Molecular & Cell Bio. - Exam 2 - Glucose Transporters
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
what are glucose transporters (GLUTs)?
channel proteins which allow glucose to be transported across a cell membrane
- 11 GLUTs are found in the body
GLUTs 1, 3, and 4 are involved in...? where are they found?
glucose uptake from the blood
- GLUT1/3 are responsible for basal glucose uptake; found in most tissues
- GLUT4 removes excess glucose from the blood; found in skeletal muscle and adipose (fat) tissues
what are the primary functions of GLUT2? where is it found?
found in the liver, kidneys, and pancreas
- transports glucose INTO cells when blood glucose is HIGH
- transports glucose OUT of cells and into the blood when blood glucose is LOW
what is the function of GLUT5? where is it found?
found in the small intestine and testes
- transports fructose
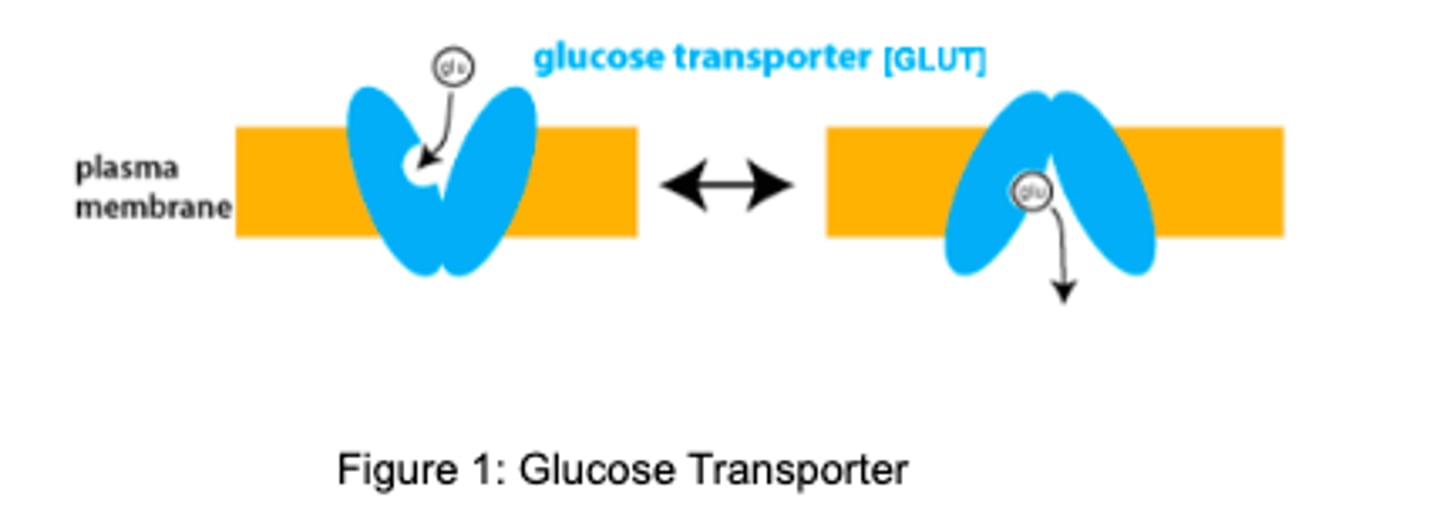
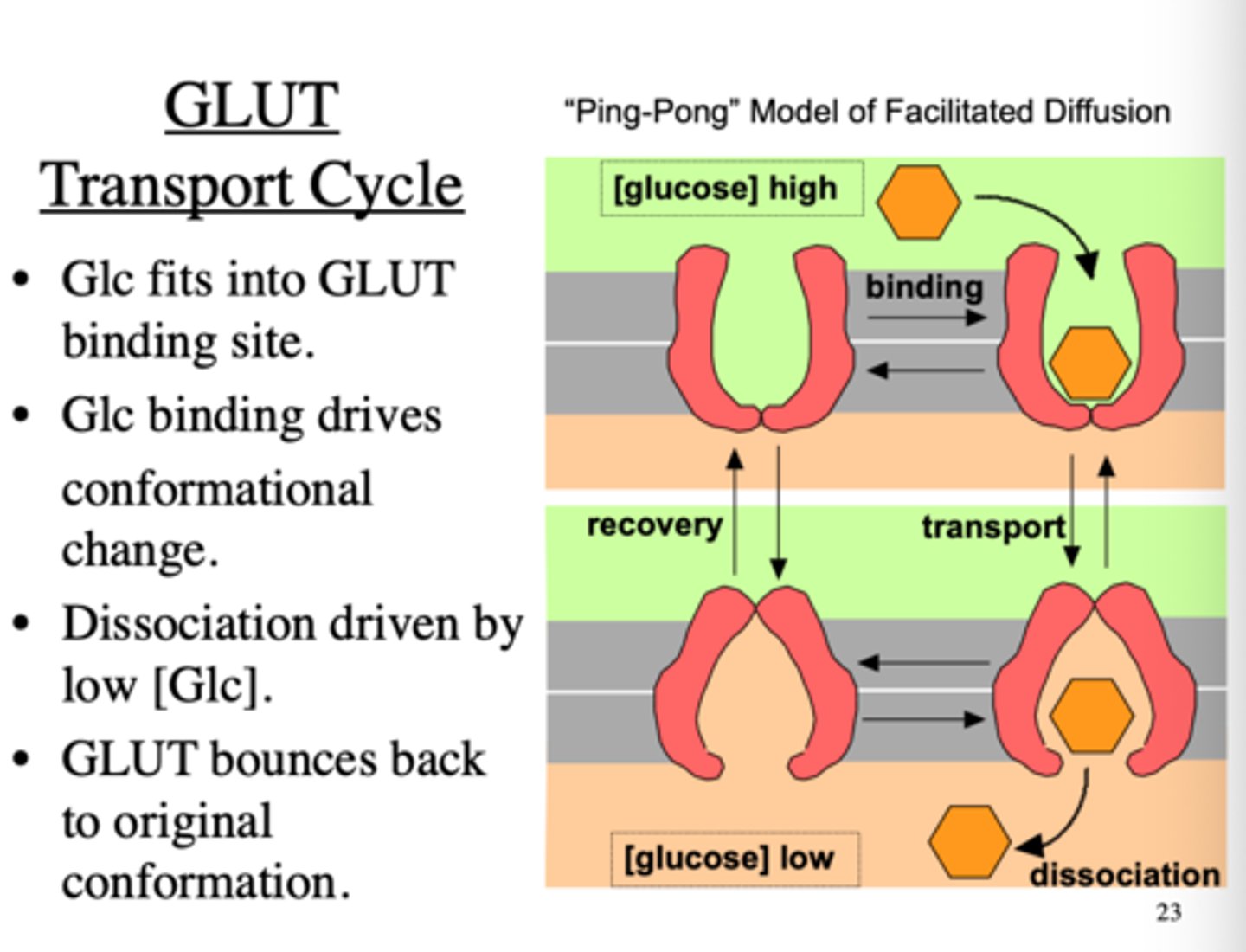
describe the general mechanism of glucose transport by GLUTs
glucose transport occurs from an area of higher concentration to lower concentration via facilitated diffusion
- when the glucose binds to the GLUT, the membrane direction of the enzyme reverses to carry the molecule across
