(pt 1) exam #2 - immunohematology (cls 544)
1/89
Earn XP
Description and Tags
abo discrepancies, rh system
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
categories of ABO discrepancies
Group I Discrepancies
Group II Discrepancies
Group III Discrepancies
Group IV Discrepancies
ABO discrepancies (general)
Unexpected reactions in the forward and/or reverse typing
Can appear as extra positive or weak/missing reactions
Must be resolved prior to reporting a patient or donor's ABO group
main causes of ABO discrepancies (generally; 3)
Problems with the patients' serum/plasma
Missing or weak reaction in reverse typing
Unexpected positive result in reverse typing
Problems with the patients' red blood cells
Missing or weak reaction in forward typing
Unexpected positive result in forward typing
Mixed field
Problems with both the patient serum and RBCs
group I discrepancies
Associated with unexpected reactions in the reverse typing due to weakly reacting or missing antibodies
Depressed antibody production
No ABO antibodies
Discrepant results in reverse typing more common than in forward typing
Common population: newborns, elderly patient, immunocompromised, etc
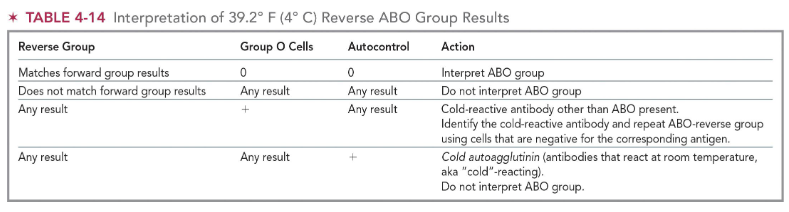
interpretation of 39.2 F (4 C) reverse ABO group results & action:
reverse type: matches forward type results
group O cells: 0
autocontrol: 0
interpret the ABO group as normal; no discrepancy present
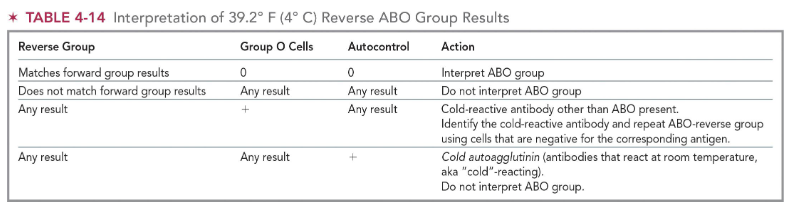
interpretation of 39.2 F (4 C) reverse ABO group results & action:
reverse type: does not match forward type
group O cells: any result
autocontrol: any result
do NOT interpret ABO group; investigate possible cause of discrepancy
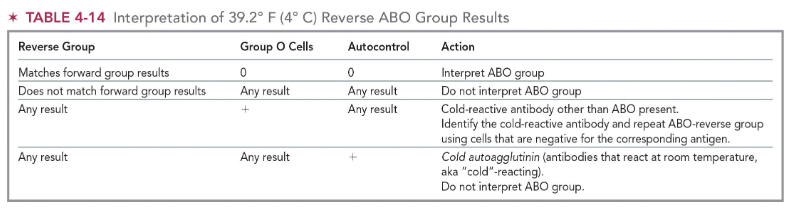
interpretation of 39.2 F (4 C) reverse ABO group results & action:
reverse type: any result
group O cells: +
autocontrol: any result
cold-reactive antibody other than ABO present
identify the cold-reactive antibody and repeat ABO-reverse group using cells that are negative for the corresponding antigen
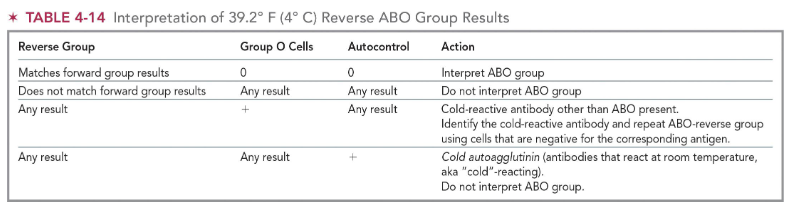
interpretation of 39.2 F (4 C) reverse ABO group results & action:
reverse type: any result
group O cells: any result
autocontrol: +
cold agglutinin (antibodies that react at RT; aka “cold-reacting”)
do NOT interpret ABO group
group II discrepancies
Associated with unexpected reaction in the forward typing due to weakly reacting or missing antigens (the least common)
ABO subgroups or weak ABO subgroups
Diseases that alter the ABO antigen expression
Excessive soluble substances
Enhance weakly reacting antigens with room or colder temperature incubation
Pretreatment of RBCs with enzymes
(group II) causes of unexpected positive reactions in forward type
Substances in plasma if testing done using unwashed cells
Acquired B—bacterial infection
More than one ABO group: mixed field agglutination
True chimerism or mosaicism
RBCs transfusion
Bone marrow/stem cell transplantation
Fetal-maternal bleeding
Unexpected other antibodies
Anti-B reagent
Person makes ABYs that recognize yellow dye
group III discrepancies
Protein or plasma abnormalities result in rouleaux formation
Rouleaux is described as the non-specific agglutination of RBCs
Diseases
Wharton's jelly
Saline replacement technique
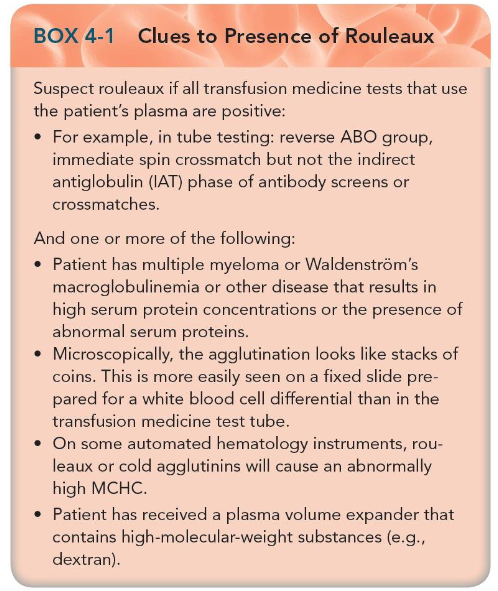
when to suspect rouleaux?
