ANAT 3001 reproductive system (internal pelvic anatomy)
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
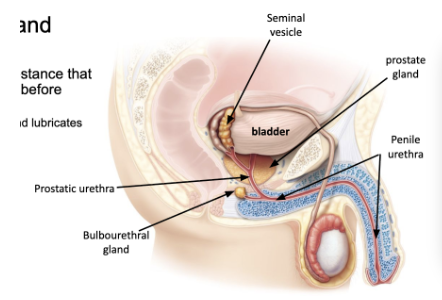
male pelvic structures
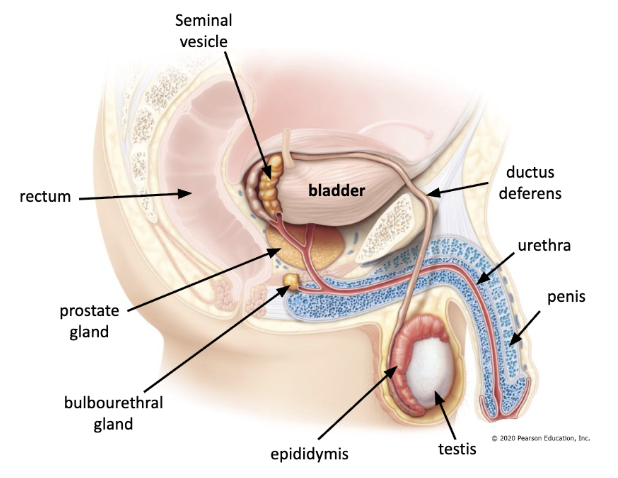
ductus deferens and seminal vesicle
ductus (vas) deferens enters pelvic cavity through inguinal canal
ductus deferens joined by seminal vesicle to create ejaculatory duct within prostate gland
seminal vesicles release into semen
fructose - energy supply for sperm cells
prostaglandins - promote dilation of cervical canal and contraction of uterus
clotting proteins - coagulates semen after ejaculation
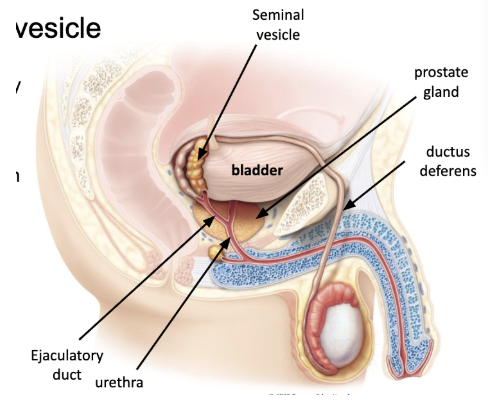
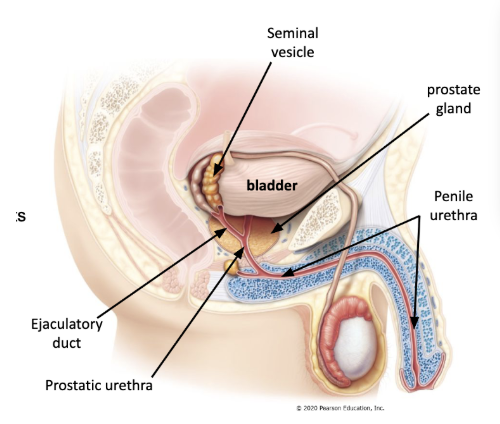
prostate gland
prostate gland located inferior to bladder
ejaculatory duct joins the urethra within the prostate gland
seminalplasmin - antibiotic to combat urinary tract infections
prostate specific antigen (PSA) - liquefies semen after ejaculation
urethra
carries urine and semen to exit the penis
has specific regions
prostatic urethra - through prostate, joined by ejaculatory ducts
penile (spongy) urethra - through penis
bulbourethral gland
produces mucus like substance that conditions penile urethra before ejaculation
