Chapter 14: Identification of Semen
14.1: Biological Characteristics
A typical ejaculation releases 2–5 mL of semen, which contains seminal fluid and sperm cells.
A normal sperm count ranges from 107 to 108 spermatozoa per milliliter of semen.
Spermatogenesis: The process of generating spermatozoa.
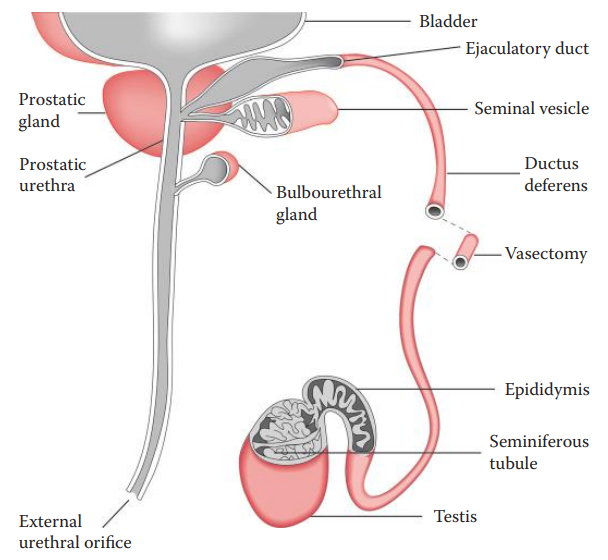
Seminal fluid is a complex mixture of glandular secretions.
Prostatic fluid secretions account for approximately 30% of the ejaculate.
- This portion of semen contains high concentrations of acid phosphatase (AP) and prostate-specific antigen (PSA).
Vasectomy: The surgical removal of a bilateral segment of the ductus deferens. It prevents spermatozoa from reaching the distal portions of the male reproductive tract.
Oligospermia: The condition by which males have abnormally low sperm counts.
Azoospermia: A condition that causes males to produce no spermatozoa.
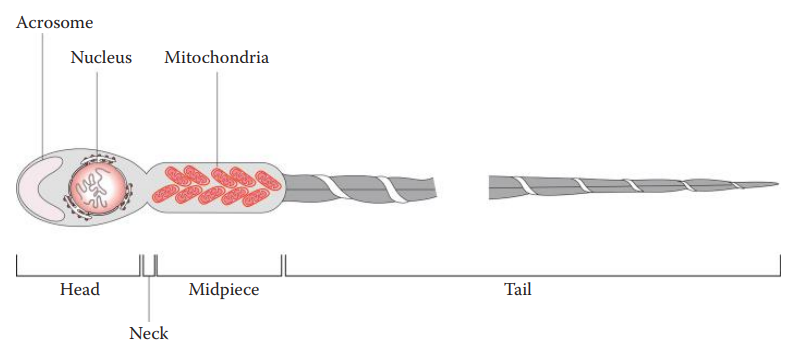
Spermatozoa
The head contains a nucleus with densely packed chromosomes.
Acrosomal Cap: A membranous compartment containing enzymes essential for fertilization found at the tip of the head.
The head is attached to the middle piece through a short neck where the mitochondria that provide the energy for moving the tail are located.
The tail or flagellum is responsible for spermatozoon motility.
Acid Phosphatase
- Acid phosphatase (AP) consists of a group of phosphatases with optimal activity in an acidic pH environment.
- The greatest forensic importance of AP is that prostate-derived AP contributes most of the AP activity present in semen.
- The half-life of AP activity at 37°C is 6 months.
- Elevated levels of prostatic AP found in serum are useful in diagnosing and monitoring prostate carcinoma.
Prostate-Specific Antigen (PSA)
- It is a major protein present in seminal fluid at concentrations of 0.5–2.0 mg/mL.
- PSA is produced in the prostate epithelium and secreted into the semen. It can also be found in the paraurethral glands, perianal glands, apocrine sweat glands, and mammary glands.
- PSA is a protein that has a molecular weight of 30 kDa and is thus also known as P30. It is responsible for hydrolyzing semenogelin (Sg), which mediates gel formation in semen.
- It is a member of the tissue kallikrein family and is encoded by the KLK3 locus located on chromosome 19.
Seminal Vesicle–Specific Antigen
- Human seminal vesicle–specific antigen (SVSA) includes two major types, semenogelin I (SgI) and semenogelin II (SgII).
- In humans, both SgI and SgII are present in a number of tissues of the male reproductive system, including the seminal vesicles, ductus deferens, prostate, and epididymis.
