[Exam 2: 1 of 2] CVD / HLD / HTN
1/269
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
270 Terms
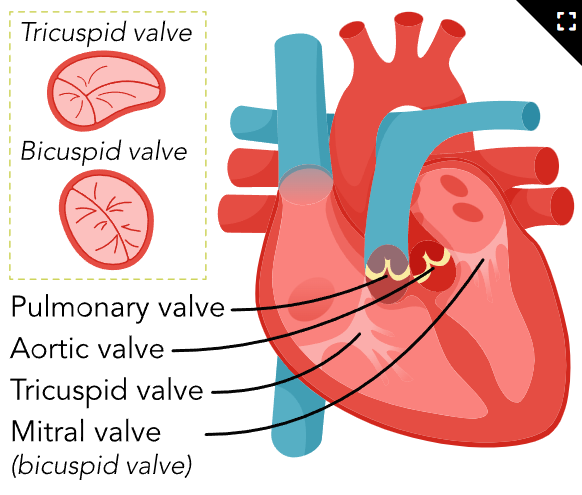
Heart Chambers and Valves (Image)
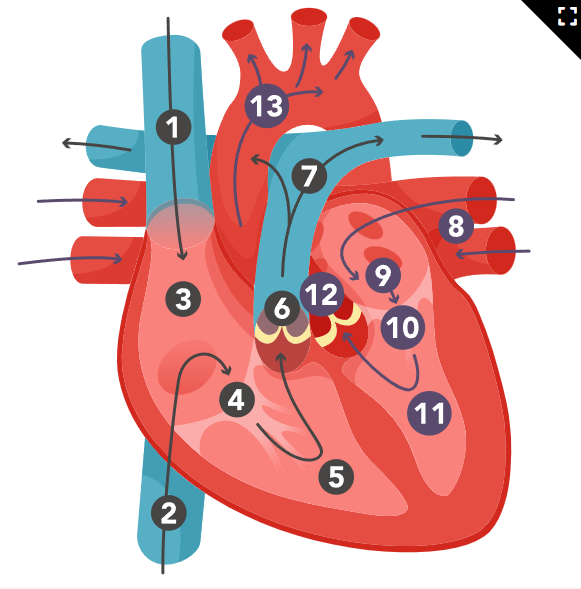
Blood Flow Through the Heart (Image)
Blood Vessels and Their Functions
Arteries
High-pressure blood is transported from the heart to arteries and arterioles.
Arterioles
Join arteries and capillaries.
Veins
Act as a reservoir of blood and carries low-pressure blood to the heart from venules.
Venules
Joins capillaries and veins.
Capillaries
Permits gas exchange, the transfer of nutrients, and the removal of waste between blood and the fluid of tissues.
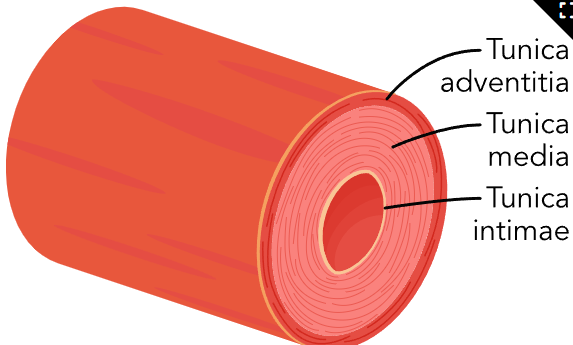
Layers of Arteries (image)
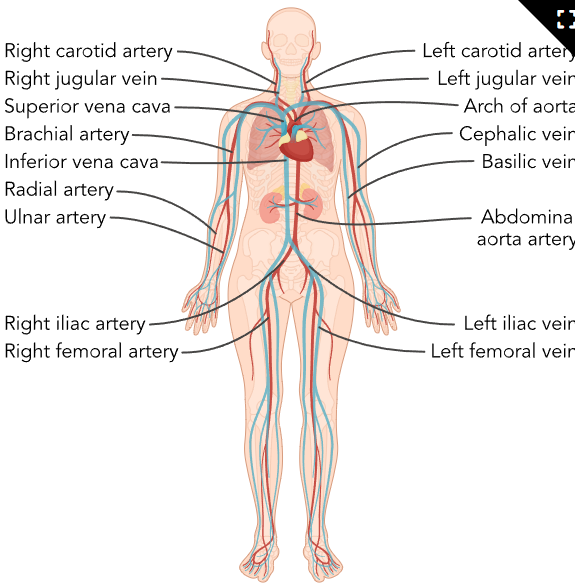
Circulatory system (image)
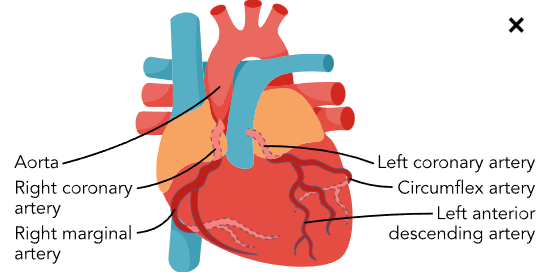
Coronary arteries (image)
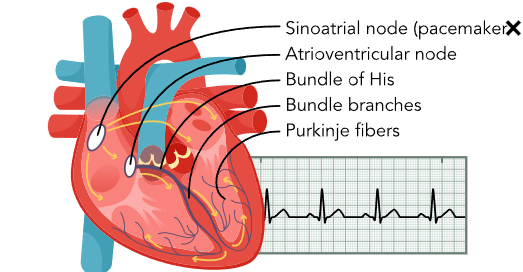
Basic Cardiac Electrophysiology (image)
Systems w/in Heart (3)
Electrical (conduction/rhythm)
Circulatory (blood flow/arterial health)
Mechanical / Pumping System (contractility/valves)
Electrical (conduction/rhythm)
Creates and sends signals to make the heart beat.