if all transfusion medicine tests that use the patient’s plasma are positive
ex: in tube testing: reverse ABO group, immediate spin crossmatch but not the indirect antiglobulin (IAT) phase of antibody screens or crossmatches
and one or more of the following:
pt has multiple myeloma or Waldenstrom’s macroglobuilnemia or other disease that results in high serum protein/abnormal serum proteins
agglutination looks like stack of coins microscopically
high MCHC
pt has receive a plasma volume expander that contains high MW substances (dextran)
group IV discrepancies
Cold autoantibodies
Unexpected ABO isoagglutinin
Tested with Dolichos biflorus to confirm the presence of an A subgroup
Cis-AB
Inheritance of both A and B genes from one parent on same (cis) chromosome 9
O gene inherited from the other parent
Offspring inherit 3 ABO genes instead of 2
Unexpected non-ABO alloantibodies (Anti-M)
(resolution of ABO discrepancies) anti-A1
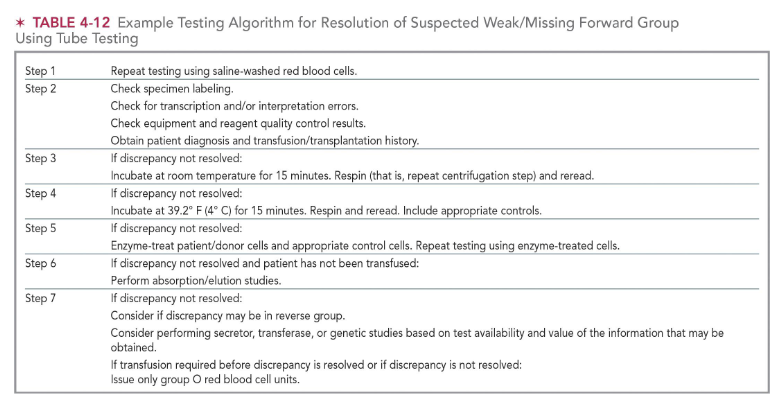
to confirm the presence of anti-A1 in an individual who has not been recently transfused, type RBCs with anti-A1 lectin (see pic for testing algorithim)
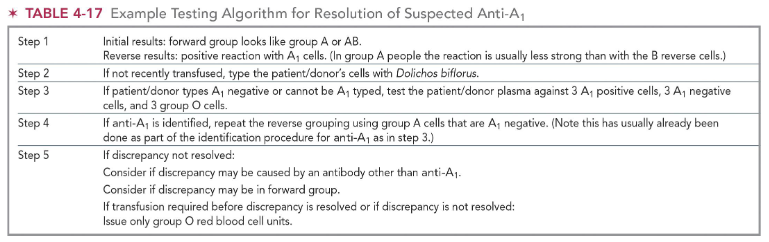
plasma reaction patterns for identification of anti-A1 & interpretation:
A1 pos cells: +
A1 neg cells: 0
O cells: 0
interpretation: anti-A1 present
plasma reaction patterns for identification of anti-A1 & interpretation:
A1 pos cells: some or all +
A1 neg cells: + or 0
O cells: some or all +
interpretation: antibody other than anti-A1 alone or in combination with anti-A1
plasma reaction patterns for identification of anti-A1 & interpretation:
A1 pos cells: 0
A1 neg cells: + or 0
O cells: some or all +
interpretation: antibody other than anti-A1
plasma reaction patterns for identification of anti-A1 & interpretation:
A1 pos cells: 0
A1 neg cells: 0
O cells: 0
interpretation: likely an antibody to a low-incidence antigen
techniques to rule out ABO discrepancies
Check for any clerical errors
Check for any technical errors
Confirm daily reagent QC results
Repeat testing
resolution strategies for ABO discrepancies (general)
Check manufacturer's instructions
Run (or repeat) appropriate controls
Follow your laboratory's standard operating procedure
Blood components from donors with unresolved ABO discrepancies may be diverted for non-transfusion purposes
(ABO discrepancy examples) interpret the following:
Anti-A: 4+ ; Anti-B: 0
A1 cells: 0 ; B cells: 0
likely group A with missing anti-B
alternate: group AB with missing B antigen
(ABO discrepancy examples) interpret the following:
Anti-A: 1+ ; Anti-B: 4+
A1 cells: 4+ ; B cells: 0
likely group B with extra reaction with anti-A
(ABO discrepancy examples) interpret the following:
Anti-A: 1+ ; Anti-B: 4+
A1 cells: 2+ ; B cells: 0
likely group B with an extra reaction with anti-A
alternate: group AB with a weakly reactive A antigen and an extra reaction with A cells
(ABO discrepancy examples) interpret the following:
Anti-A: 0 ; Anti-B: 4+
A1 cells: 4+ ; B cells: 2+
likely group B with an extra reaction with B cells
(ABO discrepancy examples) interpret the following:
Anti-A: 0 ; Anti-B: 0
A1 cells: 0 ; B cells: 4+
likely group A with missing A antigen reaction
alternate: group O with missing anti-A reaction
(ABO discrepancy examples) interpret the following:
Anti-A: 0 ; Anti-B: 0
A1 cells: 0 '; B cells: 0
likely group O with missing antibody reactions
alternate: group AB with missing antigen reactions
(ABO discrepancy examples) interpret the following:
Anti-A: 4+ ; Anti-B: 0
A1 cells: 1+ ; B cells: 4+
