Parasitology
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
What 3 major questions should clinicians ask before designing a parasite control program?
What parasites occur in the local small-animal population?
Is parasite control justified? (risk of infection, disease potential, zoonotic risk, local zoonotic pressure, clinician’s own risk tolerance)
What control program should be implemented?
What additional considerations affect the choice of parasite control program?
Client risk aversion
Financial constraints
Downsides or limitations of the program (e.g., side effects, compliance, cost, environmental impact)
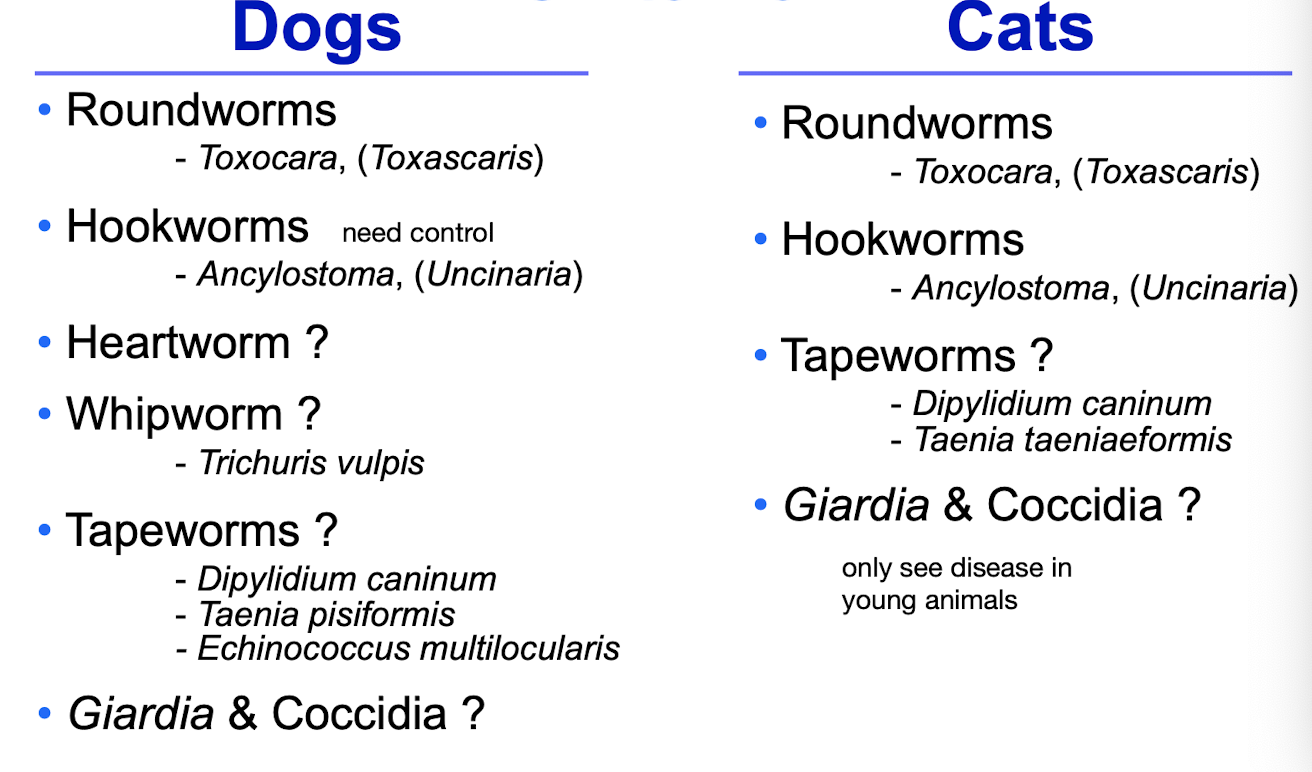
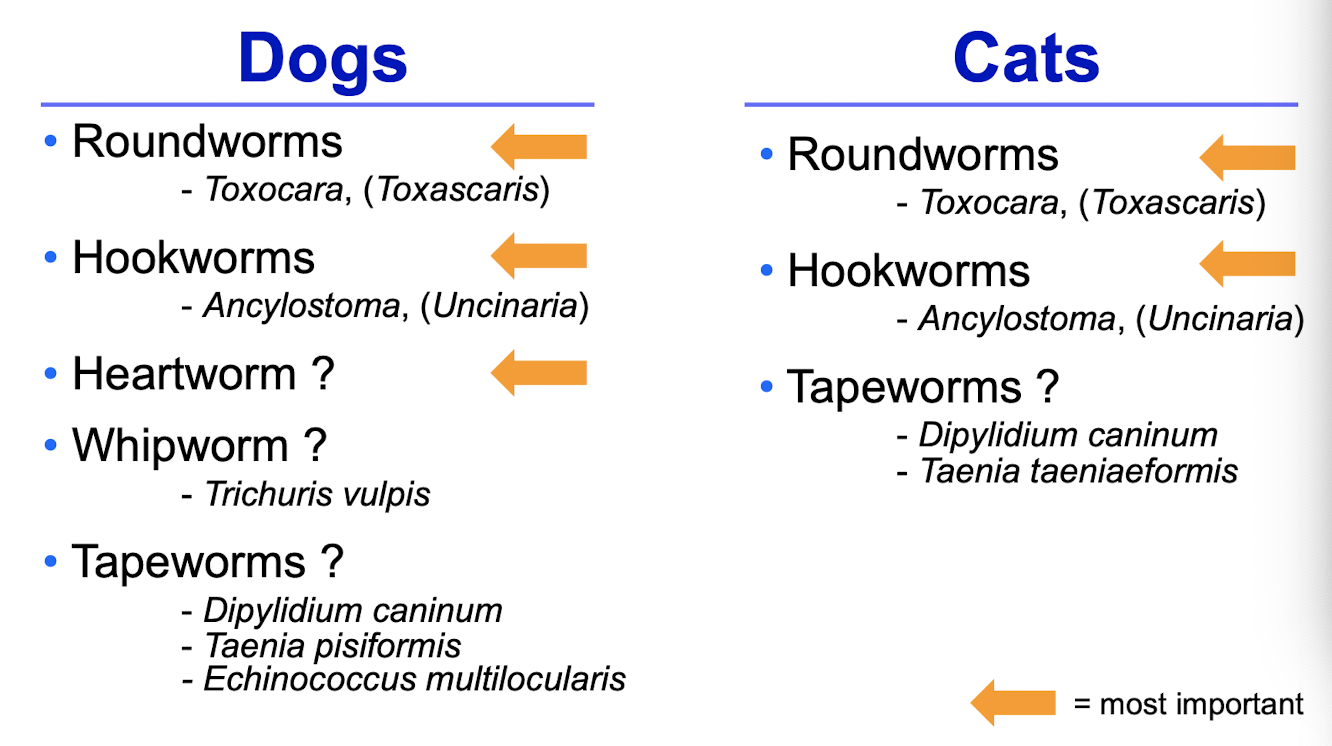
What are the key endoparasites of dogs and cats in Ontario?
