Comprehensive Pharmacology and Drug Therapy for Nursing Practice
1/251
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
252 Terms
Drug
any chemical that can affect living processes
Pharmacology
study of drugs and their interactions with living systems (animals, plants)
Pharmacotherapeutics
the use of drugs to diagnose, prevent, or treat disease or to prevent pregnancy
Brand Name
A drug sold by a drug company under a specific name or trademark and that is protected by a patent
Generic Name
a prescription drug that has the same active ingredients as the brand name
Effectiveness
ability of a drug to produce a desired effect - most important property a drug can have
Safety
drug can not produce harmful effects
Selectivity
drug produces only the response for which it is given
Therapeutic Effect
the desirable and intended outcome or response from a drug
Maximum Benefit with Minimal Harm
the ideal outcome for a response by having a maximum positive effect while minimizing any potential risks associated with that specific drug therapy
10 Rights of Medication Administration
Right drug, Right route, Right Patient, Right Dose, Right Time, Right Assessment, Right Documentation, Right Evaluation, Right of patient education, Right of patient to refuse care
Preclinical Testing
Testing for 1-5 yrs on animals before applying to FDA for human testing permissions
Clinical Testing
4 phases encompassing 2-10 yrs
Phase 1
healthy volunteers typically unless severe side effects as in cancer drugs etc. 3 goals: Evaluate drug metabolism, Pharmacokinetics, Biologic effects
Phases 2&3
Patients utilized to determine therapeutic effects, dosage range, safety, and effectiveness. 500-5000 pt's receive the drug and only a few hundred take it for more than 3-6 months
Phase 4
Postmarketing Surveillance - Drug is released for general use, permitting observation of its effects in a large population
FDAAA of 2007
increased effectiveness of postmarketing surveillance
Pharmacokinetics
the study of drug movement throughout the body
Pharmacodynamics
study of biochemical and physiological effects of drugs on the body and the molecular mechanisms by which those effects are produced
Absorption
Movement of drug from its site of administration into the blood.
Factors affecting Absorption
Rate of dissolution, Surface area, Blood flow, Lipid solubility, pH partitioning, Distribution, Metabolism.
Metabolism
How the body converts medication into a less, or more active form (these forms are also known as metabolites).
Liver
Most drug metabolism takes place in the liver.
Hepatic microsomal enzyme system
Also known as the p450 system, it performs drug metabolism.
First-pass effect
A drug that undergoes rapid hepatic metabolism is often administered parenterally.
Enterohepatic recirculation
Drugs can remain in the body much longer than they otherwise would.
Excretion
Drugs and their metabolites can exit the body in urine, bile, sweat, saliva, breast milk, and expired air.
Kidney
Most important organ for drug excretion.
Intravenous Administration
Advantages include Rapid Onset, Precise Control, Permits use of large fluid volumes, Permits use of irritant drugs.
Disadvantages of Intravenous Administration
High Cost, Difficulty, Inconvenience, Irreversibility.
Intramuscular and Subcutaneous Administration
Rate of absorption is determined by blood flow and drug solubility.
Advantages of Intramuscular and Subcutaneous Administration
No significant barriers (only barrier is capillary wall), Suitable for poorly soluble drugs and depot preparations.
Disadvantages of Intramuscular and Subcutaneous Administration
Discomfort, Inconvenience, Potential for injury.
Oral Administration
Barriers include a layer of epithelial cells and capillary wall.
Absorption Pattern in Oral Administration
Multiple factors affect absorption.
Advantages of Oral Administration
Easy and Convenient.
Plasma drug level
The minimum effective concentration (MEC) is defined as the plasma drug level below which therapeutic effects will not occur.
Toxic concentration
The plasma level at which toxic effects begin.
Therapeutic Range
Plasma drug levels falling between the MEC and the toxic concentration.
Narrow therapeutic range
Drugs that have a narrow therapeutic range are less safe.
