”
social participation: intimate partner relationships
“engaging in activities to initiate and maintain a close relationship, including giving and receiving affection and interacting in desired roles; intimate partners may or may not engage in sexual activity”
sexuality is considered an activity of daily living and is part of life, and important to most people
OTP are holistic and consider the person, the activity, and the context
OTP are experts in adaptive equipment and assistive technology
OTs are skilled at activity analysis
therapeutic use of self
but this is a team approach
lessons from OTs who have been successful in addressing sexuality
bringing sexuality out of the closet: what can we learn from OTs who successfully address the area of sexuality in everyday practice
themes & sub-themes
sexuality matters
know your boundaries
person
professional
organizational
just do it
tap into existing skill set
commitment to self-education and practice
seek support and mentoring
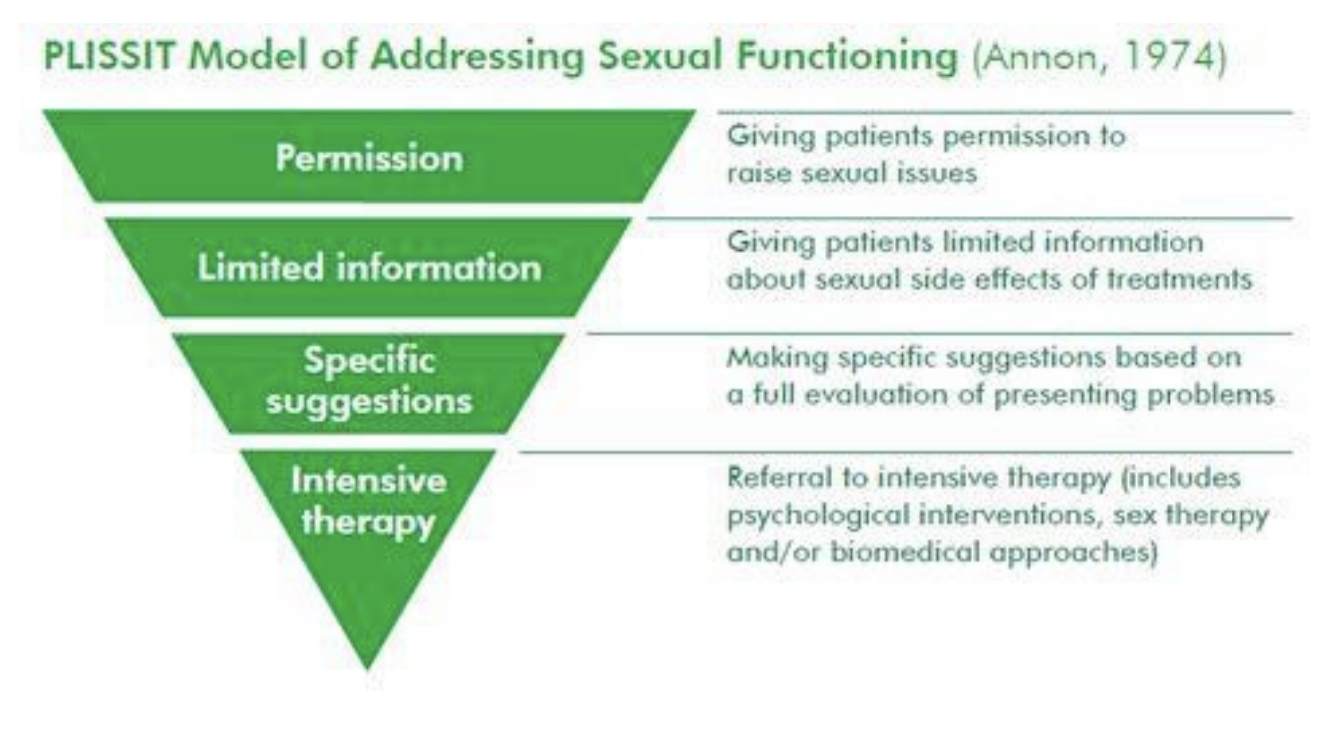
PLISSIT model
4 stage progressive/linear model (kind of a limitation —> EXPLISSIT)
PLISSIT Model Permission (P): permitting patients to raise sexual issues
Limited Information (LI): giving patients limited information about the sexual side effects of treatments