neutralizes acidic urine and lubricates urethra
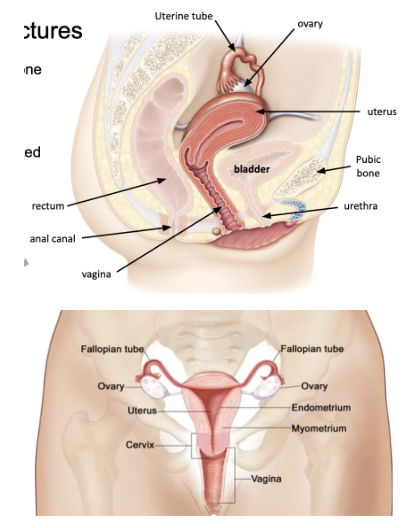
female pelvic structures
bladder sits behind pubic bone
vagina and uterus between bladder and rectum
uterus arches anteriorly
uterine (fallopian) tube located anterior to ovary
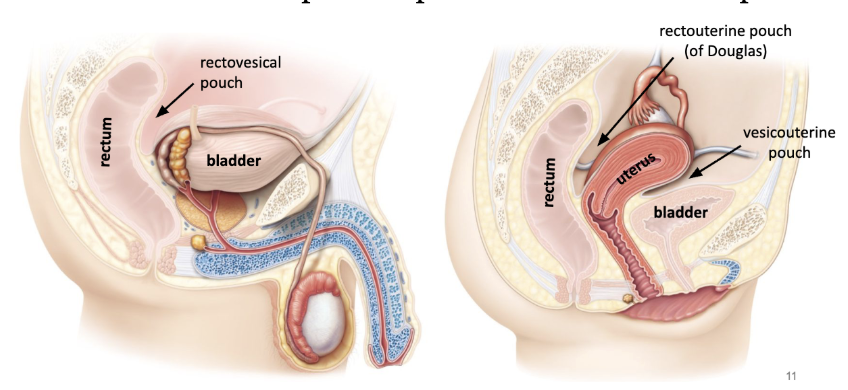
pouches in the pelvis
peritoneum drapes over pelvic structures to form pouches
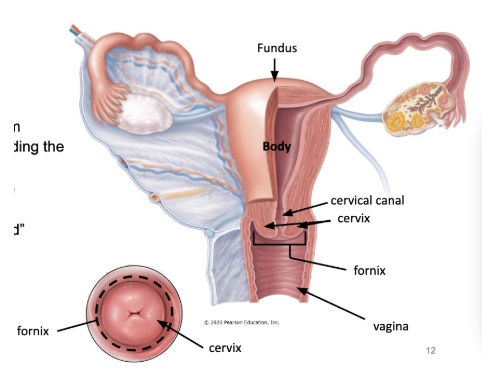
vagina and uterus
vagina - muscular canal
stratified squamous epithelium
fornix - circular area surrounding the cervix
uterus - hollow organ where embryo/fetus develops
cervix - inferior “donut shaped” projection into vaginal canal
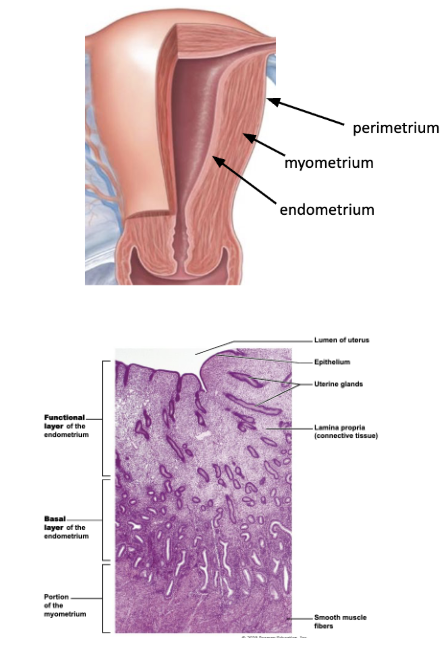
uterine wall - 3 layers
perimetrium
outer serous membrane (peritoneum)
myometrium
thick muscular layer
produces contractions during childbirth
endometrium
mucosal lining of uterine cavity, simple columnar epithelium with connective tissue
highly vascularized
functional layer - thick inner layer, shed during menstruation
basal layer - thinner, not shed, forms new functional layer
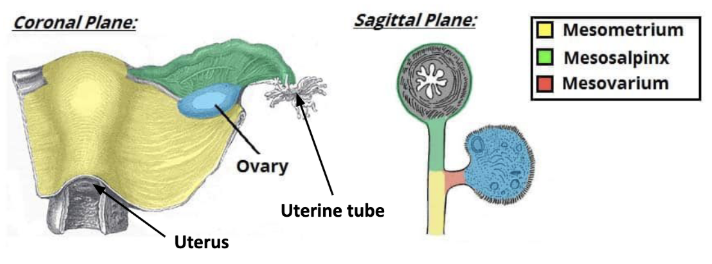
uterus and adnexa
adnexa - 3 structures that hand from the uterus
uterine (fallopian tube
transports oocytes from ovaries to uterine cavity
