Non-communicable diseases epidemic
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
Life span meaning
Maximum number of years an individual can live (122 years)
Life expectancy meaning
An average number of years you can expect to live
What were the major health challenges during the Neanderthals era (30,000 BC) ? (4)
Injuries
Conflict
Malnutrition
Diseases from animals
What were the major health challenges during the Neolithic era (8500 - 3500 BC)? (3)
Urbanisation
Lack of sanitation
Faeces/insects
What were the major health challenges during the Greece/Rome era (500 BC - 500 AD)? (3)
Urbanisation
Malnutrition
Violence
During early medieval times (500 AD - 1500 AD) how did healthcare improve?
Solving problems of urbanisation (e.g basic waste disposal systems and separate clean water sources)
What was the major health challenge during the Late Medieval era (500 AD - 1500 AD)? (1)
Famine disease
What were the major health challenges during the Victorian era (1850 - 1900)? (3)
Crowded
Diseases
Malnutrition
During 1900 - now, how did healthcare improve (4), but how has it gone worse (1)?
70s:
Heathcare
Sanitation
Refrigeration
Vaccination
80s:
Vaccination
Non-communicable diseases increased
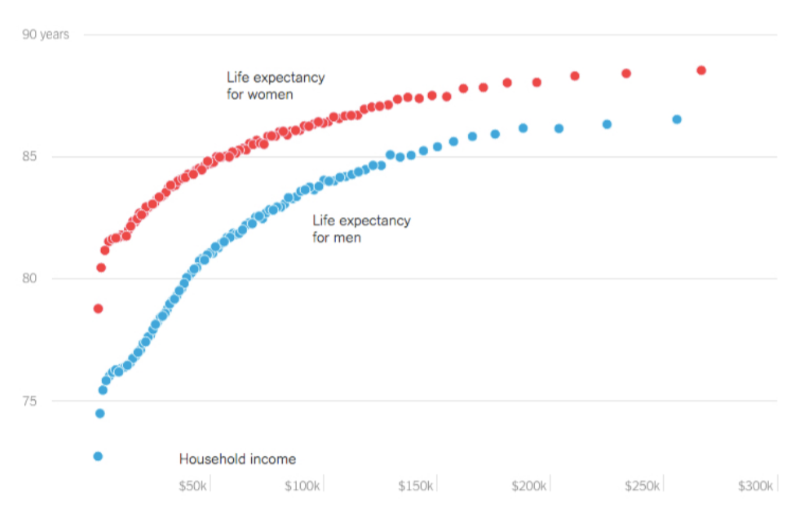
How does sex influence life expectancy?
Women live longer than men in nearly every country worldwide.
(The sex gap varies by country but is consistently present
Biological factors (e.g., hormones like oestrogen) and behavioural factors (e.g., risk-taking, healthcare usage) may contribute
Socioeconomic status further amplifies the gap — wealthy women have the highest life expectancy overall)
How have we shaped our environment to affect health? (6)
Cooking
Agriculture - Cultivation/Irrigation
Accommodation
Sanitation
Refrigeration
Vaccination
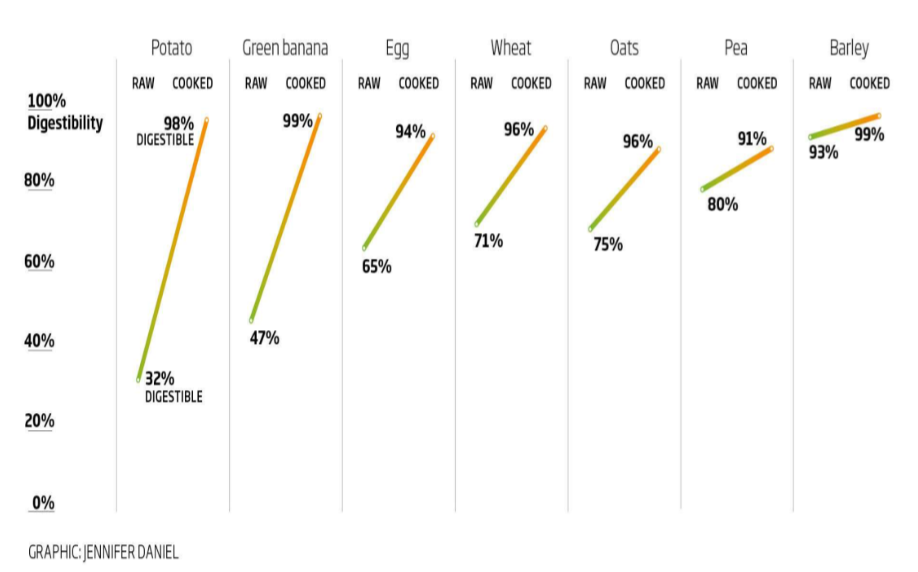
How does cooking improve food safety and nutrition?
