ANATOMY FINAL EXAM
1/299
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
300 Terms
Boundaries of the Temporal Fossa
Posteriorly and superiorly by the superior and inferior temporal lines
Anteriorly by the frontal and zygomatic bones
Laterally by the zygomatic arch
Inferiorly by the infratemporal crest
Floor of temporal fossa is formed by portions of four cranial bones: frontal, parietal, temporal, and sphenoid
Temporalis fascia forms the roof and extends from the superior temporal line to the zygomatic arch
Boundaries of the Infratemporal Fossa
Laterally: ramus of the mandible
Medially: lateral pterygoid plate
Anteriorly: posterior aspect of the maxilla
Posteriorly: tympanic plate and the mastoid and styloid processes of the temporal bone
Superiorly: inferior surface of the greater wing of the sphenoid bone
Inferiorly: where the medial pterygoid muscle attaches to the mandible near its angle
Contents of the Infratemporal Fossa
superficial
• Inferior part of the temporalis muscle
• Lateral pterygoid muscles
• Maxillary artery
deep
• Pterygoid venous plexus
• medial pterygoid muscle
• Mandibular, inferior alveolar, lingual, buccal, and chorda tympani nerves and the otic ganglion
Temporalis
Proximal attachment: Floor of temporal fossa. Deep temporal fascia
Distal attachment: coronoid process and ramus of mandible
Action on mandible: elevates mandible, closing jaw; retracts mandible
Innervation: Anterior trunk of mandibular nerve via deep temporal nerves
Blood Supply: Superficial temporal and deep temporal branches of maxillary
Masseter
Proximal attachment: maxillary process of zygomatic bone and zygomatic arch
Distal attachment: angle and lateral surface of ramus of mandible
Action on mandible: elevates mandible; some contribution to protrusion
Innervation: Anterior trunk of mandibular nerve via masseteric nerve
Blood supply: Transverse facial artery and masseteric branches from maxillary and facial arteries
Lateral Pterygoid
Proximal attachment: Superior head – infratemporal surface of greater wing of sphenoid, Inferior head – lateral pterygoid plate
Distal attachment: Superior head – joint capsule and articular disc of TMJ, Inferior head – pterygoid fovea
Action on mandible: Bilaterally – protrudes mandible; Unilaterally and alternating– larger lateral chewing movements
Innervation: Anterior trunk of mandibular nerve via nerves to lateral pterygoid
Blood Supply: Pterygoid branch of maxillary artery
Medial Pterygoid
Proximal attachment: lateral pterygoid plate; tuberosity of maxilla
Distal attachment: medial surface of ramus of mandible, inferior to mandibular foramen (“mirror image” of masseter)
Action on mandible: Bilaterally – elevates and protrudes mandible; unilaterally and alternately – small grinding movements
Innervation: Anterior trunk of mandibular nerve via nerve to medial pterygoid
Blood supply: Pterygoid branches of facial and maxillary arteries
Branches of the Mandibular N.
Mandibular nerve
Descends through foramen ovale to enter the infratemporal fossa
Divides into anterior and posterior trunks
Posterior trunk is larger and gives rise to:
Auriculotemporal
Inferior alveolar
Lingual
Anterior trunk is smaller and gives rise to:
Buccal
Branch to temporalis
Branch to masseter
Branch to medial pterygoid
Branch to lateral pterygoid
Once the inferior alveolar nerve passes through the mandibular canal it forms the
Inferior Dental Plexus which contains the mental nerve
Before entering the mandibular foramen the inferior alveolar nerve gives off
Nerve to mylohyoid
The lingual nerve gives sensation to
anterior 2/3 of tongue, the floor of the mouth, and lingual gingivae
The chorda tympani nerve carries two types of fibers for different functions. What are they?
Carries taste fibers from the anterior 2/3 of tongue
Carries presynaptic parasympathetic secretomotor fibers for submandibular and sublingual glands
What type of joint is TMJ?
Modified hinge type synovial
Permits movement in three planes
What are the articular surfaces of TMJ?
Head of mandible
Articular tubercle of temporal bone
Mandibular fossa
What prevents posterior dislocation of the TMJ?
Postglenoid tubercle and the lateral ligament
What are the two extrinsic ligaments of the TMJ?
