PAM2HP2
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
55 Terms
What is the location of the kidneys in the body?
retroperitoneally, near the level of the lower ribs.
What are the major functions of the kidneys?
regulation of volume/bp, osmolarity, ion balance and pH. excretion of waste. production of hormones.
What is the structure of the renal corpuscle?
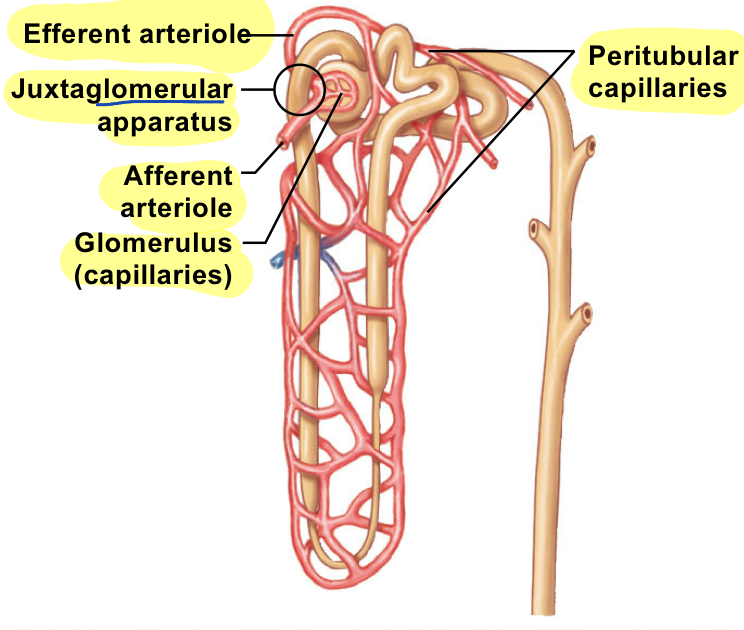
The renal corpuscle is composed of the glomerulus (capillary network) and Bowman’s capsule.
What does the proximal tubule do in the nephron?
reabsorbs water, ions, and nutrients.
Which part of the nephron concentrates filtrate?
The Loop of Henle concentrates filtrate, extending into the medulla.
What are the filtration barriers in the glomerulus?
The filtration barriers consist of endothelial cells, a basement membrane, and podocytes.
What is the primary force driving glomerular filtration?
Glomerular Capillary Hydrostatic Pressure (GHP) is the primary force driving filtration.
How does the myogenic mechanism regulate GFR?
The myogenic mechanism responds to changes in blood pressure by constricting or dilating arterioles.
What is the function of the RAAS system in kidney regulation?
The RAAS system elevates blood pressure and increases glomerular filtration rate (GFR).
What effect does Atrial Natriuretic Peptide (ANP) have on GFR?
ANP increases GFR, promoting sodium (Na+) excretion.
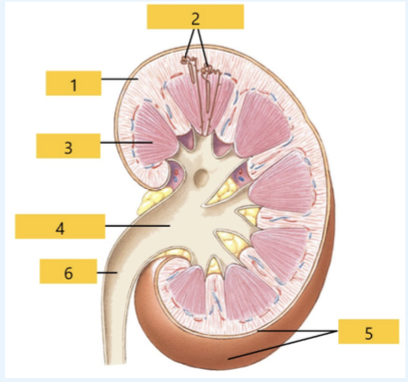
What is structure 1?
Cortex
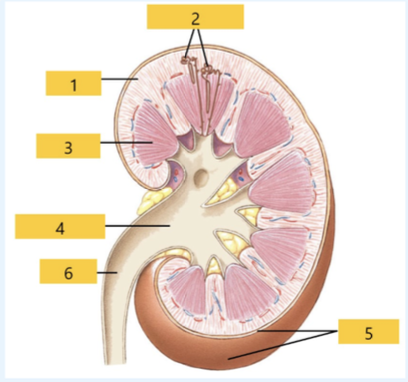
What is structure 2?
Nephron
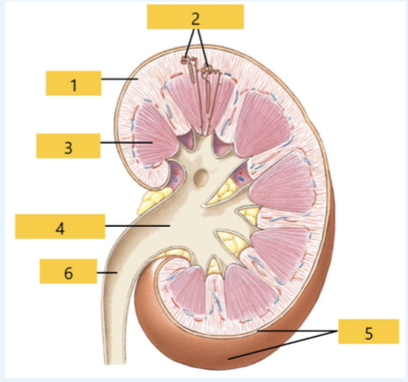
What is structure 3?
Medulla
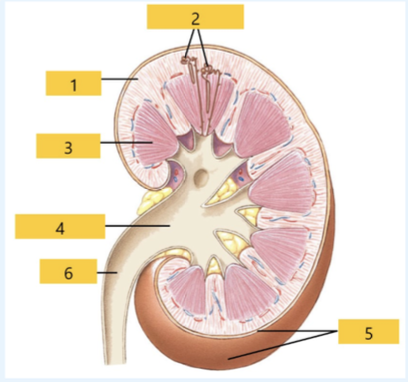
What is structure 4?
Renal pelvis
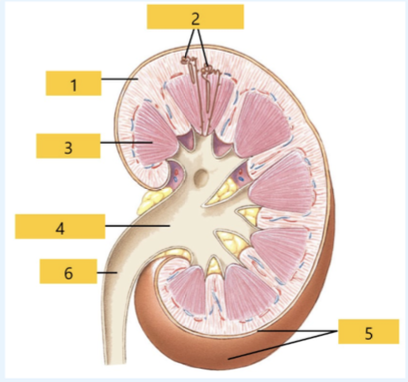
What is structure 5?