fimbriae - finger like projections that draw oocyte
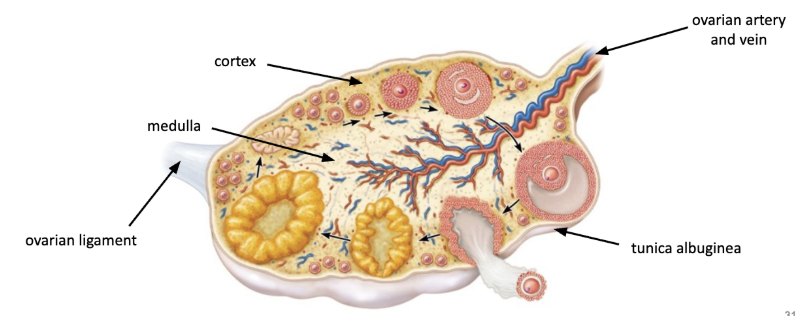
ovary and ovarian ligament
ovaries - gonads, produce gametes (oocytes)
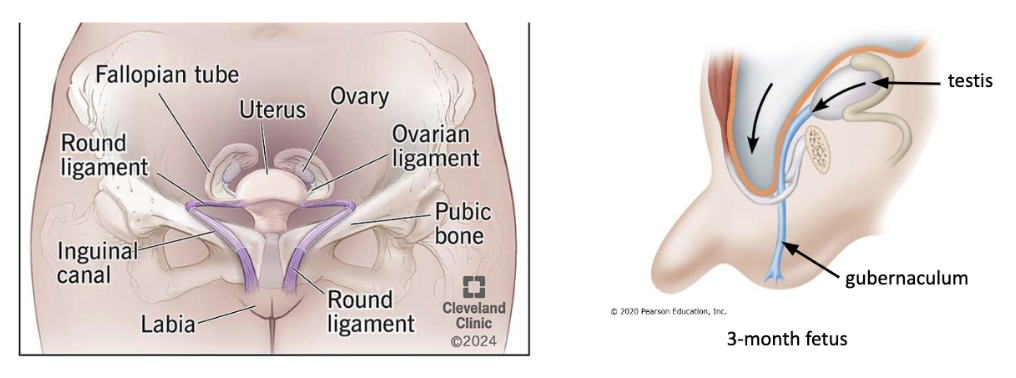
round ligament
travels anteriorly through inguinal canal on each side and attach to labia majori
positional support and anchor for uterus
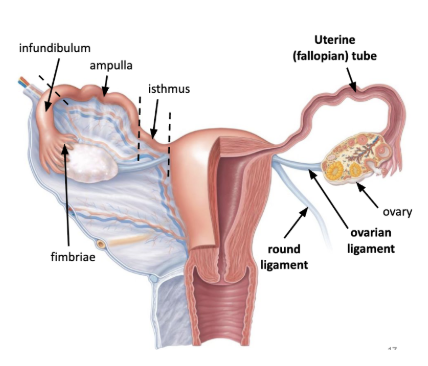
homologous to the gubernaculum…
broad ligament
draping of peritoneum over the uterus and adnexa
has three parts
mesometrium
mesosalpinx
mesovarium
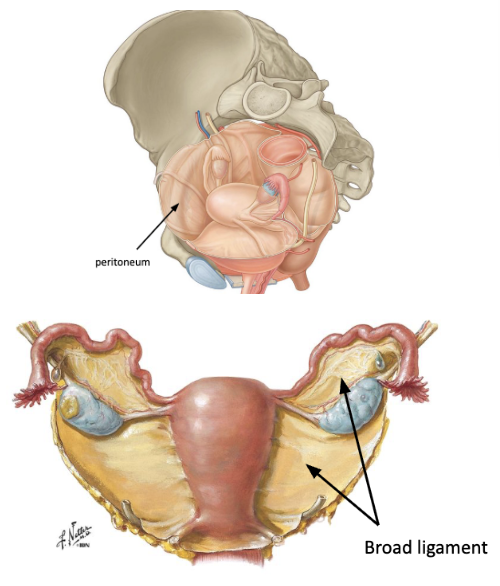
3 parts of broad ligament
mesometrium - covers uterus
mesosalpinx - covers uterine tube
mesovarium - covers ovarian ligament and ovaries
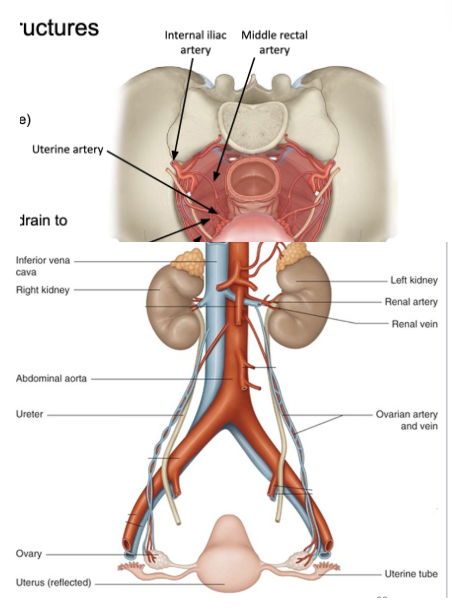
blood supply to pelvic structures
internal iliac artery gives off many branches to supply blood to pelvic structures
vesical artery - to bladder (and prostates)
uterine artery - to uterus
vaginal artery - to vagina
middle rectal artery - to rectum
each has corresponding veins that drain into the IVC
ovarian (gonadal) artery - from abdominal aorta, supply ovaries
ovarian (gonadal) vein
left joins left renal vein
right joins IVC
similar pattern to testicular arteries and veins but stay inside pelvis