Stylomandibular ligament
Thickening of the fibrous capsule of the parotid gland
Runs from styloid process to angle of mandible
Sphenomandibular ligament
Runs from spine of sphenoid to the lingula of the mandible
Primary passive support and “swing rope” of mandible
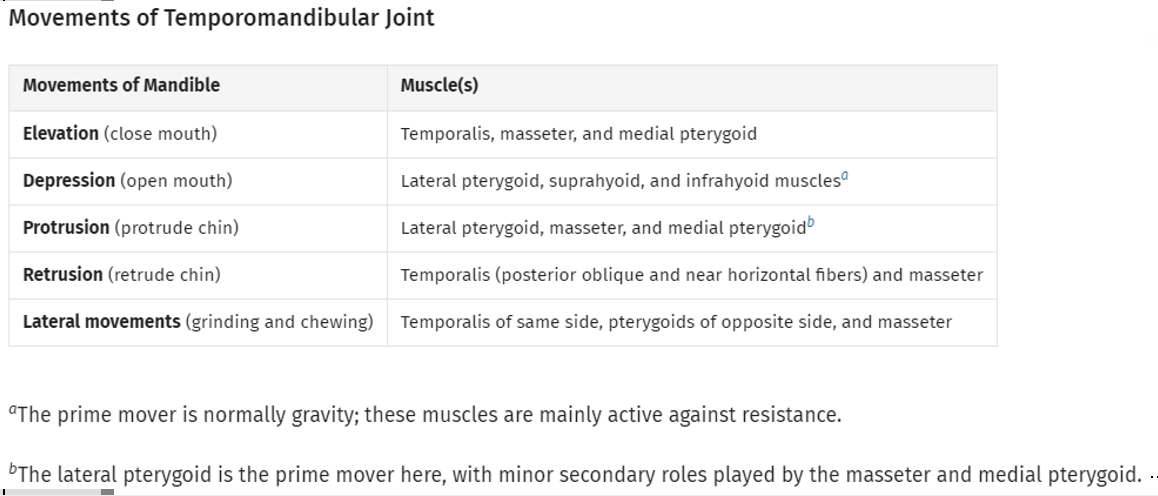
What muscles mandate the movement of the TMJ?
What are the borders of the pterygopalatine fossa?
Posterior wall: pterygoid process of sphenoid
Anterior wall: posterior aspect of the maxilla
Medial wall: perpendicular plate of palatine bone
Roof: greater wing of sphenoid
Floor: pyramidal process of palatine bone
Superior end opens into the inferior orbital fissure
Inferior end is closed except for the palatine foramina
What are the various communications of the pterygopalatine fossa?
Laterally with infratemporal fossa through the pterygomaxillary fissure
Medially with nasal cavity through the sphenopalatine foramen
Anterosuperiorly with the orbit through the inferior orbital fissure
Posterosuperiorly with the middle cranial fossa through the foramen rotundum
Posteriorly with the middle cranial fossa through the pterygoid canal
Posteroinferiorly with the nasopharynx through the pharyngeal canal (aka palatovaginal canal)
Nerves of the Pterygopalatine Fossa
The branches of the pterygopalatine ganglion and the maxillary nerve. Note: For simplicity, this schematic does not show: the contribution of the facial nerve (CNVII) to the pterygopalatine ganglion, the posterior superior alveolar nerves, or the nerve of the pterygoid canal.
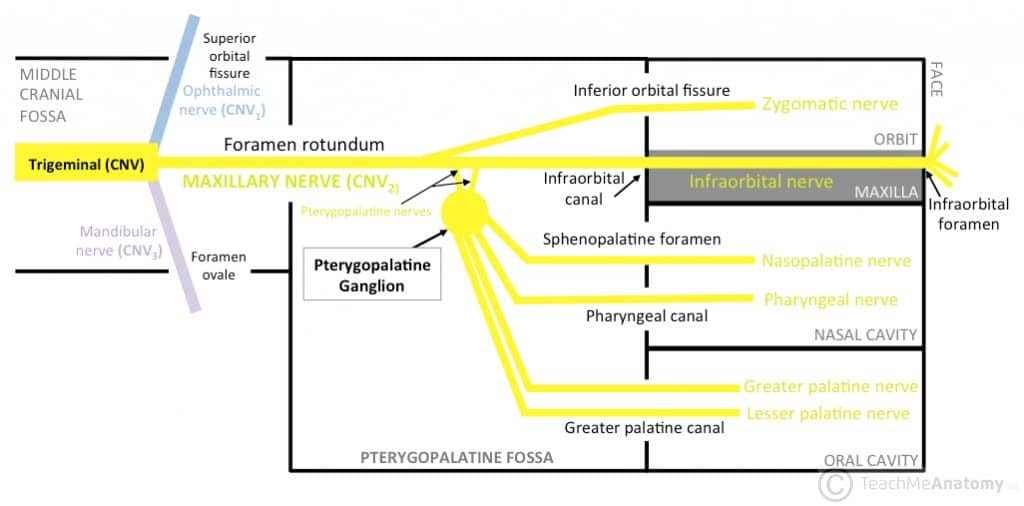
Where do parasympathetic fibers transverse through the pterygopalatine fossa?