likely group A with extra reaction with A cells
(ABO discrepancy examples) interpret the following:
Anti-A: 4+ ; Anti-B: 4+
A1 cells: 2+ ; B cells: 2+
likely group AB with extra reactions with A and B cells
suspect possible rouleaux
(ABO discrepancy examples) interpret the following:
Anti-A: 2+ ; Anti-B: 2+
A1 cells: 4+ ; B cells: 4+
likely group O with extra reactions with anti-A and anti-B
(causes of ABO discrepancies) missing or weak reaction in forward type
ABO subgroup
diseases that alter the ABO antigen expression (leukemia, Hodgkin’s lymphoma)
transfusion of transplantation
excessive solution ABO antigens in pt/donor’s plasma
(causes of ABO discrepancies) missing or weak reactions in reverse type
age (neonates/elderly)
hypogammaglobulinemia (either primary disease or secondary to leukemia/lymphoma)
agammaglobulinemia or other congenital immunodeficiencies
patients on immunosuppressive therapy
transplantation
patients whose antibodies have been diluted by plasma exchange therapy
ABO subgroup
(causes of ABO discrepancies) unexpected positive reaction in the forward group
panagglutinating cells due to changes in red blood cell membrane or interference from plasma proteins
Wharton’s jelly in cord samples
acquired B antigen
B(A) phenomenon
transplantation
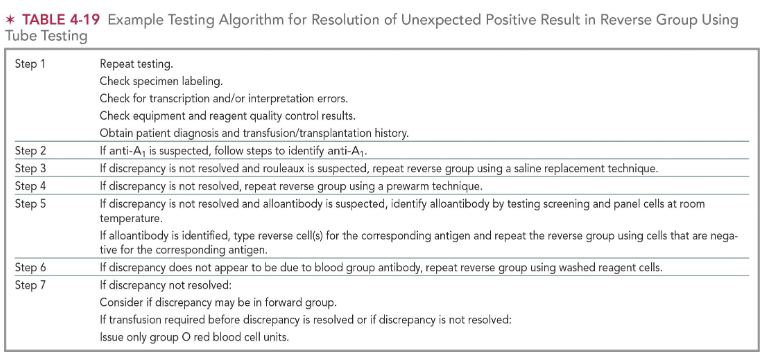
(causes of ABO discrepancies) unexpected positive reaction in reverse type
ABO subgroup
cold reactive auto/alloantibody
antibody to reagent
excess serum protein due to multiple myeloma, Waldenstrom’s, or other disease
treatment with plasma expanders (dextran)
passive ABO antibodies (e.g. transfusion of IVIG, maternal transfer of antibodies to child)
(causes of ABO discrepancies) mixed field agglutination in the forward group
recent transfusion
transplantation
feto-maternal hemorrhage
ABO subgroup, notably A3
chimerism (twins/dispermy)
(causes of ABO discrepancies) different current ABO group from historic ABO group
patient/sample ID error during collection
patient is victim or perpetrator of identity theft
sample mix up during testing
pt has received an ABO nonidentical BMT
intro to Rh blood group system
Rh blood group system is one the MOST important systems in transfusion medicine
Considered second to ABO blood group
Rh antigens are VERY immunogenic (are proteins)
Clinically significant Rh antibodies are common in pregnancy and in blood transfusion recipients
Produced in response to an incompatible transfusion or pregnancy
rh blood group system history (1939-1940)
1939: Levine and Stetson first described a hemolytic transfusion reaction case involving an OB patient
1940: Landsteiner and Wiener discovered an antibody made by rabbits and guinea pigs after injection with Rhesus monkey RBCs ; anti-Rh(D) discovered and named after the rhesus monkeys
For each case, there was a different Rh antibody responsible
Rh retained for the antibody produced by humans (anti-D)
Anti-LW for the Rh antibody produced by rabbits and guinea pigs
Further research led to implication of Rh antibodies as the primary cause of HDFN and a significant cause of HTRs
rh blood group system history (1940s-today)
By the mid-1940s, 5 antigens made up the Rh blood group system
1982: identification and isolation of Rh polypeptides
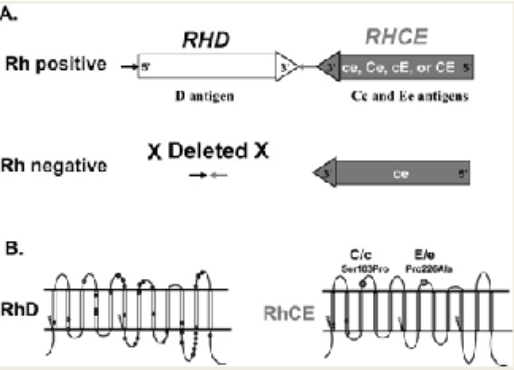
RhD and RhCE proteins
1986: Rh genetic expression controlled by two closely linked genes
RHD and RHCE genes located on chromosome 1
Today: over 60 different specificities within the Rh blood group system
what chromosomes are the RHD and RHCE genes located on?
chromosome 1 (!!!)
