Psychiatric Mental Health Module 1
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
123 Terms
What is mental health?
State of well-being in which individuals reach their own potential, cope with the normal stresses of life, word productively, and contribute to the community.
What is mental illness?
Refers to all mental disorders with definable diagnoses and includes developmental, biological, and psychological disturbances in mental function.
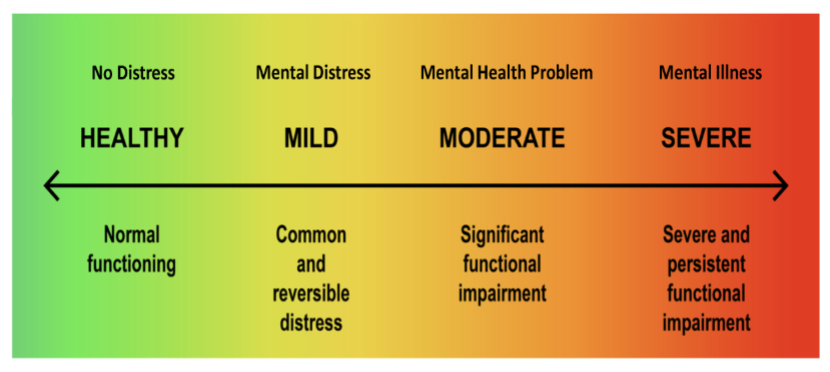
Mental Health Continuum Scale
JUST MEMORIZE THIS OKAY!
Diathesis-Stress Model
Combination of genetic vulnerability and negative environmental stressors.
Diathesis is biological predisposition and stress is environmental.
Diathesis-stress model is most accepted explanation for mental illness.
Example: Oxygen is diathesis, stress is the spark, & fire is the psychological event.
Risk Factors
Inborn vulnerability (genetically-influenced predisposition).
Poor social environment.
Economic hardship.
Poor health policy.
Protective Factors
Resiliency - improve a person’s ability to respond to stress, trauma, and loss.
Essential to recovery.
Occurence of Mental Disorders
Epidemiology: Study of the distribution of mental disorders.
Incidence: # of new cases in a given time.
Prevalence: # of cases regardless of when they began.
Lifetime Risk: Risk of developing a disease during lifetime.
Influences on Mental Health Care
Legislation and Funding: Mental Health Parity Act and Patient Protection & Affordable Care Act.
Social Support and Organization: Mental health recovery
EX: NAMI (National Alliance on Mental Illness).
Mental Health Diagnoses
DSM-5
The Diagnostic and Statistical Manual of Mental Disorders, 5th edition.
Official medical guidelines of the American Psychiatric Association.
Diagnoses mental health disorders following standard criteria.
Psychiatric Mental Health Nursing
Promote mental health using nursing process.
Use holistic approach to care for clients - biological, social, spiritual, and psychological.
Care based on standards set by the:
American Nurses Association
American Psychiatric Nurses Association
International Society of Psychiatric-Mental Health Nurses
Levels of Education for Psych Nurses
Basic Level
Psychiatric mental health registered nurse (PMH-RN)
2 years full-time work, 2000 clinical hours, 30 hours continuing education, followed by certification exam to add “BC” to the RN title (RN-BC)
Advanced Practice
Psychiatric-mental health advanced practice registered nurse (PMH-APRN).
Master of Science (MSN) or Doctor of Nursing Practice (DNP)
Trends Affecting the Future
Educational challenges
Demand for mental health professionals
Aging population
Cultural diversity
Science, technology, and electronic healthcare
Advocacy and legislative involvement
Psychoanalytic Therapy
Developed by Signmund Freud.
Classic psychoanalysis rarely used.
Intrapsychic conflict thought to be cause for all mental illness (3-5x/wk, expensive)
Purpose: Uncover unconscious conflicts
Free association
Dream analysis
Defense mechanism recognition
Transference & Countertransference in Psychoanalytic Theory
Transference: The client unconsciously projects feelings about significant people in their life onto the therapist.