Dogs: roundworms, hookworms, heartworm (?), whipworm, tapeworms, Giardia, coccidia.
Cats: roundworms, hookworms, tapeworms, Giardia, coccidia.
Species include Toxocara, Ancylostoma, Dipylidium, Taenia, and Echinococcus (dogs)
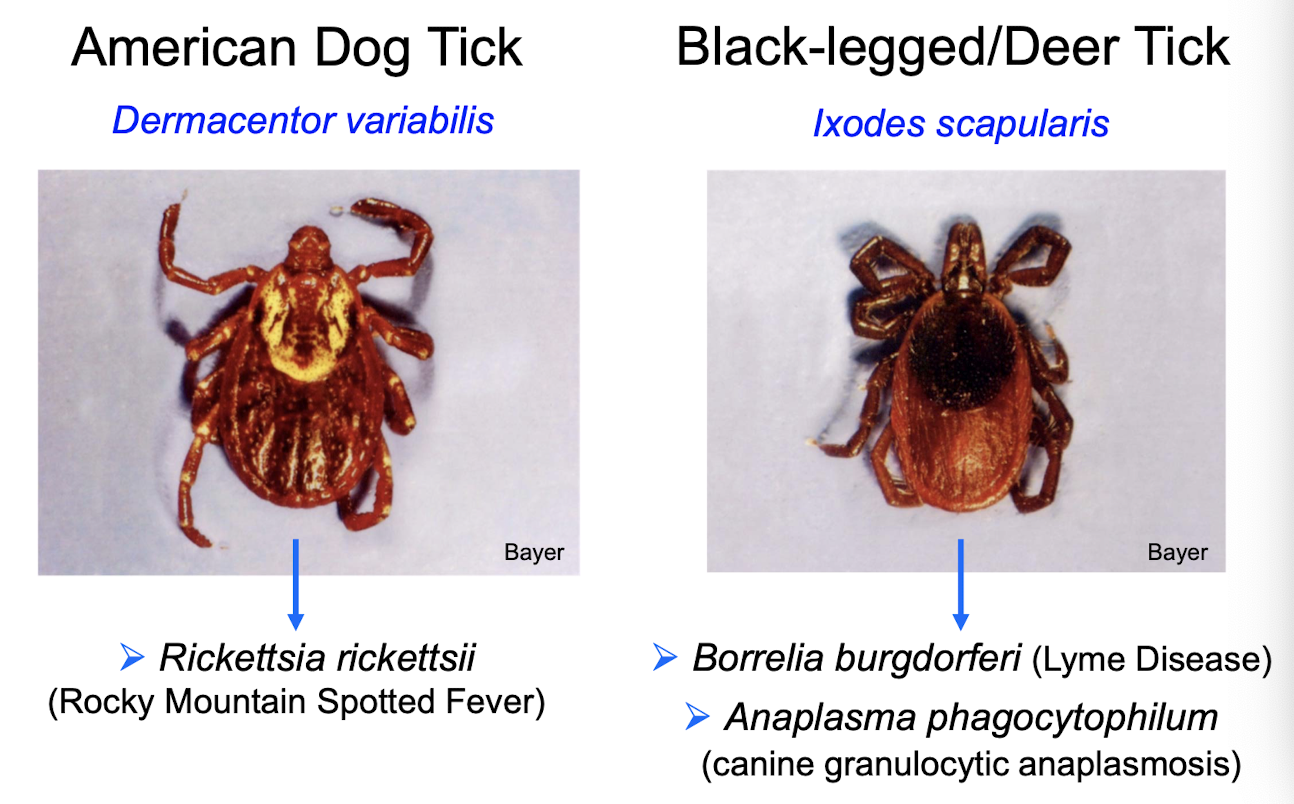
What are the primary ectoparasites of dogs and cats in Ontario?
Fleas
Ticks (Dermacentor variabilis, Ixodes scapularis), animals need to be outside in the grass
Otodectes (in cats)
What principles guide appropriate use of antiparasitic drugs?
Use the narrowest spectrum drug possible.
Use a route that ensures compliance.
Use as few products as possible.
Treat only when the animal is at risk.
Monitor efficacy routinely
Which human groups are at highest risk for parasitic zoonoses, and how should this influence deworming?
YOPIs: young children, older adults, pregnant individuals, immunocompromised patients.
These households should follow more aggressive preventive deworming strategies
Which two parasites are NOT routinely targeted by preventive treatment in dogs/cats?
Giardia → common but subclinical
466 dogs ≥6 months old
Giardia prevalence: 11.8%
More common in <1-year-olds
>95% had no diarrhea (subclinical)
Coccidia
Because subclinical infections are common and typically don’t justify routine treatment
Do Giardia infections in Ontario dogs and cats present significant zoonotic risk?