when ovarian arteries and veins covered in peritoneum, called suspensory ligament
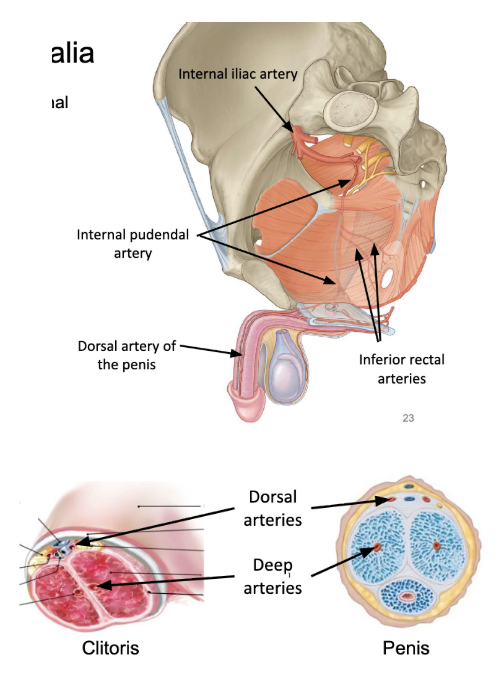
blood supply to external genitalia
internal pudendal artery - branch from internal iliac artery
main artery of perineum and external genitalia, also rectum
inferior rectal arteries
dorsal arteries of the penis/clitoris
deep arteries of the penis/clitoris
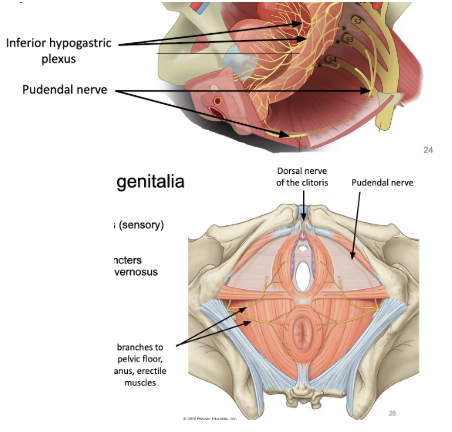
innervation to pelvic structures
inferior hypogastric plexus - visceral sensory and motor innervation to pelvic structures and external genitalia
sympathetics via sympathetic trunk
parasympathetics via pelvic splanchnic nerves (S2-S4)
pudendal nerve - from S2-S4, innervation of external genitalia
dorsal nerve of clitoris/penis (sensory)
somatic motor branches to
muscles of pelvic floor
external anal/urethral sphincters
bulbospongiousis, ischiocavernosus
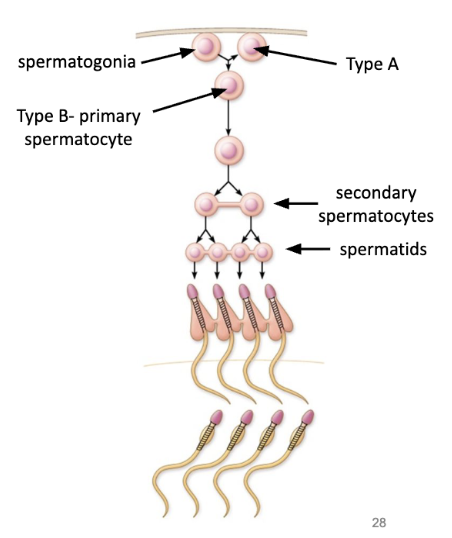
spermatogenesis
formation of sperm within testes
spermatogonia (stem cells) differentiate into sperm, takes ~75 days
occurs in seminiferous tubules of testes
produce 400 million sperm per day
starts at puberty and continues until death (declines with old age)
3 stages
stage 1
formation of spermatocytes
