Gas exchange/Transoort and pH
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
What is the primary purpose of breathing?
The purpose of breathing is to provide a continual supply of fresh O2 for pickup by the blood and to constantly remove CO2 unloaded from the blood.
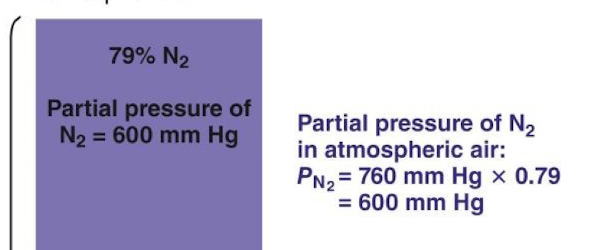
What is the formula for calculating the Partial Pressure of gas X (Px)?
Px = percentage of concentration of the specific gas in a mixture of gases x total pressure of all gases
How is the partial pressure of a gas dissolved in a liquid determined?
The partial pressure of a gas dissolved in a liquid is taken to be that partial pressure of gas that would be in equilibrium when that gas is in contact with the liquid
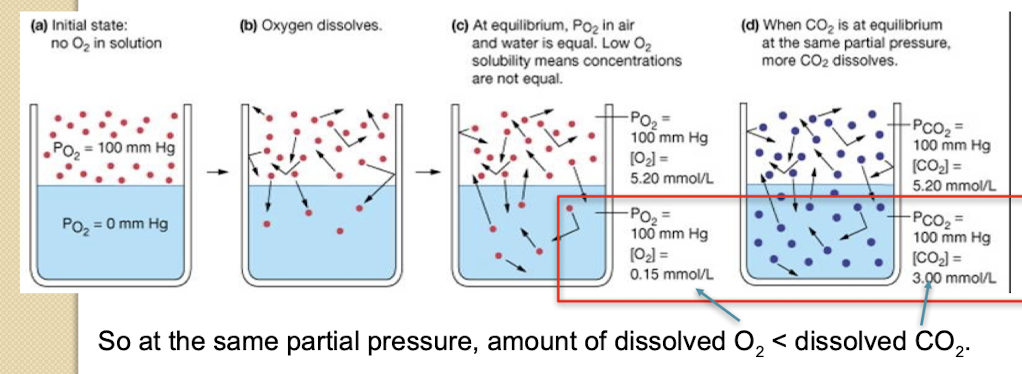
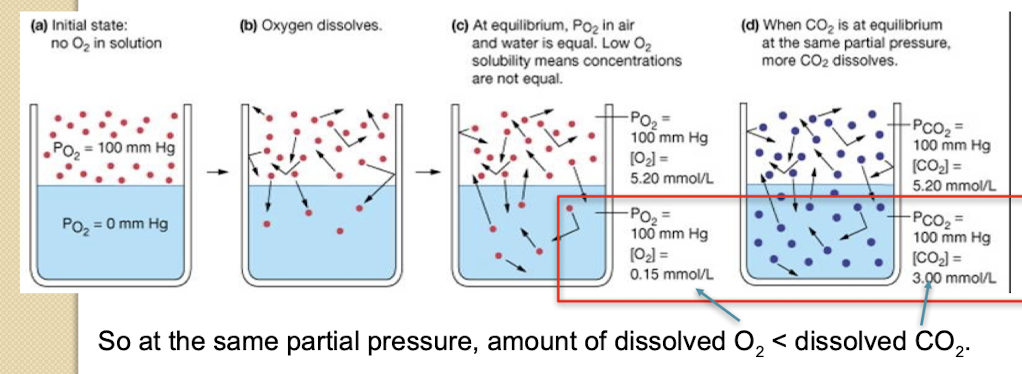
What two factors determine the amount of gas dissolved in a liquid?
The amount (concentration) of a gas dissolved depends upon its partial pressure above the liquid and its solubility in that liquid.