Countertransference: This is the therapist’s emotional reaction to the client, which may relate to a triggering of the therapist’s own unresolved issues
Psychodynamic Theory
Similar to psychoanalytic therapy.
Difference is increased involvement of therapist, interacts with patient more than traditional psychoanalysis.
Weekly sessions (may be >20 sessions).
Focus on here and now, and not origin of conflict.
Best candidates are relatively health, “worried well".”
Interpersonal Theory
Short-term therapy to improve interpersonal functioning and satisfaction with social relationships.
Goal to decrease symptoms of anxiety or depression.
3 types of problems treated:
Grief and loss
Interpersonal disputes
Role transition
Behavioral Therapy
Behavior Management - modifying or replacing behaviors.
5 Types of Behavior Therapy
Modeling - therapist as role model.
Operant Conditioning - Positive rewards for positive behaviors.
Exposure & Response Prevention: Face fears and emotionally process them in safe environment.
Aversion Therapy - Negative stimulus on behavior to stop the behavior.
Biofeedback - Controlling body’s physiological response to stress and anxiety.
Cognitive Behavioral Therapy
CBT based on cognitive psychology and behavioral therapy.
Focuses on changing thinking and behaviors to improve emotional regulation.
3 Phases:
Thoughts: What we think affects how we feel and act.
Behaviors: What we do affects how we think and feel.
Emotions: What we feel affects how we think and act.
Trauma Informed Care
Recognizing trauma can affect people and groups.
Knowing signs and responses to trauma.
Avoid re-traumatization.
Goal is providing safe environment - physically and psychologically and building trust.
Trauma-Focused CBT (TF-CBT)
Short-term treatment combines trauma-sensitive interventions with CBT.
Usually for children, includes family therapy.
Helps identify negative thoughts and replace with more positive thoughts.
Dialectical Behavioral Therapy (DBT)
Long-term therapy (1-1.5 yrs)
Uses strategies from CBT
Developed for individuals with intractable behavioral disorders involving emotional dysregulation.
Effective treatment for depression, suicidal thoughts, hopelessness, anger, substance use, and dissociation
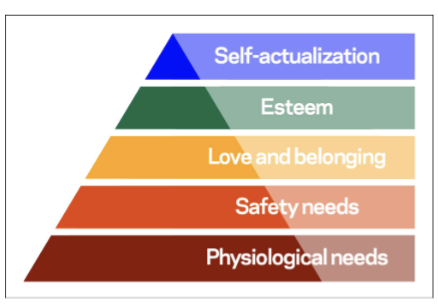
Humanistic Theories: Maslow’s Hierarchy of Needs
Human beings are active participants in life, striving for self-actualization.
When lower needs are met, higher needs can emerge.
Biological Model
Medical model assumes that abnormal behavior is from a physical problem.
Recognizes that mental disorders are physical in origin (like diabetes, heart disease, etc.)
Focuses on neurological, chemical, biological, genetic.
Locates illness or disease in body.
Biological Therapies - Pharmacotherapy
Uses medication to treat psychiatric illness.
1st psych meds.
Chlorpromazine (Thorazine) and Lithium.
Psychotropic medication effective for treating psychosis, mania, depression, and anxiety.
Biological Therapies - Brain Stimulation Therapies
All methods involve focused electrical stimulation of brain.
Types of brain stimulation therapies
Electroconvulsive therapy (ECT)
Transcranial magnetic stimulation - repetitive (rTMS)
Vagus nerve stimulation (VNS)
Deep brain stimulation (DBS)
Developmental Theories
Assess client’s developmental level.
Helps determine what types of interventions are most likely to be effective.
