Lecture 3 Disorders Featuring Somatic Symptoms
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
What is illness in clinical psychology?
A cluster of symptoms or complaints with a specific cause, course, and outcome

Cluster of symptoms or complaints
It has a specific (organic) cause
A defined course
A specific outcome
What can a symptom be part of?
Disease→biological / medical substrate
Disorders→of disturbances, typically with a known biomedical underpinning, but not necessarily (e.g., depression)
Illness→the feeling of being ill (self-report)
Sickness→not fulfilling social roles, calls sick at work, limited functioning, patient role.
What is a psychological disorder (syndrome)?
Cluster of symptoms (and signs) that co-occur more often than expected by chance (not ‘at random’); often without a clear cause / pathology.
Represents non-normal behavior or experiences, the symptoms belong together.
Clusters are clearly defined (recognizable) and saliently different from other clusters.
Purely descriptive known. the (somatic) cause is not necessarily known.
What makes a psychological disorder recognizable?
Symptoms belong together, are distinct from other clusters, and describe non-normal experiences
What percentage of general physician patients show symptoms without a physical cause?
17% (Greenberg, 2016), consistent with estimates of ~20% for persistent somatic symptoms
What is are the factors leads to somatic symptom?
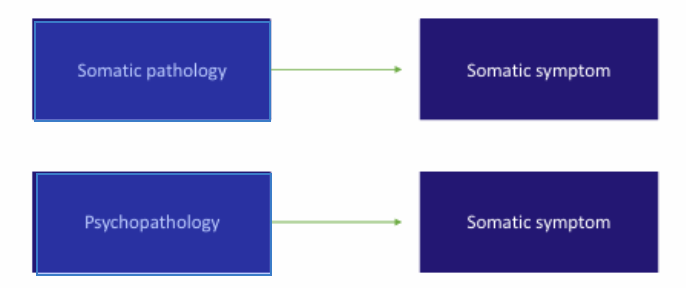
What is are the factor of somatic symptoms?

Predisposing, precipitating and perpetuating factors
Predisposing
Precipitating
Perpetuating
What are predisposing factors?
Factors that make someone vulnerable to developing a disorder (“Why me?”)
What are precipitating factors?
Factors that trigger the onset of a disorder at a specific time (“Why now?”)
What are perpetuating factors?
Factors that maintain or worsen a disorder over time (“Why still?”)
Predisposing Factors
Biological: Genetic vulnerability
Psychological: Personality traits (e.g., poor self-efficacy)
Social: Disorganized attachment
Precipitating Factors
Biological: Poor sleep, substance use/misuse
Psychological: Stressful life events (stressors)
Social: Loss of a significant relationship
Perpetuating Factors
Biological: Poor response to medication due to genetic factors
Psychological: Rumination, impaired reasoning and memory
Social: Role of stigma as a barrier to accessing treatment
Protective Factors
Biological: Adequate diet and sleep
Psychological: Cognitive behavioral strategies
Social: Support from family, friends, and community
Somatic symptom disorder (SSD) in DSM-5 300.82 Criteria
One or more somatic symptoms that are distressing or result in significant disruption of daily life
Excessive thoughts, feelings, or behaviors related to the somatic symptoms
Disproportionate and persistent thoughts about the seriousness of one’s symptoms (cognitions)
Persistently high level of anxiety about health or symptoms (affect)
Excessive time and energy devoted to these symptoms or health concerns (behavior)
Complaints present more than 6 months.
With predominant pain
Persistent
What is the DSM-5 Specify severity:
Mild→Only one of the symptoms specified in Criterion B is fulfilled.
Moderate→Two or more of the symptoms specified in Criterion B are fulfilled.
Severe→Two or more of the symptoms specified in Criterion B are fulfilled, plus multiple somatic complaints or one very severe somatic symptom.
How prevalent is SSD?