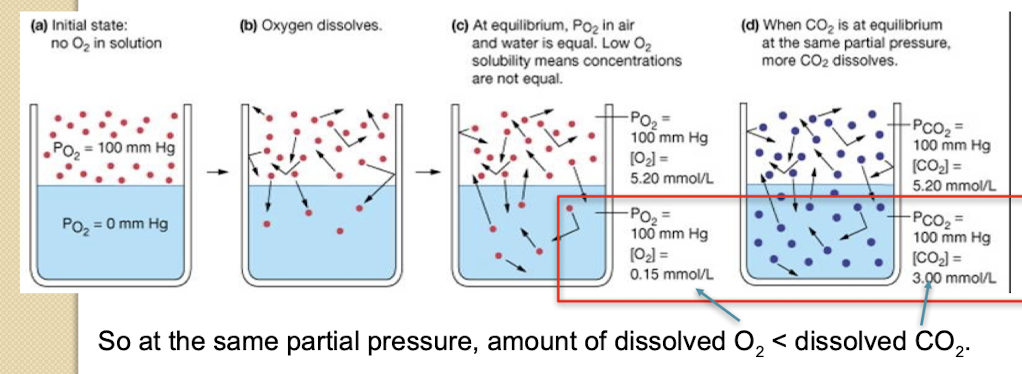
When comparing O2 and CO2 dissolved in liquid at the same partial pressure; which gas has a higher concentration?
The amount of dissolved O2 is less than the amount of dissolved CO2. Oxygen has lower solubility
What is the partial pressure of CO2 (PCO2) in atmospheric air at sea level?
PCO2 = 0.2 mmHg.
Why is alveolar air composition different from inspired atmospheric air (Reason 1)?
As atmospheric air enters the respiratory passages; exposure to the moist airways saturates it with H2O vapor; which exerts a partial pressure.
What is the partial pressure of H2O vapor at body temperature?
The partial pressure of H2O vapor is 47 mmHg.
Why is alveolar air composition different from inspired atmospheric air (Reason 2)?
Fresh inspired air is mixed with the large volume of old air that remained in the lungs at the end of the preceding respiration.
What is the average alveolar PO2 and how does it compare to atmospheric PO2?
Average alveolar PO2 is 100 mmHg; compared to the atmospheric PO2 of 160 mmHg.
Due to humidification and smaller turnover of alveolar air.
Why does alveolar PO2 fluctuate only slightly during inspiration and expiration (Reason 1)? (instead of increasing significantly with inspiration and decreasing with expiration)
Only a small proportion of the total alveolar air is exchanged with each breath during normal resting ventilation.
This is due to the large volume of residual air remaining in the lungs (lower PO2), which keeps the overall composition stable.
Why does alveolar PO2 fluctuate only slightly during inspiration and expiration (Reason 2)?
O2 continually diffuses from the alveoli into the blood; O2 arriving in the newly inspired air simply replaces the O2 diffusing out of the alveoli into the pulmonary capillaries.
SOOO alveolar PO2 remains pretty much 100mmHg throughout the respiratory cycle/
What is the PO2 of systemic venous blood returning to the lungs?
40 mmHg.
What is the PCO2 of systemic arterial blood leaving the lungs?
40 mmHg.
What purpose does the extra O2 contained in the venous blood beyond that normally consumed serve?
It represents an immediately available O2 reserve that can be tapped by the tissue cells whenever their O2 demands increase.
What important physiological role does the CO2 remaining in the blood after passage through the lungs play?
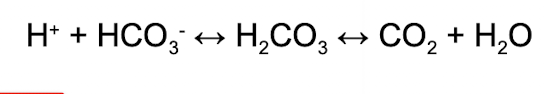
It plays an important role in the body’s acid-base balance. CO2 generates carbonic acid. Furtherore, arterial PCO2 is important in driving respiration
What is the major determinant of the rate of gas transfer across the alveolar membrane?