The heart's "power source" or "electric wiring."
Responsible for creating and sending out electrical signals that make the heart contract and pump blood.
How it works: The heart has a special group of cells that create electrical impulses.
The main one is called the SA node (Sinoatrial node) located in the upper part of the right atrium. The SA node is like the heart’s natural pacemaker, setting the rhythm of the heart by sending out signals that spread through the atria, causing them to contract and push blood into the ventricles.
After the atria contract, the electrical signal reaches the AV node (Atrioventricular node), which acts like a gatekeeper. It slows down the signal slightly before it continues down to the ventricles, ensuring the atria have time to fully contract before the ventricles take over.
The signal then moves through the Bundle of His and the Purkinje fibers, causing the ventricles to contract and pump blood out to the lungs and the rest of the body.
Lightbulb (heart muscle), switch (SA node) and wiring (AV node, Bundle of His, Purkinje fibers)
Circulatory (Blood flow/arterial health)
Delivers oxygen and nutrients to the heart muscle
This system supplies blood to the heart itself. Just like any other organ, the heart needs oxygen and nutrients to work properly.
Delivers these by using coronary arteries and veins that wrap around the outside of the heart.
How it works: The heart gets its O2 blood from two main arteries called the left and right coronary arteries.
These branch off from the aorta, the body’s largest artery, which carries blood from the heart to the rest of the body.
The coronary arteries split into smaller branches to deliver oxygen and nutrients to every part of the heart muscle. After the heart uses up the oxygen, the CO2 blood is carried back by coronary veins into the right atrium, where it can go to the lungs to pick up more oxygen.
Personal delivery service
Mechanical (contractility/valves)
Controls the actual squeezing and pumping of blood throughout the body.
This system is responsible for the actual "squeezing" or contraction of the heart muscle, which pushes blood through the heart and out to the body.
This is what people often refer to as the "heartbeat."
How it works: The heart has four chambers – two atria (top chambers) and two ventricles (bottom chambers).
Blood flows into the right atrium from the body, goes to the right ventricle, and gets pumped to the lungs to pick up oxygen. After the blood is oxygenated in the lungs, it flows into the left atrium, then into the left ventricle, which is the heart's strongest chamber. The left ventricle pumps the oxygen-rich blood out to the entire body.
Pumping happens in two phases: Systole (the heart's squeezing phase) and Diastole (the heart's relaxing and filling phase). When the ventricles squeeze (during systole), they send blood out to the body and lungs. When the heart relaxes (diastole), the atria fill with blood, getting ready for the next heartbeat.
Water balloon
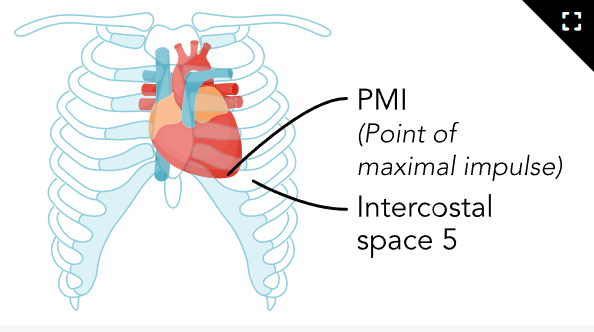
Point of maximum impulse PMI (image)
Coronary Arteries (RP-LCD)
RCA
Marginal Artery: Supplies the lateral side of the right heart.
Posterior Descending Artery: Provides blood to the posterior heart.
LCA
Left Main Coronary Artery: Originates from the aorta.
Left Anterior Descending (LAD) Artery: Supplies blood to the front (anterior) of the left ventricle.
Circumflex Artery: Wraps around the left lateral side of the heart and supplies the left atrium and the posterior-lateral left ventricle.
Nursing Considerations
During increased heart rates, nurses must monitor for reduced coronary perfusion.
Blockages in these arteries (like in the LAD or RCA) can lead to ischemia, increasing the risk of heart attacks
Coronary Nursing Considerations
During increased heart rates, nurses must monitor for reduced coronary perfusion.