Parasympathetic fibers to the pterygopalatine ganglion come from facial nerve by way of the greater petrosal nerve
Greater petrosal joins with lesser petrosal in the foramen lacerum region to form the nerve of the pterygoid canal that passes to the pterygopalatine fossa
Parasympathetic fibers synapse in the ganglion
Where do sympathetic fibers transverse through the pterygopalatine fossa?
Deep petrosal nerve arises form the sympathetic plexus on the internal carotid
Conveys postsynaptic fibers from cell bodies in the superior cervical sympathetic ganglion
Do not synapse in pterygopalatine ganglion but join branches of the ganglion
Both sympathetic and parasympathetic pass to the pterygopalatine ganglia and glands in the nasal cavity, palate and superior pharynx
slay this is satan
What is the function of the cranial meninges? What are the three layers?
Functions:
Protect the brain
Create an enclosed space for CSF
Provide supporting framework for vasculature
Composed of:
Dura mater
Arachnoid mater
Pia mater
What are the three meningeal spaces? Describe their location and contents.
Dura-cranial interface (extradural or epidural “space”)
Between cranium and periosteal layer of dura
Not continuous with spinal epidural space
Dura-arachnoid interface (subdural “space”)
Between meningeal layer of dura and arachnoid mater
Like spinal layers, not a true space as pressure from CSF holds arachnoid right up against dura
Subarachnoid space
Between arachnoid and pia
Only true space, contains CSF arteries and veins
What are the two layers of the dura mater?
Composed of two layers:
Periosteal layer
Formed from periosteum of internal surface of calvaria
Continuous with the periosteum of external surface at foramina
Meningeal layer
Fibrous membrane
Continuous with dura of spinal cord
Has it’s own blood supply and innervation
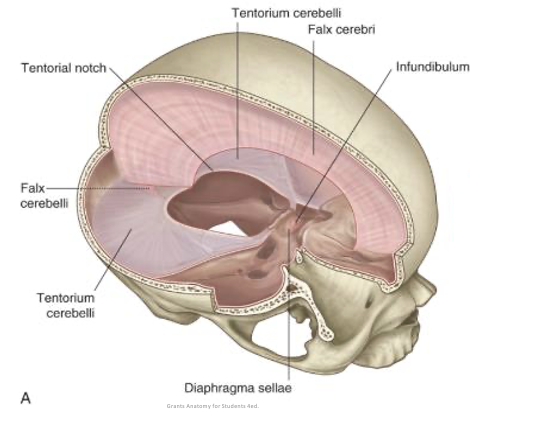
What are the dural infoldings?