Mostly no—because genetic assemblages infecting pets are largely host-specific and not the zoonotic A/B assemblages
Which Giardia assemblages affect dogs and cats, and are they zoonotic?
Dogs: C, D (dog-specific, non-zoonotic)
Cats: F (cat-specific, non-zoonotic)
Zoonotic: A & B (infect humans + multiple hosts)
Thus >98% of dog infections in Ontario are not zoonotic
What are the major takeaways regarding Giardia infections in Ontario dogs/cats?
98% of dog infections are dog-specific.
Most cases are subclinical.
Do NOT treat subclinical infections unless zoonotic concern and genotyping cannot be done
How should Giardia be treated when clinical disease is present?
Fenbendazole(use this)
Metronidazole(approved for dogs, but is broad spectrum and can lead to resistance)
Reinfection from environment/coat is common
Treat all animals, bathe on day 1 and last day, clean environment, reduce stress
Should healthy animals be screened for Giardia and how can infection be prevented?
Routine monitoring not justified for healthy animals.
Prevention: keep animal & environment clean and dry; cysts lose infectivity with dryness and freeze-thaw cycles
What animals are most at risk for coccidiosis Cystoiosospora and what factors trigger disease?
Mostly affects dogs <6 months
Triggered by stress: weaning, overcrowding, travel, rehoming
Ideal environment for outbreaks: kennels
Treatment: sulfas, TMS, amprolium, toltrazuril (all off-label)
What are important environmental control strategies for coccidia?
Daily feces removal
Keep floors clean and dry
Oocysts resistant to disinfectants → use steam/pressure wash, hot water
Consider sealing floors
How should subclinical coccidia infections be handled?
Typically not treated so immunity can develop naturally
What is the most important intestinal parasite in cats in Ontario?
Roundworms (Toxocara spp.) are the most significant
What are the 5 major preventive areas for small animals?
Heartworm
Intestinal parasites
Fleas
Ticks
Wellness plans
What lifecycle stage do heartworm preventives target?
They target L3/L4 larvae acquired during the previous month. Preventives work with 1-month “reach-back” activity
What factors determine whether a dog needs heartworm prevention?
Local risk (geography).
Travel history.
Client risk tolerance
What drug classes are used for oral, topical, and injectable heartworm prevention?
Oral: ivermectin+pyrantel, milbemycin(+praziquantel)
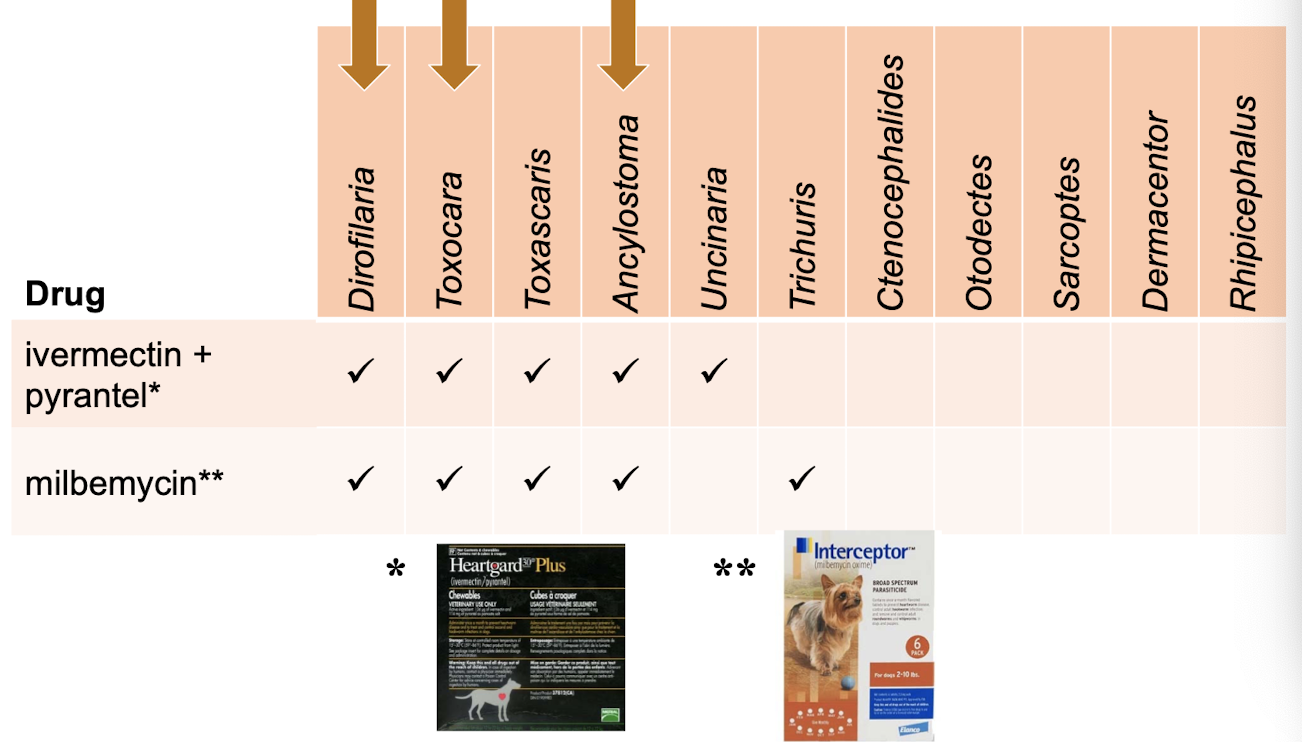
Topical: selamectin, moxidectin+imidacloprid.
Injectable: moxidectin (6 or 12-month).