Specific Suggestions (SS): making specific suggestions based on a full evaluation of presenting problems
Intensive Therapy (IT): referral to intensive therapy (includes psychological interventions, sex therapy, and/or biomedical approaches)
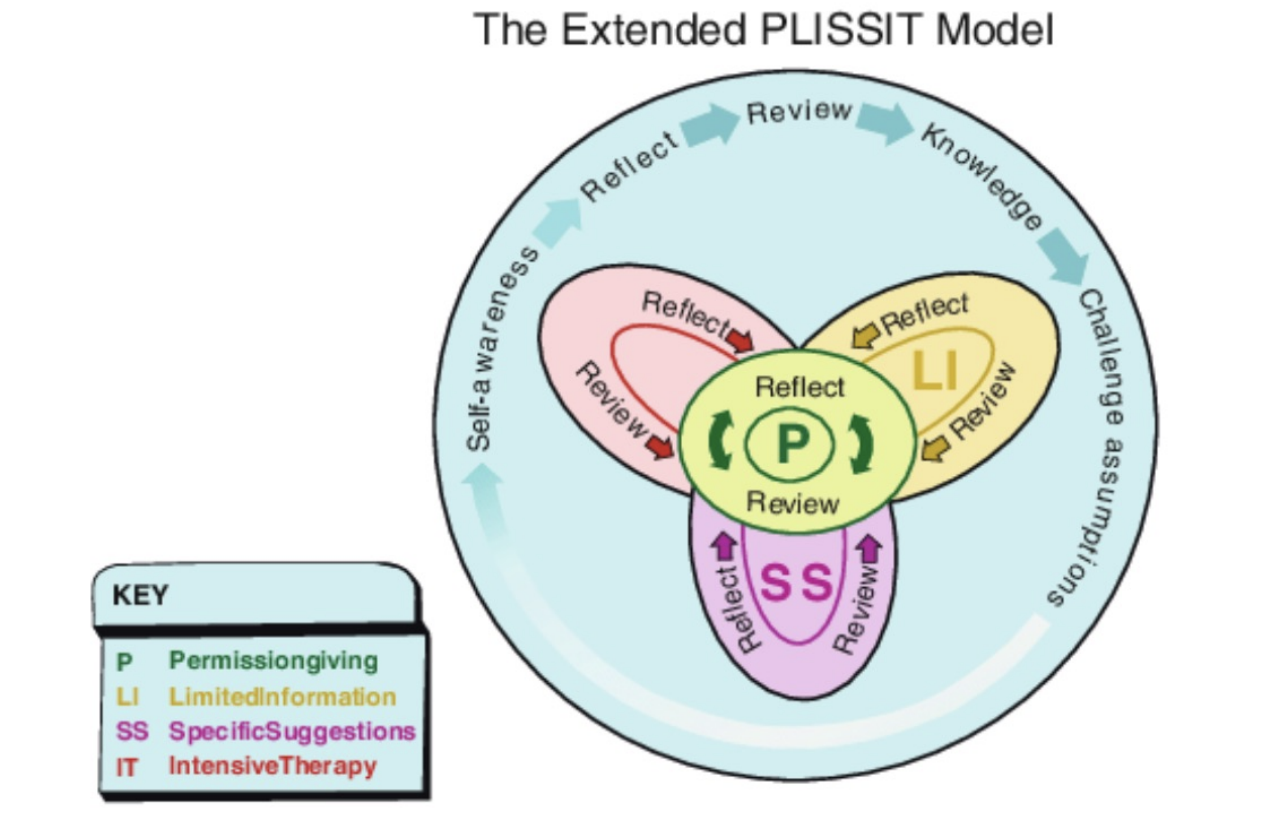
extended PLISSIT model
updated more where it’s less linear and more circular
P: permission giving
LI: limited information
SS: specific suggestions
IT: intensive therapy
recognition model
== specific skills that health practitioners can use to protect and promote sexual health in people with disabilities, thus the HOW this can be achieved
stage 1: recognize the service user as a sexual being
validation/acknowledgement, normalization and affirmation, importance, relevance
“you may have sexual concerns (acknowledgment), may clients do (normalization); it is not an area of expertise of mine (limitations), but I appreciate the importance (affirmation); if you wish, I can speak to my colleague about this”
stage 2: provision of sensitive, permission-giving strategies
invite disclosure, respect privacy
“i find some people also want to talk to me about relationships, or have questions about sex; I am happy to discuss this if you have any concerns”
information leaflets and posters, or pins that would invite questions of sexuality