Falx Cerebi
Separates left and right hemisphere
Tentorium Cerebelli
Separates occipital lobes from cerebellum, creating two supratentorial compartments and one infratentorial compartments
Falx Cerebelli
Partially separates the cerebellar halves
Diaphragma Sellae
Circular sheet of dura attaching between clinoid processes
Forms a partial roof over hypophysial fossa
Pierced by the pituitary stalk
Anterior ‘limbs’ create the cavernous sinus
Confluence of Sinuses
meeting place for superior sagittal, straight, occipital and transverse sinuses; located at the internal occipital protuberance
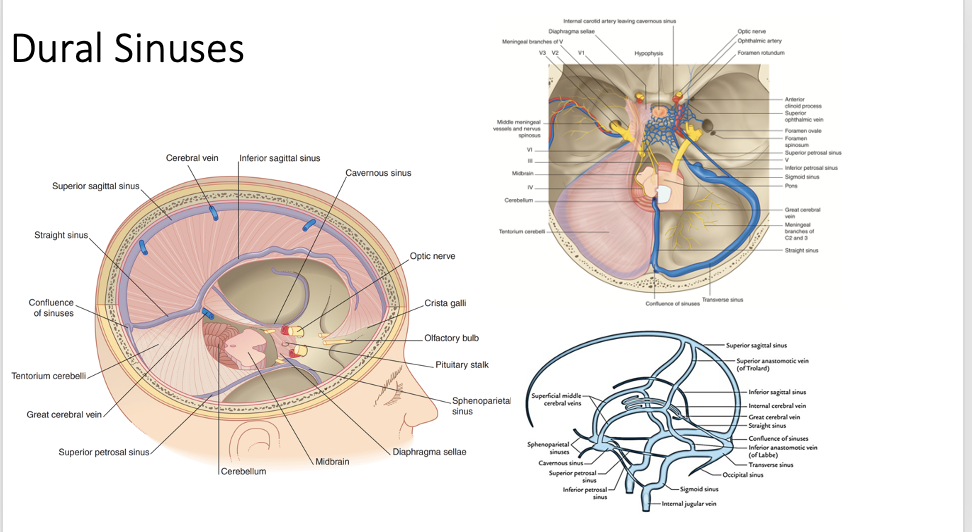
Superior Sagittal Sinus
at attached edge of falx cerebri; runs from crista galli to confluence; receives superior cerebral veins via communication with lateral venous lacunae
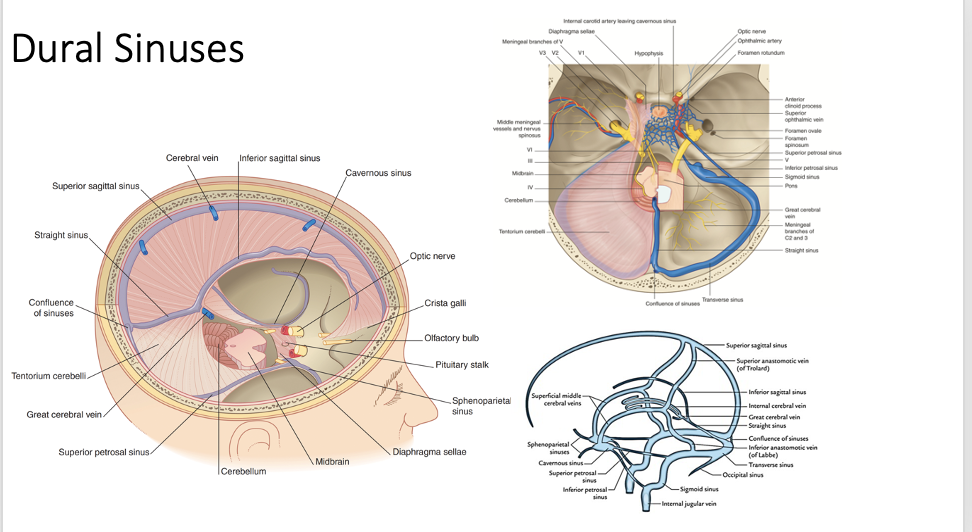
Inferior Sagittal Sinus
runs in free edge of falx cerebri; ends in straight sinus
Straight Sinus
formed from union of inferior sagittal and great cerebral vein; runs at attachment of falx cerebri to tentorium cerebelli
Transverse Sinus
run inferior to attached side of tentorium cerebelli; runs laterally from confluence; becomes sigmoid sinus at the posterior aspect of petrous part of temporal bone
Sigmoid Sinus
s-shaped course through posterior cranial fossa; traverses the jugular foramen to become the IJV
Occipital Sinus
run in attached border of falx cerebelli; ends in confluence; communicates inferiorly with internal vertebral venous plexus
Cavernous Sinus Pathway
large venous plexus on each side of sella turcica; extends from superior orbital fissure to apex of petrous part of temporal bone; receives blood from superior and inferior ophthalmic, superficial middle cerebral and sphenoparietal veins; drains to superior and inferior petrosal sinuses
Intercavernous Sinus
channels anterior and posterior to stalk of pituitary gland; allows for communication between left and right cavernous sinuses
Superior Petrosal Sinus
runs from cavernous sinus to junction of transverse/sigmoid sinuses; lies in anterolateral attached margin of tentorium cerebelli
Inferior Petrosal Sinus
runs from cavernous sinus to sigmoid sinus at jugular foramen; run in groove between petrous part of temporal and basilar part of occipital bone; basilar plexus joins the inferior petrosal sinuses from each side and communicates with internal vertebral venous plexus
Cavernous Sinus Contents
Internal carotid artery and its small branches
Carotid plexus of sympathetic nerves
Abducent nerve (CN VI), Oculomotor nerve (CN III), trochlear nerve (CN IV), two divisions of trigeminal nerve (CN V)
REMEMBER OTOMCAT
What is the main arterial supply to the dura?