spermatogonia (stem cells) located in outer region of seminiferous tubules
spermatogonia undergo continuous mitosis (cell division) that results in 2 daughter cells:
type A - remain in outer region to maintain germ cell line
type B - move toward lemur as primary spermatocyte
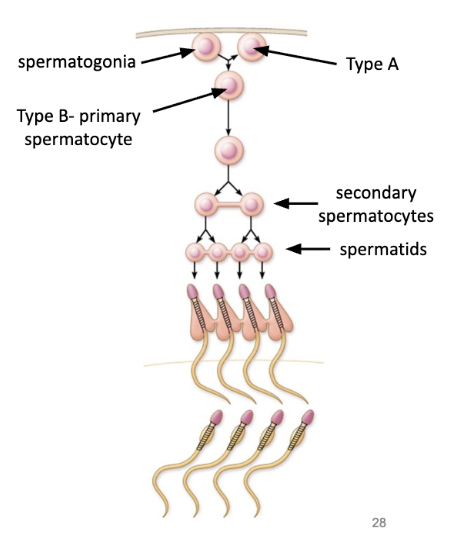
stage 2
meiosis
spermatocytes undergo meiosis
a process of 2 subsequent divisions
1 diploid cell → 4 haploid cells (spermatids)
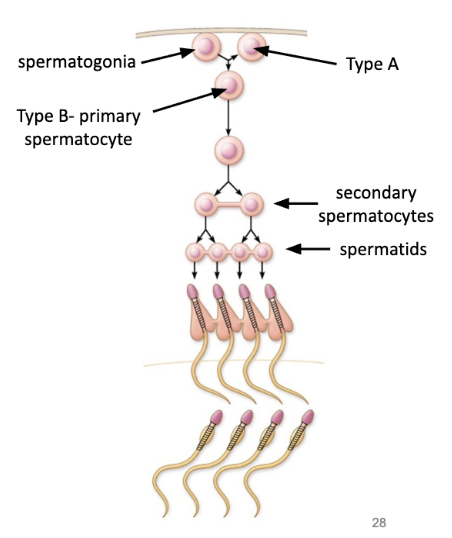
stage 3
spermiogenesis
spermatids differentiate into sperm
sperm have 3 parts
head - with nucleus
midpiece - with mitochondria to produce energy for tail
tail - flagellum that whips around to proper sperm
sperm detaches from epithelium of seminiferous tubule and enters lumen
supporting cells - interstitial (leydig) cells
located in connective tissue between seminiferous tubules
produce androgens (testosterone)
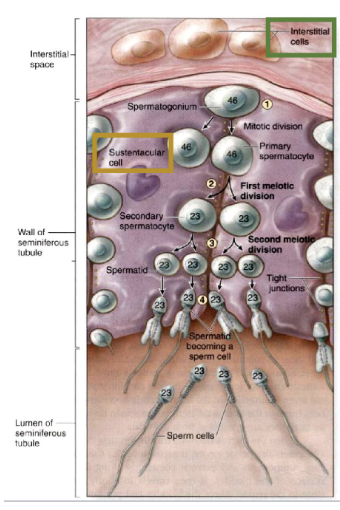
supporting cells - sustentacular (sertoli) cells
with seminiferous tubules
sperm cells pass towards the lumen between sustentacular cells
nutritional support of sperm cells
produce inhibin (prevent spermatogenesis when sperm count is too high)
ovaries
produce oocytes (oogenesis) in cortex
produce estrogen and progesterone (sex hormones)