Capsule
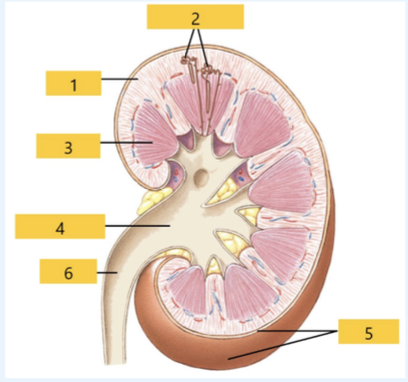
What is structure 6?
Ureter
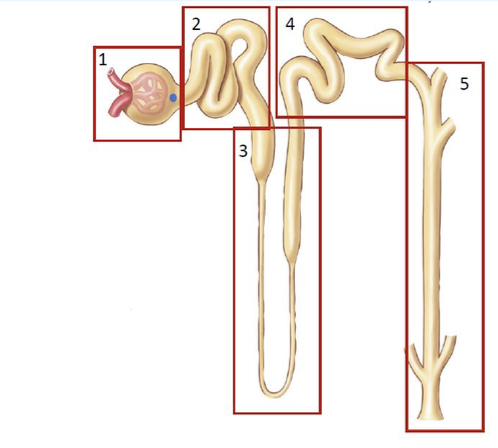
What is structure 1?
glomerulu
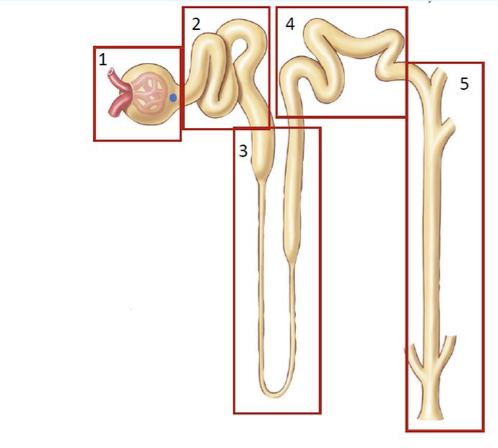
What is structure 2?
proximal tubule
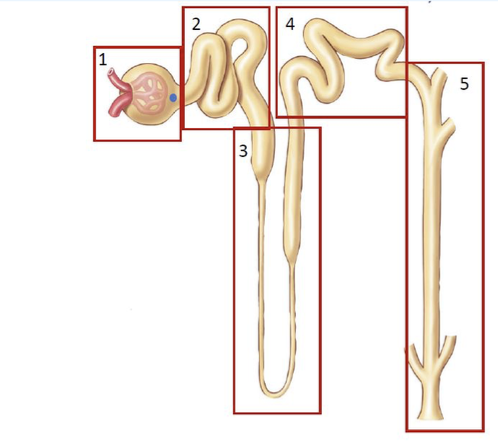
What is structure 3?
loop of henele
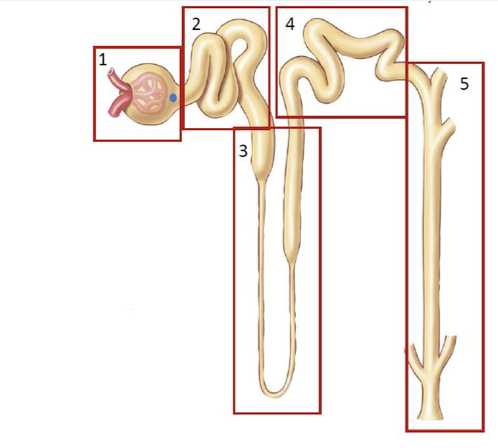
What is structure 4?
distal tubule
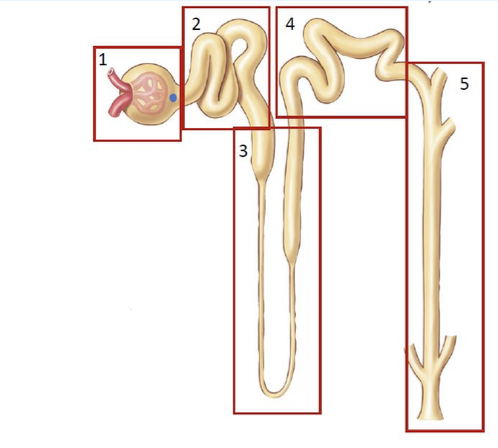
What is structure 5?