Partial pressure gradients of O2 and CO2
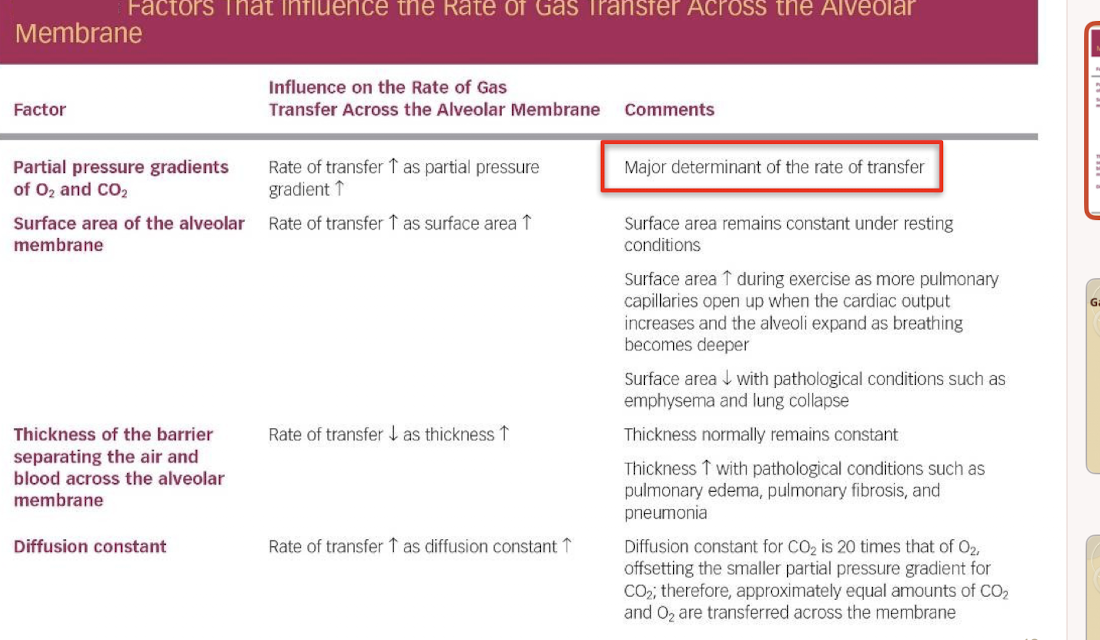
How does increased tissue metabolism affect O2 and CO2 transfer gradients?
Lower cellular PO2 and higher cellular PCO2 (such as in a very actively metabolizing tissue) lead to larger blood-to-cell partial pressure gradients; causing more O2 diffusion from blood into cells and more CO2 movement out.
What percentage of the O2 in the blood is transported by being physically dissolved in plasma and water?
Only 1.5% of the O2 in the blood is dissolved
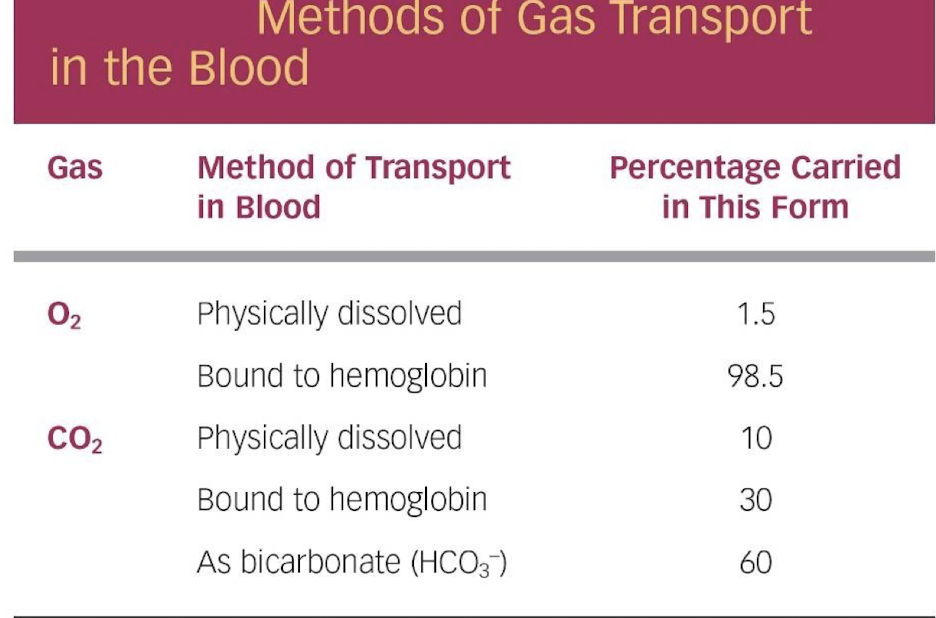
What is most of CO2 in the body transported as? Runne rup?