Blockages in these arteries (like in the LAD or RCA) can lead to ischemia, increasing the risk of heart attacks
Circulatory Pathway (4)
1. Blood enters the heart (Right Side - Pulmonary Circulation):
Deoxygenated blood (blood low in oxygen) returns from the body through two large veins:
Superior Vena Cava: Carries blood from the upper part of the body (head, arms, upper torso).
Inferior Vena Cava: Carries blood from the lower part of the body (legs, abdomen).
The blood flows into the right atrium (the upper right chamber of the heart).
From the right atrium, blood passes through the tricuspid valve into the right ventricle (the lower right chamber).
2. Blood is pumped to the lungs (Pulmonary Circulation):
When the right ventricle contracts, it pumps blood through the pulmonary valve into the pulmonary artery.
The pulmonary artery carries this deoxygenated blood to the lungs, where it picks up oxygen and releases carbon dioxide.
3. Oxygenated blood returns to the heart (Left Side - Systemic Circulation):
After the blood becomes oxygenated in the lungs, it returns to the heart via the pulmonary veins.
The oxygen-rich blood enters the left atrium (the upper left chamber of the heart).
From the left atrium, blood passes through the mitral valve (also called the bicuspid valve) into the left ventricle (the lower left chamber).
4. Blood is pumped to the body (Systemic Circulation):
The left ventricle, which is the strongest chamber of the heart, contracts and pumps the oxygen-rich blood through the aortic valve into the aorta (the largest artery in the body).
From the aorta, the blood is distributed through smaller arteries to the rest of the body, delivering oxygen and nutrients to tissues and organs.
The cycle repeats:
Once the oxygen in the blood is used up by the body's tissues, the deoxygenated blood returns to the heart through the vena cavae, starting the cycle all over again.
Circulatory Path (1 of 4)
Blood enters the heart (Right Side - Pulmonary Circulation):
Deoxygenated blood (blood low in oxygen) returns from the body through two large veins:
Superior Vena Cava: Carries blood from the upper part of the body (head, arms, upper torso).
Inferior Vena Cava: Carries blood from the lower part of the body (legs, abdomen).
The blood flows into the right atrium (the upper right chamber of the heart).
From the right atrium, blood passes through the tricuspid valve into the
Circulatory Path (2 of 4)
Blood is pumped to the lungs (Pulmonary Circulation):
When the right ventricle contracts, it pumps blood through the pulmonary valve into the pulmonary artery.
The pulmonary artery carries this deoxygenated blood to the lungs, where it picks up oxygen and releases carbon dioxide.
Circulatory Path (3 of 4)
Oxygenated blood returns to the heart (Left Side - Systemic Circulation):
After the blood becomes oxygenated in the lungs, it returns to the heart via the pulmonary veins.
The oxygen-rich blood enters the left atrium (the upper left chamber of the heart).
From the left atrium, blood passes through the mitral valve (also called the bicuspid valve) into the left ventricle (the lower left chamber).
Circulatory Path (4 of 4)
Blood is pumped to the body (Systemic Circulation):
The left ventricle, which is the strongest chamber of the heart, contracts and pumps the oxygen-rich blood through the aortic valve into the aorta (the largest artery in the body).
From the aorta, the blood is distributed through smaller arteries to the rest of the body, delivering oxygen and nutrients to tissues and organs.
Valve Order
Tricuspid → Pulmonary → Bicuspid/Mitral → Aortic
Arterial System
Carries O2 blood (bright red) away from heart to tissues/organs (exception: pulmonary carries CO2 from heart to lungs for oxygenation)
High pressure system (thicker, more muscular)
No valves (except semilunars) due to little backflow risk
Deeper in body
15% of blood volume
Venous System
Carries CO2 blood (blue) back to heart (exception: pulmonary carries O2 blood from lungs to heart)
Low pressure system (thinner, more flexible)
One-way valves to prevent back-flow
Superficial in body
65-75% of blood volume
Varicose Veins
Definition: Swollen, twisted veins that are visible just under the skin, usually in the legs.
Cause: Weak or damaged vein valves, which allow blood to pool and cause the veins to enlarge.
Symptoms: Bulging veins, leg pain, swelling, and a feeling of heaviness or cramping.
Nursing Considerations: Encourage movement to promote circulation, use compression stockings, and elevate legs to reduce swelling.
Aneurysm
Definition: An abnormal bulge in the wall of a blood vessel, often in the aorta or brain.
Intima, Media, Adventitia (All 3 Layers)
Slowing → Arterial Clot (Thrombus) → Embolism (DEADLY)
Cause: Weakening of the blood vessel wall due to high blood pressure, atherosclerosis, or genetic factors.
Symptoms: Often asymptomatic until rupture; can cause pain or pressure. A ruptured aneurysm can lead to severe internal bleeding and is a medical emergency.