biochemistry of Rh antigens
Rh specific antigens reside on transmembrane PROTEINS vs the carbohydrate antigens of ABH antigens
Cross the RBC membrane 12 times, 6 small extracellular loops where the antigens are expressed on the surface
Maintain RBC structural integrity
Maybe act as molecular transporters
Rh phenotypes controlled by two genes
RHD—encodes for D antigen
RHCE—encodes for Cc and Ee antigens
characteristics of Rh antigens
Rh antigens are non-glycosylated proteins expressed on the RBCs
Rh antigens are very immunogenic
Well developed at birth
D antigen is the most immunogenic of all Rh antigens
Remember: D > c > E > C > e
D antigen causes immunization at least 50% of the time in cases where a Rh D-negative individual receives one unit of Rh D-positive RBCs
Number of D antigen sites vary depending on the Rh phenotype
C/c and E/e antigens, co-dominate alleles
If gene present for antigen, it will be expressed on RBCs
order of immunogenicity of Rh antigens
D > c > E > C > e
Rh antigen frequency in Caucasian population (know this!)
D: 85% ; absence of D: 15%
Highest incidence of the Rh-negative type in comparison to other populations
African descent--7%
C: 70%
E: 30%
c: 80%
e: 98%
importance of RhD typing
critical in pretransfusion testing
principal antigen is D
HDFN (Rh-negative mom & Rh-positive fetus)
Hemolytic transfusion reaction (HTR)
Individuals who lack RhD are deemed "Rh-negative"
Lack the D antigen on their RBCs
Individuals who possess RhD are deemed "Rh-positive"
possess the D antigen on their RBCs
Rh pos vs Rh neg
Rh positive individuals have RHD gene
D is the most important Rh antigen
Presence of a single D antigen confers the designation of Rh-positive
Absence of D antigen = Rh-negative
The letter "d" is used to denote the lack of D antigen in Rh-negative individuals
Rh positive phenotype / genetics
Rh-positive individuals may inherit one or two codominant RHD genes, which result in expression of RhD antigen
In addition to the RHD genes(s), two RHCE genes are inherited, one from each parent
Rh negative phenotypes
Rh-negative individuals can arise from at least three different mutations
most often found in individuals falling into the following three different ethnic backgrounds:
European ethnicity → deletion of RHD gene
African ethnicity → RHD pseudogene (don’t produce RhD protein)
Asian ethnicity → alteration of RHD gene (Del phenotype)
Rh associated glycoprotein (RhAG)
RhAG is not part of the Rh blood group system
It is a separate blood group system
The product of RHAG gene: Rh-associated glycoprotein (RhAG)
Located on chromosome 6
RhAG is a co-expressor and MUST be present for successful expression of the Rh antigens
Does not carry the Rh antigens
In the absence of the RHAG gene, multiple molecular defects in the red blood cell membrane can occur
May result in missing or significantly altered RhD and RhCE proteins, affecting antigen expression
where is the RHAG gene located?
chromosome 6 (!!!)
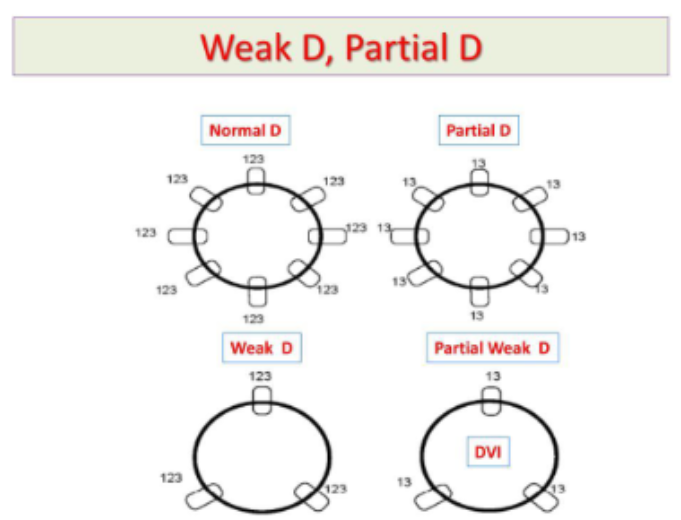
(variations of D antigen) weak D
rarely form anti-D
Position effect: c in trans to D, D is complete
Quantitative: D is complete, fewer number Del
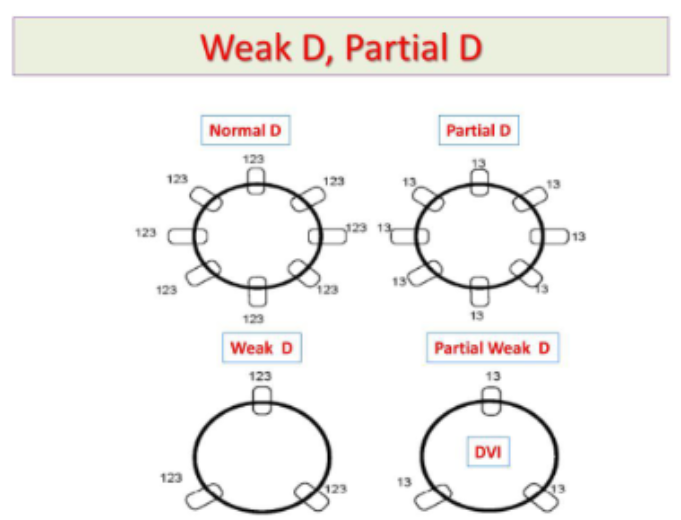
(variations of D antigen) partial D
D antigen is not complete, missing or altered epitopes, can form anti-D against the missing epitope(s)
(Rh deficiency) Rh null
Very rare, lack LW and FY5 antigens
Lack all Rh antigens
Mutation in RHAG gene (regulator-type)
Mutation in RHCE gene, deletion in RHD gene (amorphic type)