Bicarbonate, Bound to hemoglobin
Approximately how much dissolved O2 (ml/dl) is present at an arterial PO2 of 100 mmHg? What about O2-Hb
0.31 ml of dissolved O2. 19.5 ml
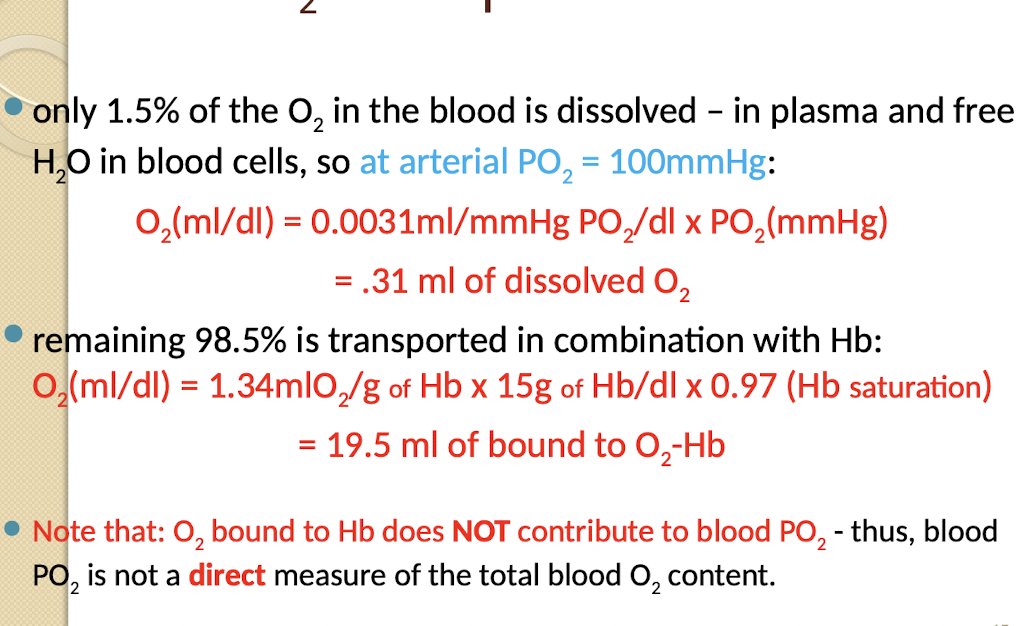
What percentage of O2 is transported in combination with Hemoglobin (Hb)?
The remaining 98.5% is transported in combination with Hb.
Does O2 bound to Hb contribute to blood PO2?
No; O2 bound to Hb does NOT contribute to blood PO2; thus; blood PO2 is not a direct measure of the total blood O2 content.
What is hemoglobin?
Hemoglobin is an iron bearing protein contained within the red blood cells t
Describe the combination formed between Hb and O2?
It is a loose; easily reversible combination.
What is the maximum O2 carrying capacity of one Hb molecule?
Up to four molecules of O2.
When is hemoglobin considered fully saturated?
Hb is considered fully saturated when all the Hb present is carrying its maximum O2 load.
What measures the extent to which Hb is combined with O2?
The percent Hb saturation; which can vary from 0% to 100%.
What describes the relationship between blood PO2 and %Hb saturation?
The relationship is not linear; but follows an S-shaped curve; the O2-Hb dissociation curve
Doubling partia pressure of O2 does not double % Hb saturation
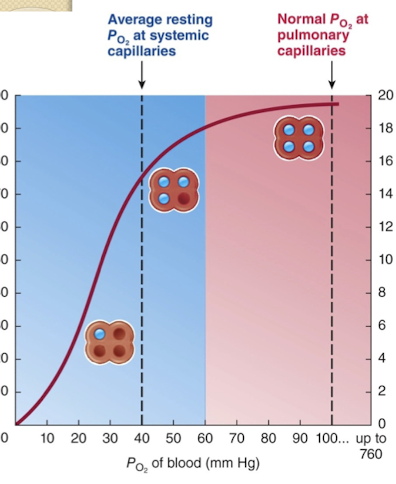
In the O2-Hb dissociation curve; in what PO2 range does the curve flatten or plateau? Why?