Nursing Considerations: Monitor for signs of rupture (sudden severe pain, drop in blood pressure) and manage blood pressure to prevent worsening.
Thrombus vs. Embolism
Definition: A blood clot that forms in a blood vessel and stays there VS when a piece of a thrombus breaks off and travels through the bloodstream to block another vessel
Symptoms: Depending on location, may cause pain, swelling (thrombus), or shortness of breath and chest pain (embolism).
Nursing Considerations: Prevent blood clots by encouraging mobility, using anticoagulant medications, and assessing for signs of embolism.
Buerger’s Disease (Thromboangiitis Obliterans)
Definition: Inflammatory autoimmune condition of the small and medium-sized arteries and veins, leading to blocked blood flow, primarily in the hands and feet.
Small arterial clots (finger and toe necrosis)
Cause: Strongly associated with smoking.
Symptoms: Pain in limbs, ulceration, and tissue death (gangrene).
Nursing Considerations: Encourage smoking cessation, monitor for signs of reduced circulation, and educate on foot and hand care to prevent injury.
Raynaud’s Disease
Definition: A condition where small blood vessels in the extremities (fingers and toes) spasm, limiting blood flow in response to cold or stress.
Vasospasm, usually remedied with warmth and circulation
Cause: Overreaction of blood vessels to cold or stress.
Symptoms: Color changes in skin (white to blue to red), numbness, tingling, and pain in affected areas.
Nursing Considerations: Keep extremities warm, reduce stress, and avoid triggers like smoking or caffeine.
Treatment: Vasodilators (especially CCBs)
Arteriosclerosis
Definition: General term for the thickening and hardening of arterial walls, reducing their flexibility.
Cause: Aging, high blood pressure, and high cholesterol
Symptoms: Reduced blood flow can cause pain or increase the risk of heart attack or stroke.
Nursing Considerations: Manage blood pressure, promote healthy lifestyle changes (diet and exercise), and monitor for cardiovascular complications.
Atherosclerosis
Definition: A specific type of arteriosclerosis where fatty deposits (plaques) build up inside the artery walls.
Leads to INFLAMMATION
Cause: High cholesterol, smoking (intima lining damaged), high blood pressure, and diabetes.
Symptoms: Can lead to narrowed arteries, resulting in chest pain (angina), heart attack, or stroke.
Nursing Considerations: Focus on cholesterol management, encourage a heart-healthy diet, exercise, and medications like statins to slow plaque buildup.
Lipoprotein
Made up of proteins and fat, carry cholesterol in the bloodstream.
LDL
Action: Transports cholesterol from the liver to the rest of the body.
Cells use this cholesterol for building cell membranes and producing hormones.
However, if too much circulates in the blood, it can deposit cholesterol on the walls of arteries, forming plaques, which narrow the arteries and increase the risk of heart disease and stroke.
Key Point: High levels can lead to atherosclerosis, where arteries become clogged and hardened.
Nursing Focus: Encourage patients to lower levels by adopting a heart-healthy diet (low in saturated fats), exercising, and possibly using medications like statins to reduce cholesterol production.
Normal: <100
Normal: <100
LDL
HDL
Action: Responsible for removing excess cholesterol from the bloodstream and artery walls and transporting it back to the liver for disposal.
This process helps protect the arteries from cholesterol buildup and reduces the risk of atherosclerosis.
Key Point: Higher levels are beneficial because they help "clean up" cholesterol deposits, reducing the risk of heart disease.
Nursing Focus: Promote activities and dietary habits that raise HDL, such as regular physical exercise, healthy fats (like omega-3 fatty acids), and reducing smoking or alcohol consumption.
Normal: 45-60 or >40
Normal: 45-60 or >40
HDL
VLDL
Action: Mainly responsible for transporting triglycerides (another type of fat) from the liver to tissues throughout the body.
Once it delivers triglycerides, it transforms into LDL.
High levels increase the risk of plaque formation in the arteries, contributing to heart disease.
Key Point: Carries triglycerides, which also contribute to fat buildup in arteries, similar to LDL, making it another risk factor for heart disease.
Nursing Focus: Encourage lowering triglyceride levels through weight loss, exercise, limiting alcohol, and reducing sugar and refined carbohydrate intake in the diet.
Normal = 2-30
Normal: 2-30
VLDL
homocysteine
An amino acid the body uses to make proteins.