Examples of Developmental Theories:
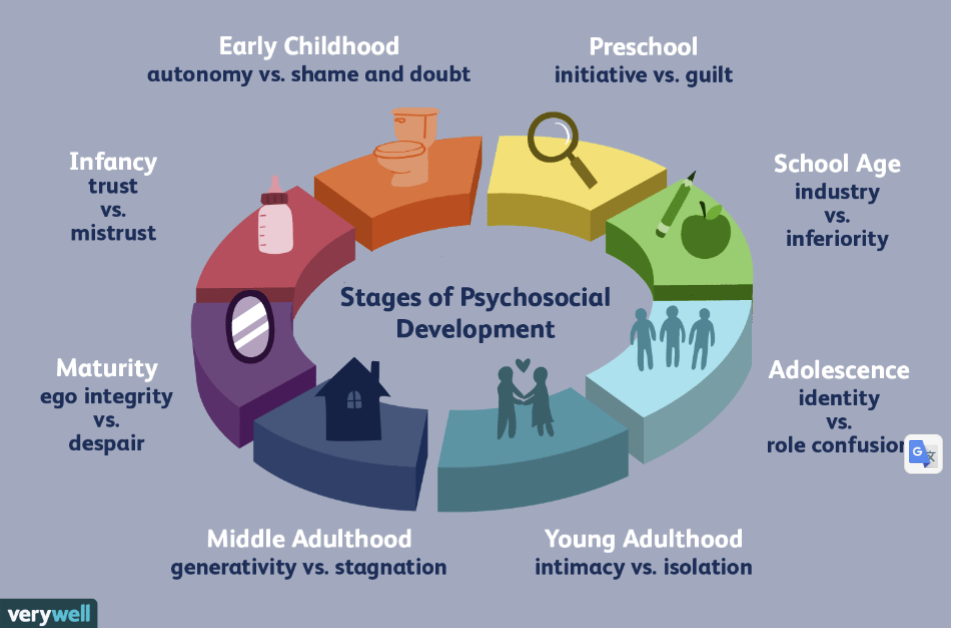
Psychosocial Development = Erikson
8 psychosocial life stages for personality development.
Personality evolves throughout life in consecutive stages.
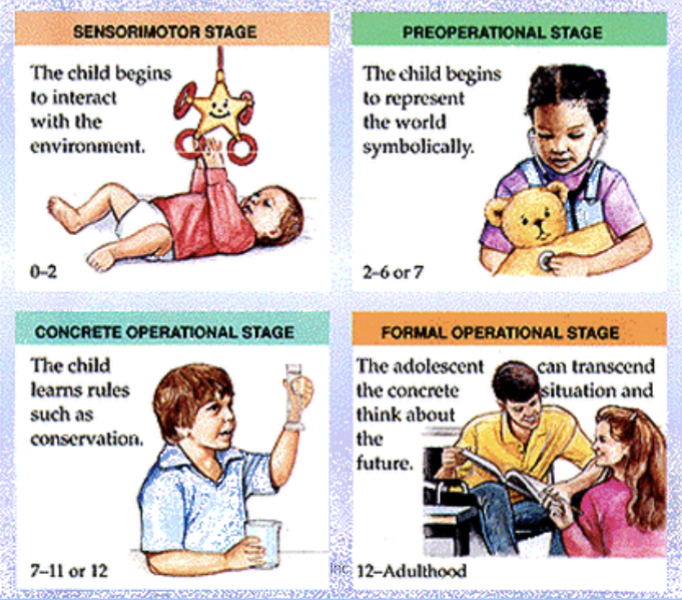
Cognitive Development = Piaget
4 cognitive stages.
Erikson’s Stages of Psychosocial Development
Piaget’s Stages of Cognitive Development
Outpatient Care Settings
Primary care providers.
Specialized psychiatric care providers
Patient-centered medical homes (PCMHs)
Patient-centered
Comprehensive Care
Coordination of Care
Improved Access
Systems Approach
Community mental health centers
Psychiatric home care
Assertive community treatment (ACT)
Intensive outpatient programs and partial hospitalization.
Other outpatient venues for psychiatric care.