Between a blood PO2 of 60 mmHg and 100 mmHg. Within this pressure range, a rise in PO2 produces only a small increase in the extent to which Hb is bound with O2.
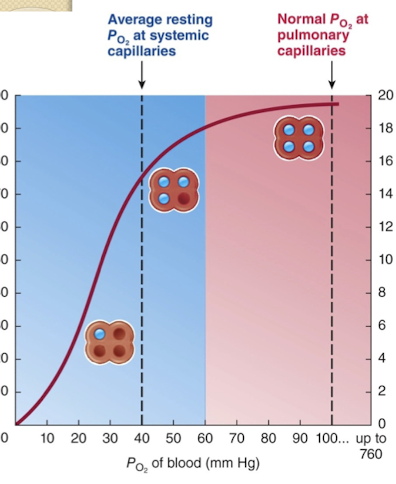
In the O2-Hb dissociation curve; in what PO2 range does a small change in PO2 result in a large change in %Hb saturation?
In the steep lower part of the curve; in the PO2 range of 0 to 60 mmHg.
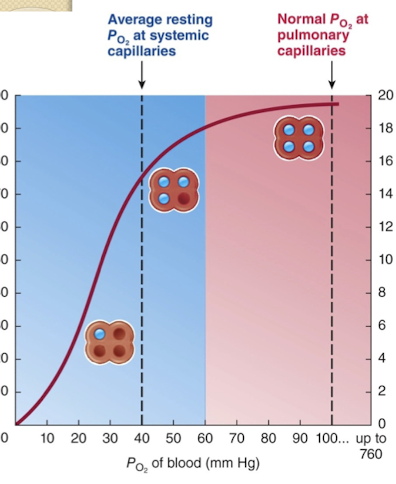
Where is the plateau portion of the curve physiologically relevant? Why?
At the pulmonary capillaries; where O2 is being loaded onto Hb.
The plateau ensures safe O₂ loading in the lungs even if alveolar oxygen levels fluctuate slightly.
Pulmonary capillaries = O₂-loading zone → hemoglobin quickly saturates and stays near 100% on the plateau.
What is the normal %Hb saturation of systemic arterial blood leaving the lungs (PO2 100 mmHg)?
Hb is 97.5% saturated.
If arterial PO2 falls significantly (e.g.; from 100 mmHg to 60 mmHg); how high is the %Hb saturation still maintained?
90% saturated.
If arterial PO2 falls by 40% (from 100 to 60 mmHg); how much is the concentration of dissolved O2 reduced?
The concentration of dissolved O2 is likewise reduced by 40%. THIS IS NOT THE CASE FOR HB bound oxygen
Where is the steep portion of the O2-Hb dissociation curve physiologically relevant?
At the systemic capillaries; where O2 is unloaded from Hb.
Steep portion = O₂-unloading zone in tissues → small PO₂ drops release O₂ efficiently.
What is the typical PO2 in systemic capillaries?
Approximately 40 mmHg.
What is the typical %Hb saturation of venous blood returning from the systemic capillaries?
75% saturated
Under normal resting conditions; what percentage of HbO2 typically dissociates in the systemic capillaries?
Nearly 25% of the total HbO2 must dissociate (from 97.5% down to 75% saturation) BECAUSE at a PO2 of 40 mmHg 75% is the max Hb saturation
Once O2 is released from Hb; how does it reach the tissues?
The released O2 is free to diffuse down its partial pressure gradient from the red blood cells through the plasma and the tissue cells.
Vignette: If a patient's tissue PO2 drops from 40 mmHg to 20 mmHg due to intense exercise; why is this PO2 drop highly effective in O2 delivery?
This 20 mmHg drop operates in the steep portion of the curve; decreasing %Hb saturation from 75% to 30%; resulting in an additional 45% of total HbO2 unloading its O2
What are the four factors at the tissue level that promote Hb-O2 unloading (shifting the curve to the right)?