Normally broken down into other substances the body needs by vitamin B12, vitamin B6, and folic acid, leaving very little in blood
Elevated: Modifiable CAD / MI Risk Factor
Excess damages artery lining and leads to blot clots
Lipoproteins (table)
Lipoprotein | Common Name | Action | Effect on Heart Health |
LDL | "Bad Cholesterol" | Delivers cholesterol to cells and arteries | High levels increase risk of atherosclerosis |
HDL | "Good Cholesterol" | Removes cholesterol from arteries, returns to liver | High levels protect against heart disease |
VLDL | Carries Triglycerides | Transports triglycerides from liver to tissues | High levels increase risk of plaque formation |
Desirable: Less than 200 mg/dL
Borderline High: 200-239 mg/dL
High: 240 mg/dL or above
Total Choleserol
Total Cholesterol Treatment Threshold
Begins at >=240
Hyperlipidemia
Hypertension (HTN)
Heart Disease (Angina, MI) → CAD
Blood Clots
Peripheral Artery Disease (PAD)
Hepatic 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors (statins)
Cholesterol absorption inhibitor
Bile-acid sequestrants
Fibrates
Monoclonal Antibodies
CAD
Heart Disease (Angina, MI)
Nonpharmacological Methods for Cholesterol Reduction (5)
Reduce saturated fats and cholesterol in diet
Reduce total fat intake to 30% or less of caloric intake
Reduce cholesterol intake to 300 mg/day or less
Exercise
Stop smoking
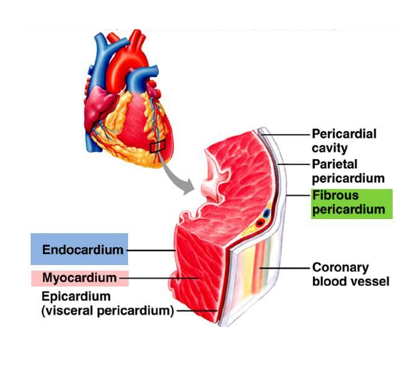
Epicardium
Structure: The outermost layer of the heart wall. It’s a thin, protective membrane that consists of connective tissue and fat. It also forms part of the pericardium, which is the double-walled sac that encloses the heart.
Function: The epicardium provides a smooth outer surface for the heart and acts as a protective layer. It contains coronary blood vessels, nerves, and lymphatics that supply the heart muscle.
Myocardium
Structure: The thickest layer of the heart wall and is composed of cardiac muscle tissue. This layer varies in thickness, being thicker in the ventricles (especially the left ventricle) than in the atria, as the ventricles need more force to pump blood.
Function: The contractile layer, responsible for pumping blood out of the heart and throughout the body. The muscle fibers in the myocardium are arranged in a spiral pattern, which allows the heart to contract in a coordinated and efficient manner.
Endocardium
Structure: A thin, smooth layer of endothelial cells that lines the inner chambers of the heart and covers the heart valves. It is continuous with the inner lining of blood vessels (the vascular endothelium).
Function: Provides a smooth surface that allows blood to flow easily inside the heart and helps prevent clot formation. It also plays a role in regulating the heart’s function by responding to signals from the bloodstream.
The Heart Wall (image)
Left Main Coronary Artery (LMCA)
Location: Branches directly off the aorta, the body’s largest artery, just above the aortic valve.
Function: Quickly divides into two major branches that supply blood to the left side of the heart. It serves as the primary source of blood to the left heart.
Left Anterior Descending Artery (LAD)
Location: Branch of the left main coronary artery and runs down the front of the heart (anterior surface), along the interventricular septum, which separates the left and right ventricles.
Function: Supplies blood to the front (anterior) part of the left ventricle and the front of the interventricular septum. It is a critical artery because the left ventricle pumps blood to the entire body.
Circumflex Artery (CX)
Location: Branch of the left main coronary artery. It curves around the left side of the heart and travels along the groove that separates the left atrium and left ventricle.
Function: Supplies blood to the lateral (side) and posterior portions of the left ventricle, as well as the left atrium.
Right Coronary Artery (RCA)
Location: Branches off the aorta and travels down the right side of the heart, following the groove between the right atrium and right ventricle.
Function: Supplies blood to the right atrium, right ventricle, and parts of the bottom (inferior) portion of both the left and right ventricles. It also supplies blood to the AV node, which plays a role in regulating the heart's electrical conduction system.
Posterior Descending Artery (PDA)
Location: Branches off the right coronary artery (in most people, but in some cases, it can branch from the circumflex artery). It runs along the back (posterior) part of the heart, in the groove between the ventricles.
Function: Supplies blood to the posterior part of the ventricles, particularly the inferior wall of the heart and part of the interventricular septum.
Angina Infarction
When the heart muscle (myocardium) doesn’t receive enough oxygen-rich blood to meet its needs
Typically during times of increased demand, such as physical exertion or stress.
Causes temporary ischemia (lack of blood supply) but doesn’t result in permanent damage to the heart muscle.
Angina Infarction Pathophysiology
Coronary artery narrowing: Usually caused by atherosclerosis
Mismatch between oxygen demand and supply (due to narrowed arteries): During physical exertion, emotional stress, or after eating a large meal, the heart’s demand for oxygen increases.
Ischemia and pain: The lack of oxygen (ischemia) in the heart muscle leads to chest pain or discomfort
The hallmark symptom of angina.
Pain usually resolves with rest or medications like nitroglycerin, which dilate the blood vessels and improve blood flow.