menstrual cycle
approximately monthly hormone induces cycling of the ovary (ovarian cycle) and uterus (uterine cycle)
ovarian cycle - stimulates development of ovarian follicles and the production of oocytes
uterine cycle - prepares the uterine wall for implantation and nourishment of a fertilized ovum
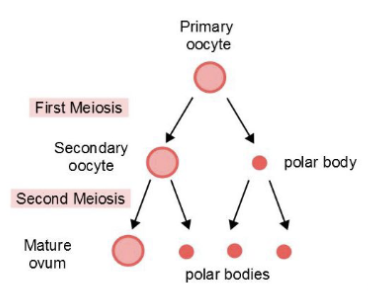
oogenesis
formation and development of oocytes
starts in ovary, finishes in uterine tube
1 oocyte → 1 ovum + 2-3 polar bodies
ovum retains most of cytoplasm, polar bodies have primarily DNA and degenerate
takes many years to complete (many steps)
spermatogenesis
formation and development of sperm
starts in testes, finishes in epididymis
1 spermatocyte → 4 sperm cells
occurs continuously, takes ~75 days

process of oogenesis
process that begins before birth and stalls until puberty
in fetus
oogonium (stem cell) → primary oocyte
primary oocytes stalls before first division until puberty
after puberty during ovarian cycle
primary oocyte → secondary oocyte
secondary oocyte arrests before second division until after ovulation, and will only produce an ovum when sperm attaches to oocyte
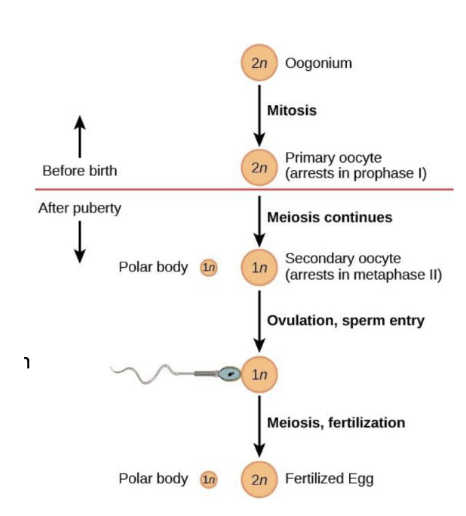
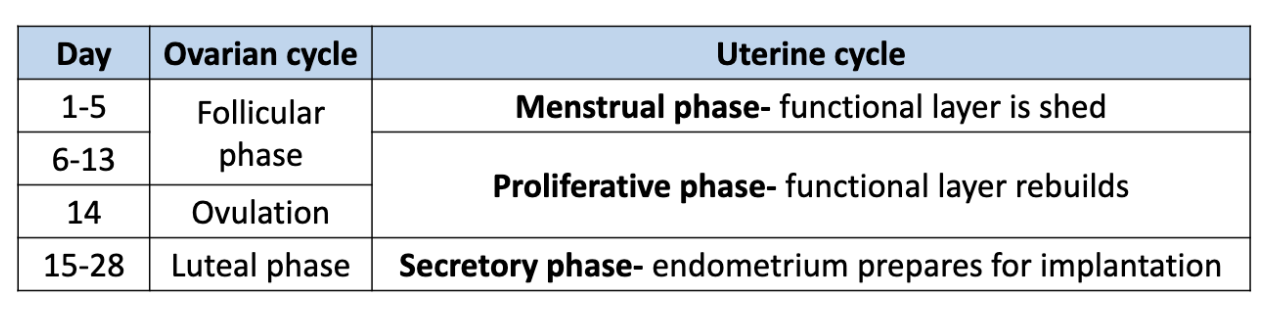
ovarian cycle
3 phases