- The concentration of Sg in seminal fluid is much higher than that of PSA, and this is beneficial for the sensitivity of detection.
- Sg is present in seminal fluid and absent in urine, milk, and sweat, where PSA can be found.
- Although Sg compounds are present in skeletal muscle, kidney, and colon, this is not a great concern because these tissue samples are not routinely collected for semen detection in sexual assault cases.
14.2: Analytical Techniques for Identifying Semen
Presumptive Assays
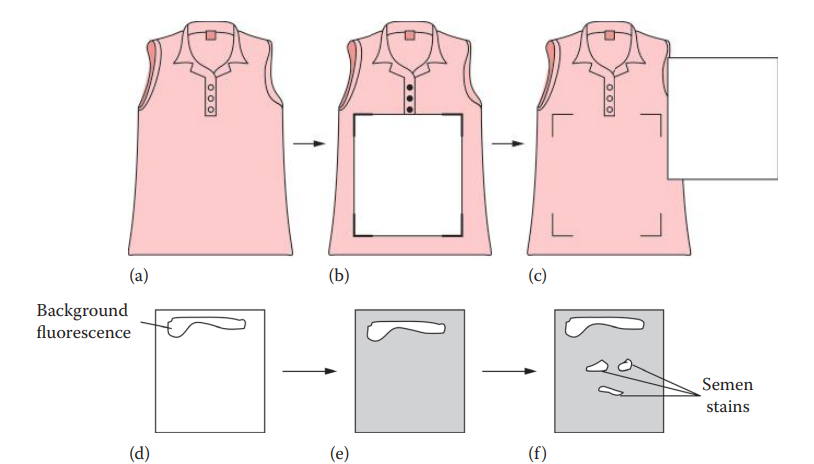
Lighting Techniques for Visual Examination of Semen Stains
- A dried semen stain fluoresces under certain light sources such as ALSs or argon lasers.
- ALSs are most commonly utilized for the visual examination of semen stains,
- Excitation wavelengths between 450 and 495 nm can be used, allowing for the visualization of fluorescence with orange goggles.
- The intensity of the fluorescence can be affected by different colors of substrates, and the material, such as clothing, where semen stains have been deposited.
Acid Phosphatase Techniques
Colorimetric Assays
The AP contained in semen can hydrolyze a variety of phosphate esters.
It catalyzes the removal of the phosphate group from a substrate.
An insoluble colored precipitate at sites of acid phosphatase activity is formed with a stabilized diazonium salt.
Fluorometric Assays
These are more sensitive than the colorimetric detection of AP and are used for semen stain mapping.
AP catalyzes the removal of the phosphate residue on a 4-methylumbelliferone phosphate (MUP) substrate a reaction that generates fluorescence under ultraviolet light.
Confirmatory Assays
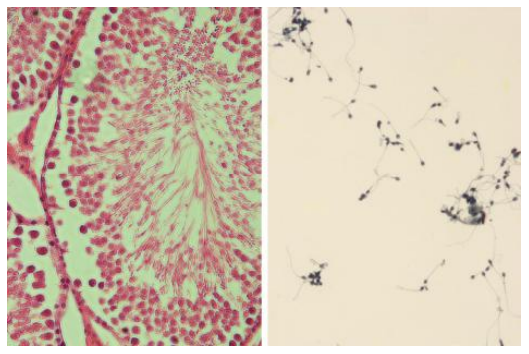
Microscopic Examination of Spermatozoa:
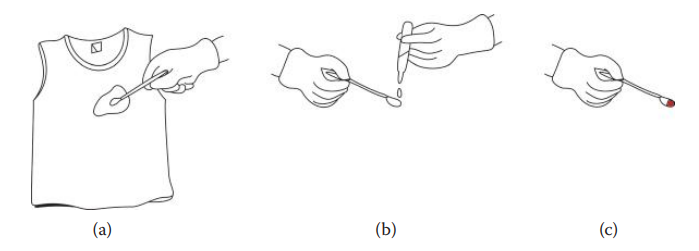
- The cells from a questioned stain on an absorbent material can be transferred to a microscope slide by extracting a small portion of a stain with water, followed by gentle vortexing.
- The suspension is then transferred to a slide and evaporated at room temperature or fixed with low heat.
- The most common staining technique is the Christmas tree stain.
- Nuclear Fast Red (NFR): A dye used for staining the nuclei of spermatozoa in the presence of aluminum ions.
- Picroindigocarmine (PIC): A green component that stains the neck and tail portions of the sperm.
- Epithelial cells appear blue-green and have red nuclei.