Middle Meningeal Artery
Where does the middle meningeal artery enter and exit the cranium?
Enters through the foramen spinosum and exits through the foramen spinosum or foramen ovale
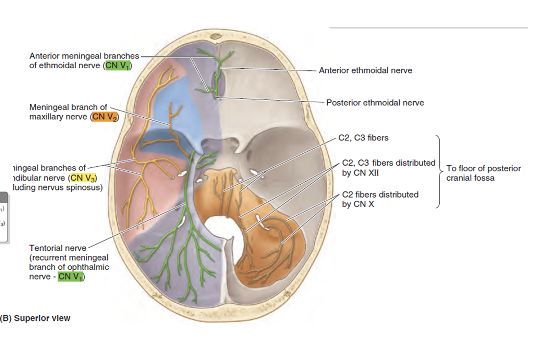
Innervation of the Dura
Dura is pain sensitive. Source for headaches.
Anterior meningeal branches of ethmoid nerves (CN V1) – anterior cranial fossa, anterior falx cerebri
Meningeal branches of maxillary (CN V2) – anterior and middle cranial fossa
Meningeal branches of mandibular (CN V3) – anterior and middle cranial fossa
Tentorial nerve (branch of CN V1) – roof of posterior cranial fossa and posterior part of falx cerebri
Nerves from C2 and C3 (via spinal nerves, vagus nerve (CN X) or hypoglossal nerve (CN XII) – floor of posterior cranial fossa. Pain in the posterior floor can cause refered pain behind the ears or back of the neck
Which is vascular/avascular; cranial pia, cranial arachnoid?
Cranial Pia: Highly Vascularized
Cranial Arachnoid: Avascular
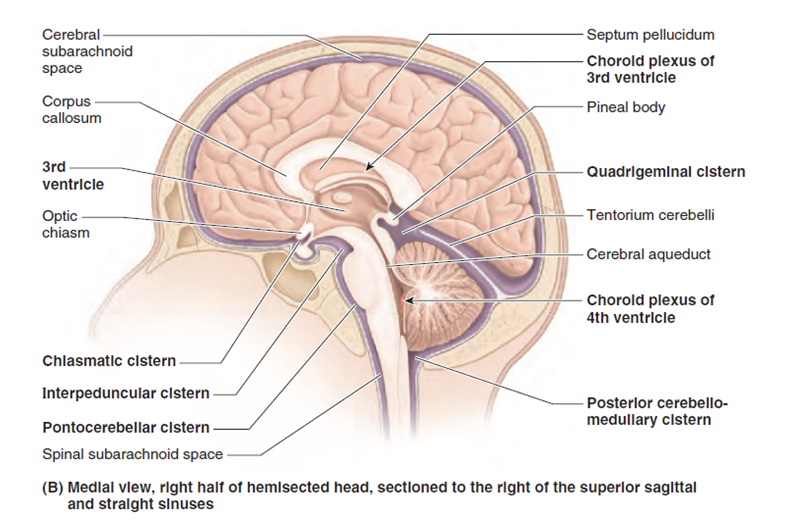
What are subarachnoid cisterns?
Areas on base of brain where pia and arachnoid mater are widely separated
Contain CSF, and soft tissue structures like arachnoid trabeculae, vasculature and cranial nerve roots
What are the four lobes of the brain?
Frontal – the anterior most lobe, extends to the central sulcus posteriorly and the lateral sulcus inferiorly; anterior most portion is the frontal pole
Parietal – from the central sulcus to the parieto-occipital sulcus (best viewed on medial surface), sits above lateral sulcus
Occipital – most posterior lobe behind the parieto-occipital sulcus; posterior most portion is the occipital pole
Temporal – inferior to lateral sulcus, anterior to parieto-occipital sulcus; anterior most portion is the temporal pole
What are the three portions of the brainstem?
Midbrain - most rostral portion; at junction of middle and posterior cranial fossae; associated with CN III and IV
Pons – caudal to midbrain; lies in anterior part of posterior cranial fossa; associated with CN V
Medulla oblongata – most caudal portion; continuous with spinal cord; in posterior cranial fossa; associated with CN IX, X, XII
CN XI, XII, XIII associated with pons-medulla junction.