characteristics of Rh null syndrome
compensated hemolytic anemia
slight to moderate decreased hgb/hct
reticulocytosis/stomatocytosis
decresed haptoglobin
increased hemoglobin F
absence of FY5 antigen
(Rh deficiency) Rh mod
Partial suppression of RH gene expression caused by mutations in the RHAG gene
Characteristics similar to Rhnull phenotype
(other Rh antigens) G antigen
Serine at position 103 on Rh polypeptides
On most D positive and all C positive RBCs
Combination antigen present on RBCs that have either C or D antigens
Distinction between anti-G, anti-C, and anti-D important in pregnant Rh-negative patients
If anti-G is present in Rh-negative pregnant patient, then Rhogam (RhIG) administration is needed
If anti-C and anti-D present, then Rhogam administration is not indicated
Anti-G looks like an inseparable anti-D,-C
(other Rh antigens) f (ce) antigen
When both c and e antigens are present on RBC and respective genes in cis position or on the same chromosome, the f antigen is expressed
RHCE encodes for c, e, and f antigens
f antigen present in majority of D-negative individuals
Anti-f implicated in HDFN and HTRs
(other Rh antigens) Ce antigen
when C and e in cis position, Ce antigen present
(other Rh antigens) Cw antigen
Low frequency antigen
Antithetical to high-incidence antigen, MAR
Found in 1-2% Caucasian population, rare in people of African descent
Naturally occurring antibodies (anti-Cw implicated in some cases HTRs and HDFN)
(other Rh antigens) V antigen
Rare in Caucasian population (1%): more common in people of African descent
V antigen associated with VS antigen (not antithetical)
IgG antibodies react best at 37 C (some reactivity at RT)
Usually present with other antibodies such as anti-D
Anti-V is not clinically significant
Rh antibodies (general)
Anti-c is the second most important antibody in the Rh blood group
Anti-E is more common
Can be detected as a naturally occurring antibody
Anti-c and anti-e are produced in response to antigenic exposure
Rh antibodies are primarily of the IgG class--able to cross the placenta
Dosage
Do not bind complement
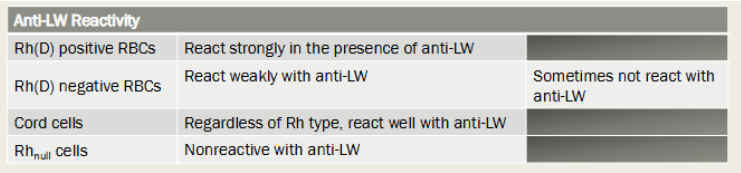
landsteiner wiener (LW) blood group system
Four alleles compose the LW blood group system
LWa, LWab, and LWb
Phenotypically, there is a similarity between the Rh and LW systems
Note the following reactions:
Anti-LW reacts strongly with most D-positive RBCs, weakly (sometimes not at all) with Rh-negative RBCs, and never with Rhnull cells
React well with cord cell regardless of Rh type
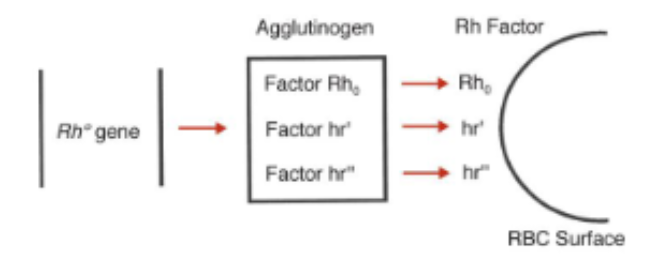
molecular genetic theories of Rh genetic control (2)
Wiener's Agglutinogen Theory
One gene is responsible for defining Rh—the agglutinogen produced contains three Rh factors
Antibody will recognize each factor within the agglutinogen
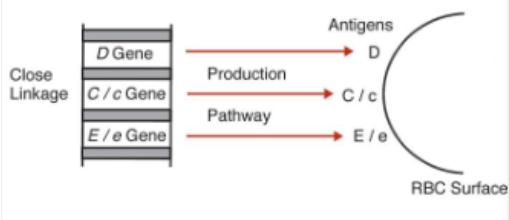
Fisher-Race
Antigens produced by closely linked genes
Each gene produces one antigen on the RBC surface
Wiener’s Agglutinogen Theory
Wiener postulated that a single gene produces a single product that contains separately recognizable factors
This Rh gene produced at least three factors within an agglutinogen
agglutinogen may be considered the phenotypic expression of the haplotype
Gene = agglutinogen Rh factors
Each factor is an antigen recognized by an antibody
Antibodies recognize single/multiple factors or antigens
Nomenclature (R0, R1, R2, RZ, r, r', r", ry)
Rh0 = Dce (0 = no CE)
hr' = Ce = 1
hr" = cE = 2
CE = z or y
Fisher-Race Theory