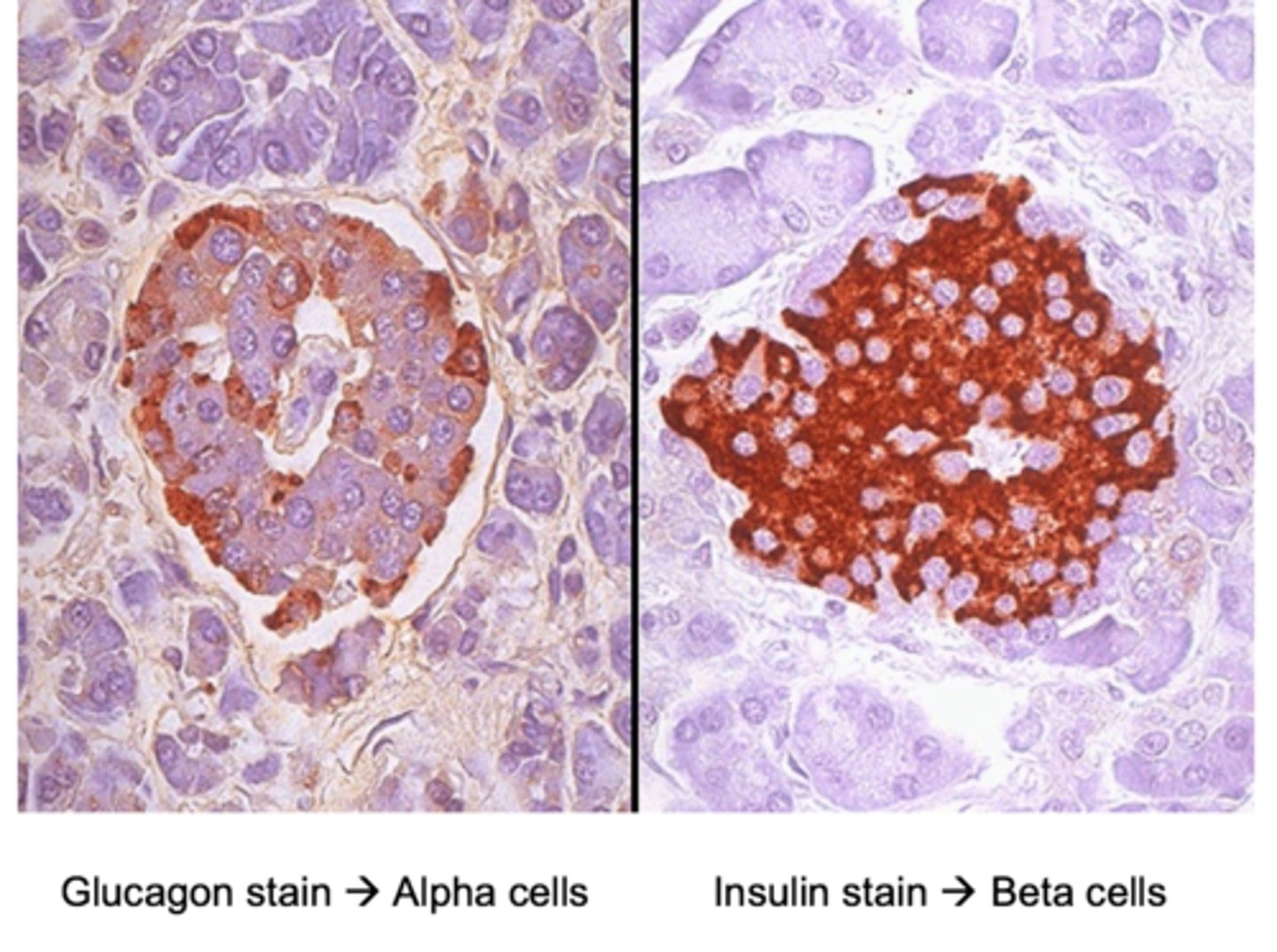
where in the body is insulin produced? what stimulates its release?
beta cells of the islet of Langerhans in the pancreas
- released in response to carbohydrates (including glucose) and amino acids
how does epinephrine impact insulin release?
inhibits insulin release
- hormone is secreted in response to stress
where does insulin-sensitive facilitated transport occur in the body?
skeletal muscle and adipose
where does insulin-insensitive active transport occur in the body? insulin-insensitive facilitated transport?
