MS
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
5 main cell types in the CNS
- Neurons (50% of neural cells)
- Neuroglia (50% of neural cells)
- Astrocytes (~80%)
- Oligodendrocytes (~5%)
- Microglia (~10-15%)
- Ependymal cells (~5%)
which cell makes myelin
oligodendrocytes
are there immune cells in the CNS under normal conditions
no
what molecules can easily pass from the blood to the CNS
small lipophilic molecules
importance of BBB
barrier between blood and CNS tissue that regulates the entry of substances and cells to the CNS
prevent the passage of many harmful substances such as toxins, antibiotics and chemicals from the blood to the nervous tissue
Components of BBB / BSB
Tight junctions between the endothelial cells of the capillaries in the nervous tissue primarily form BBB or BSB.
´Astrocytic end-feet “vascular feet” surround and ensheath these capillaries, are partly involved in the formation and maintenance of BBB or BSB
what limit the migration of immune cells from the blood into the CNS
The BBB and the glia limitans together
what is multiple sclerosis
immune mediated demyelination disease of the central nervous system
MS occurs when activated immune cells infiltrate the CNS and attack myelin
BBB becomes leaky, cells penetrate CNS tissue, recruits astrocytes and microglia - leading to inflammation
Target is myelin
what are the most common symptoms of MS
numbness, tingling
walking difficulty
fatigue
pain
muscle spasms
predisposing factors (triggers) of MS
• Genetic : 200 genes have been associated with MS
• Identical twins show 30% chance
• Siblings 2-5% chance
• Sex biased: Female > Male (3:1)
• Pollutants
• Vitamin D deficiency
• Smoking (increases progression rate)
• Excessive salt intake
• Viruses (Epstein Barr Virus, Varicella zoster virus)
which virus is thought to be the possible cause f MS
Epstein-Barr virus
MS Diagnosis
Blood tests, to check for specific biomarkers associated with MS and rule out other conditions
Spinal tap (lumbar puncture), to check abnormalities in antibodies that are associated with MS and also rule out infections and other conditions with symptoms similar to MS.
Neurological and evoked potential tests, visual or electrical stimuli, a moving visual pattern, or short electrical impulses are applied to nerves in legs or arms.
Magnetic resonance imaging (MRI), to check for MS (lesions) in the brain and spinal cord. Normally, intravenous injection of a contrast agent identify active lesions.
clinical classification of MS
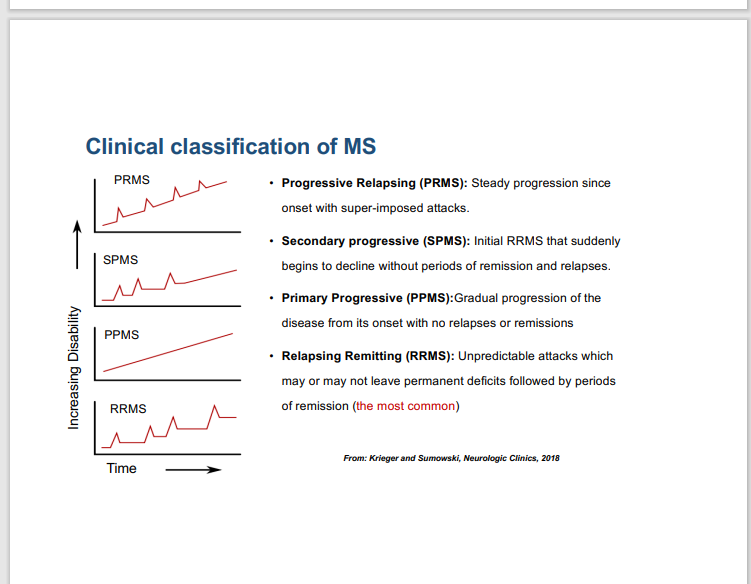
progressive relapsing (PRMS)
steady progression since onset with super-imposed attacks
Secondary progressive (SPMS)
Initial RRMS that suddenly begins to decline without periods of remission and relapses
Relapsing Remitting (RRMS)
Unpredictable attacks which may or may not leave permanent deficits followed by periods of remission (the most common)
Primary Progressive (PPMS)
Gradual progression of the disease from its onset with no relapses or remissions
what is the most common type of MS
Relapsing Remitting (RRMS)
MS mainly affects
younger adults
Does MS involves both immune responses
yes, MS involves both innate and adaptive immune response peripherally and in the CNS
what two immune cells are involved in MS
astrocytes and microglia
where does the MS start from
periphery
Immune response in the pathogenesis of MS
1) Autoreactive T cells recognize a specific autoantigen presented by MHC class II molecules on the cell surface of antigen presenting cells (APCs), such as macrophages, in the systemic immune compartment
2) Activated T cells can cross the BBB in order to enter the CNS. Within the CNS, T cells activate microglia cells/macrophages. Then these cells produce proinflammatory cytokines, release toxic mediators, and increase their myelin phagocytosis and propagating demyelination