Wide therapeutic range
Drugs that have a wide therapeutic range can be administered safely with relative ease.
Drug-receptors
Receptors are any functional macromolecule in a cell to which a drug binds to produce its effects.
Dose-response relationships
Relationship between the size of an administered dose and the intensity of the response produced.
Relative potency
The amount of drug we must give to elicit an effect.
Maximal efficacy
The largest effect that a drug can produce.
Interpatient variability
The dose required to produce a therapeutic response can vary substantially from patient to patient.
ED50
The dose that is required to produce a defined therapeutic response in 50% of the population.
LD50
The dose that is lethal to 50% of the animals treated.
Therapeutic index
A measure of a drug's safety.
Drug-drug interactions
Interactions that can occur from multiple drug ingestion, often when patients take a variety of drugs throughout the day.
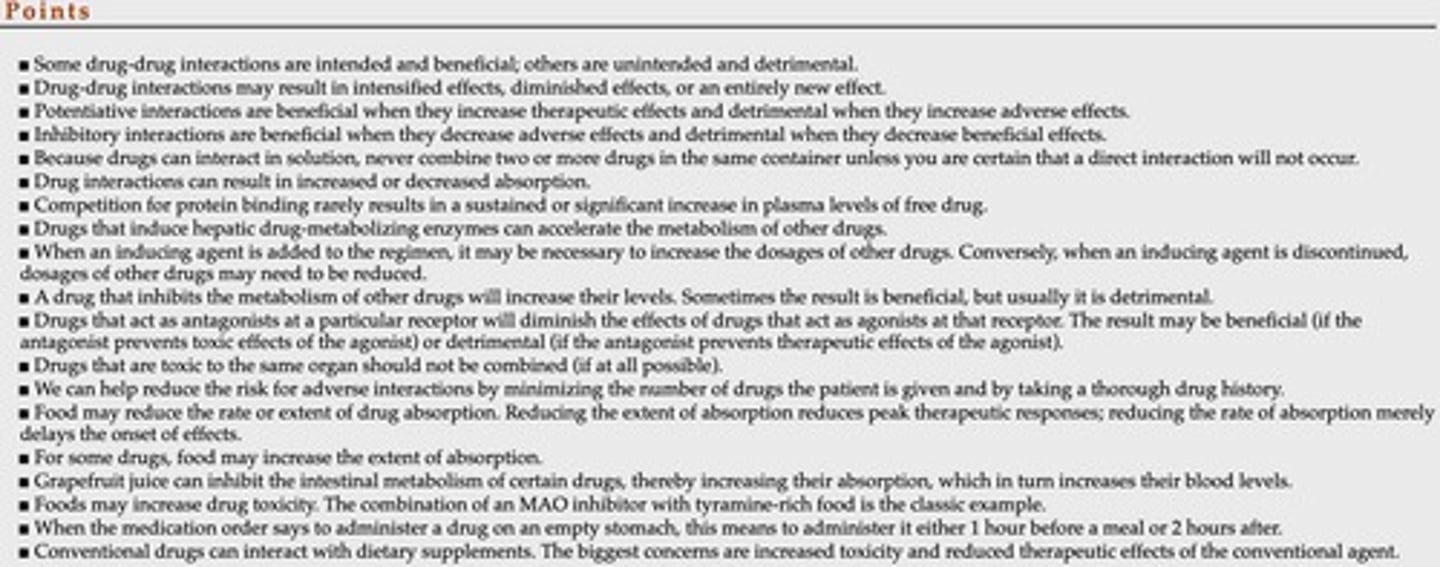
Consequences of drug-drug interactions
Include intensification of therapeutic effects, reduction of therapeutic effects, and/or creation of a unique response.
Grapefruit juice effect
Inhibits metabolism of certain drugs, raising blood levels, but does not affect IV drugs.
MAOIs + tyramine
Can cause life-threatening hypertension.
Potassium sparing diuretics
Can have toxic effects when combined with salt substitutes.