active transport
- intestinal epithelia
- renal tubules
- choroid plexus
facilitated transport
- erythrocytes
- leukocytes
- lens and cornea of the eyes
- liver
- brain
erythrocytes, leukocytes, hepatocytes, and brain cells express insulin-insensitive GLUT___/___/___ Rs
GLUT 1/2/3 Rs
describe the role of GLUT2 in the renal tubule cells
- absorbs the glucose from the lumen of the small intestine
- reabsorbs the glucose from the glomerular filtrate in the kidneys and returns it to the blood
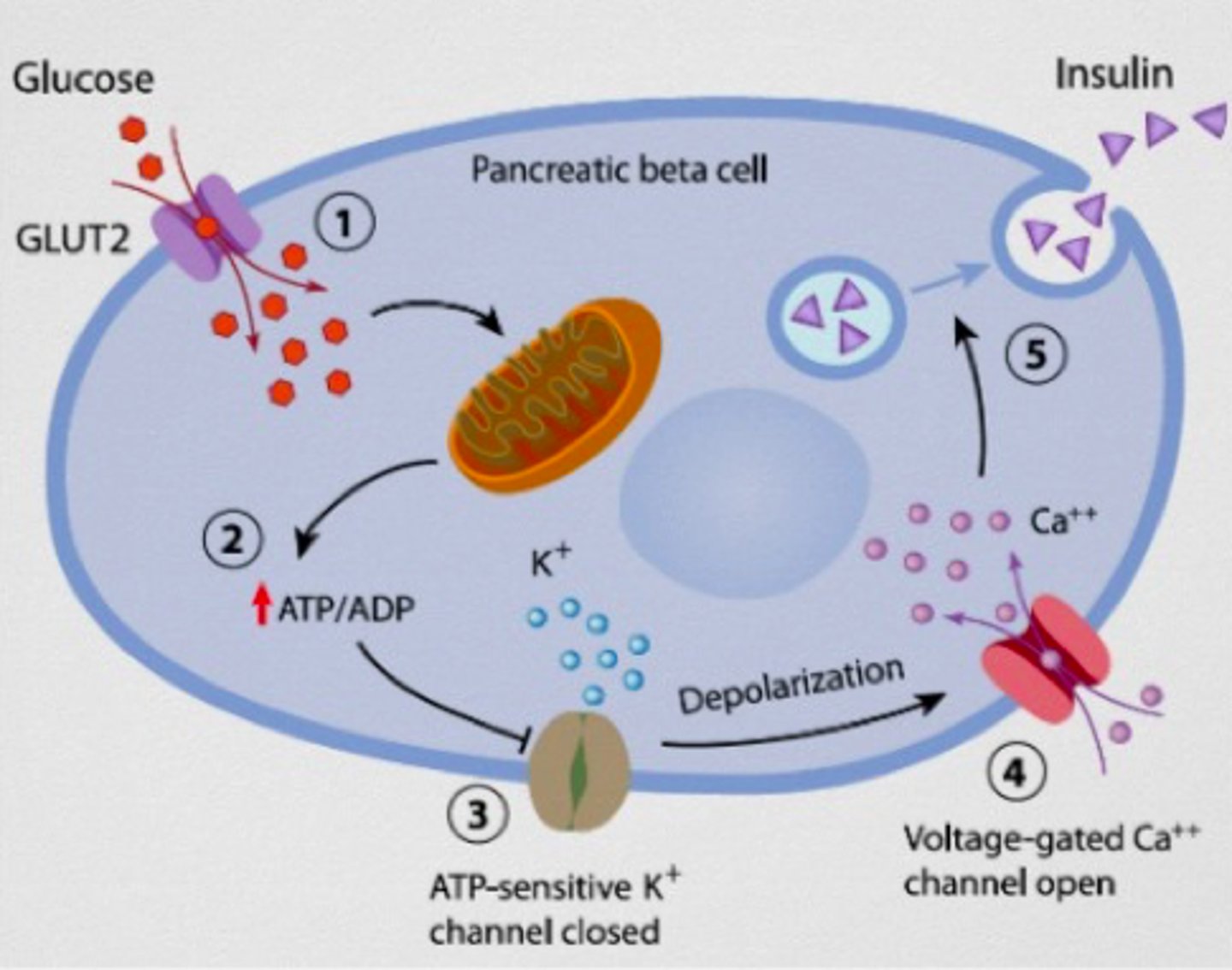
describe the process of how GLUT2 activity leads to the release of insulin from the pancreatic beta cells
exogenous glucose is taken up by the pancreatic cells via GLUT2
- glycolysis occurs, increasing the ATP levels inside the cell