Spectrum varies widely (fleas, ticks, GI parasites)
What does interceptor used for?
Milbemycin → Dirofilaria, Toxocara, Toxascaris, Ancylostoma, Trichuris
Praziquantel → D. caninum(eating fleas), T. pisiformis, E. multilocularis (eating rodents)
Why might dogs require monthly praziquantel?
To prevent Echinococcus multilocularis egg shedding if they ingest infected rodents—important in high-risk regions/households
What parasites does revolution cover?
Selamectin
Heartworm
Toxocara
Ancylostoma(cats)
Fleas
Some ticks
Ear mites
What parasites does Proheart 6 cover?
Heartworm
Ancylostoma
Uncinaria
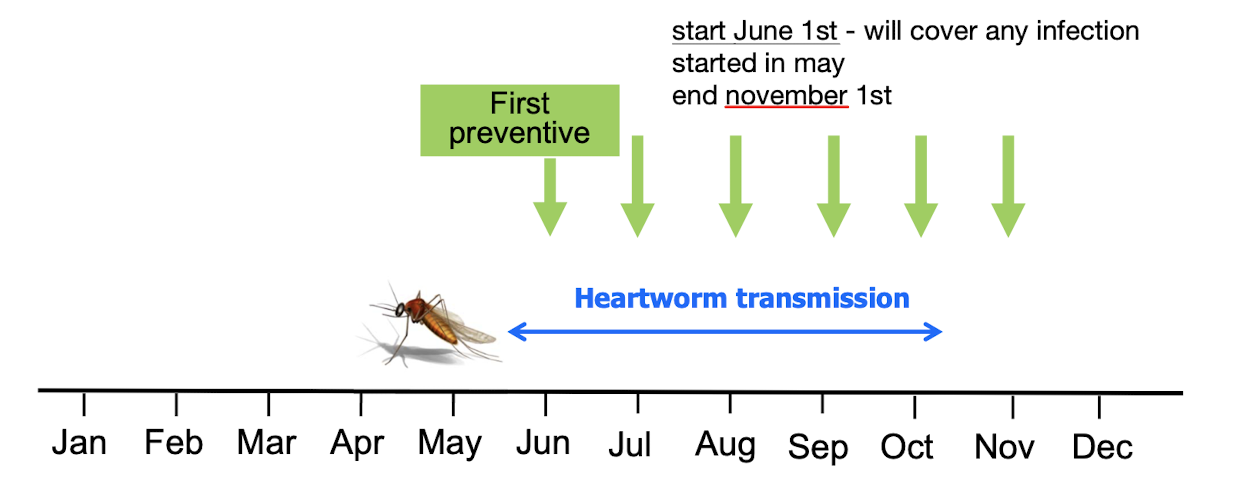
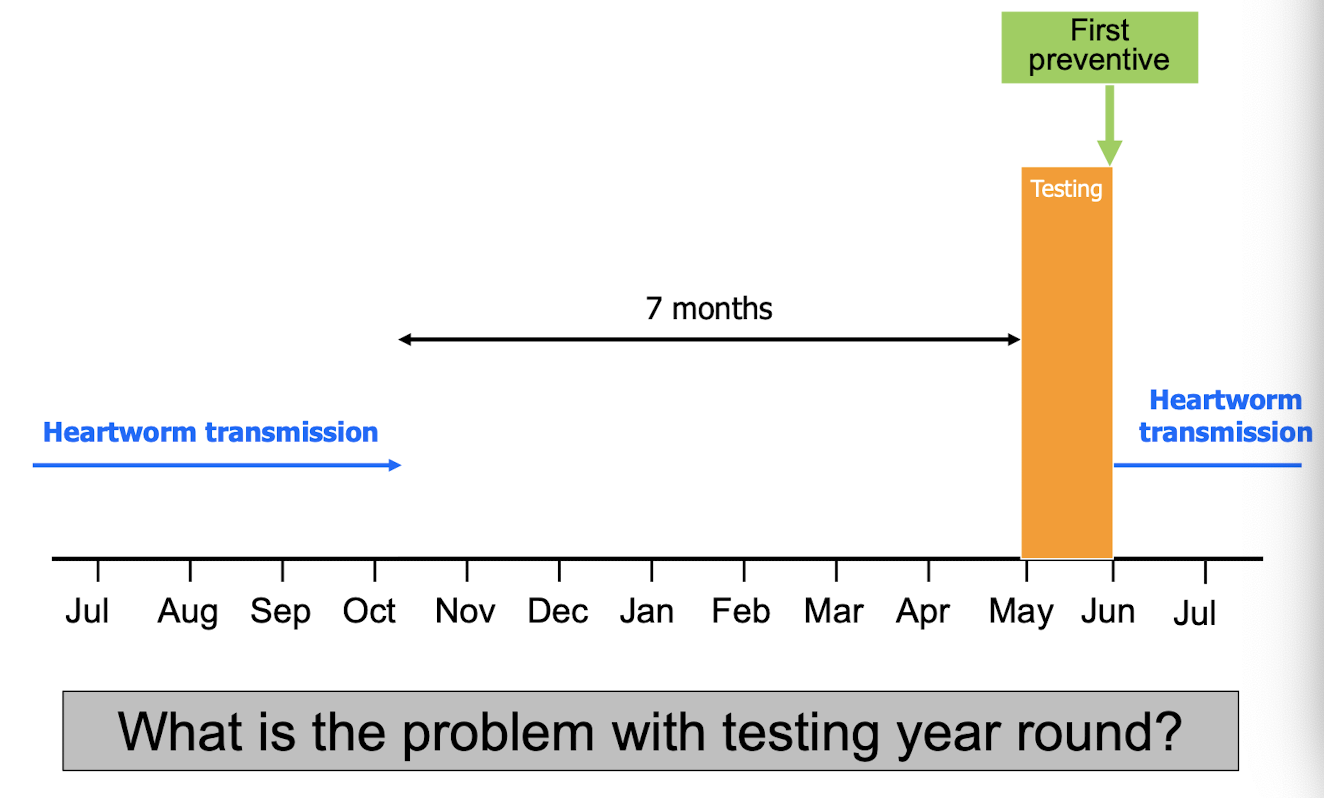
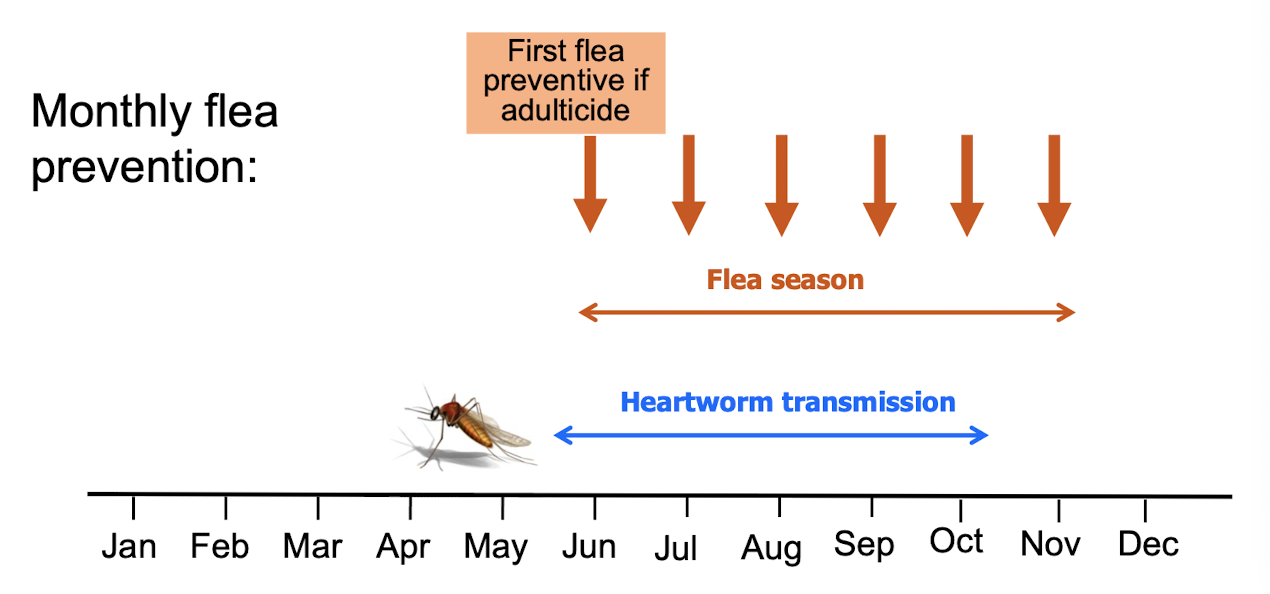
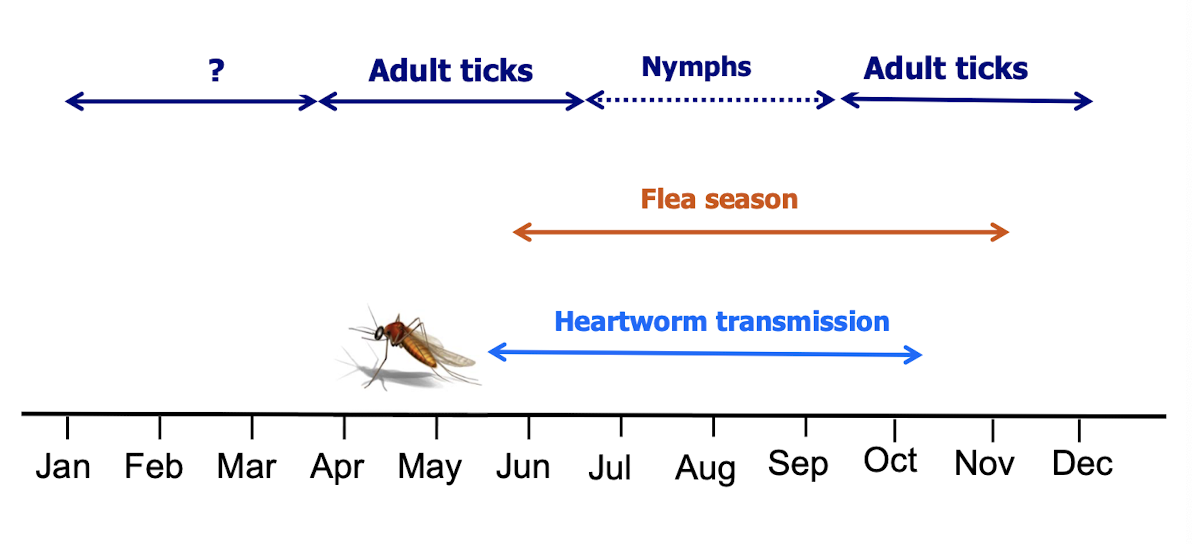
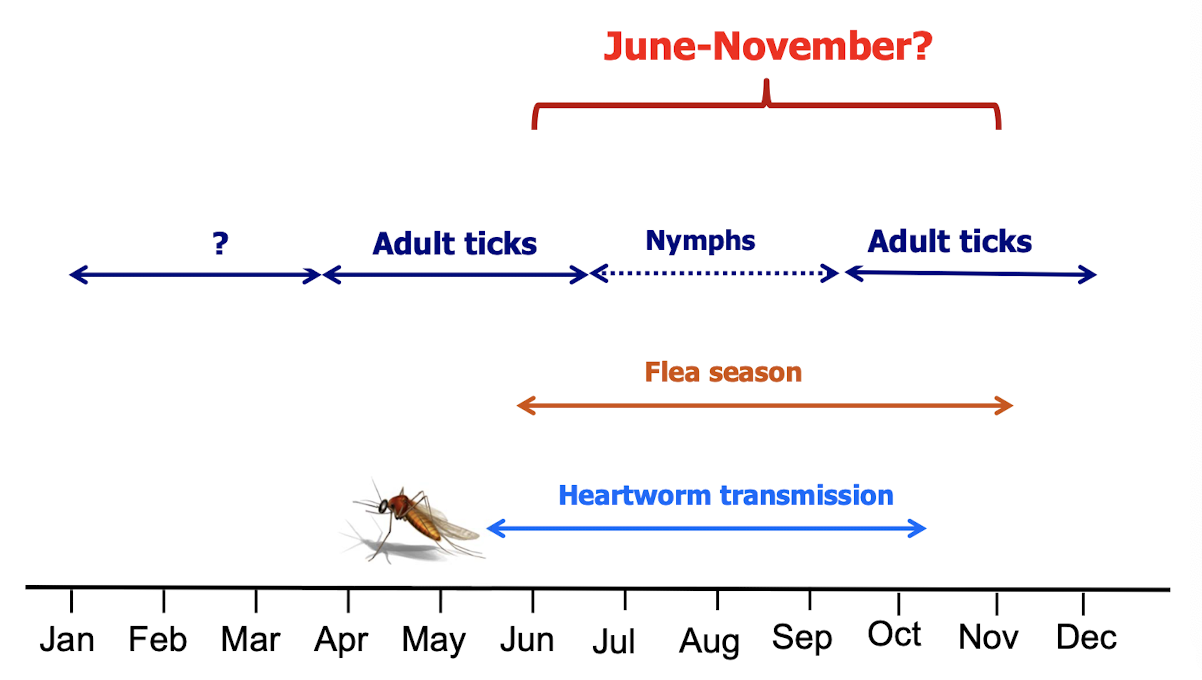
When should heartworm prevention start and end in Canada?
Start: Within 1 month after transmission season begins
End:
Most products: 1 month after transmission season ends
Interceptor Plus / NexGard SPECTRA: 6 months after season.
Credelio PLUS: 2 months after season.
If transmission >6 months → year-round prevention
If a puppy is born in July in a heartworm-risk area, when should it get its first dose?