CO2, Acidity (H+), Temperature, and 2;3-biphosphogycerate (2,3-DPG) (lots in RBC)
What does a shift to the right of the O2-Hb curve signify?
A shift to the right represents a decrease in O2 affinity
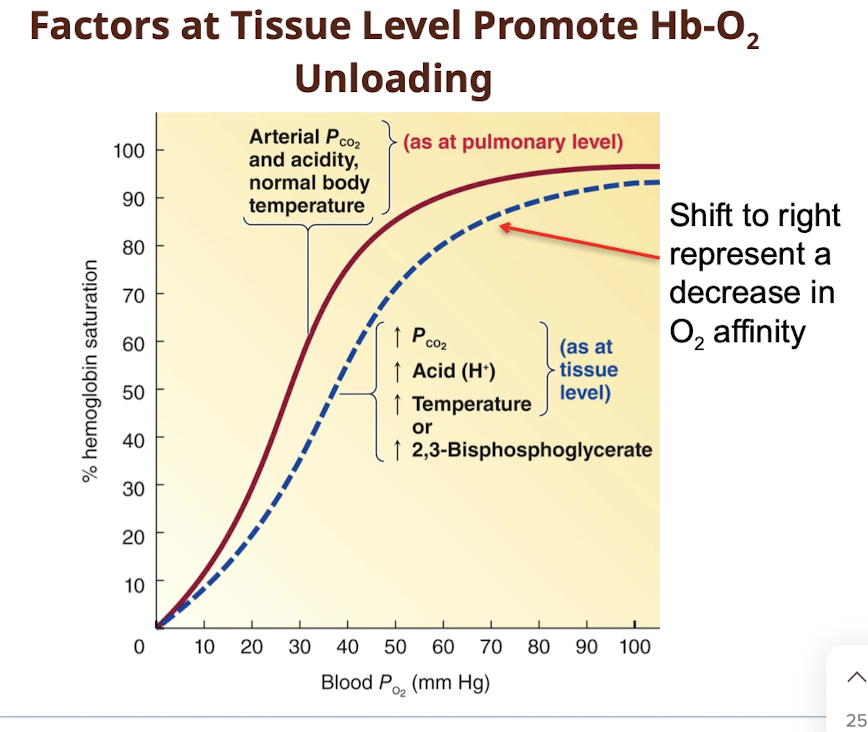
What is the Bohr effect?
The influence of CO2 and acid (H+) on the release of O2.
How do CO2 and H+ promote O2 unloading from Hb?
They combine reversibly with Hb at sites other than the O2-binding sites; reducing Hb-O2 affinity and shifting the curve to the right.
How does increased temperature affect O2 unloading in tissues?
A rise in temperature shifts the O2-Hb curve to the right; resulting in more unloading of O2 at a given PO2
Why does an actively metabolizing cell enhance O2 release from Hb via temperature change?
An exercising muscle or other actively metabolizing cell produces heat; enhancing O2 release from Hb.
What is 2,3-biphosphogycerate (2,3-DPG) and what causes its production?
It is a substance plentiful in red cells; produced by RBCs when O2-Hb is chronically low or during exercise of untrained athletes; which shifts the O2-Hb curve to the right resulting inmore release of O2 at a given PO
How much greater is hemoglobin's affinity for Carbon Monoxide (CO) than for O2?
Hb has 240 times greater affinity for CO than for O2.
Describe the properties of Carbon Monoxide (CO)?
It is an odorless; colorless; tasteless; and nonirritating poisonous gas produced during the incomplete combustion (burning) of carbon products.
Why does CO exposure seriously reduce the O2 content of the blood even if arterial PO2 is normal?
CO competes for the same binding sites on Hb; tying up a disproportionately large share of Hb and making it unavailable for O2 transport.
Why does a victim of carbon monoxide poisoning not feel breathless or attempt to increase ventilation?
Chemoreceptors measure partial pressure of O2 and CO2; which are normal; providing no stimulus for increased ventilation.
How does the solubility of CO2 in blood compare to O2?