Telepsychiatry
Mobile mental health units
Emergency Care - Comprehensive Emergency Service Model
Dedicated psychiatric space and staff, often affiliated with a full-service emergency department (ED) in a hospital or medical center.
Emergency Care - Hospital-Based Consultant Model
No dedicated space or seperate staffing; psychiatric staff on-site or on-call for ED.
Emergency Care - Mobile Crisis Team Model
Stabalization in the field to assess and de-escalate.
Prevention in Outpatient Care - Primary Prevention
Occurs before any problem appears.
Seeks to reduce rate of new cases.
Prevention in Outpatient Care - Secondary Prevention
Early identification of problems, screening, and prompt and effective treatment.
Prevention in Outpatient Care - Tertiary Prevention
Treatment with a focus on preventing progression.
Closely related to rehabilitation.
Inpatient Care Settings
Crisis stabilization/observational units.
General hospital and private hospitals.
State psychiatric hospitals.
Inpatient Psychiatric Nursing Care
Completing Comprehensive data collection that includes the patient, family, and other health care workers.
Completing comprehensive data collection that includes the patient, family, and other health care workers.
Developing, implementing, and evaluating plans of care.
Assisting or supervising mental health care workers.
Maintaining a safe and therapeutic environment.
Facilitating health promotion through teaching.
Monitoring behavior, affect, and mood.
Maintaining oversight of restraint and seclusion.
Coordinating care by the treatment team.
Rights of the Hospitalized Patient
Hospitalized patients retain their rghts as citizens.
Patient’s need for safety must be balanced against patient’s rights as a citizen
Mental Health facilities have written statements of patient’s rights and applicable state laws.
Teamwork and Collaboration
Members of each discipline are responsible for gathering data and participating in the planning of care.
Treatment plan or clinical pathway provides a guideline for patient’s care during hospital stay.
Nurse’s role is often to lead planing meetings.
For standardization in treatment and improved outcomes, inpatient unis use clinical pathways.
Therapeutic Milieu
Surroundings and physical environment.
Managing behavioral crises.
Safety
Unit design
Goals of unit design:
Promote an environment of safety and empower patients to partner with clinical staff and take ownership of their own health and safety.
Specialty Treatment Settings
Pediatric psychiatric care
Geriatric psychiatric care
Veteran’s administration centers
Forensic psychiatric care
Alcohol and drug use disorder treatment
Self-help options
Family Therapy
The focus is on the family as a system, rather than each person as an individual.
Families can be health or dysfunctional in one or more areas of functioning.
Family Assessments
Include focused interviews and use of various family assessment tools.
Concepts Related to Family Dysfunction - Scapegoating
Family member with little power is blamed for all the problems within the family.
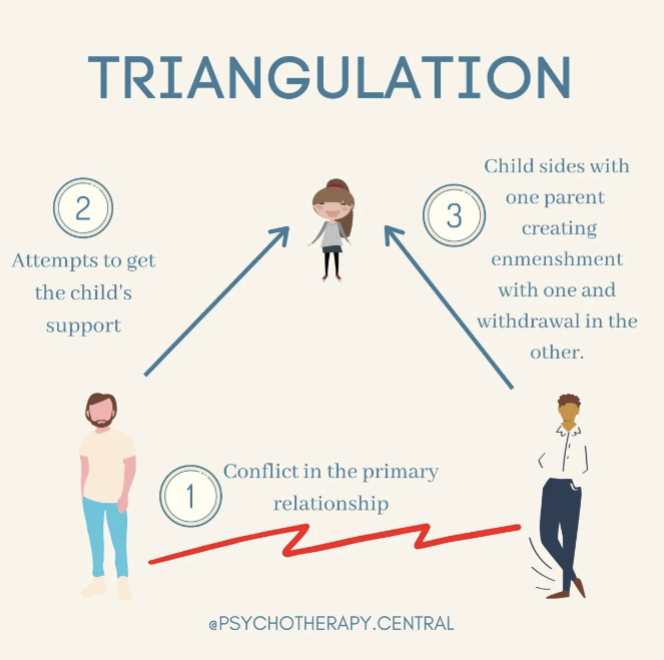
Concepts Related to Family Dysfunction - Triangulation
A third party is drawn into the relationship with two members whose relationship is unstable.