At ~8 weeks old (typically August–September), within the seasonal prevention window
What is the minimum age to test for heartworm antigen and why?
7 months old, because antigen is not detectable until worms mature (≈6–7 months post-infection)
How often should dogs be tested for heartworm?
At first visit if >7 months.
Annually if following label instructions (USA recommendation).
Less frequent = off-label, must justify based on low risk + informed consent
What steps should be taken if a dog tests heartworm antigen positive?
Repeat test using fresh sample.
Perform microfilaria test (Knott’s or Difil).
Assess travel and compliance history.
Evaluate for true infection vs. false positive/imported case
What additional diagnostics are recommended for dogs that test positive?
Evaluate travel/compliance history.
If clinical signs present:
Thoracic radiographs
Echocardiography
To assess cardiopulmonary impact
Goes to the R heart: immature adults enter the venous bloodstream, which returns blood to the right atrium → right ventricle → pulmonary arteries
What clinical signs occur in heartworm-infected dogs?
Usual: exercise intolerance, coughing, dyspnea.
Severe: weight loss, hemoptysis, ascites, hydrothorax.
Signs depend on worm burden + activity level
Which intestinal parasites in dogs and cats require routine preventive treatment, and why must this be justified?
Roundworms (Toxocara) and hookworms (Ancylostoma) clearly require preventive treatment. Whipworms and tapeworms may or may not justify routine prevention depending on risk. Justification is required because parasite risks vary by region, animal age, lifestyle, and zoonotic potential
What factors influence the risk of intestinal parasite infection in dogs and cats?
Important factors include age (young animals), environment (indoor/outdoor, kennel, urban/rural), season, geographic location, and pregnancy status. Young animals and breeding females have higher risk
What is the relevance of the Toxocara canis life cycle to prevention programs?
Puppies can shed eggs by 3 weeks of age because larvae can be transmitted transplacentally and via milk. This means very early preventive treatment is required, beginning as early as 2 weeks old, to reduce environmental contamination and puppy disease
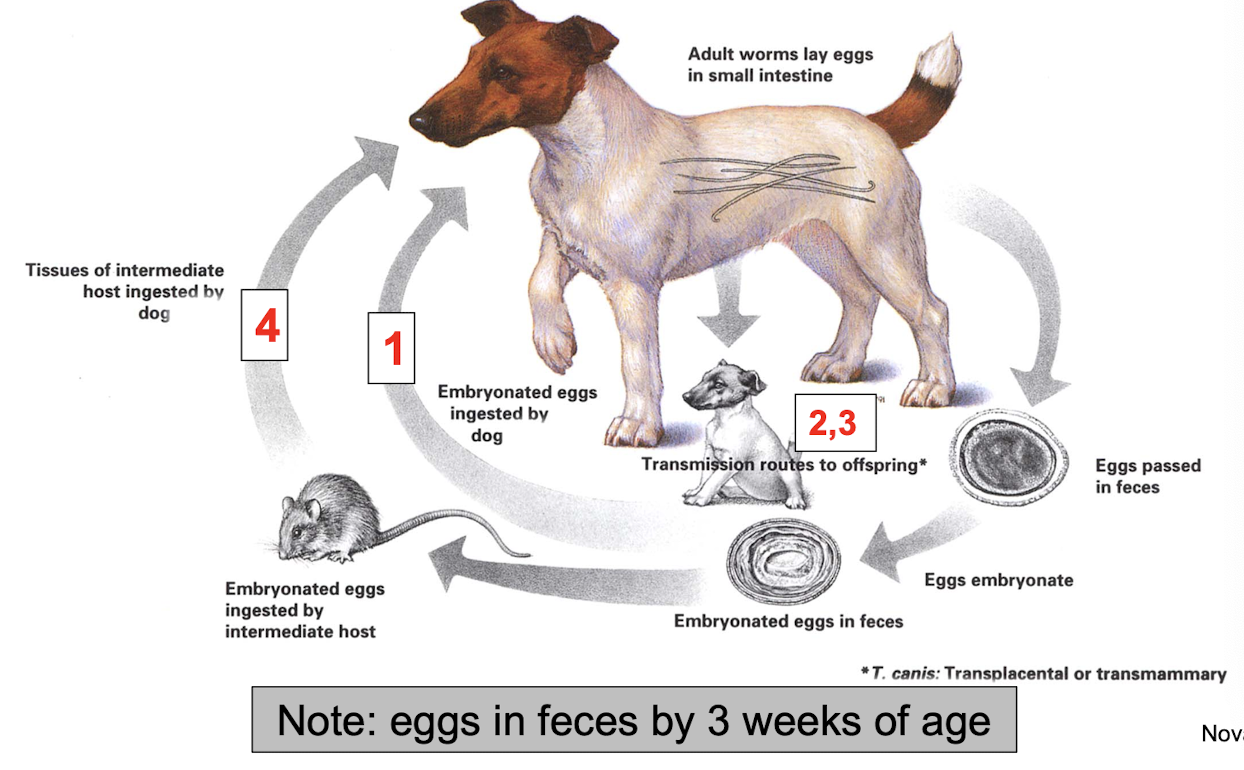
How do Toxocara canis infections persist in bitches and contribute to puppy infection?