stage 3: exploration of the sexual problem/concern
this can be with the OT or a specific team member
permission may lead to a referral for exploration by other team members
stage 4: address issues that fit within the team’s expertise and boundaries
analysis of sexual concern, treatment planning, goal setting, and interprofessional work
PT (biomechanical issues that cause discomfort), OT (energy conservation, body image, ADLs related to sexuality, positioning, adaptation, if knowledgeable about sexual toys, creams, cock rings, vibrators, penis pumps, etc.), speech (communication), physicians (medications, surgeries)
stage 5: referral if necessary
fall outside of the disability team’s role, such as intensive therapy, surgeries, and relationship counseling
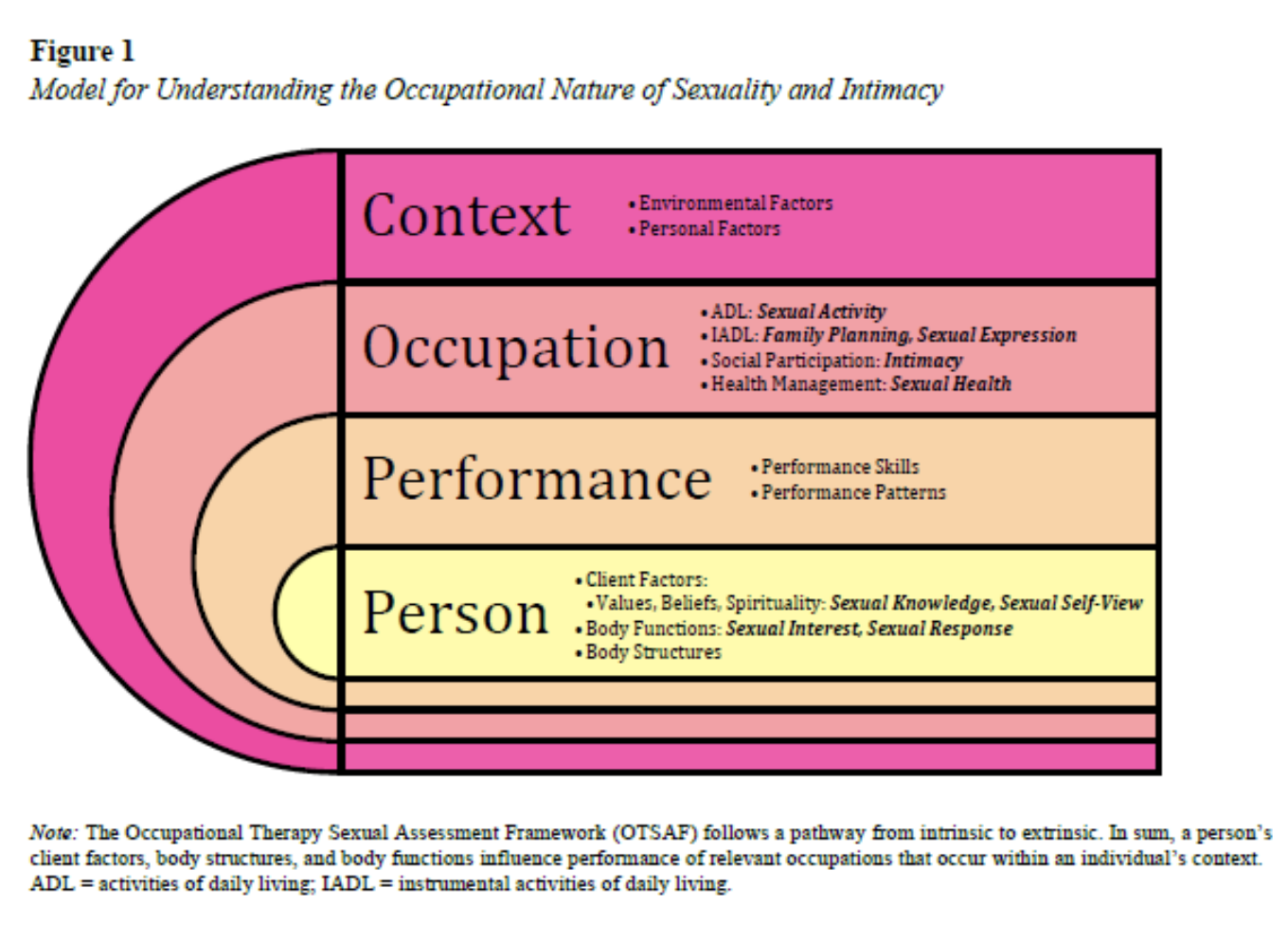
occupational therapy sexual assessment framework (OTSAF)
person
performance
occupation
context
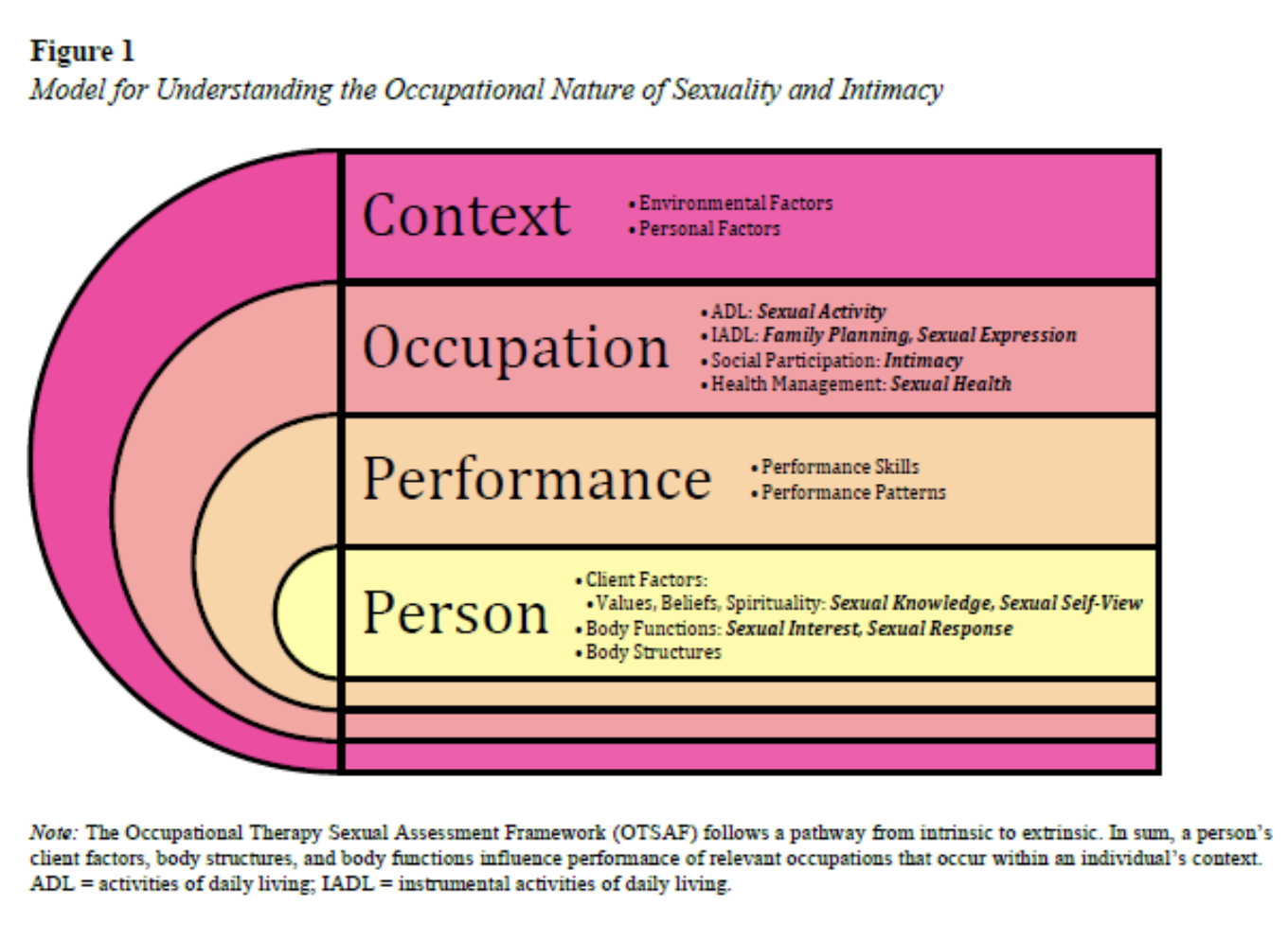
evaluating sexuality and intimacy
OT evaluation
Occupational Profile (sexual history)
person
client factors
values (e.g., sexual self-view, sexual knowledge)
beliefs
spirituality
body functions
body structures
performance
performance skills
motor skills (e.g., grasp, thrust)
socialization (e.g., initiating conversations about sex)