Fisher and Race proposed that the Rh locus contains three distinct genes that control production of their respective antigens
Each gene was responsible for producing a product (or antigen) on the RBC surface
Genes and gene product defined by same letters and order is DCE
Nomenclature
More widely adopted than Wiener nomenclature
Used to interpret serological workups
Eight possible combinations possible
Dce, DCe, DcE, DCE, dce, dCe, dcE, dCE
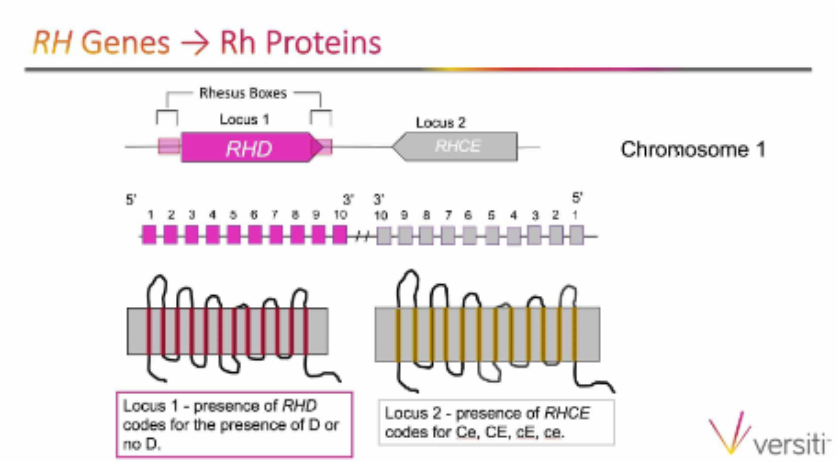
Tippett’s theory (the correct one)
There are two RH genes: RHD and RHCE
closely linked genes on chr 1
These genes control expression of Rh antigens, D and C/c and E/e, respectively
RHD—codes for presence/absence of D antigen
RHCE—codes for presence/absence of C/c and E/e antigens in various combinations
RhCE, rhcE, Rhce, RhCe
Both genes differ by 32 to 35 amino acids (dependent on phenotype)
Each gene possesses 10 exons in its genetic structure
Most Rh-negative phenotypes are the result of the complete deletion of the RHD gene
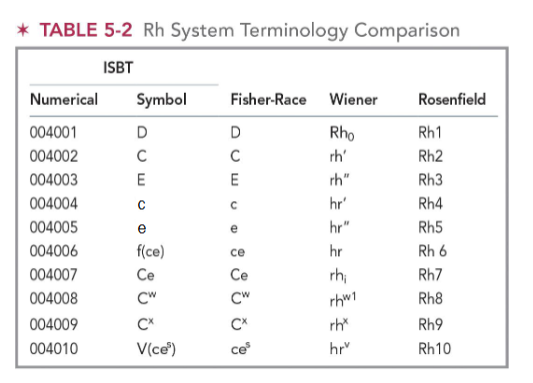
nomeclature (general; 4)
Fisher-Race Terminology
Three closely linked genes within the Rh system (DCE)
Wiener terminology
Individuals inherit Rh antigens as product of single gene at a single locus (Rr)
Rosenfield terminology
Alpha-numeric system (1, 2, 3, 4, 5)
Antigens identified by letters to blood group and numbers to antigens
International Society of Blood Transfusion (ISBT)
System based on genetic classification
Both alphanumeric and strictly numeric system used
(nomenclature) fischer-race
aka DCE terminology
The phenotype of a given RBC is defined by the presence of D, C, e, E, and e antigenic expression
lack of D antigen = d
Weakened antigen expression documented with parenthesis, e.g., (D), (C , (e)
Haplotype is the complement of genes inherited from either parent
DCe--most common haplotype for Caucasian and Asian populations
Dce--most common haplotype for African-Americans
(nomenclature) wiener
aka Rh-Hr
R = presence of D antigen
r = absence of D antigen
Italics and subscripts are used
Rh0 = D
0 = no C and E
Single prime ‘ or 1 = C
no (‘) or 1 = c
Double prime ‘‘ or 2 = E
no (‘‘) or 2 = e
z or y = presence of C and E
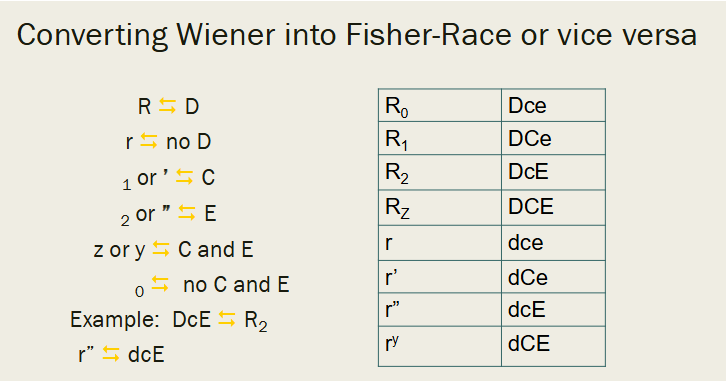
converting Weiner terminology into Fisher-Race & vice versa
R = D / r = no D
subscript 1 or ‘ = C
subscript 2 or ‘‘ = E
subscript z/y = C and E / subscript 0 = no C and E
ex: DcE = R2 ; r’’ = dcE
(nomenclature) rosenfield & coworkers
aka alphanumeric terminology
In the early 1960s, Rosenfield and associates proposed a system that assigns a number to each antigen of the Rh system in order of its discovery or recognized relationship to the Rh system
This system demonstrates the presence or absence of the antigen on the RBC
Rh1, Rh2, Rh3, Rh4, Rh5
D is Rh1, C is Rh2, E is Rh3, c is Rh4, e is Rh5
A minus sign preceding a number designates absence of the antigen
e.g., -1, 2, 3, 4, 5 (D antigen is absent)
If an antigen has not been typed, its number will not appear in the sequence
e.g., 1, 2, 4, 5 (E antigen has not been typed)
(nomenclature) international society of blood transfusion committee (ISBT)
formed the Committee on Terminology for Red Cell Surface Antigens
mandate was to establish a uniform nomenclature that is both eye- and machine-readable
ISBT adopted a six-digit number for each authenticated antigen belonging to a blood group system
first three numbers represent the system and the remaining three the antigenic specificity