Estimated: 5-7% (exact % still unknown)
Expectation: higher than that for somatization disorder (<1%)
Lower than that of the undifferentiated somatoform disorder (19%)
More common in women than men
Possibly more common in people with medical disorders
Key Point for SSRD
In the DSM-5, it is no longer required to distinguish whether somatic symptoms are medically explained or unexplained. This reflects a shift in how Somatic Symptom and Related Disorders (SSRD) are defined.
What does the Dutch term "SOLK" stand for?
“SOLK” – Somatisch Onvoldoende verklaarde Lichamelijke Klachten→ Somatic symptoms with insufficient medical explanation
What is the updated Dutch term since 2021 for SOLK?
Since 2021: “ALK” – Aanhoudende Lichamelijke Klachten→Persistent Physical Symptoms (PPS)
What is MUSS or MUPS?
Medically Unexplained Somatic/Physical Symptoms
Used when no medical or biological explanation is found after investigation
What is FSD (Functional Somatic Disorder)?
Similar to MUSS; includes functional syndromes like IBS or fibromyalgia.
What is the DSM-5 position on MUSS?
Persistent somatic symptoms (lasting > weeks)
No sufficient biological or medical cause
Must rule out other somatic and psychiatric explanations
Used in Dutch clinical guidelines: Multidisciplinaire Richtlijn SOLK (2013)
Examples of MUSS / FSD Conditions
Non-cardiac chest pain
Fibromyalgia
Chronic fatigue syndrome
Irritable bowel syndrome
Patient Perspective for MUSS / FSD conditions
Many patients prefer somatic explanations
Often resist psychological framing of their symptoms
There's ongoing debate about the terminology
Current preferred term: Persistent Physical Symptoms (PPS)
Prevalence of MUSS / FSD / PPS
Somatic Symptoms in General Population
Prevalence of MUSS (Medically Unexplained Somatic Symptoms)
Somatic Symptoms in General Population
85–95% of people report at least one somatic symptom.
Prevalence of MUSS (Medically Unexplained Somatic Symptoms
General population: 20–26%
Primary care: 25–84%
Secondary care: 35–53%
Most Common Symptoms of MUSS / FSD / PPS
Headache
Backache
Pain in joints
Stomach ache
Fatigue
Nausea
Functional Somatic Disorders (MUSS / PPS)
Pain in joints and muscles→ Fibromyalgia
Fatigue, feeling drained→ Chronic Fatigue Syndrome
Abdominal pain, nausea→ Irritable Bowel Syndrome (IBS)
Headache, dizziness→Tension-related Headache
Comorbidity
Frequent comorbidity between somatic and psychological symptoms.
The more somatic symptoms, the higher the risk of anxiety and depressive disorders.

Depression and Medically Unexplained Somatic Symptoms (MUSS)
69% of patients with Major Depressive Disorder (MDD) present only with physical symptoms
31% present with both psychological and physical symptoms
11% deny emotional complaints altogether
A. Preoccupation with having or acquiring a serious illness.
B. Somatic symptoms are not present or if present, are only mild in intensity. If another medical condition is present or there is a high risk for developing a medical condition (e.g., strong family history is present), the preoccupation is clearly excessive or disproportionate.
C. There is a high level of anxiety about health, and the individual is easily alarmed about personal health status.
D. The individual performs excessive health-related behaviours (e.g., repeatedly checks his or her body for signs of illness) or exhibits maladaptive avoidance (e.g, avoids doctor appointments and hospitals).
E. Illness preoccupation has been present for at least 6 months, but the specific illness that is feared may change over that period of time
F. The illness-related preoccupation is not better explained by another mental disorder (such as somatic symptom disorder, panic disorder, generalized anxiety disorder, body dysmorphic isorder, obsessive compulsive disorder, or delusional disorder, somatic type).
Medical care, including physician visits or undergoing tests and procedures, is frequently used.
Medical care is rarely used
With weakness or paralysis
With abnormal movement
With swallowing symptoms
With speech symptom
With attacks or seizures
With anesthesia or sensory loss
With special sensory symptom (e.g., visual, olfactory, or hearing disturbances)
With mixed symptoms
Symptoms are often triggered by an emotional event (trauma)
The individual does not consciously produce or fake the symptoms→ This distinguishes it from factitious disorder or malingering
A stress experience is assumed to be "converted" into somatic symptoms
This process gives rise to the name “Conversion Disorder”
However, the term Functional Neurological Disorder (FND) is now seen as more precise and less stigmatizing
A. Falsification of physical or psychological symptoms, or induction of injury/disease, associated with identified deception.