sequencing, initiation
occupation
ADL (e.g., sexual activity)
IADL (e.g., family planning, sexual expression)
social participation (e.g., intimacy)
health management (e.g., sexual health)
context
environmental factors
e.g., privacy in a nursing home, having a single-bed
personal factors
evaluating sexuality and intimacy:
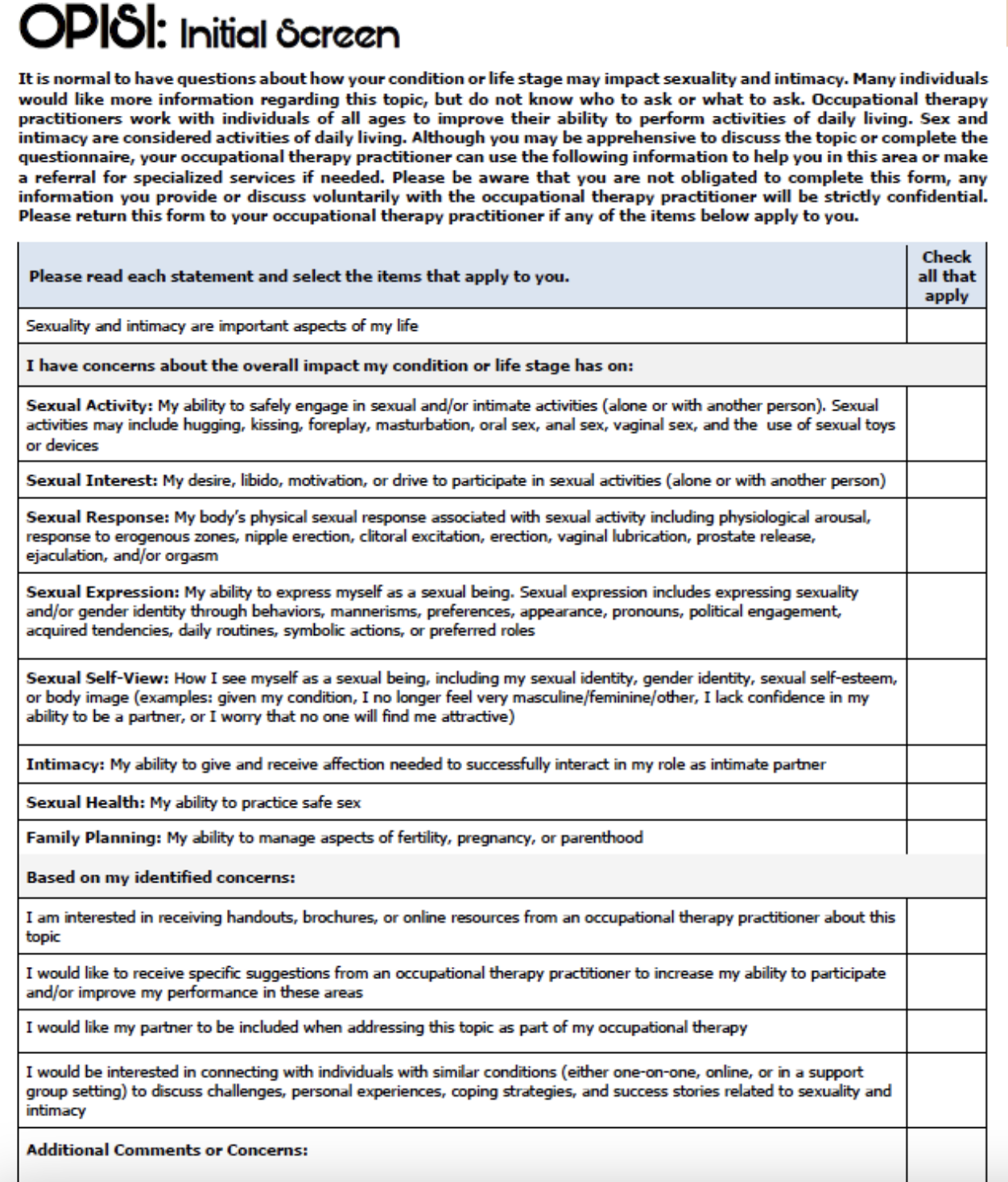
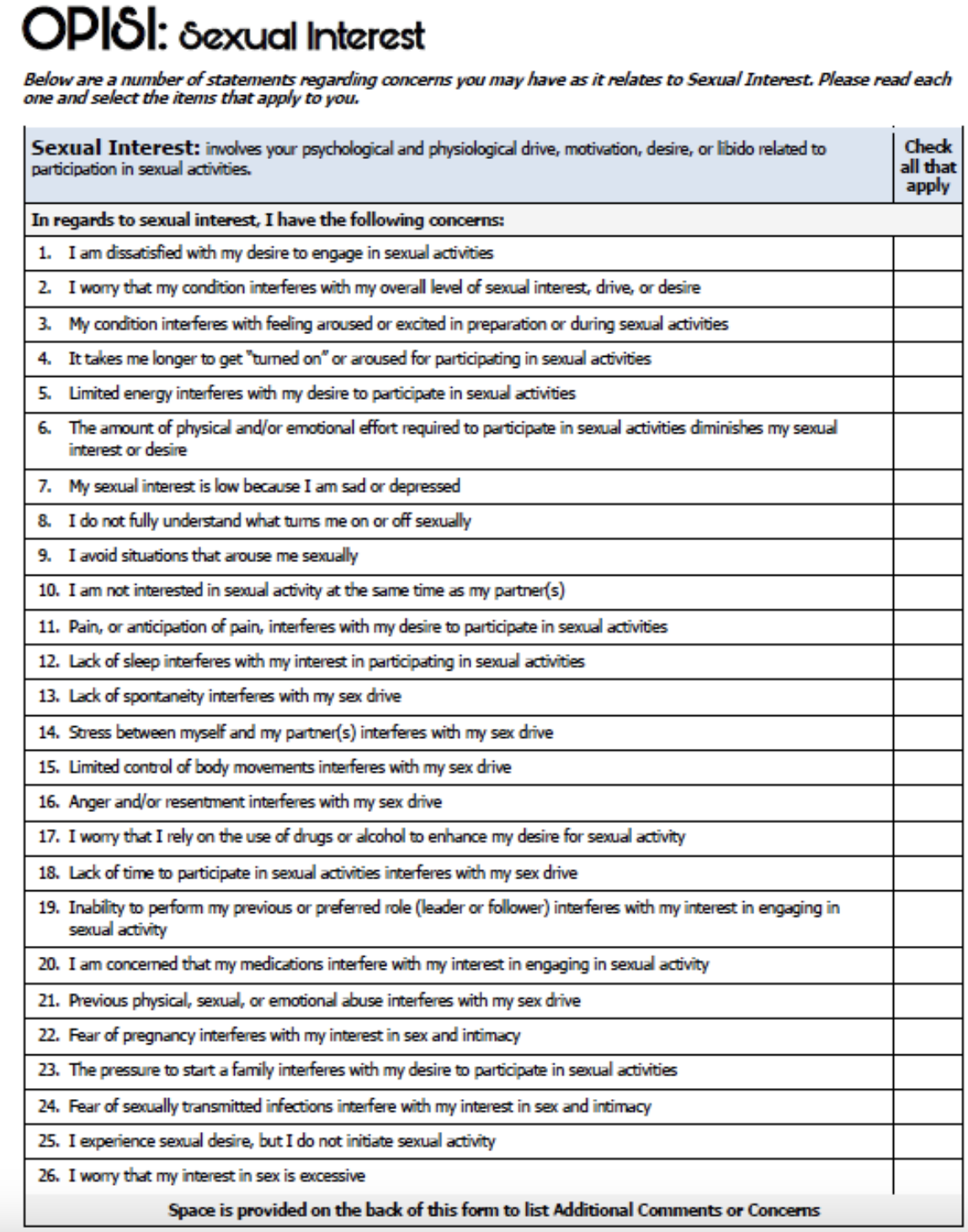
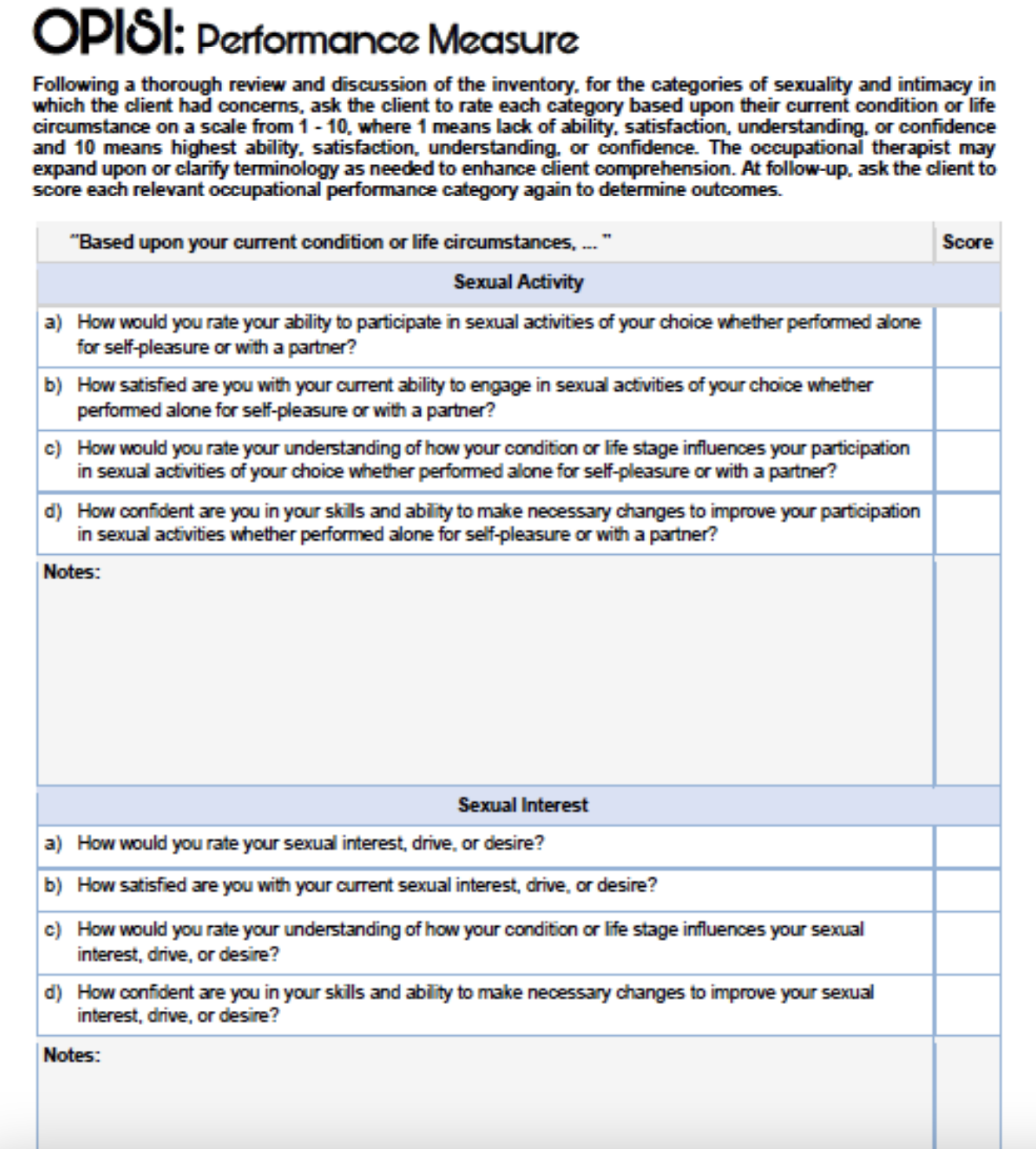
Occupational Performance Inventory of Sexuality and Intimacy (OPSI)
developed to define the occupational nature of sexuality and intimacy
created to be a theoretical occupation-based screen, an in-depth self-assessment, and a performance measure to address sexuality and intimacy
initial screen
in-depth self-assessment (covers sexual activity, sexual interest, sexual response, sexual expression, sexual self-review, intimacy, and sexual health and family planning)
performance measure
scoring form
goals
referral
OPISI: Initial screen
OPISI: In depth assessment
OPISI: Performance Measure
Prevalence of Sexual Activity
Decreases with age
Is lower among women
Is lower among those with poorer health status
Remains significant in the elderly
issues and challenges
stereotypical beliefs and myths
demographics
psychological