Number 004 was assigned to the Rh blood group system, and then each antigen assigned to the Rh system was given a unique number to complete the six-digit computer number
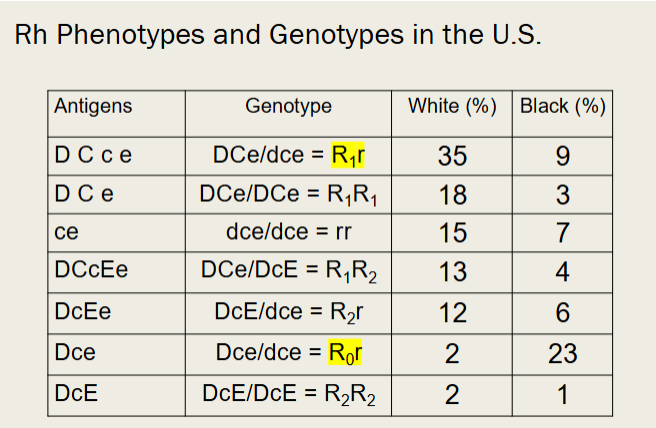
prevelance of the principal Rh haplotypes (whites)
DCe = R1 = 42%
ce = r = 37%
DcE = R2 = 14%
Dce = R0 = 4%
Ce = r’ = 2%
DCE = Rz = <0.01
Rh phenotypes and genotypes in the US (pic)
most prevalent: R1r = DCe/dce
35% of Caucasians ; 9% of African Americans
least prevalent: R0r = Dce/dce
2% of Caucasians ; 23% of African Americans
Rh testing (general)
The presence/absence of D antigen tested for all blood donors and recipients in most countries
Rh phenotype defined by testing with anti-D, anti-C, anti-E, anti-c, and anti-e reagents
An individual's Rh genotype determined by molecular testing (e.g. DNA analysis) or phenotyping in a family study
Weakened expression of D
Rh(D) positive RBCs give readable, macroscopic reactions when tested with anti-D commercial reagent
Some cells may appear Rh(D) negative with some anti-D reagents and positive with others
weak D (Du) testing
Performed to test for weak expression of the D antigen
RBCs may react weakly (2+ or less) or not at all in direct testing with anti-D reagent
Rh typing taken through the AHG testing phase
In tube testing, anti-D tube incubated at 37°C to examine for agglutination
Transfusion considerations
Weak D test must be performed on all Rh-negative blood donors
Only when D and weak D tests negative is unit given Rh(D) negative designation
Weak D patients – transfuse with D negative RBCs
Rh typing reagents (3)
Monoclonal antisera
Made from cell culture
Cell line capable of growing outside a body in liquid medium
Derived from cancer cells or hybridoma
High and low-protein human antisera
Anti-D and Rh control regents made from human plasma divided into high and low-protein formulations
Rh control and Weak D test
Controls used when Rh typing test taken through AHG phase
(sources of error in Rh typing) causes of false positive reactions
contaminated reagents
abnormal proteins in patient/donor plasma causing rouleaux
use of wrong antiserum
failure to follow manufacturer’s directions
cold agglutinins (auto/alloantibodies) in patient or donor plasma
(sources of error in Rh typing) causes of false negative reactions
failure to add antiserum
use of wrong antiserum
RBC suspension too heavy
patient/donor RBC with a variant Rh antigen that does not react w the antiserum
failure to follow manufacturer’s directions
Rh alloantibodies
RBC stimulated
Must be exposed to antigen BEFORE antibody formed
Highly immunogenic
Individuals who have developed anti-D more prone to develop other Rh blood group system antibodies
Rh autoantibodies
Rh specificity to a common Rh antigen or high-prevalence Rh antigen
Weaker reaction when tested with RBCs having normal Rh antigen expression
Controversy over transfusion
Risk of alloimmunization
Patients with autoantibodies increased tendency to produce alloantibodies
characteristics of rh antibodies
are IgG and react optimally at 37 C OR after AHG testing
IgG1, 2, 3 and 4 subclasses of Rh antibodies have been reported
IgG1 and IgG3 are of the greatest clinical significance
RBCs coated with IgG1 and IgG3 are rapidly cleared from circulation (extravascularly) by the reticuloendothelial systems (RES)
Are usually produced following exposure to foreign RBCs
May demonstrate dosage
Enhanced when testing with enzyme-treated RBCs
Often persist for years
Do NOT bind complement
Can cross the placenta
transfusion considerations for Rh types