Describe the flow of CSF in the brain.
CSF is primarily produced in the choroid plexus, a network of blood vessels in the ventricles of the brain, especially the lateral and fourth ventricles. The choroid plexus filters blood plasma and secretes CSF, which is a continuous process.
From the choroid plexus, CSF flows through the ventricular system of the brain, which includes the lateral ventricles, third ventricle, cerebral aqueduct, and fourth ventricle.
The cerebral aqueduct connects the third ventricle to the fourth ventricle, allowing CSF to move between these compartments.
CSF exits the fourth ventricle through small openings called the foramina of Luschka (two lateral openings) and the foramen of Magendie (a midline opening). These foramina allow CSF to enter the subarachnoid space, which is the space between the arachnoid mater and the pia mater, surrounding the brain and spinal cord.
CSF circulates within the subarachnoid space, bathing the brain and spinal cord in nutrients and providing a cushioning effect. It also helps to remove waste products from the brain and maintain a stable environment for neural function.
CSF is absorbed back into the bloodstream through structures called arachnoid granulations or villi, which are protrusions of the arachnoid mater into the venous sinuses. These structures allow for the reabsorption of CSF into the venous blood, completing the circulation cycle.
Extradural (epidural) Hemorrhage
Occurs when blood from a torn meningeal artery collects between the calvaria and periosteal layer of the dura
Usually caused by a blow to the head (fracture of the pterion as it overlies the anterior branch of middle meningeal artery)
As blood pools it forms an extradural (epidural) hematoma that can cause pressure on the brain
Symptoms: initially a brief concussion, followed by lucidity (for hours), then drowsiness and coma
Blood needs to be drained and vessel repaired
Dural Border Hematoma
Occurs as blood collects creating a space between the dura and arachnoid maters
Hemorrhage is usually caused by hard blow to head that jerks the brain causing a hemorrhage
Usually damage is done to the venous system, most commonly superior cerebral vein (as it enters the sagittal sinus)
Symptoms include confusion, dizziness, headache, and possibly issues with balance, nausea/vomiting, loss of consciousness or seizures
Subarachnoid Hemorrhage
Collection of blood in the subarachnoid space, usually arterial
Often from rupture of a saccular aneurysm, sometimes due to head trauma (involving cranial fractures and cerebral lacerations)
Causes severe headache, stiff neck and possibly loss of consciousness
Stroke (Differentiate between the four types)
Generally caused by an abrupt blockage in a major cerebral artery
Thrombotic – arteries in brain are diseased or damaged subsequently becoming blocked
Embolic – artery becomes blocked due to a clot that formed elsewhere and traveled to brain
Hemorrhagic stroke - Occurs when a vessel is ruptured, can be at the site of a saccular aneurysm
Berry aneurysm – occurring in vessels of or near cerebral arterial circle
Stroke Susceptibilities & Risks
Risk increases with age
Higher rate in women
Higher rate in African-Americans
Higher incidence in those with hypertension, heart disease, smoking, diabetes
Meningitis
Inflammation of the meninges surrounding the brain
Symptoms: Fever, HA, Stiff neck, Photophobia, N/V, confusion/altered mental state
Can have several different causes
Bacterial – 70% are children under 5. Life threatening. Vaccines are available for some kinds of bacterial meningitis
Viral – Most people who have the virus will not develop meningitis
Fungal - Rare
Parasitic - Rare
Drug – Induced – Rare. NSAIDS and some antibiotics
Transtentorial Herniation
Transtentorial herniation is a medical condition characterized by the displacement of brain tissue through the tentorial notch, which is a narrow opening in the skull that separates the cerebellum from the cerebral hemispheres. The tentorium cerebelli is a fold of the dura mater, the tough outer layer of the meninges that surround the brain.
When there is increased intracranial pressure due to various reasons such as tumors, hemorrhage, or swelling of the brain, the brain tissue may be forced downward through the tentorial notch. This can lead to compression of vital structures in the brain, including the brainstem.
There are different types of transtentorial herniation, including:
Central (or "downward") Transtentorial Herniation: In this type, the brain tissue is displaced downward through the tentorial notch, putting pressure on the midbrain and other structures.
Uncal (or "lateral") Transtentorial Herniation: This occurs when the innermost part of the temporal lobe, the uncus, herniates through the tentorial notch. This can compress the third cranial nerve and lead to specific neurological symptoms.