- the increase in ATP leads to closure of ATP-sensitive K+ channels
- closure of the K+ channels causes membrane depolarization, which opens the voltage-gated Ca2+ channels
- Ca2+ influx stimulate the insulin-containing vesicles to fuse with the membrane and release their contents into circulation
insulin increases glucose uptake by muscle and adipose tissue via the ___________ transporter
GLUT4
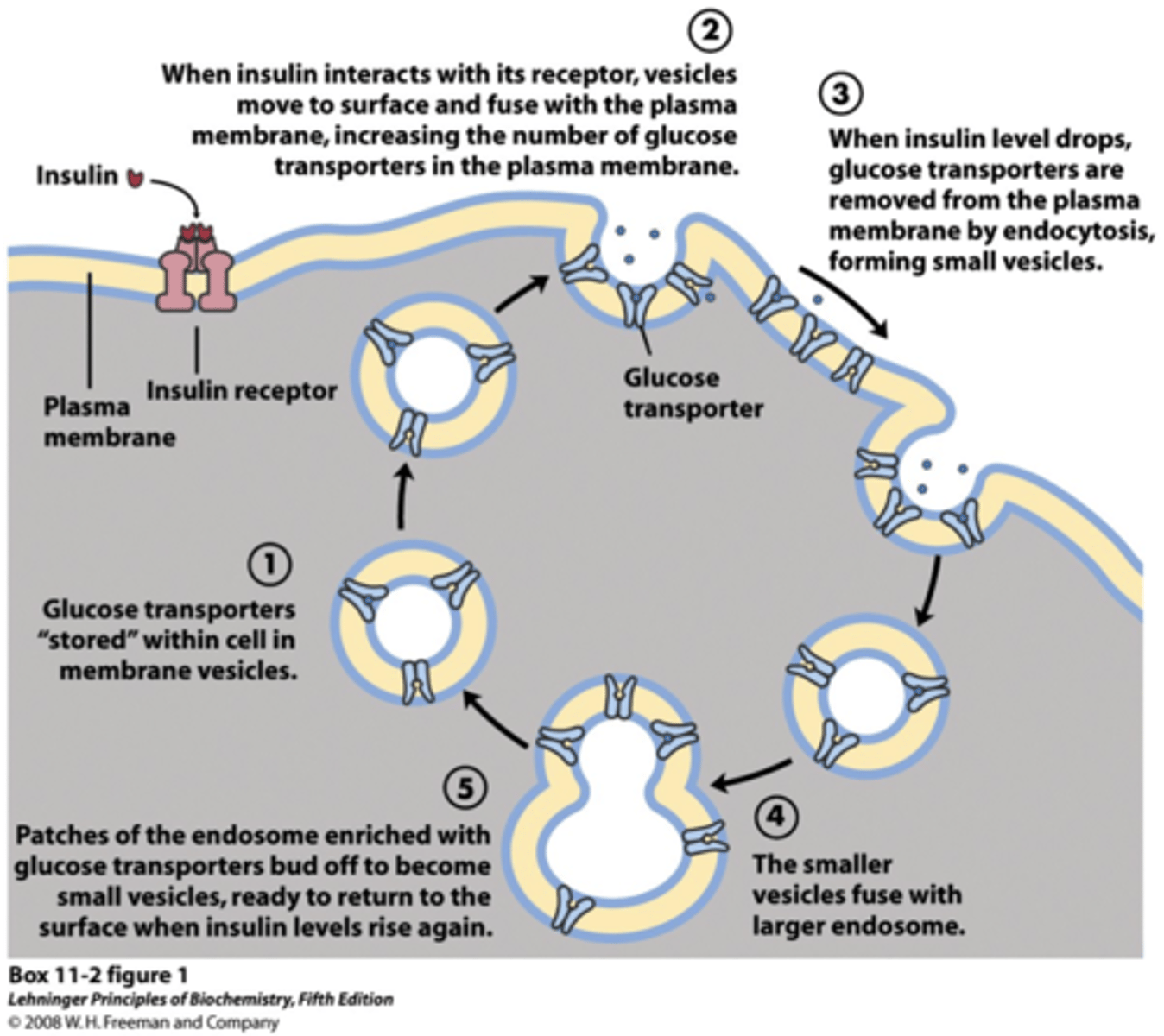
where is the GLUT4 transporter stored in the cell, and how is it activated?
normally stored in IC vesicles, inactive and bound to the Golgi body
- insulin signaling translocates the GLUT4 to the cell membrane (insulin-SENSITIVE!), and glucose can then be taken up by the cell
- when insulin levels decrease, GLUT4 is returned to their IC vesicles
how does insulin promote energy synthesis?