Adult dogs accumulate somatic larvae over their lifetime. Around 3 weeks before whelping → larvae reactivate and migrate to the uterus → fetuses → mammary gland → milk → intestine → resulting in puppies being born infected and the bitch shedding eggs
What is the prevalence of Toxocara canis in dogs, and which groups are highest risk?
Overall prevalence in southern Ontario is ~4%, but ~14% in young pups. Adult infection is more common in lactating bitches. Stray dogs have higher prevalence than well-cared-for dogs
What clinical signs are associated with Toxocara canis infection in dogs?
Many cases are subclinical. Clinical signs include emaciation, rough coat, mucoid diarrhea, vomiting (sometimes with worms), and abdominal distension(sometimes due to parasites but mostly muscle weakening from malnutrition). Disease is most severe in young puppies
What is the relevance of the Toxocara cati life cycle to prevention programs?
Cats become infected by ingestion of eggs or infected intermediate hosts. Kittens may be infected transmammarily. Eggs can appear in feces by 4–5 weeks, so early deworming is needed. Hunting cats have higher ongoing risk due to intermediate hosts
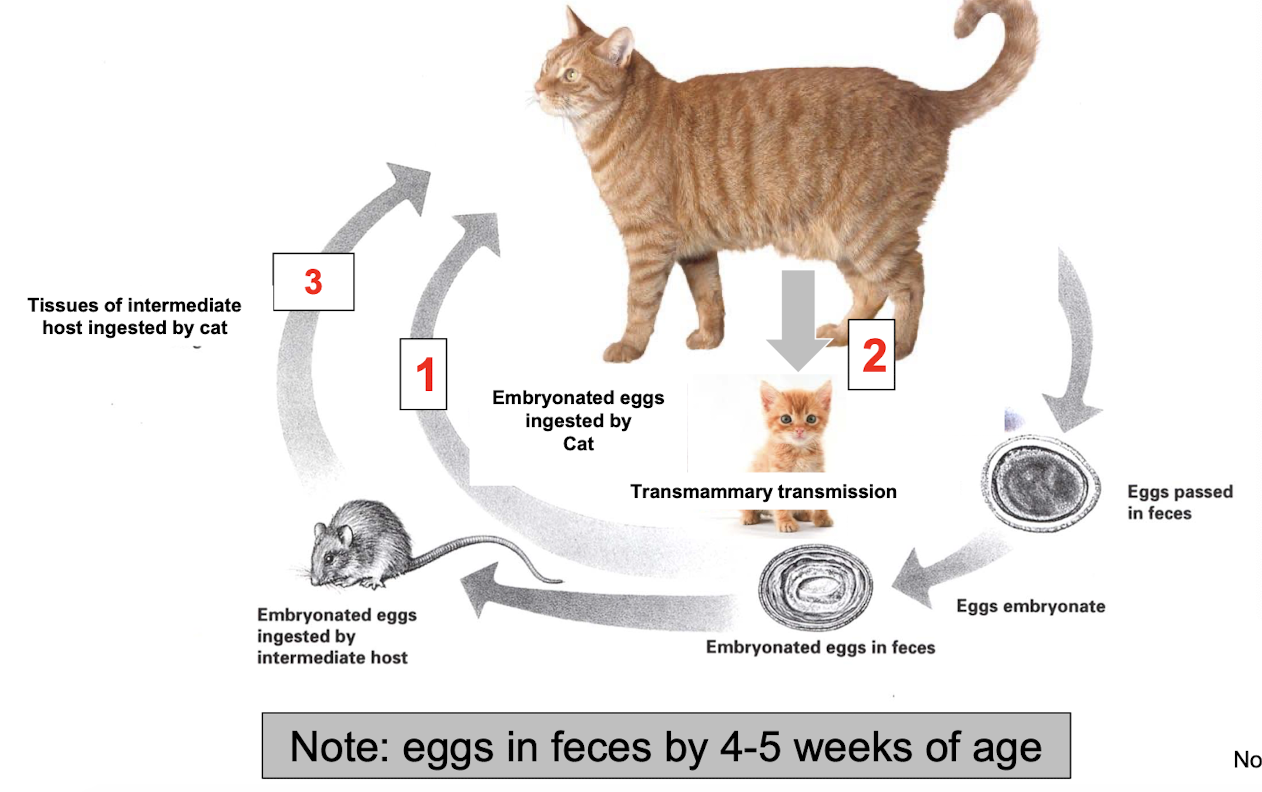
What is the prevalence of Toxocara cati in cats, and which groups are highest risk?