Tissue/muscle is not getting blood and oxygen past a blockage or spasming vessel (artery)
Myocardial Infarction (MI)
Occurs when blood flow to a portion of the heart muscle is completely blocked, usually due to the rupture of an atherosclerotic plaque and the formation of a blood clot (thrombus).
Results in prolonged ischemia and causes permanent damage (necrosis) to the affected part of the heart muscle.
Myocardial Infarction Pathophysiology
Plaque rupture: A plaque inside a coronary artery ruptures or tears, exposing its contents to the bloodstream. This activates platelets, causing them to aggregate and form a blood clot (thrombus) over the plaque.
Complete blockage of the artery: The clot completely occludes the coronary artery, blocking blood flow to a portion of the myocardium.
Prolonged ischemia: Without oxygen, the affected area of the heart cells begin to die (necrosis).
This results in the disease.
Cellular damage and death: The lack of oxygen leads to cellular injury and eventually myocardial necrosis (death of heart muscle cells). The longer the blockage lasts, the larger the area of infarction and the greater the damage.
Inflammatory response: The body mounts an inflammatory response to the dead tissue, and this damage can weaken the heart muscle, leading to complications like heart failure or arrhythmias.
Stable Angina (Classic)
Predictable chest pain that occurs with exertion
Relieved by rest or medication.
Around 70% blockage
Usually due to a fixed narrowing of the coronary arteries.
Educate on triggers and proper use of nitroglycerin
Unstable Angina (Preinfarction)
Chest pain that occurs at rest or with minimal exertion (unrelated to activity)
More severe or prolonged, and does not always respond to medication.
Around 90% blockage
Sign that a plaque has ruptured or a clot has formed, creating a greater risk of heart attack.
Monitor for signs as it may precede a heart attack
Variant Angina (Prinzmetal’s, Vasopastic)
Caused by spasms of coronary arteries, not necessarily due to plaque
Occurs during rest
May not have blockage
Common in women (postmenopausal)
Nonpharmacological Control of CAD & Angina (7)
Avoiding heavy meals
Smoking cessation (vasoconstricts)
Avoiding extreme weather changes
Avoiding strenuous exercise
Avoiding emotional upset
Proper nutrition (avoid caffeine) and moderate exercise
Adequate rest, relaxation techniques
ST-Elevation Myocardial Infarction (STEMI)
A severe heart attack where the coronary artery is completely blocked, leading to extensive damage.
A medical emergency
Non-ST-Elevation Myocardial Infarction (NSTEMI
A partial blockage of a coronary artery, leading to less extensive damage.
Still a medical emergency.
MI Nursing Considerations
Immediate actions: Call for emergency help, administer oxygen, aspirin (to reduce clotting), and nitroglycerin to improve blood flow.
Continuous monitoring: Monitor for complications like arrhythmias, heart failure, or shock.
Education: Post-MI, educate the patient about lifestyle changes, medications (such as beta-blockers, ACE inhibitors, or statins), and rehabilitation to reduce the risk of future heart events.
MI S/S
Severe chest pain or discomfort (often described as crushing or squeezing), which may radiate to the jaw, neck, arm, or back.
Shortness of breath, sweating, nausea, and lightheadedness.
Women and people with diabetes may experience less typical symptoms, such as fatigue, indigestion, or back pain.
Systole (S1)
Ventricles: Contract to pump blood out.
Aortic and Pulmonary Valves: Open to allow blood to exit the heart.
Mitral and Tricuspid Valves: Close to prevent backflow into the atria (LUB)
Diastole (S2)
Ventricles: Relax and fill with blood.
Mitral and Tricuspid Valves: Open to allow blood to flow from the atria into the ventricles.
Aortic and Pulmonary Valves: Close to prevent backflow from the arteries (DUB)
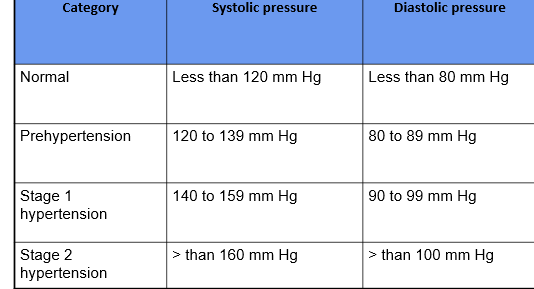
Normal BP
120/80
No treatment required, but maintaining a healthy lifestyle is key to keeping BP in this range.
Prehypertension
120+/80+
Lifestyle modifications, such as dietary changes, exercise, stress management, and possibly monitoring. Medications are generally not needed at this stage unless there are other cardiovascular risks.
Hypertension Medication Treatment
Starts at Stage 1 (140+/90+)
Combination Therapy
Medication dosage increased gradually if blood pressure does not reach target goal.
Additional medications added if needed.
Multiple medications may be needed to control blood pressure.