follicular phase (~day 1-13)
ovulation (~on day 14)
luteal phase (on ~day 15-28)
follicular phase
(~day 1-13)
about 1.5 million primordial follicles (w/primary oocytes) present at birth, about 300-400 thousand at puberty
follicle stimulating hormone (FSH) - stimulates release of 6-12 primordial follicles
one primordial follicle continues to develop into tertiary follicle
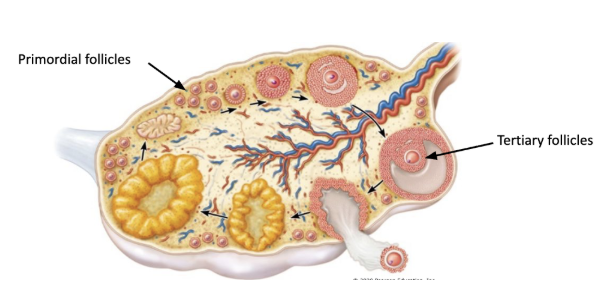
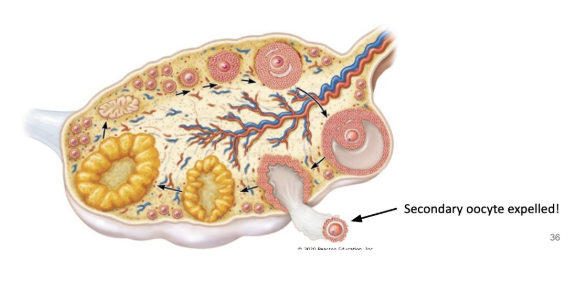
ovulation
(~on day 14)
mature follicle ruptures and releases secondary oocyte from the one of the persons two ovaries
secondary oocyte is swept into the uterine tube by the fimbriae
secondary oocyte does not complete secondary division unless sperm attaches
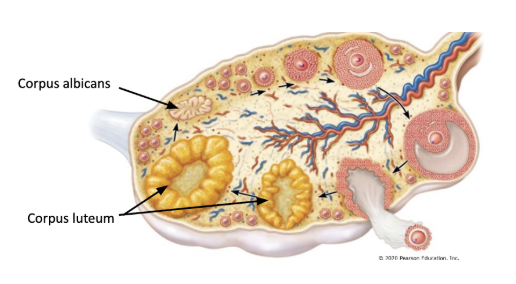
luteal phase
(on ~day 15-28)
after ovulation, remaining part of the follicle collapses, called corpus luteum
corpus luteum persists as an endocrine gland, secretes estrogen and progesterone
stimulate build up of endometrium in preparation for pregnancy
if there is no implantation, corpus luteum dies after 2 weeks and becomes scar like tissue (corpus albicans)
menstrual cycle (review)
uterine phases are closely coordinated with phases of ovarian cycle