✅ Chemically & physically transforms food via heat
✅ Kills harmful bacteria
✅ Increases digestibility — improves nutrient absorption
Digestibility meaning
Measures the degree to which macronutrients are
digested and absorbed by the gastrointestinal tract
What is biomass and how does cooking contribute to pollution?
Biomass = Non-living biological material used for energy
Cooking requires heat, often from burning biomass (e.g. wood, dung)
This emits pollution, especially:
• Particulate matter (PM₂.₅)
• Tiny particles < 2.5 μm — harmful to lungs and airways
What is sedentism?
Transition from nomadic (hunter-gatherer) lifestyle to living in
groups for long periods of time
Characteristics of sedentism
At least partially related to obtaining required resources
Domestication of crops
Domestication of livestock
Population growth - increase supply of food
4 Disadvantages of sedentism
Accumulate human waste → disease (e.g., cholera)
Animal and plant waste nourishes pests → disease vectors (e.g., malaria)
Increased population = disease spreads more easily
More people → more pathogen evolution with host
Irrigation meaning, when and where did it begin? (key developments) (4)
Irrigation - artificial application of water to land or soil to assist in growing crops
Water was diverted to fields and then drained back to the river
Began ~6000 BC with Nile/Tigris-Euphrates rivers
Enabled crop growth, settlement, and population expansion
What is the significance of irrigation for human development? (3)
• Enabled sedentary life and large-scale food production
• Supported population growth
• Increased risk of waterborne diseases and vector-borne illnesses (e.g. malaria from mosquitoes)
How has sanitation evolved and why does it matter for health
Early methods (2000 BC)
Hygiene awareness (460 - 100 BC)
Modern systems (4)
Sanitation problems today (1)
Early methods: Boiling/filtering (2000 BC), latrines, aqueducts
Hygiene awareness: Hippocrates (460–377 BC), China focused on clean water (200–100 BC).
Modern systems:
1600s–1700s: Sewage prevention in rivers.
1800s: Population boom, poor sanitation → cholera outbreaks (waterborne disease from dirty water)
1848 & 1866: Public Health & Sanitary Acts.
1860: Septic tank invented (waste system invented 1860 to safely manage sewage)
Today: Sanitation breakdown (e.g. natural disasters like Tonga) still affects drinking water and disease risk.
History of refrigeration
1700 BC: Ice harvesting + cooling via evaporation
e.g. Yakhchal in Iran, icehouses
1755: William Cullen → first artificial cooling
1913: Modern fridge invented
What is the function of a fridge and how does it relate to food safety? (3)
Slows bacterial growth → reduces food poisoning risk
(e.g. Listeria grows slower at 4°C with 33–36h generation time, vs 21°C with 1.7–1.9h)Preserves food by delaying spoilage
Improves safety through controlled cold storage
What is vaccination?
Vaccination introduces a weakened or inactive pathogen to trigger an immune response without causing illness.
It builds immunity by producing antibodies and memory cells, helping prevent disease and support herd immunity.
How did vaccination reduce infectious disease burden and improve public health? (5)
Measles vaccine (1963) & MMR (1971) → sharp drop in cases (↓ from 385,000 to ~0)
Salk polio vaccine (1955) & Vaccination Assistance Act (1965) → steep US mortality decline
Halved infectious deaths by late 20th century (with antibiotics + sanitation)
Prevents outbreaks via herd immunity
Vaccine hesitancy (e.g. anti-vax) limits full benefit
What are non-communicable diseases and what causes them? (4)
NCDs are chronic, long-duration diseases that are not infectious
Leading global cause of death and disability
They arise from a mix of genetic, physiological, environmental, and behavioural factors.