collecting duct
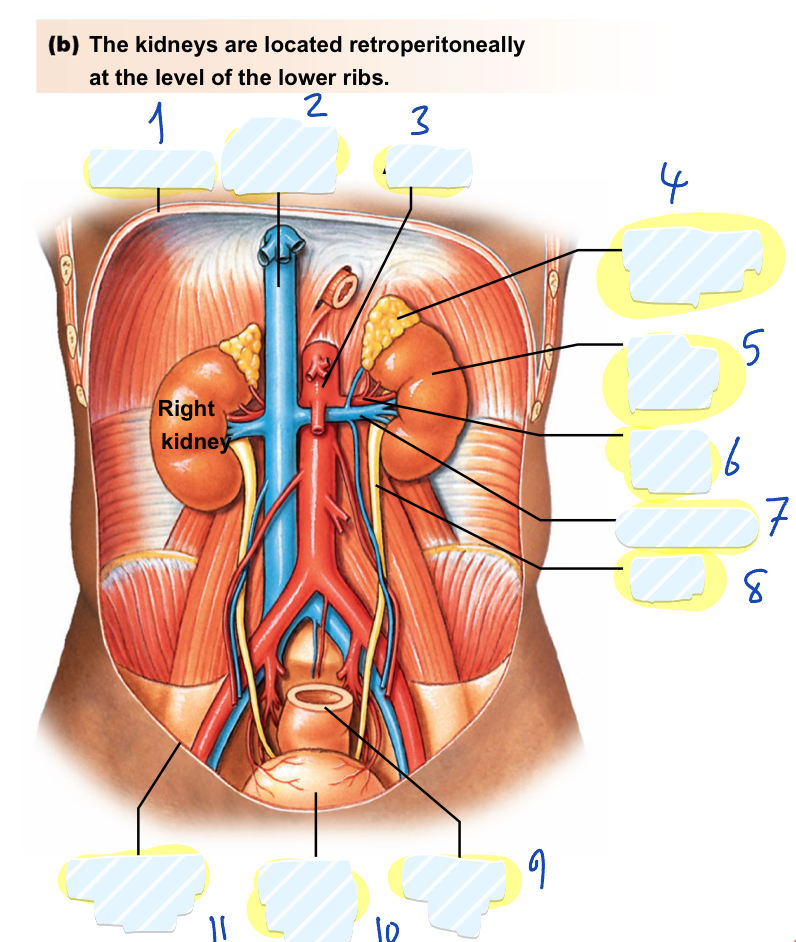
Name structures 1-11
diaphragm
inferior vena cava
aorta
left adrenal gland
left kidney
renal artery
renal vain
ureter
rectum
urinary bladder
peritoneum
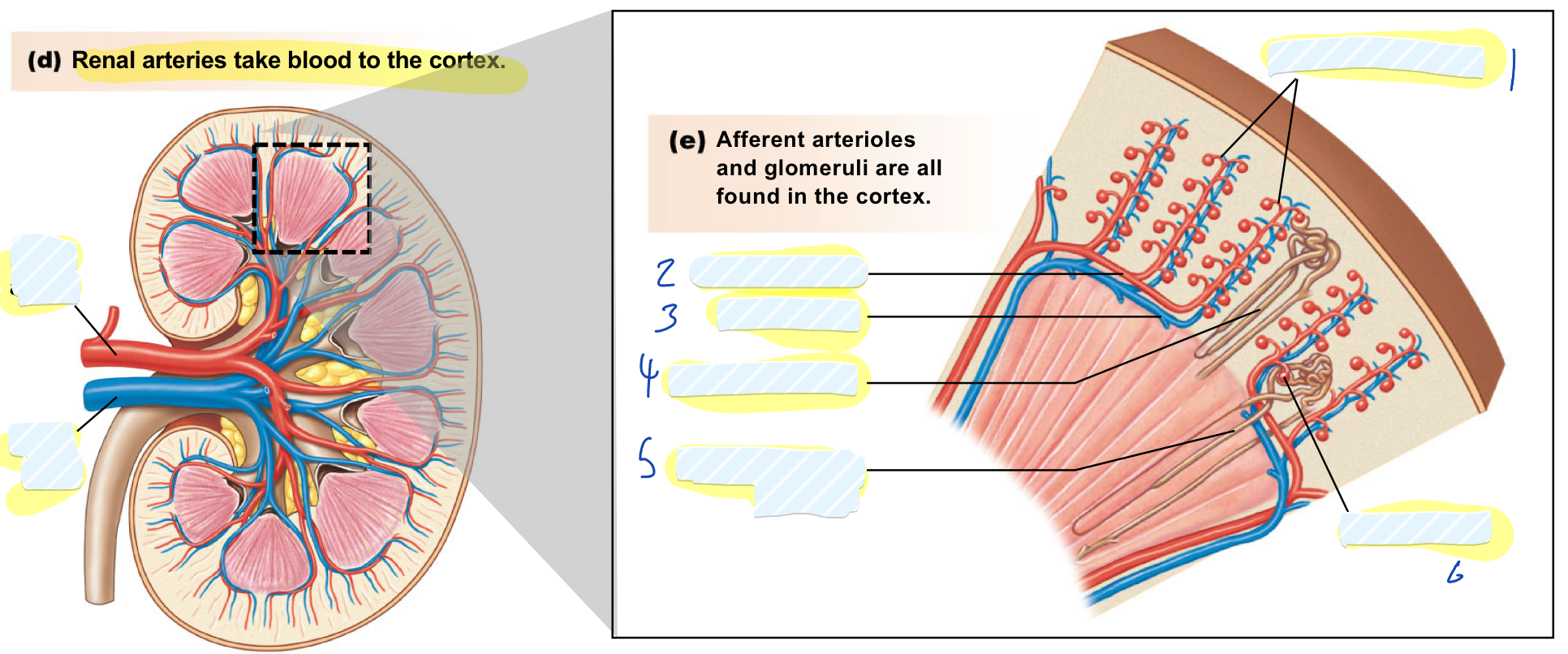
name the structures from 1-6
afferent arterioles
arcuate artery
cortical nephron
juxtamedullary nephron
how much cardiac output the kidneys receive?