Lifestyle changes maintained
Stage 1 Hypertension
140+/90+
Lifestyle changes are the first line of treatment (healthy diet, weight loss, exercise, reducing sodium intake, limiting alcohol, quitting smoking).
Medications may be prescribed if the patient has other risk factors (e.g., diabetes, kidney disease, or a history of heart disease or stroke).
Continuous monitoring and regular follow-ups with healthcare providers are necessary to manage BP.
Stage 2 Hypertension
160+/100+
Lifestyle changes remain essential.
Medications are usually necessary at this stage. Common drugs include ACE inhibitors, ARBs, calcium channel blockers, or diuretics to help lower BP.
Closer medical monitoring and adjustments to medication may be required.
Hypertensive Crisis
180+/120+
This is a medical emergency.
Immediate hospitalization is required to reduce blood pressure and prevent organ damage (e.g., heart, brain, kidneys).
Signs include severe headache, shortness of breath, chest pain, or vision problems.
Heart pumps
Systolic
Heart relaxes
Diastolic
Hypertension Causes (3)
High pressure pressing on the arterial wall can occur due to several factors:
The left ventricle empties: When the left ventricle pumps blood into the aorta, if there’s an issue with the ability of the arteries to stretch properly, it leads to increased pressure on the arterial walls.
Plaques obstructing the flow (narrowing): Atherosclerosis, or the buildup of plaques in the arteries, narrows the vessels, which increases resistance and pressure as blood tries to flow through a smaller opening.
Too much volume or high force of ejection (CO): If there is too much blood volume or a high cardiac output (CO), the force of the blood ejection increases, pressing harder against the arterial walls.
Hypertension Regulators
Kidneys via renin–angiotensin system (RAAS)
Baroreceptors in the aorta and carotid sinus
Vasomotor center in the medulla
Hormones
Antidiuretic hormone (ADH)
Atrial natriuretic peptide (ANP)
Brain natriuretic peptide (BNP)
Some Hypertension Risk Factors (8)
Lifestyle
Excess saturated fat and simple carbs (cholesterol → dyslipidemia)
ETOH (increases renin secretions)
No exercise/fiber
Smoking
Aging
Genetics (familial hypercholesterolemia)
Family Hx
Obesity
Increased CO, stroke volume, left ventricular filling
Insulin resistance
Nonpharmacological HTN Treatments (7)
Stress-reduction techniques
Exercise
Weight loss
Low Fat diet
Salt restriction
Decrease alcohol ingestion
Smoking cessation
Guidelines for HTN (image)
Renin-Angiotensin-Aldosterone System (RAAS)
Hormone system regulates blood pressure (BP), fluid balance, and electrolyte levels in the body.
Triggered when blood pressure drop
Helps restore normal blood pressure
Maintains adequate blood flow to organs.
Overactivity leads to high blood pressure and heart failure
Inhibited by ACE inhibitors or ARBs (can lead to hyperkalemia due to aldosterone inhibition)
RAAS (tl;dr)
Low BP / Na2+ / Renal blood flow → Renin
Renin → Angiotensinogen (liver) → Angiotensin I (inactive precursor)
Angiotensin I + Angiotensin-Converting-Enzyme ACE (lungs) → Angiotensin II
Angiotensin II → Vasoconstricts → Triggers Aldosterone (adrenal) → Na2+/H2O retention + K+ excretion
Angiotensin II → Vasoconstricts → Triggers Antidiuretic Hormone ADH (pituitary) → H2O retention
RAAS (1 of 5)
Activation of Renin
Trigger: The RAAS is activated in response to a decrease in blood pressure, low sodium levels, or reduced blood flow to the kidneys.
For example, if the body experiences dehydration or hemorrhage, blood pressure will fall.
Kidney response: Special cells in the kidneys called the juxtaglomerular cells detect this drop in blood pressure and release an enzyme called renin into the bloodstream.
RAAS (2 of 5)
Conversion of Angiotensinogen to Angiotensin I
Renin’s role: Once in the bloodstream, renin converts a protein produced by the liver called angiotensinogen into angiotensin I. Angiotensin I is an inactive precursor, so it needs to be further converted to exert its effects.
RAAS (3 of 5)
Conversion of Angiotensin I to Angiotensin II
ACE (Angiotensin-Converting Enzyme): As blood circulates, angiotensin I is converted into angiotensin II by an enzyme called angiotensin-converting enzyme (ACE), which is primarily found in the lungs.
Angiotensin II: This is the key active molecule in the RAAS system and is a potent vasoconstrictor.
RAAS (4 of 5)
Angiotensin II vasoconstricts, then triggers Aldosterone and/or ADH
Angiotensin II has several actions that work together to increase blood pressure and restore fluid balance:
Vasoconstriction: It causes the blood vessels to narrow (vasoconstriction), which increases vascular resistance, raising blood pressure.