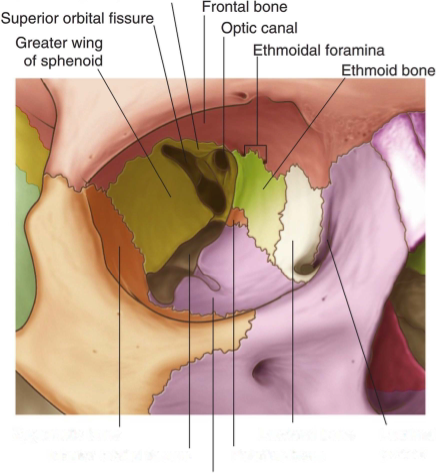
Structure of the Orbit
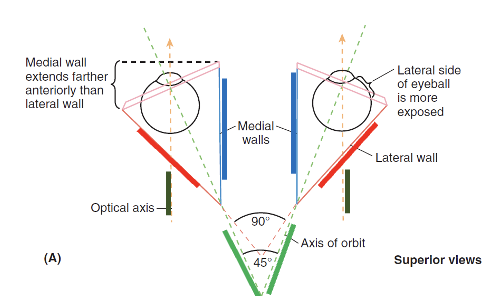
Bones within the Orbit Space
Base – outlined by the orbital margin and surrounds the orbital opening
Superior wall – Frontal bone and lesser wing of sphenoid
Medial wall – ethmoid, maxilla, lacrimal and sphenoid bones
Inferior wall – (floor) maxilla, palatine and zygomatic bones
Lateral wall – formed by frontal process of zygomatic bone and greater wing of sphenoid.
Apex – at the optic canal in lesser wing of sphenoid
Palpebra Composition
Skin
Subcutaneous tissue
Orbicularis oculi
Tarsus - dense connective tissue plates
Superior and inferior tarsus
Tarsal glands
Loss of sympathetic innervation to the Palpebra would result in
Partial Ptosis
Conjunctiva
inner surface of the lids conjunctiva lining the eyeball
Chalazion
Blockage and inflammation of a tarsal gland
On the inner surface of the eyelid
Stye
Blockage and inflammation of sebaceous and sweat glands
On the edge of the eyelid
Lacrimal Gland
Has its own fossa
Ducts are on the superior fornix of the conjunctiva (upper eyelid)
Gland → Duct → Puncta → Canaliculi → Sac
Lacrimal Apparatus Innervation
Sensory via Lacrimal N. (V1)
Secretomotor:
Parasympathetic via VII and then V
Preganglionic axons (VII) to Pterygopalatine ganglion
Postganglionic axons via V2 V1
Sympathetic innervation -
Postganglionic axons from superior cervical ganglion
Layers of the Eyeball
Outer fibrous layer: sclera (posterior) and cornea (anterior, transparent)
Middle vascular layer : choroid (posterior) and iris and ciliary body (anterior).
Retina: Sensory neural layer
Optic portion (posterior) and nonvisual portion (anterior)
Two parts of the uvea
Choroid: Dense Vasculature
Ciliary Body
Muscle: Accommodation for near vision
Processes: Attachment of zonular fibers
Iris
The central opening in the iris is the pupil.
Two sphincters for pupil
Sphincter Pupillae: Arranged in a circular pattern
Dilator Pupillae: Arranged in a radial pattern
Optic Disc
where neurovasculature enters/exits the eye. Insensitive to light = blind spot
Macula
contains the fovea centralis which is the area of most acute vision (can only be seen when using red-free light)
Describe the path of light within the eye.
Lens would form a round shape in the absence of ciliary muscles
In relaxed state (no nerve stimulation), lens is stretched and can refract light for distance vision
Parasympathetic stimulation via oculomotor nerve (CN III) cause a sphincter like contraction reduces stretching on lens and allows it to refract light for near vision
Thickness of lens increases with age and lens shape changes become restricted after age 40
Orbicularis Oculi
Palpebral portion: involuntarily closes eyelids gently
Innervation – CN VII
Levator palpebrae superior
Raises eyelid
Innervation – CN III
Superior Tarsal Muscle
Innervation - Superior Cervical Ganglion
The four Rectus Muscles
Rectus Muscles:
Medial Rectus Muscle: This muscle is responsible for moving the eye medially (towards the nose).
Lateral Rectus Muscle: This muscle moves the eye laterally (towards the temple).
Both the medial and lateral rectus muscles play a crucial role in horizontal eye movements.