3) B cells produce antibodies crossing the BBB or locally produced by infiltrating B cells into the CNS contribute to this process. Autoantibodies activate the complement cascade resulting in the formation of the membrane-attack complex and subsequent lysis of myelin sheath
4) Axon degeneration: The upregulation of Na+ and Ca2+ channels on the axon as well as mitochondrial dysfunction and loss of trophic support contribute to axonal disintegration and degeneration
5) The inflammatory response is regulated by anti-inflammatory cytokines, such as IL-10 or TGF-β, as well as IL-2 inducing programmed cell death (apoptosis) in immunoreactive T lymphocytes
T regulatory cells
good cells
TH 17 cells
breakdown of BBB
Inflammation is dominant in
RRMS
Neurodegeneration is dominant in
SPMS
TNF blocker
inhibits TNF from activated microglia and oligodendrocytes
pathological consequences of immune mediated attacks in MS
Demyelination and neurodegeneration
Progressive MS is associated with axon degeneration causing irreversible and permanent deficits. Without myelin and oligodendrocyte support systems, axons degenerate permanently resulting in permanent neurological impairments
How is MS treated
currently no treatment but disease modifying treatments that reduces immune attacks slowing disease progression and managing MS symptoms
Examples of disease modifying treatments to reduce immune attacks in MS
Corticosteroids, such as oral prednisone and intravenous methylprednisolone, are prescribed to reduce inflammation
Plasma exchange, plasma is removed and separated from blood cells. The blood cells are then mixed with albumin and put back into the body. Plasma exchange may be used if symptoms are new, severe and have not responded to steroids. This will remove proteins that are harmful.
Immunosuppressants: methotrexate, Azathioprine.
why are corticosteroids not that helpful
they suppress T cells including T regulatory cells (which are needed)
Drugs for primary-progressive MS
ocrelizumab (Ocrevus) is the only approved drug in Canada
drugs for relapsing-remitting MS
Interferon beta has been the earliest approved medication for MS
MS attacks often recur when these medicines are stopped
why is myelin repair important
Myelin repair is essential for restoration of structure, conduction of neural signals along axons, and protection of axons from degeneration
Effective treatment to promote remyelination will protect axons from permanent degeneration in progressive MS
Initially in the course of MS, remyelination happens successfully resulting in remission. But as MS progresses, relapses are longer as remyelination becomes challenging
Generation of oligodendrocytes and myelin is a complex process that requires proper differentiation and maturation of OPCs to myelinating cells
Remyelination becomes challenging as in chronic MS microenvironment is not supportive
Vitamin D and MS
• Deficiency in VitD3 is a risk factor for MS
• VitD3 Promotes the Differentiation of Immunosuppressive Regulatory T Cells
• The incidence of MS is increased in northern climates with colder temperature, where vitamin D deficiency is common. Since exposure of the skin to ultraviolet light aids in the conversion of inactive vitamin D to the active form (VitD3), the short days, low UV intensity, and lack of exposed skin common to winter months, decrease the amount of active VitD3 that can be produced
is exercise important for MS
yes, exercise can inhibit inflammation
Medications that have been tested in clinical trials for remyelination
Anti-LINGO
rHIgM22
Clemastine
Domperidone
how does Lingo works
LINGO-1 suppresses oligodendrocyte precursor cell (OPC) maturation and myelination and its inhibition by opicinumab has been tested in clinical trials