The solubility of CO2 in blood is about 20 times that of O2. Therefore, considerably more CO2 than O2 is present in solution at equal partial pressure
What transport mechanism allows HCO3- to leave the RBC and Cl- to enter in systemic capillaries?
The RBC membrane has a HCO3--Cl- carrier that passively facilitates the diffusion of these ions in opposite directions across the membrane (Chloride Shift).
What ion is relatively impermeable to the RBC membrane during CO2 transport? What is the consequence?
RBC’s membrane is relatively impermeable to H+ - consequently, HCO3-, but not H+ diffuse down its concentration gradient out of RBCs
Because oxyhemoglobin has _____ affinity for CO2 than deoxyhemoglobin – O2 release from hemoglobin ____its affinity for CO2.
lower, increases
What is the Haldane effect?
The increased capacity of deoxygenated hemoglobin (deoxyhemoglobin) to bind and carry CO2.
Why does venous blood carry more total CO2 than arterial blood?
Because of the Haldane effect; deoxygenated hemoglobin has an increased capacity to bind and carry CO2.
How does the presence of O2 influence CO2 transport (Haldane effect)?
Oxyhemoglobin has lower affinity for CO2 than deoxyhemoglobin; so O2 release from Hb increases its affinity for CO2.
Where is CO2 uptake facilitated and where is CO2 release facilitated by the Haldane effect?
CO2 uptake is facilitated in the tissues (where O2 is low); and CO2 release is facilitated in the lungs (where O2 is high).
List the four categories of hypoxia?
Hypoxic hypoxia, anemic hypoxia, circulatory hypoxia, and histotoxic hypoxia.
What condition is characterized by having insufficient O2 for normal cellular respiration?
Hypoxia.
What is the primary characteristic and cause of hypoxic hypoxia? How is it typified?
Low arterial blood O2 caused by respiratory malfunction involving inadequate gas exchange; typified by either normal or reduced alveolar PO2.
What are common causes of hypoxic hypoxia?
Blocked airway; COPD; or exposure to high altitude.
Mechanism: At higher altitude, atmospheric pressure (P_atm) decreases, which lowers the partial pressure of oxygen (PO₂) in inspired air.
What defines anemic hypoxia?
Reduced O2 carrying capacity of the blood while the lungs function normally.
a decrease in circulating red blood cells
an inadequate amount of Hb within the red blood cells or CO poisoning.
What are the typical arterial blood gas measurements in anemic hypoxia?
Arterial PO2 is normal; but the O2 content is lower than normal because of inadequate availability of Hb.
A runner has a reduced total HbO2 content due to severe anemia; while a construction worker has the same reduced total HbO2 content due to CO poisoning. Which patient is likely to be more seriously incapacitated and why?
The construction worker with CO poisoning is more seriously incapacitated because the presence of COHb shifts the O2-Hb dissociation curve of the remaining HbO2 to the left; increasing O2 affinity and further decreasing O2 release to the tissues; whereas the anemic individual may still tolerate moderate work.
If a patient with severe heart failure develops systemic hypoxemia despite normal lung function; what type of hypoxia is this?
Circulatory hypoxia.
What defines circulatory hypoxia?
The lungs function normally; but too little oxygenated blood is delivered to the tissues.
restricted to a limited area by a local vascular blockage - the body may experience circulatory hypoxia in general from heart failure or circulatory shock.
In generalized circulatory hypoxia; what are the typical arterial blood gas measurements?
Arterial blood PO2 and O2 content are typically normal.
What defines histotoxic hypoxia and what is a classic example?
O2 delivery to the tissues (blood flow and arterial PO2 and O2) are typically normal; but the cells cannot use the O2 available to them; e.g.; cyanide poisoning
What is the typical concurrent abnormality seen with CO2 accumulation in most lung diseases?
CO2 accumulates in arterial blood concurrently with an O2 deficit because both O2 and CO2 exchange are affected.
What condition refers to having excess CO2 in arterial blood and what is its cause?
Hypercapnia; caused by hypoventilation.
What condition refers to having below normal arterial PCO2 levels and what is its cause?
Hypocapnia; brought about by hyperventilation.
What determines hypocapnia?