Concepts Related to Family Dysfunction - Multigenerational Issues
Emotional issues within a family that continues for at least three generations.
Areas of Functioning - Communication
Healthy Families
Clear understandable messages between family members, and each member is encouraged to express individual feelings and thoughts.
Dysfunctional Families
Blaming: Blame others to shift focus from own inadequacies.
Manipulating: Dishonest to support own agendas.
Placating: One member takes responsibility for problems to keep peace at all costs.
Distracting: Inserts irrelevant information during problem-solving.
Generalizing: Members use overall descriptions for a family encounters, such as “always” and “never.”
Areas of Functioning - Management
Healthy Families
Adults of family agree on important issues, such as rule-making, finances, and plans for the future
Dysfunctional Families
Management can be chaotic, with a child making decisions at times.
Areas of Functioning - Boundaries
Healthy Families
Distinguishable family roles. Clear boundaries define roles of each member are understood by all
Dysfunctional Families
Enmeshed boundaries: Individual roles are unclear because roles and feelings are blended.
Rigid boundaries: Rules are not flexible, family members isolate themselves, and communication is minimal.
Areas of Functioning - Socialization
Healthy Families
All members interact, plan, and adopt healthy ways of coping. Children learn to function as family members, as well as members of society.
Dysfunctional Families
Children do not learn healthy socialization skills within the family and have difficulty adapting in society.
Areas of Functioning - Emotional/Supportive
Healthy Families
Emotional needs of family are met most of the time, and members have concerns about each other.
Dysfunctional Families
Negative emotions most of the time. Members are isolated and afraid and do not show concern for each other.
Focus of Family Therapy
Family needs and problems with family dynamics
Improving family functioning
Goals of Family Therapy
Learn effective ways for dealing with mental illness within the family.
Improve understanding among family members.
Maximize positive interactions among family members.
Interventions
Family Psychoeducation
Nurses work with families to provide teaching.
EX: RN teaches a family on medication administration, or ways to help a family member manage their mental health disorder.
Mobilize Family Resources
Improve communication and strengthen the family’s ability to cope with the illness of one member.
Psychological Therapies
Role of psychiatric advanced practice nurse.
What is stress?
The brain’s natural response to any demand, can be physical or psychological stressors.
Stress Management
Ability to cope with stress.
Too much stress or too many stressors can cause distress; stress causes anxiety.
Effects of stressors are cumulative.
Responses to stress are affected by multiple factors- age, gender, culture, life experiences, lifestyle.
Distress
Negative draining energy that results in anxiety, depression, confusion, helplessness, hopelessness, and fatigue.
Eustress
Normal physiological positive energy that motivates individuals and results in positive feelings and purposeful movement.
Defense Mechanism
Can be used to manage conflict in response to anxiety.
Can be adaptive (healthy) or maladaptive (unhealthy).
Examples of common defense mechanisms:
Suppression: Voluntarily deny unpleasant thoughts and feelings.
Repression: Unconsciously putting unacceptable thoughts and feelings out of awareness.
Regression: Sudden use of childlike behaviors.
Displacement: Shift feelings to another less threatening object, person, or situation.
Denial: Pretend the truth is not reality.
Signs of Acute Stress (Fight or Flight)
Apprehension
Unhappiness or sorrow
Decreased appetite
Increased respiratory rate, heart rate, cardiac output, blood pressure
Increased metabolism and glucose use
Depressed immune system
Prolonged Stress (Maladaptive Stress)
Chronic anxiety or panic attacks
Depression, chronic pain, sleep disturbances
Weight gain or loss
Increased risk for myocardial infarction, stroke
Poor diabetes control, hypertension, fatigue, irritability, decreased ability to concentrate
Increased risk for infection
Chronic exposure to stress hormones, specific ally cortisol, weakens the immune system, resulting in increased susceptibility to illness and infection.