at puberty, pituitary gland releases follicle stimulating hormone (FSH) and luteinizing hormone (LH) to initiate ovarian cycle
FSH and LH initiate changes in the ovaries during oogenesis
FSH stimulates growth of primordial follicles
cells in follicles release estrogen to rebuild functional layer of endometrium
LH increases fluid and pressure in tertiary follicle until rupture (ovulation)
corpus luteum releases estrogen and progesterone to prepare endometrium for implantation
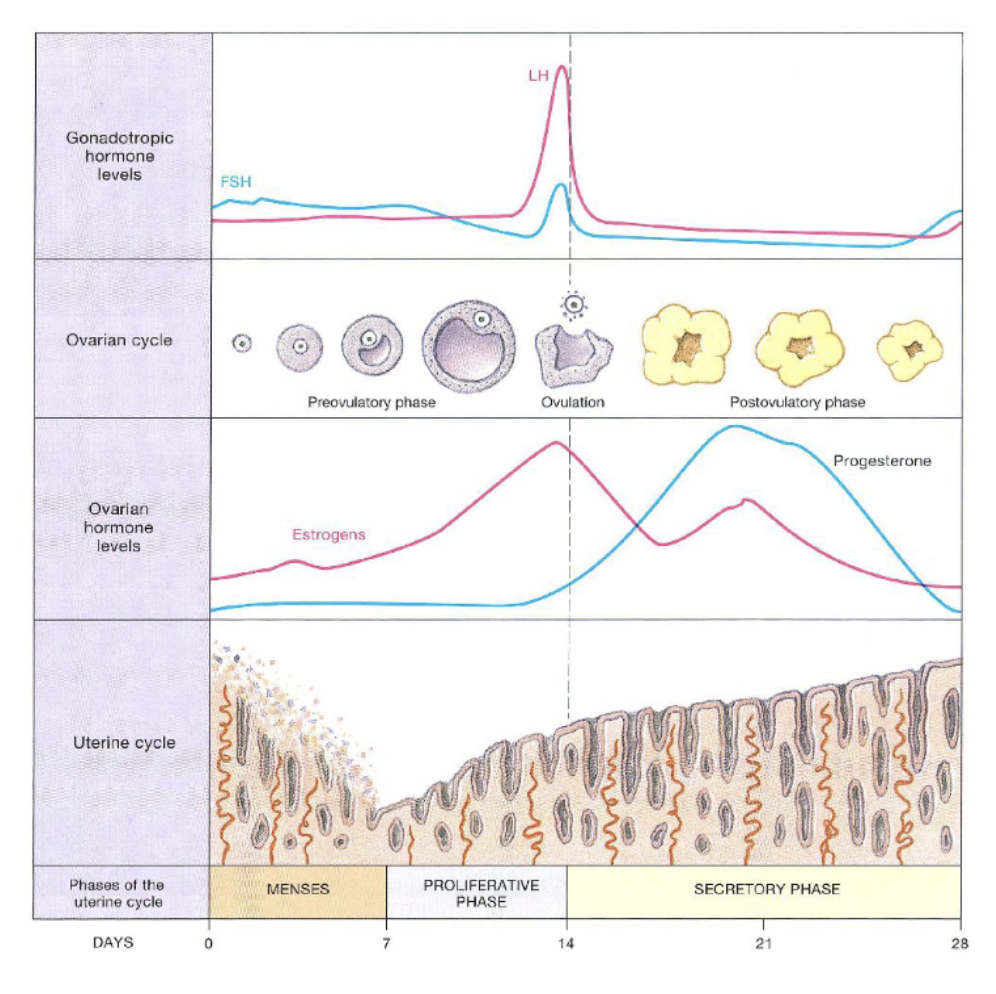
uterine cycle coordination
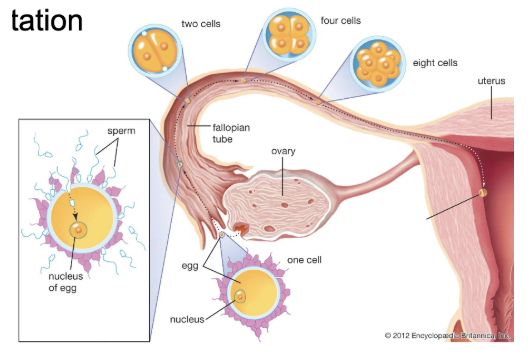
fertilization
secondary oocyte swept into uterine tube by fimbriae
sperm cells deposited at the cervix travel through uterus to uterine tube
oocyte can remain in reproductive tract for 24 hours, sperm for 4 days
fertilization - one sperm cell fuses with oocyte to form new diploid cell
occurs in ampulla typically
fertilized ovum (zygote) moves toward uterine cavity and divides
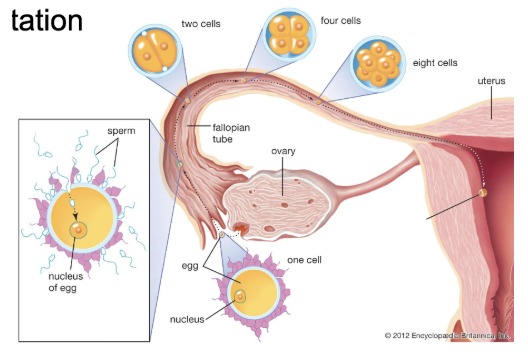
implantation
after 6 days, zygote implants in uterine wall (pregnancy)
corpus luteum keeps producing progesterone to stabilize uterine lining (placenta at 3 months)
if no implantation, menstruation occurs
corpus luteum regresses, stops producing progesterone and estrogen