1L/min, 20%
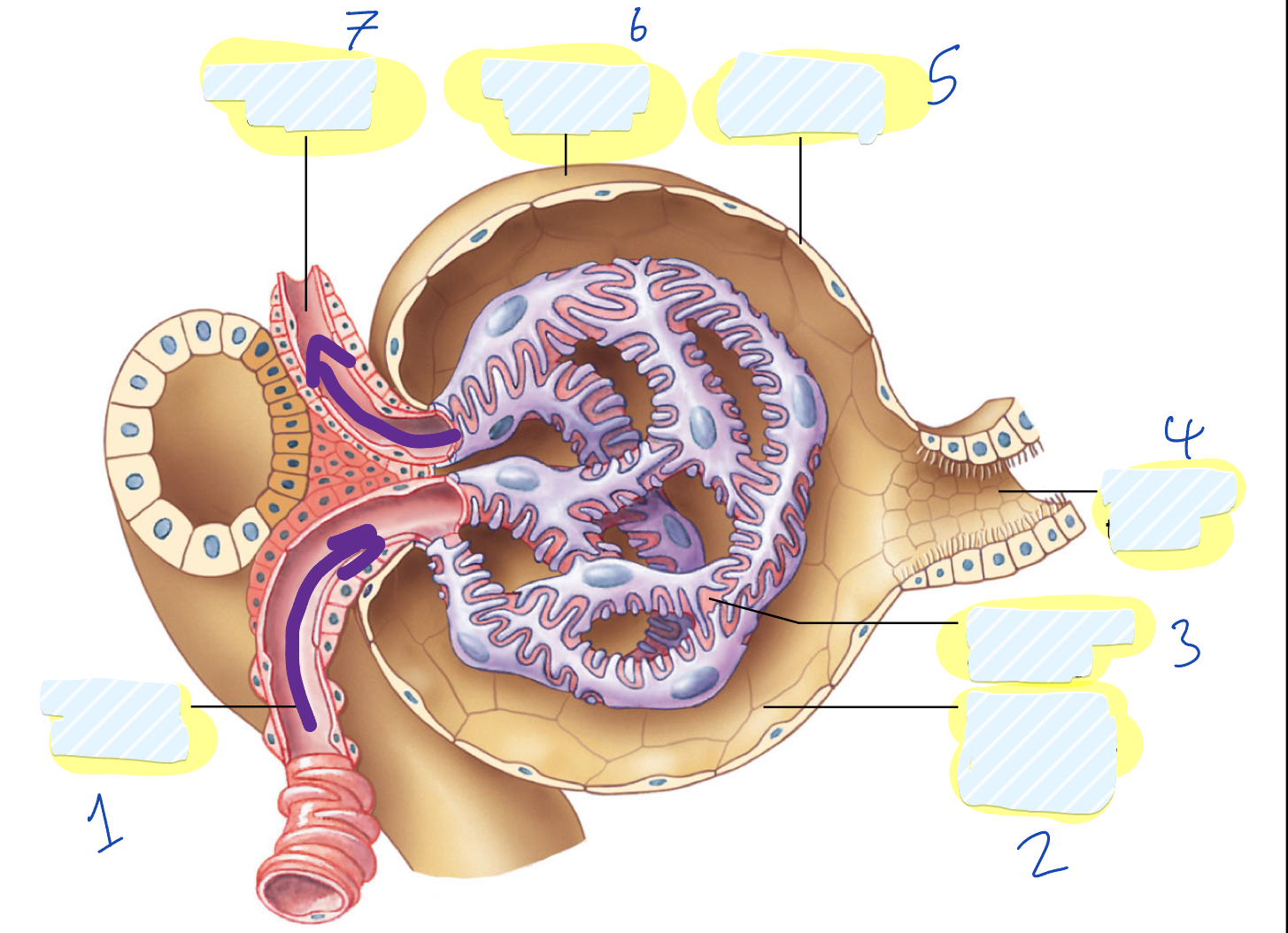
label the structures 1-7
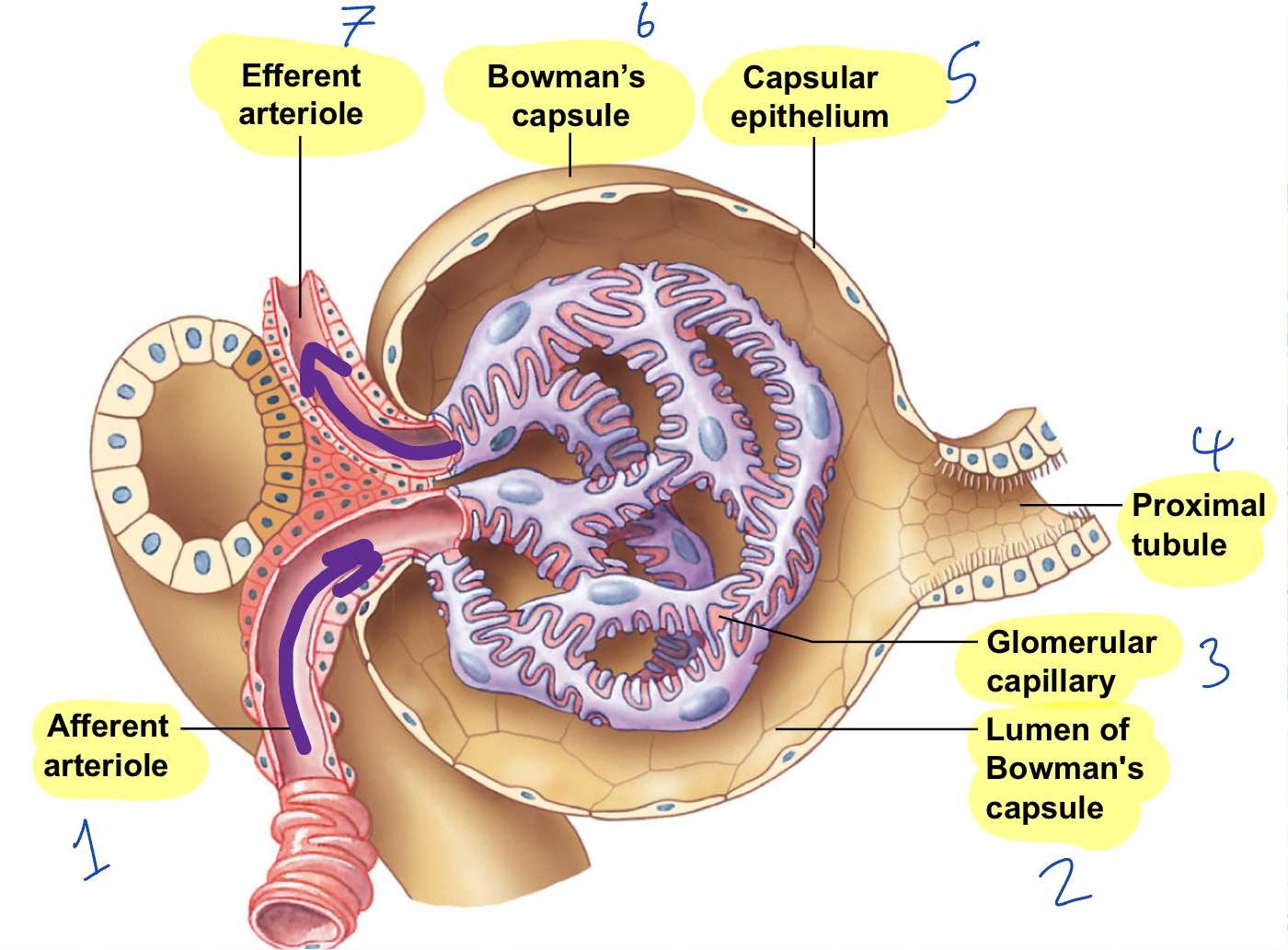
what is this magnified cross section of?