Superior Rectus Muscle: This muscle primarily elevates the eye, externally rotates, and adducts.
Inferior Rectus Muscle: The inferior rectus muscle depresses, externally rotates, and adducts.
The superior and inferior rectus muscles are involved in vertical eye movements.
The Two Oblique Muscles
Oblique Muscles:
Superior Oblique Muscle: The superior oblique muscle is responsible for depressing and abducting the eye (moving it downward and outward).
Origin: From the Sphenoid and passes through the trochlea.
Inferior Oblique Muscle: This muscle elevates and abducts the eye (moving it upward and outward).
Origin: Orbital surface of the maxilla
Insertion: Just under lateral rectus.
The oblique muscles contribute to diagonal eye movements.
Extrinsic Eyeball Muscle Innervation
Medial Rectus
C 3
Lateral Rectus
C 6
Superior Rectus
CN 3
Inferior Rectus
CN 3
Superior Oblique
C 4
Inferior Oblique
C 3
Which structures pass through the common tendinous ring?
Optic Nerve, Ophthalmic A., Nasociliary branch of Ophthalmic N., Abducent N., Superior & Inferior Branch of Oculomotor N.
What are the three branches of the opthalmic nerve?
Nasociliary N.
Eyeball, eyelids, nose, anterior cranial fossa
Lacrimal N.
Lacrimal Gland, Conjunctiva
Frontal N.
Supratrochlear, Supraorbital
Which cranial nerves are responsible for the pupillary light reflex?
2 & 3
Which cranial nerves are responsible for the corneal reflex?
absence is CN V1, impairment is CN VII
What muscles compose the external layer of the pharynx?
Superior, Middle, and Inferior pharyngeal constrictor
What muscles compose the internal longitudinal layer of the pharynx?
Palatopharyngeal, Stylopharyngeus, Salpingopharyngeus
What are the four constrictor gaps of the pharynx?
Between superior constrictor and cranium
Between superior and middle constrictors
Between middle and inferior constrictors
Inferior to inferior constrictor
Stylopharyngeus Innervation
Glossopharyngeal N.
Nasopharynx
Pharyngeal orifice of pharyngotympanic tube
Tubal and pharyngeal (adenoid) tonsils
What are the muscles within the Nasopharynx?
Torus Tubarius, Torus Levatori, Levator Veli Palatini, Salpingopharyngeus (within the salpingopharyngeal fold)
Tonsil problems can arise due to….
An infected adenoid
Boundaries of the Oropharynx
Soft palate, base of tongue, and palatoglossal and palatopharyngeal arches
What are the three stages of deglutition (swallowing)?
Stage 1: voluntary bolus compression
Stage 2: involuntary superior contraction
Stage 3: involuntary pharyngeal constrictors contraction
What can happen during a palatine tonsillectomy?
Because of rich blood supply, bleeding commonly arises from external palatine vein and tonsillar artery.
It is also common to injury CN IX which accompanies the tonsillar artery due to the thin wall. This can cause loss of taste to the posterior 1/3 of the tongue as well as loss of afferent limb of gag reflex.
Where is oropharyngeal squamous cell carcinoma?
Base and posterior 1/3 of tongue
Tonsils
Soft palate
Posterior and lateral pharyngeal walls
Laryngopharynx Boundaries
Extends from epiglottis to inferior border of cricoid cartilage
Laryngopharynx Landmarks
Middle and inferior pharyngeal constrictors, palatopharyngeus, stylopharyngeus
How does the layngopharynx communicate with the larynx?
Via the laryngeal inlet in the piriform fossa
Foreign bodies in the laryngopharynx can be especially bad because…
Sharp objects may pierce mucous membrane and injure internal laryngeal nerve
Superior laryngeal nerve vulnerable during object removal
What is the main arterial supply to the pharynx?
Ascending pharyngeal artery (ECA), Inferior Thyroid Artery (Subclavian portion of TCT)
What is the main venous drainage of the pharynx?
Pharyngeal Veins → Internal Jugular Vein
Where does the pharynx drain to?
Deep cervical nodes → Retropharyngeal, Paratracheal, Infrahyoid nodes
Where does the palatine tonsil lymph drain to?
Jugulodiagastric nodes
What supplies motor to the pharynx?
CN X via pharyngeal branches
What supplies sensory fibers to the three different parts of the pharynx?
Naso: V2
Oro: IX
Laryngo: X