Protectie Factors
Increase a client’s resilience, or ability to resist the effects of stress.
Physical health
Strong sense of self
Religious or spiritual beliefs
Optimism
Hobbies and other outside interests
Satisfying interpersonal relationships
Strong social support systems
Humor
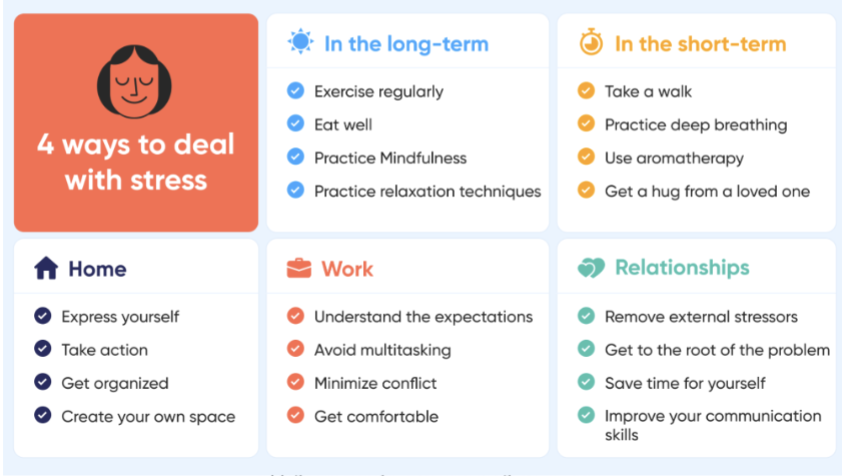
Stress Reduction Strategies
Cognitive Techniques
Cognitive reframing - positive self-talk
Behavioral techniques
Meditation - train mind for greater calm
Guided Imagery - guided through images to relax
Breathing exercises - decrease rapid breathing and promote relaxation
Progressive muscle relaxation - testing specific muscle groups and relaxing them
Physical exercise - yoga, walking, biking, etc.
Stress Reduction Strategies
Priority Restructuring - Prioritize differently to reduce stressors.
Biofeedback - track sleep and heart rates (i.e. device such as smart watch)
Mindfulness - using senses to be mindful and positive of surroundings,
Assertive training - learn to communicate in more assertive manner to decrease psychological stressors.
Other - Music therapy, art therapy, pet therapy, journaling, etc.
Importance of Culturally Relevant Care in Psychiatric Nursing
Increase in diverse population = psychiatric mental health nurses will care for more clients from diverse cultural groups.
Immigrants (especially refugees) and minority groups, who may suffer from effects of low socioeconomic status (such as poverty, discrimination) are at risk for mental illness.
Nurses should promote culturally competent and congruent care - apply evidence-based practice that corresponds with client values, beliefs, practices, and worldview.
Impact of Culture - Nonverbal Communication
Each culture has different patterns of nonverbal communication.
Eye contact, personal space, touch, facial expressions, and gestures.
Impact of Culture - Etiquette
Rules for polite behavior vary between cultures
Impact of Culture - Beliefs and Values
Enculturation - children learn from parents.
Ethnocentrism - Universal tendency of humans to think their way of thinking and behaving is the only correct and natural way.
Cultural Barriers to Mental Health Services - Communication
Interpreters help with language and cultural barriers.
Interpreters should not be relatives or friends.
Cultural Barriers to Mental Health Services - Stigma of Mental Illness
Mental illness may be associated with being weak, dangerous, or a failure.
Stigma and shame can prevent client from seeking help.
Cultural Barriers to Mental Health Services - Misdiagnosis
If culture has body and mind as one entity, somatization can occur (having physical problems for psychological distress).