bowman’s capsule
what type of nephron is this?
cortical
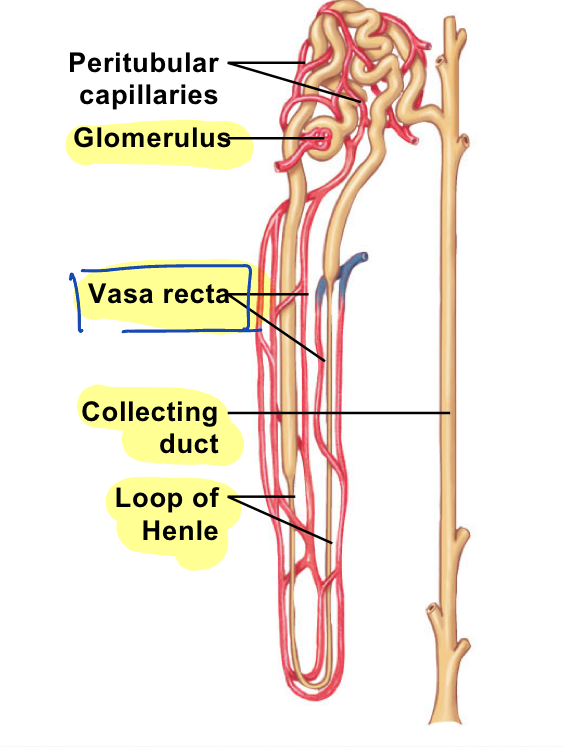
what type of nephron is this?
juxtamedullary
what flow is termed filtration?
moving from glomerulus and into bowman’s capsule
what flow is termed reabsorption ?
moving from tubule into capillaries
what flow is termed secretion?
moving from the capillaries into the tubule
what flow is termed excretion?
moving out of the nephron an d the body
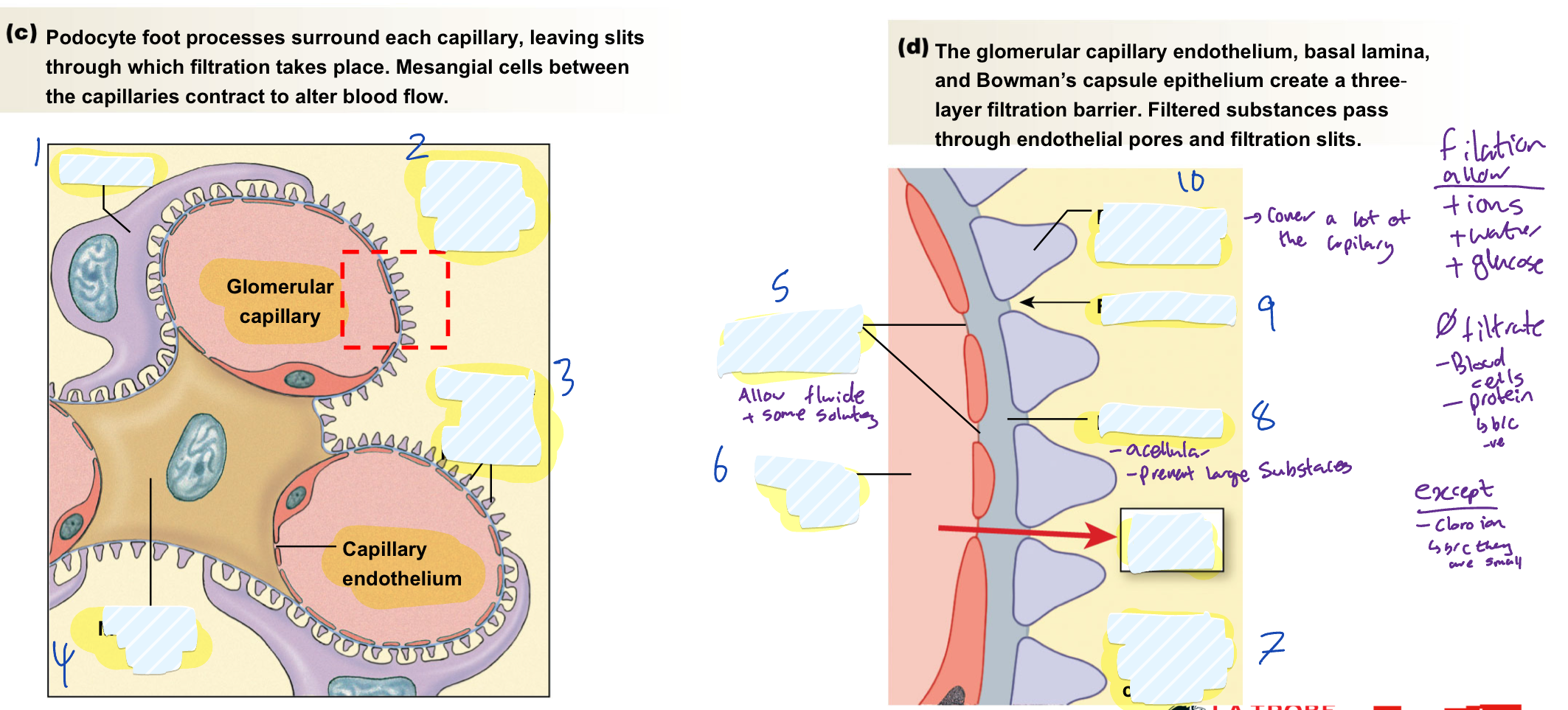