Aluminum containing antacids
Can have toxic effects when combined with citrus beverages.
Timing of administration
Some drugs are better taken on an empty stomach, while others should be taken with food.
Drug-herb interactions
Conventional drugs can interact with herbal preparations, but reliable information is often lacking.
Pharmacokinetic interaction
Altered absorption, distribution, renal excretion, or metabolism of drugs.
Altered absorption
Can be caused by elevated gastric pH, laxatives, or drugs that depress peristalsis.
Altered distribution
Can occur due to competition for protein binding and alteration of extracellular fluid pH.
Altered renal excretion
Drugs can alter filtration, reabsorption, and active secretion.
Altered metabolism
Can increase the rate of metabolism 2-3 fold over 7-10 days.
Pharmacodynamic drug-drug interactions
Interactions that occur at the same receptor, often resulting in inhibitory effects.
Combined toxicity
Drugs with overlapping toxicities should not be used together.
Minimum drug concentration
The amount of drug at a minimum which will have efficacy.
Drug half-life
The time required for the amount of drug in the body to decrease by 50%.
Drug plateau
When there is a steady level of drugs in the body.
Potency
Refers to the amount of drug required to elicit an effect.
Agonists
Molecules that activate receptors.
Antagonists
Produce effects by preventing receptor activation by endogenous regulatory molecules and drugs.
Affinity
The attraction between a drug and its receptor.
Intrinsic activity
The ability of a drug to activate a receptor.
Side Effect
A nearly unavoidable secondary drug effect produced at therapeutic doses.
Adverse Effect
Unexpected effects, severe response!
Toxicity
The degree of harmful physiological effects caused by excessive drug dosing.
Allergic reaction
An immune response.
Synergistic effect
Two drugs given together have a greater impact than when given alone.
Idiosyncratic effect
An uncommon drug response resulting from a genetic predisposition.
Paradoxical effect
Opposite of the intended drug response.
Iatrogenic disease
Disease that occurs as the result of medical care or treatment. The term is also used to denote a disease produced by drugs.
Physical dependence
The body has adapted to drug exposure in such a way that an abstinence syndrome will result if drug use is discontinued.
Carcinogenic effect
The ability of certain medications and environmental chemicals to cause cancers.
Teratogenic effect
A drug-induced birth defect.
Types of Medication Errors
Wrong patient, Wrong drug, Wrong route, Wrong time, Wrong dose, Omitted dose, Wrong dosage form, Wrong diluent, Wrong strength/concentration, Wrong infusion rate, Wrong technique, Deteriorated drug error, Wrong duration of treatment.
Ways to Reduce Medication Errors
Institutional Culture, Infrastructure, Clinical Practice, Technology.
How to Report Medication Errors
MER program: nationwide system run by ISMP reporting done online or via phone and is confidential. All information gathered by MER program is forwarded to FDA, the ISMP, and the product manufacturer.
Individual variation
Factors affecting drug responses including body weight, composition, genetics, gender, race, age.
Body Weight and Composition
Body surface area versus weight.
Age
Significant variability with age; infants and older patients especially sensitive to drugs.
Pathophysiology
Includes Kidney Disease, Liver Disease, Acid-Base Imbalance, Altered Electrolyte Status.
Tolerance
When a patient becomes tolerant to a drug, the dosage must be increased to maintain beneficial effects.
Placebo Effect
A beneficial effect produced by a placebo treatment.
Variability in Absorption
Differences in how drugs are absorbed in individuals.
Genetics
Genetic factors that can influence drug response.
Gender- and Race-Related Variations
Differences in drug response based on gender and race.
Comorbidities and Drug Interaction
The presence of multiple conditions that can affect drug response.
Diet
Nutritional factors that can influence drug metabolism and response.
Failure to Take Medicine as Prescribed
Not adhering to the prescribed medication regimen.
Kidney Disease
Reduced excretion and increased toxicity.
Liver Disease
Reduced metabolism and increased toxicity.