Lecture 4: Sodium and Water Balance II
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
The interstitial fluid of the medulla is __
hyperosmotic
There is a higher __ concentration extracellularly and higher __ concentration intracellularly.
Na+, K+
Sodium concentration remains __ and is __ and __ regulated through __.
constant; rapidly; precisely; water balance
Why is sodium concentration constant? (2)
primarily: to maintain constant osmolality in order to prevent rapidly fluctuating cell volume
secondarily: to maintain good circulating volume (euvolemia)
Because Na+ concentration is constant, what determines its volume?
amount of Na+ in ECF
amount of Na_ECF / amount of water _ ECF = [Na+]
Na+ is the principle extracellular __
cation
Changes in Na+ content stimulate __ or __ of water and determine the __ of the extracellular fluid.
addition; removal; volume
where Na goes, H2O will follow (for balance)
By adding or subtracting amounts of H2O, the [Na+] will be __, so changes in Na+ content can be monitored and regulated by __.
constant; ECF volume
Na+ regulation is in response to __ changes.
volume changes
there are no individual sodium sensors
Total volume of body water is __ L. 25L is in the __, 15L is in the __, which is made up of: (2)
40; intracellular fluid; extracellular fluid; interstitial fluid (12L) + plasma (3L)
What are 2 immediate responses to decreased Na intake?
increased sympathetic activity → constriction of afferent arterioles → dec GFR → inc Na reabsorption → dec Na excretion
dec ANP → dilation of efferent arterioles → dec GFR → inc Na reabsorption → dec Na excretion
How does oncotic pressure change in response to decreased Na intake?
inc oncotic pressure → inc Na reabsorption → dec Na excretion
What is the long-term mechanism that responds to decreased Na intake?
inc renin-angiotensin-aldosterone → inc Na reabsorption → dec Na excretion
What structures of the glomerulus and JGA are important for triggering mechanisms that will increase renin secretion?
renal sympathetic nerves
intrarenal baroreceptors (when relaxed, renin is secreted)
macula densa (have Na/Cl cells that sense load → communicates with juxtaglomerular cells, which secrete renin)
RAAS is distributed throughout __
the body
liver secretes angiotensinogen
kidneys secrete renin
adrenal cortex secretes aldosterone
__ is the rate limiting step of the RAAS.
renin
Describe the RAAS pathway.
angiotensinogen + renin → angiotenin I → angiotenin II (via ACE) → stimulates aldosterone secretion
system is stimulated by decreased plasma volume
What triggers renin release?
dec plasma volume →
inc activity of renal sympathetic nerves
dec arterial pressure
dec GFR → dec flow to macula densa → dec NaCl delivery
→ stimulates renin release
__ can regulate up to 2% of the filtered load of Na+
aldosterone
(Na filtered load = 20160, aldosterone = 400)
Aldosterone works via a feedback loop that controls the __ of Na in the body. This is called __.
amount; voluostat
How does aldosterone control the amount of Na in the body?
when ideal volume changes, aldosterone stimulates kidney → Na retention via H2O retention → inc blood volume
ideal volume change detected by volume sensors (neural and intrarenal): stretch receptors, arterial baroreceptors, intrarenal elements
The principal cell is regulated by __ for water reabsorption. How?
ADH: osmoreceptors of posterior lobe of pituitary gland sense and determine if ADH should be secreted
In principal cells, ADH binding causes cAMP to stimulate protein kinase A to __
stimulate placement of aquaporins to cell membrane surface
Both __ and __ regulate principal cells.
ADH, aldosterone
What occurs in response to water deprivation?
inc osmolarity sensed by hypothalamus → inc ADH release from posterior pituitary→ inc aquaporins → inc H2O absorption
→ inc urine osmolarity and dec urine volume = highly concentrated urine
What regions of the nephron do not have aquaporins during dehydration?
ascending limb of loop → early distal convoluted tubule
What response is made in response to water drinking?
dec osmolarity sensed by hypothalamus → dec ADH secretion from posterior pituitary → no aquaporins → no H2O reabsorption
What regions of the nephron have no aquaporins during water drinking?
ascending limb of loop → collecting duct
ADH plays a role in the feedback loop that controls the __ of water in the body. This is called __.
amount; osmostat
Describe the pathway for osmostat.