name structures 1-10
podocyte
lumen of bowman’s capsule
podocyte foot process
mesangial cell
pores in endothelium
capillary lumen
lumen of bowman’s capsule
filtered material
filtration slit
podocyte foot process
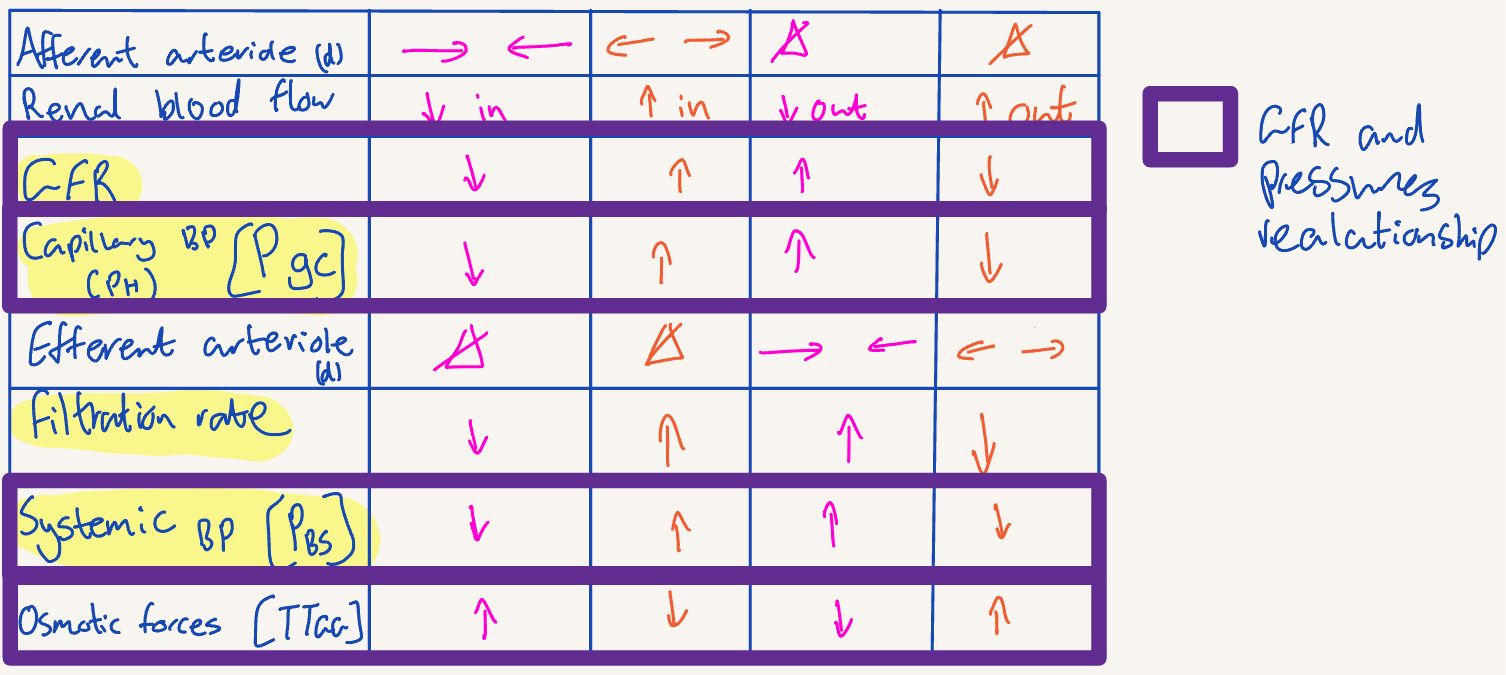
what happens to GFR, Pgc, Pbs, TTgc, filtrate rate and renal flow if afferent arteriole dilate?
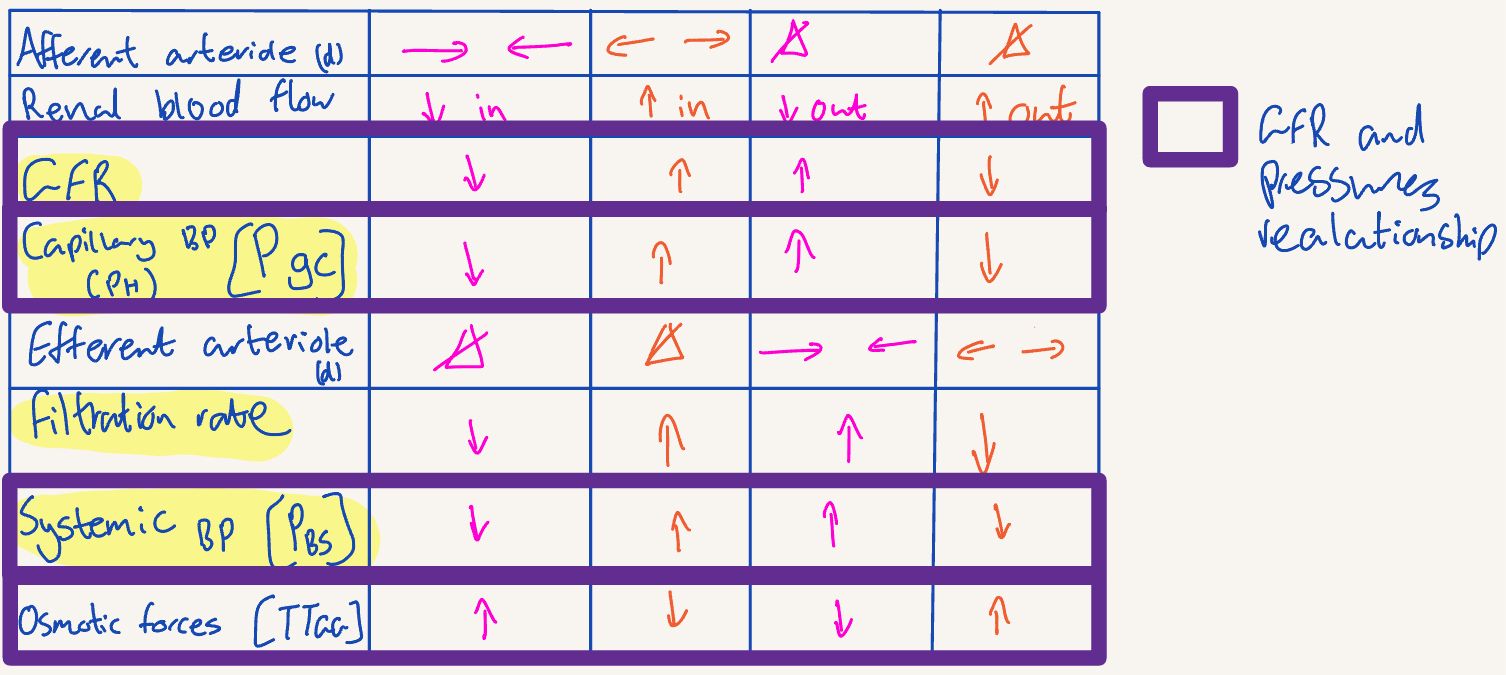
what happens to GFR, Pgc, Pbs, TTgc, filtrate rate and renal flow if afferent arteriole dilate?