cognitive changes
lack of privacy
physical concerns
age related changes in sexual function
men vs women
gradual changes
changes in hormone levels
men:
testosterone levels decrease very little
decreased sperm production and ejaculatory force
prostate enlargement
decreased desire or arousal
women:
vaginal dryness, reduced lubrication
changes in shape and in muscle tone
thinning of the vaginal wall
reduced size of the clitoris
decreased desire and arousal
age related changes in sexual function vs sexual dysfunction
DSM-5: sexual dysfunction:
female sexual arousal/interest disorder
persistent decrease in sexual interest or arousal that may include reduced desire, fewer sexual thoughts, or decreased physical arousal; in older adults, this can be influenced by hormonal changes (e.g., menopause), chronic illness, medications, fatigue, or emotional factors
male hypoactive sexual desire disorder
long-term reduction in sexual desire that causes distress or concern; in older men, this may be related to normal aging, low testosterone, medical conditions (e.g., heart disease or diabetes), medications, depression, or relationship changes
female orgasmic disorder
difficulty achieving orgasm, or experiencing significantly reduced intensity of orgasm, despite adequate stimulation; for older women, this may be affected by changes in blood flow, nerve sensitivity, pelvic floor strength, medications, or comfort with sexual activity
genito-pelvic pain/penetration disorder
ongoing pain, fear, or difficulty with vaginal penetration; in later life, this is often associated with vaginal dryness, thinning of vaginal tissues after menopause, pelvic floor muscle tightness, or past painful experiences
erectile disorder
difficulty achieving or maintaining an erection sufficient for sexual activity; this becomes more common with age and may be linked to cardiovascular health, diabetes, nerve changes, medications, or stress
premature (early) ejaculation
ejaculation that occurs sooner than desired, often with minimal stimulation, and causes distress; in older adults, it may be influenced by anxiety, changes in sexual routines, or health conditions, and can often be improved with education and behavioral strategies
delayed ejaculation
marked delay or inability to ejaculate despite adequate stimulation; in older men, this can be related to medication side effects (e.g., especially antidepressants), nerve changes, chronic illness, or psychological factors
for each diagnosis, symptoms must…
(A) be experienced 75% to 100% of the time,
(B) last for at least 6 months, and