The rate of ventilation exceeds the body's metabolic needs for CO2 removal; causing CO2 to be blown off more rapidly than it is produced.
List the four main categories of Acid–Base Balance disorders?
Metabolic acidosis; Metabolic alkalosis; Respiratory acidosis; Respiratory alkalosis.
List the causes of Metabolic Acidosis?
HCO3- loss (e.g.; diarrhea);
failure to regenerate HCO3- (carbonic anhydrase inhibitor type diuretics);
Renal failure (reduced excretion of acids);
or accumulation of organic acids (e.g.; lactic acidosis; diabetic ketoacidosis)
What are the characteristic presentation features of Metabolic Acidosis?
pH is reduced ([H+] increases); and plasma [HCO3-] decreases.
How does the renal system compensate for Metabolic Acidosis?
Kidneys increase secretion of H+ into urine and increase production of HCO3-.
How does the respiratory system compensate for Metabolic Acidosis?
Lungs compensate by increasing ventilation to blow off CO2; decreasing arterial PCO2 = decreased H+
In an uncompensated state of Metabolic Acidosis; what are the typical acid-base values? pH, PCO2, HCO3
pH decreases; PCO2 is still normal; HCO3- decreases.
In a compensated state of Metabolic Acidosis; what are the typical acid-base values? pH, PCO2, HCO3
pH increases to near normal; but PCO2 and HCO3- remain lower than normal.
List the causes of Metabolic Alkalosis?
Ingestion of alkali (e.g.; Tums: CaCO3); excess vomiting; or diuretics that lead to hypokalemia.
How can diuretics cause metabolic alkalosis?
Diuretics can lead to hypokalemia; which in turn increases pH through cellular K+ efflux and H+ influx into the cell.
What are the characteristic presentation features of Metabolic Alkalosis?
pH increases; and plasma [HCO3-] increases.
How does the renal system compensate for Metabolic Alkalosis?
Kidneys excrete more HCO3- and less H+ in urine.
How does the respiratory system compensate for Metabolic Alkalosis?
Lungs compensate by decreasing ventilation; which increases PCO2.
In an uncompensated state of Metabolic Alkalosis; what are the typical acid-base values? pH, PCO2, HCO3
HCO3- increases in the body; pH increases; PCO2 is still normal.
In a compensated state of Metabolic Alkalosis; what are the typical acid-base values?
pH decreases to normal; but PCO2 and HCO3- remain higher than normal
List the causes of Respiratory Acidosis?
Any factor that reduces pulmonary ventilation; such as a lesion or problem in the medulla; drugs depressing breathing; or obstruction of passageways (e.g.; bronchitis; emphysema).
How is Respiratory Acidosis characterized in presentation?
pH decreases because respiration is partially blocked; CO2 is retained so PCO2 increases; and [H+] increases.
How do the kidneys compensate for Respiratory Acidosis?
Kidneys increase excretion of H+ in urine AND generate HCO3-; leading to an increase in plasma HCO3- [
In an uncompensated state of Respiratory Acidosis; what are the typical acid-base values? pH, PCO2
PCO2 increases because ventilation is impaired; so pH decreases.
In a compensated state of Respiratory Acidosis; what are the typical acid-base values? pH, PCO2, HCO3
pH increases to normal; but PCO2 and HCO3- are higher than normal.
List the causes of Respiratory Alkalosis?
High altitude with low PO2 (stimulating increased respiratory rate); or neuroses leading to hyperventilation.
How is Respiratory Alkalosis characterized in presentation?
Ventilation is too high; blood PCO2 decreases; [H+] decreases; and pH increases.
How do the kidneys compensate for Respiratory Alkalosis?
Kidneys increase HCO3- excretion in urine and decrease H+ excretion; resulting in a decrease in plasma [HCO3-].
In an uncompensated state of Respiratory Alkalosis; what are the typical acid-base values? pH, PCO2
PCO2 decreases because ventilation is too HIGH; so pH increases.
In a compensated state of Respiratory Alkalosis; what are the typical acid-base values? pH, PCO2, HCO3
pH decreases to normal; but PCO2 and HCO3- remain lower than normal.