- Fluorescent detection utilizing SPERM HY-LITER Fluorescent Staining Kit can facilitate the identification of spermatozoa.
- Laser capture microdissection (LCM) has been shown to be an effective technique for separating spermatozoa from nonsperm cells.
- This technique involves using a thin layer of a thermosensitive polymer that is placed on the surface of an LCM cap.
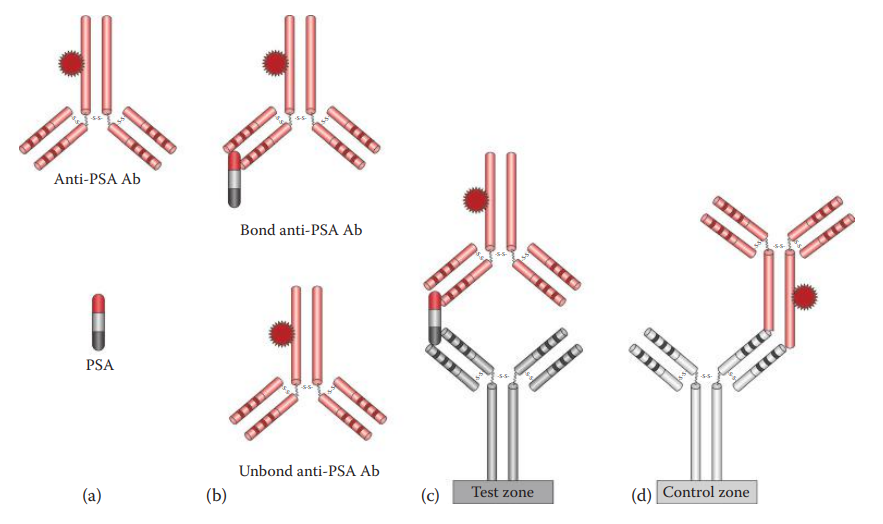
Identification of Prostate-Specific Antigen
- Immunochromatographic Assays:
- PSA-Check-1, Seratec®
- PSA Semiquant
- One Step ABAcard PSA®
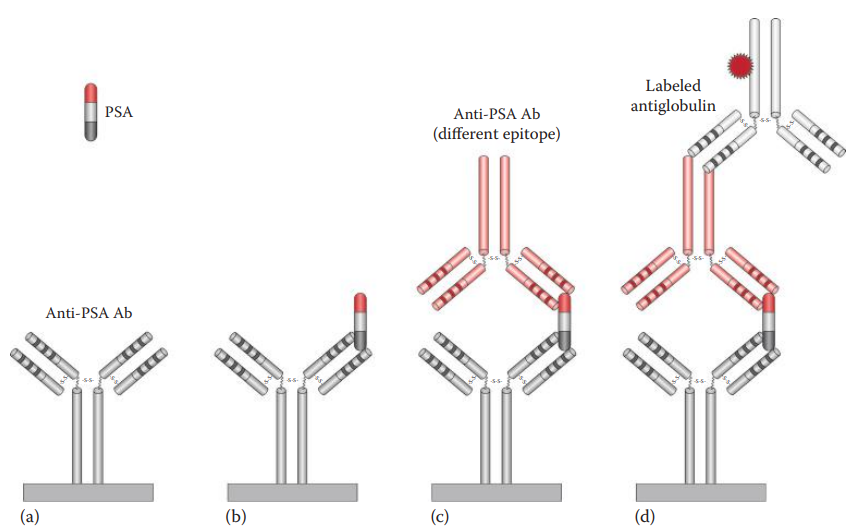
Identification of Seminal Vesicle–Specific Antigen
Immunochromatographic Assays: RSID®-Semen test and Nanotrap Sg.
ELISA: Antibody Sandwich ELISA
The intensity of the signal can be detected and is proportional to the amount of bound antigen. The amount of PSA can also be quantified by comparing a standard with known concentrations.
RNA-Based Assays
- The essays are based on the expression of certain genes in a certain cell or tissue types.
- The techniques used in the identification of semen are based on the detection of specific types of mRNA expressed exclusively in spermatozoa and in certain cells of male accessory glands.
Application of RT-PCR for Semen Identification
| Gene Symbol | Gene Product | Description |
|---|---|---|
| KLK3 | Kallikrein 3 | Also called prostate-specific antigen (PSA). |
| PRM1 | Protamine 1 | DNA-binding proteins are involved in condensation of sperm chromatin. |
| PRM2 | Protamine 2 | DNA-binding proteins involved in condensation of sperm chromatin. |