Rh (D) positive Individuals
May receive D positive or D negative blood products
Rh (D) negative Individuals
Should receive RBC containing products that lack D antigen to avoid immunization
Rh implicated transfusion reactions
D antigen is the most immunogenic antigen outside the ABO system
Clinical manifestations include the following:
Unexplained fever
Mild bilirubin elevation
Decreased hemoglobin and haptoglobin
DAT is usually positive
Extravascular hemolysis
Antibody screen may demonstrate circulating antibody
Elution studies may be helpful
characteristics of intravascular hemolysis in a transfusion reaction
ex: ABO blood group HTR
Hemolysis occurs (inside the blood vessel)
Anemia
↑ Bilirubin ; ↑ LDH
↓ Haptoglobin
Plasma with free hemoglobin
Blood in urine (hemoglobinuria) + urine hemosiderin (free heme)
RBC Morphology: Schistocytes, Reticulocytosis
Complement activation
Primarily IgM antibodies
characteristics of extravascular hemolysis in a transfusion reaction
ex: Rh blood group HTR
Hemolysis occurs via the spleen and reticuloendothelial (RES) mediated → mononuclear phagocyte system
Anemia
↑ Bilirubin ; ↑ LDH
↓ Haptoglobin
Normal plasma hemoglobin
RBC Morphology: Spherocytosis, Reticulocytosis
No complement activation
Primarily IgG antibodies
hemolytic disease of the fetus and newborn (HDFN)
Rh HDFN is often severe
Rh antigens are well developed on fetal RBCs and Rh antibodies are transplacental IgG antibodies
Clinical intervention
Rh-immune globulin (Rhogam) is a purified preparation of IgG anti-D
Administered to D-negative women during pregnancy and after delivery of a D-positive fetus
Rh-immune globulin is effective only in preventing RhD HDFN
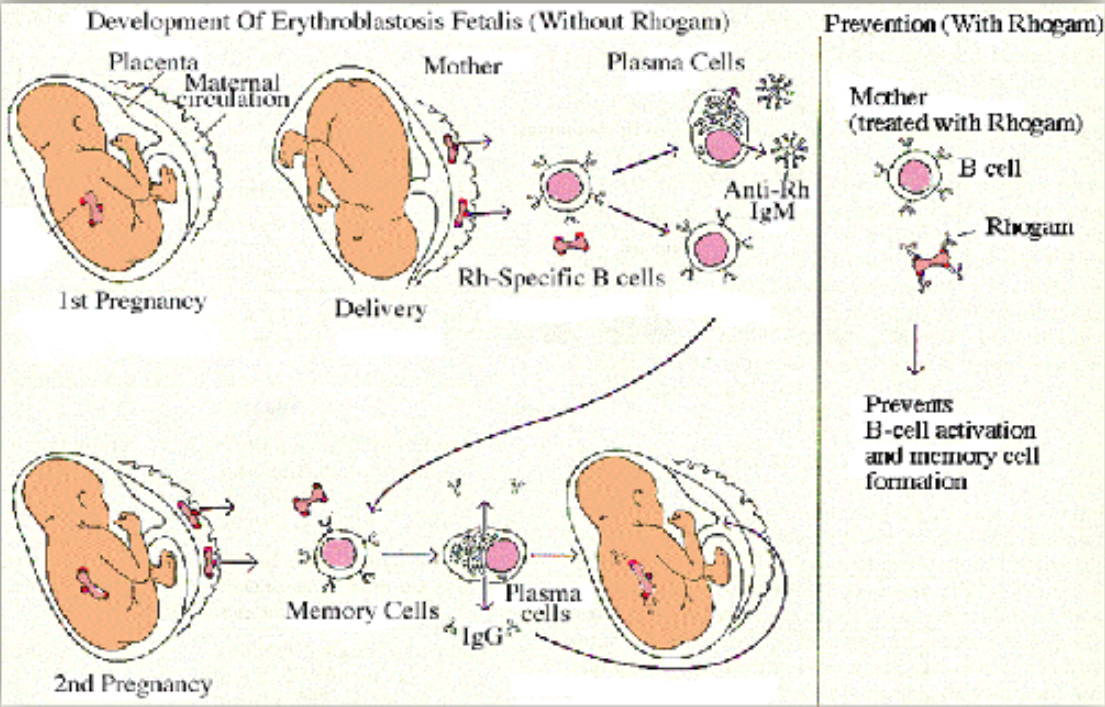
Rh-immune globulin (rhogam)
RhIG prevents immunization against D antigen ONLY and not against other blood group antigens
Rhogam is a solution of concentrated anti-Rh0(D)
Prepared from pooled human plasma from patients hyperimmunized
Contains predominantly IgG anti-D
dosing of rhogam (RhIG)
Two doses (IM)
50-μg
300-μg: Considered a full dose protective against 15 mL of D-positive RBCs or 30 mL whole blood
During pregnancy…
First 12 weeks: 50-μg IM dose indicated for abortion or miscarriage
After 12 weeks: a full dose (300-μg ) IM indicated for abortion or miscarriage
After 34 weeks: 120-μg (IV) indicated for amniocentesis or complication
Antepartum: 300-μg IM given at 28 weeks to non-immunized D-negative females
(HDFN assessment) rosette test
qualitative screening test demonstrating number of D-positive RBCs in a D-negative suspension with chemically modified anti-D reagent
Detectable in 10 mL or more of fetal whole blood in maternal circulation
Postpartum maternal blood sample collected and incubated at 37°C with monoclonal anti-D reagent
Anti-D binds to the D-positive fetal RBCs
Maternal RBCs are washed to remove unbound antibody
Indicator cells (D-positive RBCs) are added, centrifuge, resuspend and read microscopically for visible agglutinates referred to as “rosettes”
Fetal RBCs must be D-positive, maternal RBCs must be D-negative for a valid test
(HDFN) quantitative test
Fetomaternal Hemorrhage (FMH)
D-positive fetal RBCs detected in maternal circulation
If positive, must be quantified using the Kleihauer-Betke or flow cytometry test
Determine Rh status of newborn
D-positive fetal RBCs and Rh type cannot be determined on newborn (e.g., positive DAT), mother should receive full dose of RhIg
Exception: Previous active immunization against D antigen