B. The individual presents themselves as ill, impaired, or injured, even when there are no external rewards for doing so.
C. The behavior is not better explained by another mental disorder=
Delusional disorder
Another psychotic disorder
Fabricates or induces symptoms in oneself
Often knowledgeable about medicine
Willing to endure pain or invasive medical procedures
Frequent visits to multiple hospitals/doctors
Fabricates or induces illness in a dependent (commonly a child)
Done to assume the sick role by proxy and gain attention or sympathy
Caregiver appears protective, may have medical background
Considered a form of abuse
Falsification is intentional
Motivation: to assume the sick role (i.e., to be seen as a patient)
No obvious external rewards
Considered a psychiatric disorder (listed in DSM-5)
Falsification is also intentional
Motivation: external rewards (e.g., money, avoiding work/military, legal benefits)
Not about being seen as a patient, but about personal gain
Not a psychiatric disorder (not included in DSM-5)
Long history of searching for an answer; frequently undergoes medical assessments
Mentalization→The ability to understand the mental state of oneself or others that underlies behavior
Interpreting or deducing emotions based on bodily sensation
May complain about and reject treatment
May feel rejected by the therapist
High risk of misunderstandings
Difficulties in structuring their narratives
Often reject psychological perspectives on their symptoms
Psychodynamic Theory
Psychological factors (conscious or unconscious) influence somatic symptoms
Little direct evidence supports traditional psychodynamic views (e.g., repressed anger or sexuality)
Textbooks may be overly supportive of this outdated view, particularly regarding Functional Neurological Disorder (FND)
However:
Emotion regulation is often disturbed in FND
Interventions such as hypnosis can help
What does Cognitive Behavioral Theory suggest about symptom maintenance in SSRD?
Symptoms may be maintained or reinforced by rewards (e.g., attention, relief from obligations)
Research does not strongly support the reward-maintenance hypothesis
Secondary gain is acknowledged in both psychodynamic and CBT models
Alternative CBT view→Symptoms may have a communication function, expressing needs or emotions nonverbally
Symptoms may have a communication function, expressing needs or emotions nonverbally
Cultural differences in how emotions are expressed and pathologized
3 Cultural differences in how emotions are expressed and pathologized
Industrialized countries: Pathologize somatic expression of emotion
Chinese culture: Sadness is more stigmatized than somatization
South America: Somatic expression of emotion is relatively common
To motivate us toward goals and resources
Nucleus accumbens, dopamine
Driven, excited, vitality
Wanting, pursuing, achieving, progressing, focused
Detect and respond to danger — “Better safe than sorry”
Amygdala, adrenaline, cortisol
Anxiety, anger, disgust
To manage distress and promote social bonding
Prefrontal cortex, opiates, oxytocin
Content, safe, protected, cared-for, trust
Have received ineffective secondary care
Show psychological symptoms resulting from or accompanying somatic symptoms
May have explained or unexplained symptoms
Conflicts with previous clinicians
Psychological + physical comorbidity
Social limitations comparable to severe psychiatric illness
Medical intake
Physical, psychological, neuropsychological assessments
Psychiatric evaluation
Routine questionnaires
Psychiatrists, GPs, internists
Clinical and neuropsychologists
Psychomotor therapists
Psychosomatic physiotherapists
CBT (Cognitive Behavioral Therapy)
ACT (Acceptance & Commitment Therapy)
PST (Problem-Solving Therapy)
Schema Therapy
Cognitive rehabilitation therapy
Pharmacotherapy (for comorbid depression/anxiety)
What is the Gevolgenmodel ("Consequences Model")?
Somatic symptoms have cognitive, emotional, behavioral, physical, and social consequences that reinforce the problem.