insulin helps our cells absorb more glucose from the blood
- this glucose can then be used in glycolysis to synthesize ATP
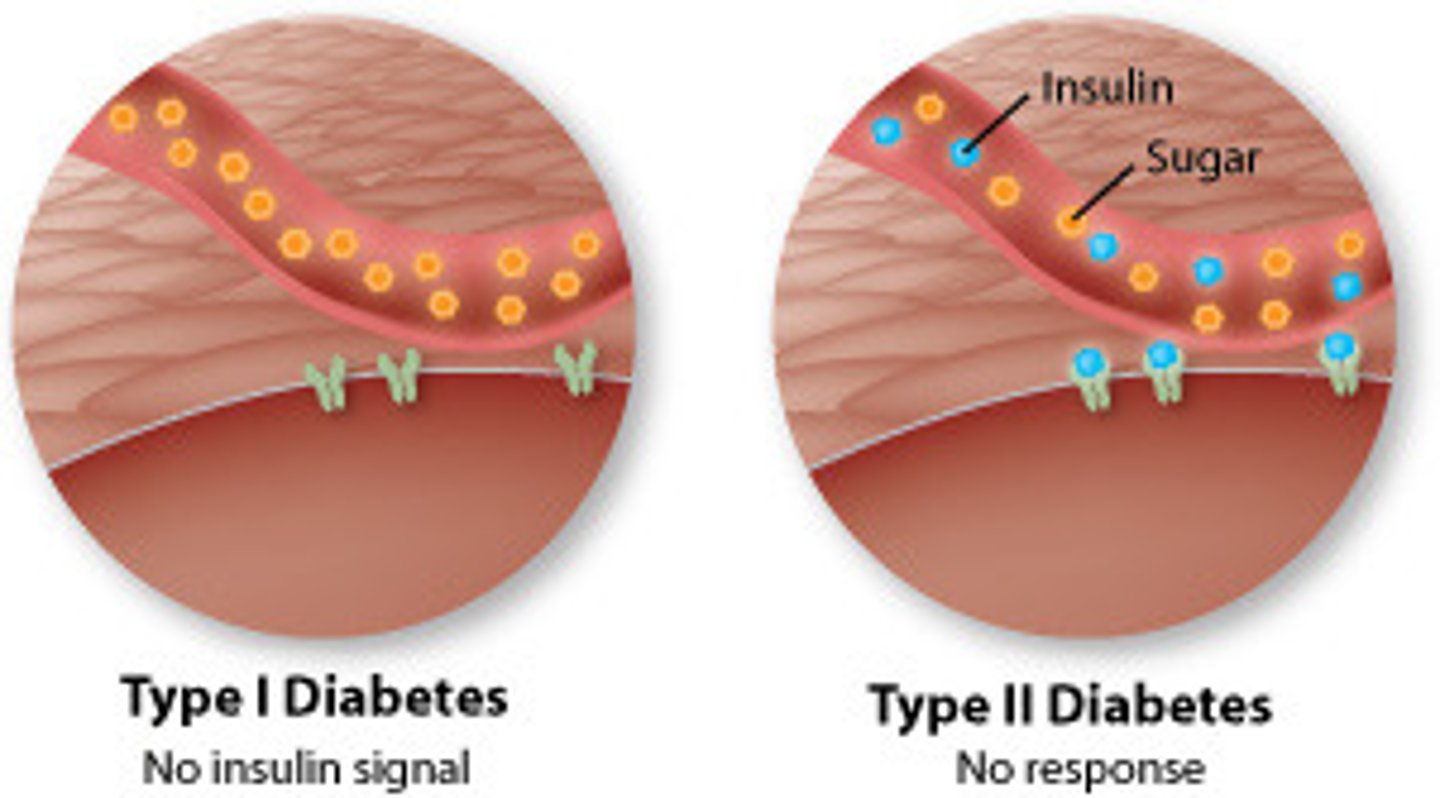
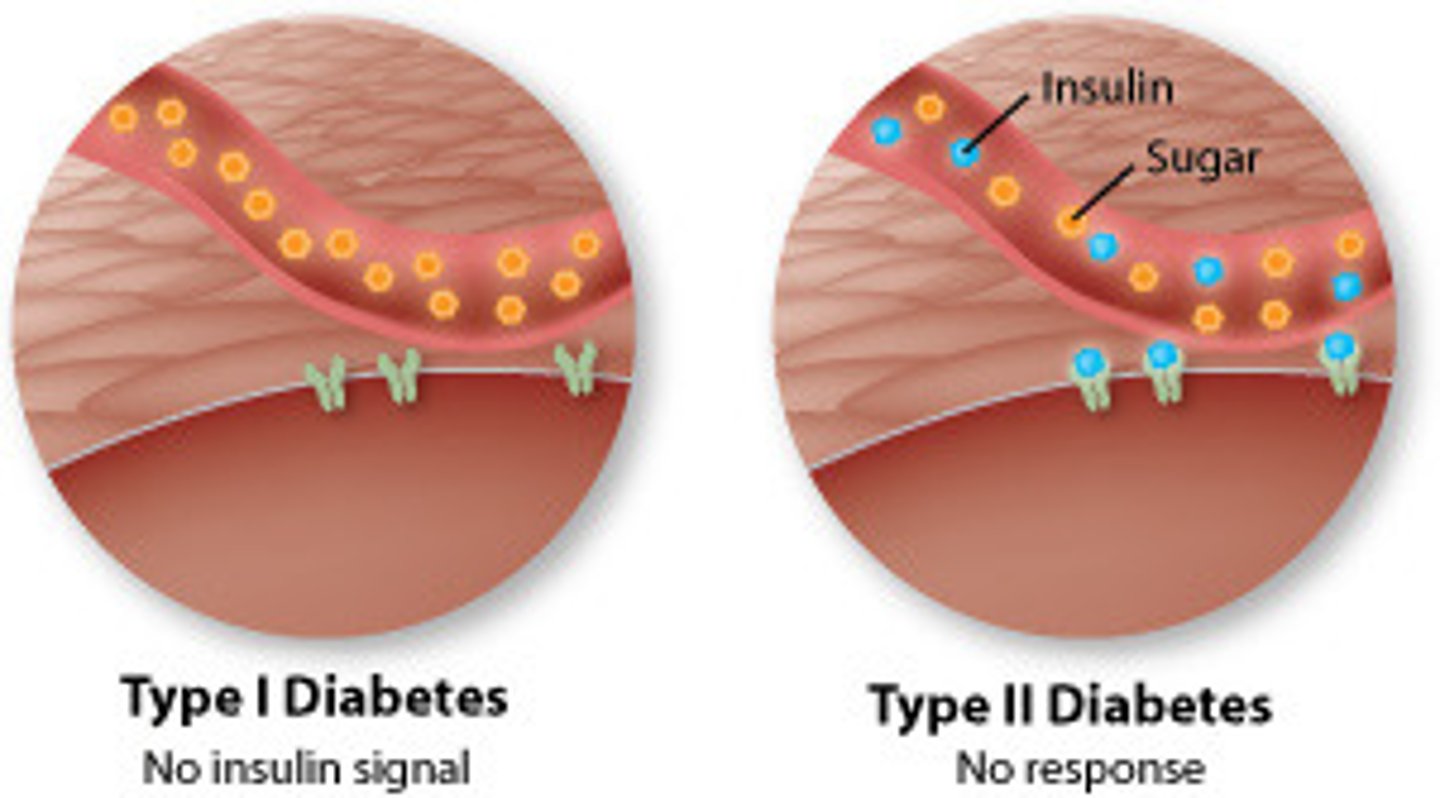
what is type 1 DM? what is the treatment for this condition?
beta cells of affected individuals are destroyed by an autoimmune response
- results in no endogenous insulin production
- treatment: exogenous insulin injection (reduces blood glucose)
T/F: insulin is catabolic
FALSE
- insulin is ANABOLIC
- favors the building of stores of carbs, fats, and proteins
what is type 2 DM? what is the treatment for this condition?
failure of cells to respond properly to insulin
- insulin-sensitive glucose transport impaired
- treatment: weight loss, diet/exercise, hypoglycemic agents (help improve insulin signaling)
what are Na+/glucose transport proteins (SGLTs)?