(C) have caused significant distress; disorder of sexual desire/interest
effects of disease on sexuality
arthritic
chronic pain
diabetes
heart disease
stroke
alcohol and drug use
pulmonary disease
incontinence
depression
anxiety
heath attack
medications
cancer
sexuality and cardiovascular disease
myths:
sex is no longer permissible after a cardiac event
just talk to a doctor to make sure you’re being safe
person with heart disease will experience chest pain during sexual activity
risk factors
MET levels guide for sexual activity
prior to resuming sexual activities:
psychological barriers
pain
decreased libido
erectile dysfunction
older adults and sexually transmitted infections
older adults may be at an increased risk for STIs
lack of screening
decline in immune function
decreased usage of protection
age-related physiologic and anatomic changes
prevalence of HIV in older adults
over half of people with diagnosed HIV were aged 50 and older; compared to all people with HIV, people aged 55 and older have higher viral suppression rates

why is the number of older people with HIV growing?
treatment of ED
large population of divorced/widowed and newly dating
lack of knowledge of HIV
programs do not target or address risk factors for older adults
afraid to discuss sex lives
may be doing unsafe practices in hiding
risk factors
sexuality concerns with LGBTQ+ older adults
under-reporting to health professionals
often do not disclose their sexual histories or practices
need for health care professionals to be culturally and clinically sensitive and competent when taking medical, social, and sexual histories
strategies and intervention for older adults
open communication
education and prevention
privacy
expand the definition of sex
manage expectation
stay sexually active
if you don’t know, just say, and then look for resources and the answers
direct OT interventions
adaptive sexual devices, lubrication, vibrators, masturbation
positions, positioning devices, time of day
decrease
other erroneous zones, body mapping, body awareness
ADLs, IADLs to prepare
self-image concerns (referral to psych)
energy conservation and sex simplification
bowel and bladder care
fine motor, oral motor interventions
pain management (referral to MD)
pharmacological intervention (referral to MD)
surgical interventions (referral to MD)
medication changes for depression/anxiety (referral to psychiatrist)
sex therapy (referral to sex therapist)
reproductive health access (referral to social work)
screening and treatment of STIs, safe sexual practices (refer to nurses or MD)