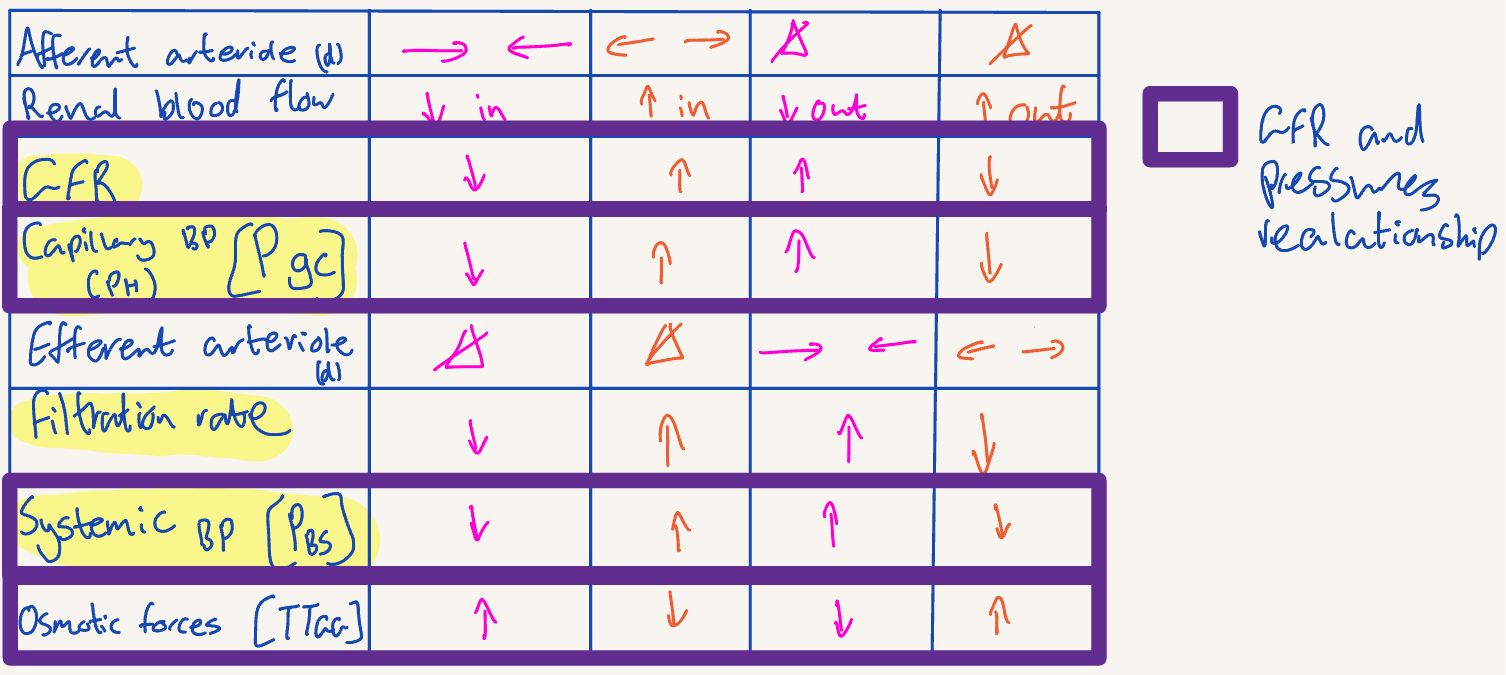
what happens to GFR, Pgc, Pbs, TTgc, filtrate rate and renal flow if efferent arteriole dilate?