catalyze the transport of glucose against its concentration gradient (active transport)
- symporter; glucose and Na+ are moved in the same direction, into the cell
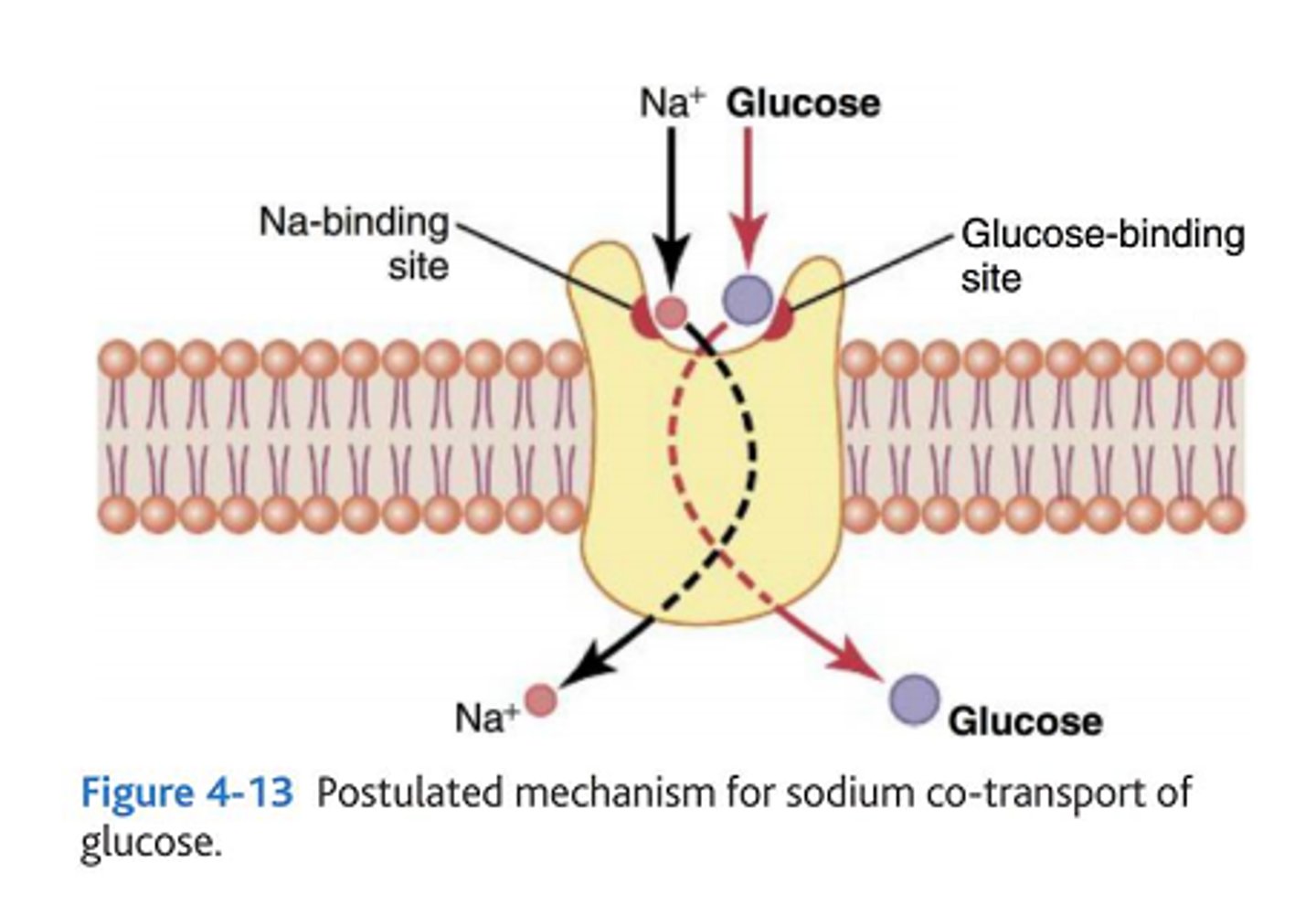
where are SGLT 1 and 2 located?
- SGLT1: proximal tubule and intestines → in intestines, dietary glucose is absorbed and entered into blood circulation
- SGLT2: kidney proximal tubule (renal glucose reabsorption)
in the renal tubules, where is 90% of the glucose absorbed? where is the remaining 10% absorbed?
- 90% is absorbed by SGLT2 in the first segment of the proximal tubules
- 10% is absorbed by SGLT1 in the distal segments of the proximal tubules
to treat type 2 DM, which transport enzyme is inhibited? what is a popular drug with this MOA?
SGLT2
- decreases reabsorption/increases excretion of glucose into the urine to allow excess glucose to exit the system
- drug: gliflozins (Jardiance)