Cultural Barriers to Mental Health Services - Cultural Concepts of Distress
DSM-5 criteria of how groups experience, understand, and communicate problem behaviors, suffering, or troubling emotions and thoughts.
Cultural Barriers to Mental Health Services - Genetic Variation in PD
How genes affect individual responses to medicines.
Culturally Congruent Care
Applying EBP nursing care that corresponds with patient’s values, beliefs, and worldview (ANA).
Culturally Competent Care
Process of demonstrating culturally congruent practice.
Cultural Awareness
Nurses recognize impact of culture on patient’s health values and practice.
Cultural Knowledge
Nurse learns about diverse cultures.
Cultural Encounters
Nurse interacts with patients from diverse cultures.
Cultural Skill
Nurse performs cultural assessment in a sensitive way.
Ethics
Study of philosophical beliefs about what is considered right or wrong in a society.
Bioethics
Used in relation to ethical dilemmas surrounds healthcare.
Ethical Dilemma
Conflict between two or more courses of action, each with favorable and unfavorable consequences.
Beneficience
The quality of doing good, can be described as charity.
Nonmaleficience
Doing no harm to the client.
Autonomy
Client’s right to make their own decisions. However, the client must accept the consequences of those decisions.
Justice
Fair and equitable treatment for all.
Fidelity
Loyalty and faithfulness to the client and to one’s duty.
Veracity
Honesty when dealing with a client.
Resources for Solving Ethical Client Issues
Code of Ethics for Nurses
Found at the American Nurse’s Association website
Patient Care Partnership
Found at the American Hospital Association’s website
Nurse Practice Act (state specific)
Legal advice from attorneys
Facility policies
Other members of the health care team, including facility bioethics
committee (if available)
Members of the clergy and other spiritual or ethical counselors
Voluntary Admission
Admits self, consents to all treatment
Can refuse treatment, including medications, unless a danger to self or others.
Free to leave the hospital at any time, even against medical advice.
Involuntary Admission
Client enters mental health facility against their will, based on the client’s need for psychiatric treatment, the risk of harm to self or others, or the inability to provide self-care.
At the end of a specified time, the client must have a court hearing or be released.
Criteria must include:
Presence of mental illness.
Poses a danger to self or others.
Demonstrates a severe disability or inability to meet basic necessities including food, clothing, and shelter.
Requires treatment but unable to seek it voluntarily related to the impact of the mental illness.
Generally for 24-96 hours.
Temporary Emergency Admission
Admitted for emergent health care due to inability to make decisions regarding care; varied stay, less than 15 days.
Long-Term Involuntary Admission
Similar to temporary admission ut must be imposed by the courts. Usually 60-180 days, sometimes no set release date.
Marchman Act
Applied to apprehension for substance abuse.
Likelihood person will harm themselves or others.
Baker Act
The Florida Mental Health Act of 1971, lets people with mental illnesses be held against their will for a mental health check, called an examination, for up to 72 hours.
Applied to apprehension for mental health care.
Likelihood person will harm themselves or others.
Due Process in Involuntary Commitment
Writ of Habeas Corpus
Used when patients believe they have been held without just cause.
Challenges unlawful detention.
Least restrictive alternative doctorine
Taking the least drastic or restrictive action.
A nurse’s priority is to promote and provide care to a client in the least restrictive environment.
Discharge Procedures - Unconditional Release
Termination of the legal patient-institution relationship.
Discharge Procedures - Release Against Medical Advice (AMA)
A patient chooses to leave a hospital or healthcare facility before the medical team recommends discharge, despite understanding the risks, often due to personal reasons like cost, work, or feeling better, but this decision increases their risk of readmission and worsening illness.
Discharge Procedures - Conditional Release
Usually requires outpatient treatment for a specified period of time with follow-through evaluation.
Discharge Procedures - Assisted Outpatient Treatment
Similar to conditional release but court-ordered