Driven by:
– Urbanisation (e.g. poor sanitation)
– Globalisation of unhealthy lifestyles
– Population ageing (longer life expectancy = more chronic illness)
How have patterns of communicable and non-communicable diseases changed over time? (3)
Since 1950:
Communicable (infectious) diseases like measles, mumps & TB have declined due to vaccination, sanitation, and antibiotics
Non-communicable diseases (NCDs) like asthma, MS, type 1 diabetes, and Crohn’s disease have risen, especially in developed nations
→ Likely linked to modern lifestyles, environmental triggers, urbanisation, and ageing populations
Examples of NCDs (6)
Cardiovascular disease (biggest killer globally)
Chronic respiratory diseases
Cancer
Type 2 Diabetes
Mental & neurological conditions (recently recognised as NCDs)
Musculoskeletal disorders (high burden of suffering, but not major cause of early death)
Neoplasms
Skin and subcutaneous diseases
Substance use disorders
Main Risk Factors for NCDs
Unhealthy diet
Tobacco use
Alcohol misuse
Physical inactivity
Air pollution
What is the global impact of non-communicable diseases (NCDs) statistics? (4)
Cause 71% of global deaths (41 million/year)
Lead to 15 million premature deaths (ages 30–69)
85% of these occur in low- and middle-income countries
Deaths rising sharply in these regions (e.g. +151% in Botswana)
Modifiable behavioural risk factors for NCDs
Tobacco (7.2 million deaths per year)
Excess salt/sodium intake (4.1 million deaths / year)
Alcohol use (>50% of deaths)
Insufficient physical activity (1.6 million deaths / year)
Obesity/unhealthy eating
What global trends illustrate the impact of physical inactivity and unhealthy diets on health?
Obesity rates are rising worldwide — especially in countries like Nauru, Kuwait, USA — due to increasing physical inactivity and poor diets, driving the global burden of non-communicable diseases (NCDs).
How is globalisation contributing to the rise in NCDs in emerging economies?
Globalisation increases fast food availability and adoption of Westernised diets, leading to lifestyle changes and rising obesity rates in middle-income countries (e.g., India, Vietnam, Argentina)
What are the key trends in causes of death in low-income and LMICs? (5)
Rising burden of NCDs: Chronic diseases (e.g. heart disease, stroke) now cause a growing share of deaths, especially in ageing populations.
Shift from infectious to chronic: Communicable diseases still matter but are no longer the dominant cause.
Hospitalisation patterns: In India (1995–2014), NCD hospitalisations increased with age and overtook infectious diseases in older adults.
Perception gap: People in high-income countries (e.g. USA) wrongly believe most deaths in LMICs are from infections, not NCDs.
Implication: Global health strategies must address this double burden and correct outdated assumptions to improve resource targeting
What recent trends are seen in life expectancy gains and population health in high-income countries like the UK? (4)
Life expectancy (LE) gains are slowing in the UK and many high-income nations.
→ UK saw sharp decline in annual increase in LE between 2001–03 and 2014–16.
→ Fewer UK areas had statistically significant LE improvements in recent years (203 → 26 for men, 128 → 17 for women).International trend: Most high-income countries show a drop in annual LE gain (e.g. USA, UK, Netherlands).
"Baby boomers" are living longer but in worse health than previous generations:
→ Rise in obesity, type 2 diabetes, heart disease, cancer at younger ages.Implies longer lifespans, but poorer quality of life and higher NCD burden
What is generational health drift?
People in their 50s, 60s and 70s more likely to have serious health problems than those born before or during second world war at an equivalent age
Even with advances in medicine and great public awareness about healthy living
Not simply because people are living longer – people born since 1945 are at greater risk of chronic illness than their predecessors
Especially when comparing those born 1955 - 1959 versus 1936 - 1945
More years in poor health and disability