Stimulates Aldosterone Release: Angiotensin II triggers the adrenal glands (located on top of the kidneys) to release aldosterone, a hormone that causes the kidneys to retain sodium and water. This increases blood volume, further raising blood pressure.
Stimulates ADH (Antidiuretic Hormone) Release: Angiotensin II also stimulates the release of antidiuretic hormone (ADH) from the pituitary gland. ADH prompts the kidneys to conserve water, increasing blood volume and blood pressure.
RAAS (5 of 5)
Aldosterone’s Role:
Kidney Function: Aldosterone acts on the kidneys, causing them to retain sodium and water while excreting potassium. Sodium retention leads to water retention, increasing blood volume, which helps to raise blood pressure.
Blood Volume Increase: As blood volume increases, more blood is pushed through the arteries, leading to a rise in cardiac output and ultimately increased blood pressure.
Angiotensin (I + ACE → II)
Peptide hormone that causes vasoconstriction and increases BP
Nutritional Considerations (CAD/HTN)
Polyunsaturated fats
Fish, avocados, nuts, seeds
Fiber
Whole grains, flaxseed, Fresh fruits & Vegetables
Lean Meats
Limit Sodium (2000mg/day)
Omega-3 Fatty Acids
Limit Caffeine
Limit Alcohol
BP Categories and Treatment Approach (Table)
BP Category | Systolic (mmHg) | Diastolic (mmHg) | Treatment Approach |
Normal | < 120 | < 80 | Maintain healthy lifestyle |
Elevated | 120-129 | < 80 | Lifestyle modifications |
Hypertension Stage 1 | 130-139 | 80-89 | Lifestyle changes + meds if risk factors |
Hypertension Stage 2 | ≥ 140 | ≥ 90 | Lifestyle changes + medications |
Hypertensive Crisis | > 180 | > 120 | Emergency care needed |
Adrenergic Receptors
Alpha-adrenergic receptors (Alpha-1 and Alpha-2)
Beta-adrenergic receptors (Beta-1, Beta-2, and Beta-3)
Beta 1 Receptors (Heart, Kidneys)
Increases cardiac contractility (inotropy)
Increases heart rate (chronotropy)
Increases renin secretion (increases BP)
Antagonist: Treats hypertension, heart failure, angina
Beta 2 Receptors (Lungs, Skeletal Blood Vessels, Uterus)
Increases bronchodilation
Decreases GI motility and tone
Increases blood flow in skeletal muscles
Relaxes uterus muscles
Activates liver glycogenolysis (increases blood glucose)
Agonists: Treats asthma and COPD
Alpha 1 Receptors (Blood Vessel Smooth Muscle, Bladder Neck, Prostate)
Increases cardiac contractility (inotropy)
Increases vasoconstriction
Dilates pupils, decreases salivary gland secretion
Increases bladder and prostate contraction
Antagonists (-zosin): Treat hypertension and BPH
Alpha 2 Receptors (Brain, Smooth Muscle, Presynapse)
Inhibits norepinephrine release
Promotes vasodilation (Decreased blood pressure)
Decreases GI motility and tone
Agonists (GMC): Lowers blood pressure but discontinuation can mean rebound HTN
Summary of Adrenergic Receptors' Mechanisms of Action (Table)
Receptor Type | Location | Agonist (Activation) Effects | Antagonist (Blocking) Effects |
Beta-1 | Heart, Kidneys | Increases heart rate, contractility, and renin release | Decreases heart rate, contractility, and BP (Beta-blockers) |
Beta-2 | Lungs, Blood Vessels, Uterus | Bronchodilation, vasodilation, uterine relaxation | Bronchoconstriction, vasoconstriction |
Beta-3 | Adipose tissue, Bladder | Lipolysis, bladder relaxation | Reduced fat breakdown, bladder contraction |
Alpha-1 | Blood vessels, Bladder, Prostate | Vasoconstriction, urinary retention | Vasodilation, improved urine flow (Alpha-1 blockers) |
Alpha-2 | Presynaptic neurons, Brain | Decreases norepinephrine release (lowers BP) | Increases norepinephrine release (raises BP) |
Beta Blockers (Beta-1 antagonists) Nursing Considerations
Commonly used for treating hypertension, heart failure, and angina.
Caution must be used in patients with asthma due to potential Beta-2 blockade, which can cause bronchoconstriction.
Alpha-1 Blockers Nursing Considerations
Used to treat hypertension and benign prostatic hyperplasia by promoting vasodilation and easing urinary retention.
Alpha-2 Agonists Nursing Considerations
Can be used to lower BP by reducing sympathetic outflow, but sudden discontinuation can cause rebound hypertension.
Sweet Apples Have Big Price
SA Node (60-100 bpm) - Pacemaker
AV Node (40-60 bpm) - Back up pacemaker
His Bundle
Bundle Branches
Purkinje Fibers - Pace
P Wave (A-DE)
Atria squeeze (contract)
DE-polarize / DE-compress → Sends charge out