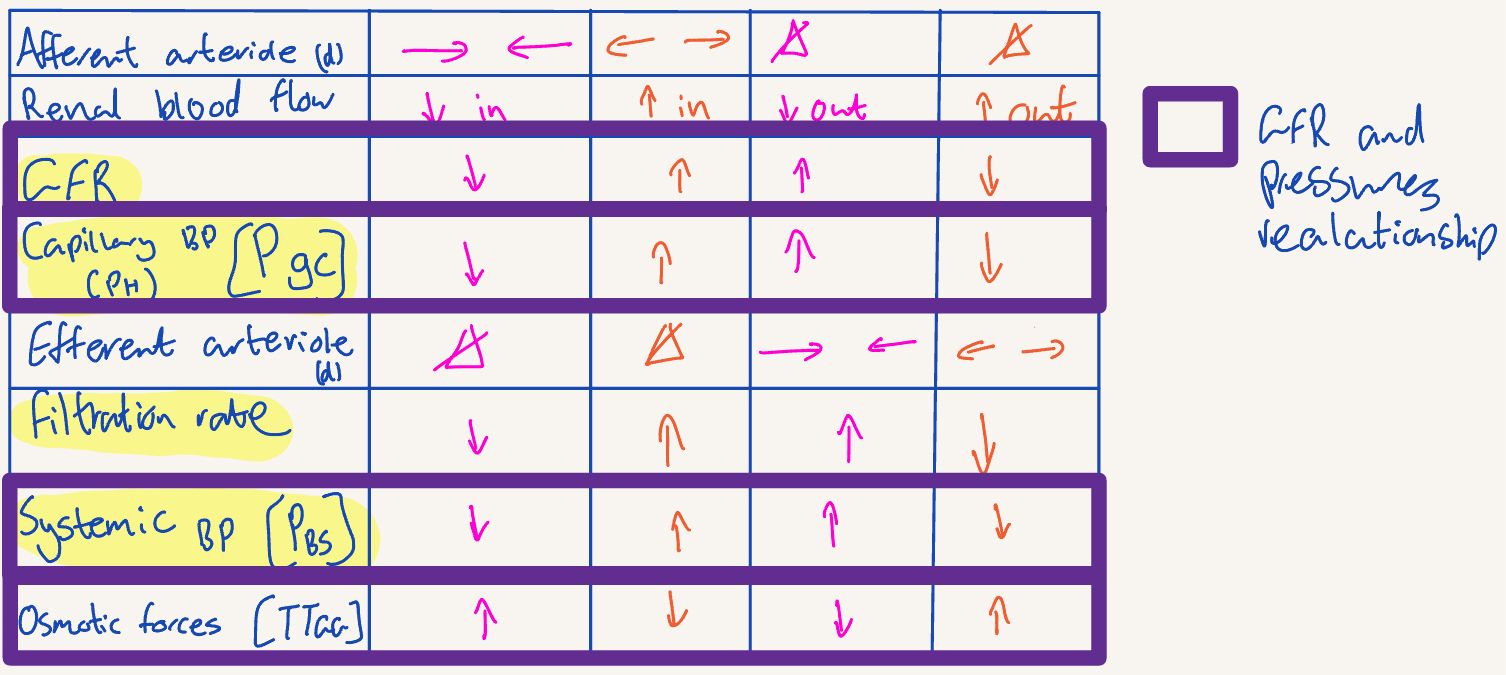
what happens to GFR, Pgc, Pbs, TTgc, filtrate rate and renal flow if efferent arteriole constrict?
Where does sodium reabsorption primarily occur, and is it passive or active?
Sodium reabsorption primarily occurs in the proximal tubule and is an active process.
How does sodium reabsorption drive the reabsorption of other molecules?
Sodium creates an osmotic gradient, allowing water, chloride, glucose, and other molecules to follow via osmosis or cotransport.
What are two key examples of substances reabsorbed in tubular reabsorption, and why is this process important?
Glucose and amino acids are reabsorbed to conserve nutrients, while Na⁺ and water reabsorption help maintain fluid and electrolyte balance.
Why is tubular secretion important in renal function?
Secretion removes waste and regulates pH, enabling the kidneys to excrete unwanted solutes like H⁺ and K⁺.
How does the descending limb of the Loop of Henle contribute to urine concentration?
The descending limb allows water to leave, increasing the filtrate’s concentration as it moves deeper into the medulla.
What role does the ascending limb of the Loop of Henle play in the counter-current multiplier system?
It actively transports Na⁺, K⁺, and Cl⁻ out but is impermeable to water, reducing the filtrate’s osmolarity.
How does the counter-current multiplier system in the Loop of Henle regulate urine concentration?
It creates a high osmolarity gradient in the medulla, enabling water reabsorption in the collecting duct based on ADH levels.
What initiates the involuntary micturition reflex?
Stretch receptors in the bladder wall activate as the bladder fills, sending signals to the spinal cord to initiate the reflex.
How do higher brain centers influence voluntary control of micturition?
They can inhibit or facilitate the micturition reflex, allowing control over the external urethral sphincter for voluntary urination.
What part of the nervous system controls the internal urethral sphincter in the micturition reflex?
The parasympathetic nervous system controls the internal urethral sphincter, triggering its relaxation during the micturition reflex.
What triggers the RAAS, and what effects does angiotensin II have on blood pressure?
RAAS is triggered by low blood pressure or low Na⁺. Angiotensin II causes vasoconstriction, increases ADH and aldosterone secretion, and activates the Na⁺/H⁺ exchanger, all raising blood pressure.
What role does aldosterone play in the RAAS?
Aldosterone promotes Na⁺ reabsorption and K⁺ secretion in the distal nephron, helping to increase blood volume and pressure.
How do natriuretic peptides (ANP and BNP) affect blood volume and pressure?
They increase Na⁺ and water excretion, inhibit RAAS, and cause vasodilation, lowering blood volume and pressure.
Why is K⁺ regulation essential for normal body function?
K⁺ maintains resting membrane potential, preventing arrhythmias and ensuring proper nerve and muscle function.
How do the kidneys contribute to long-term blood pressure regulation?
By adjusting Na⁺ and water reabsorption via RAAS and excreting excess fluids, the kidneys regulate blood volume and pressure over time.
What are some primary causes of kidney disease?
Causes include chronic hypertension, diabetes, infections, obstructions like kidney stones, and polycystic kidney disease.
What are common effects of chronic kidney disease on the body?
Effects include reduced filtration, hypertension, electrolyte imbalance, anemia, metabolic acidosis, and bone disorders.
What symptoms might indicate kidney dysfunction in a urinalysis?
Proteinuria (protein in urine), hematuria (blood in urine), glucosuria (glucose in urine), and cellular casts or crystals.