hypothalmic osmoreceptors sense change in amt of water → stimulate hypothalamus/pituitary to secrete ADH or thirst response
ADH → kidney → H2O reabsorption
thirst → drinking behavior → H2O intake
→ body fluid osmolality (inc in osmolarity)
brings osmolarity back to normal range
__ facilitate fluxes that concentrate urine.
narrow interstitial spaces
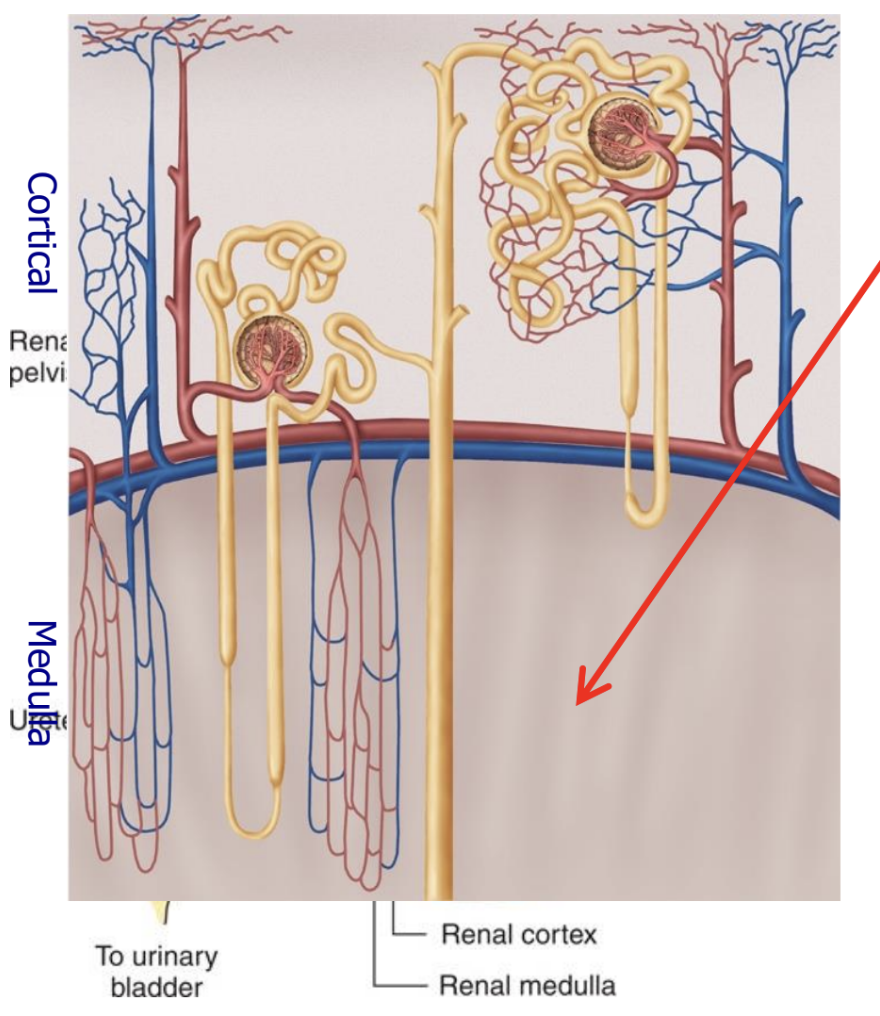
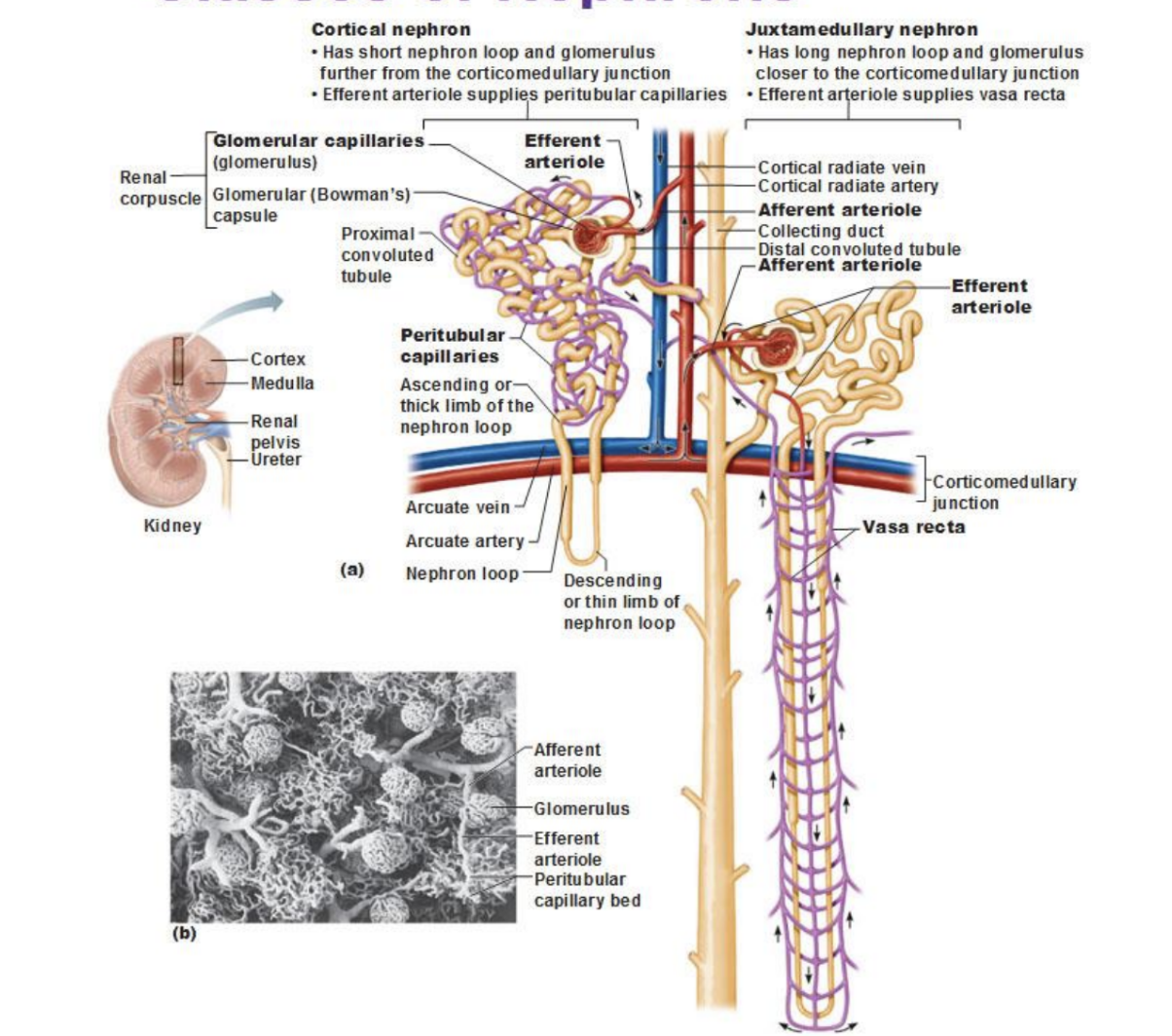
What are the 2 classes of nephrons? How are they different?
juxtamedullary nephron
long nephron loop and glomerulus closer to corticomedullary junction
efferent arteriole supplies vasa recta
cortical nephron
short nephron loop and glomerulus farther from corticomedullary junction
efferent arteriole supplies peritubular capillaries
Countercurrent multiplication is a function of the __
loop of henle
thin descending & ascending limbs
thick ascending limb
countercurrent multiplication = transferring osmolytes from thick ascending limb to descending limb
What is the single effect of the thick ascending limb?
active salt transport out of thick ascending limb → dilutes tubular fluid and increases osmolarity of interstitial fluid
How does the single effect of the thick ascending limb affect the thin segments?
causes osmotic gradient that pulls water out of thin descending limb
Osmolality of thin descending limb [inc/dec] as consequence of the process that [inc/dec] osmolality of thick ascending limb.
inc; dec
Osmolality is transferred from __ and __ limb.
ascending; descending
The size of the osmotic gradient depends on the __
length of loop of henle (LH)
For humans, a normal osmotic gradient is __
1400 mOsmol/L
__ channels are sensitive to ADH dehydration.
Na-K-2Cl
Urea is a product of __ catabolism.
amino acid
Urea contributes to __ gradient.
osmotic
__ regulates urea channels in the __ medullary collecting tubule.
ADH; inner
Urea is first concentrated in the __ collecting tubule.
outer
Urea is then reabsorbed from the __ collecting tubule into the __.
inner; medulla
In the medulla, it augments __ and increases the __ effect.
osmolality; counter-current
What are the 3 functions of ADH?
inc water permeability in principle cells by inserting more aquaporins
increases activity of Na-K-2Cl to enhance osmolality in medulla (increases transport rate in thick ascending limb)
stimulates UT1 (urea transport) production to enhance osmolality in medulla through urea reabsorption (in inner collecting duct)