Common infection but rarely see disease. About 5% of southern Ontario cats are infected. Prevalence is higher in kittens and feral cats (~12%). Transmammary infection occurs but is considered a minor route. Patent infections typically appear at 4–5 weeks
What clinical signs are associated with Toxocara cati infection?
Similar to T. canis but generally less severe. Most infections are subclinical. Clinical signs include unthriftiness, intermittent diarrhea, vomiting (± worms), and abdominal distension
What forms of human toxocarosis can be caused by Toxocara species and how are people infected?
Forms:
Visceral Larva Migrans (VLM) — most commonly caused by Toxocara canis
Ocular Larva Migrans (OLM) — both T. canis and T. cati can cause it
Infection route: ingestion of infective Toxocara eggs from contaminated environments
Who is most at risk for VLM and OLM, and what is the incidence in Ontario?
VLM:
Usually occurs in children <4 years old
Risk increases with puppies in the home, pica, and poor hygiene
Ontario incidence: ≤1 case per year, far lower than U.S. estimates
OLM:
Average age: 7–8 years old
Typically no history of pica
Ontario experts do not consider toxocarosis a major public health issue currently
What are the key strategies to control environmental contamination with Toxocara eggs?
Minimize infections in dogs/cats through proper preventive programs.
Prevent fecal contamination of yards and public areas.
Educate owners about zoonotic risks of T. canis and T. cati.
These steps reduce human exposure risk
Why is understanding the Ancylostoma caninum life cycle important for prevention?
Hookworms can infect dogs via skin penetration, ingestion, or transmammary transmission. Larvae migrate through tissues, and puppies can become infected very early. This supports the need for early and repeated deworming, similar to roundworm protocols
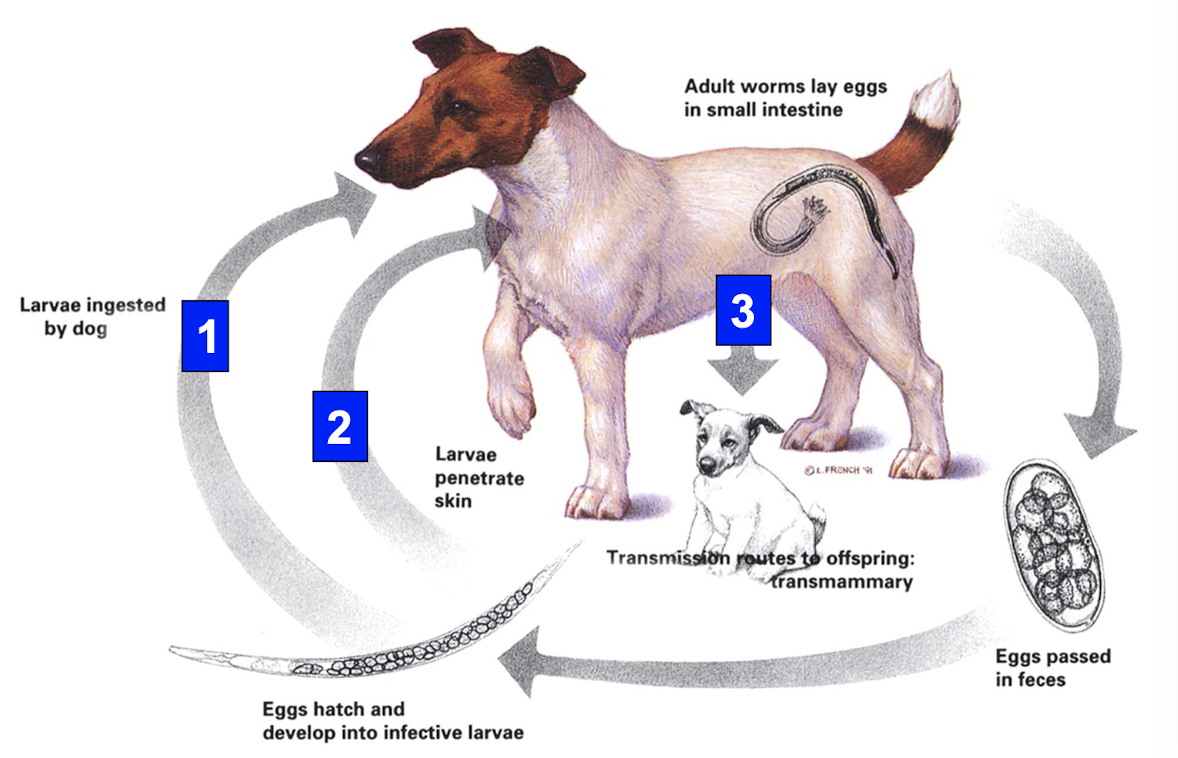
What clinical signs does Ancylostoma caninum cause, and which dogs are most at risk?
Acute disease: anemia, weakness, melena/tarry feces; sudden death possible in very young pups.
Chronic disease: subclinical anemia, especially in juveniles.
Prevalence note: 5.6% infection rate in dogs using off-leash parks in southern Ontario.
By 2025, drug resistance is widespread in the USA
How should severe hookworm problems in litters be managed (primarily outside Canada)?
Subsequent litters of an infected bitch are likely to have the same issue.
Treat pups every 2 weeks from 2 to ~10 weeks of age.
Conservative Toxocara prevention protocols often also control hookworms
Are hookworms in Ontario considered a zoonotic concern?
No — Ontario has no evidence that hookworms (unlike A. braziliense in warm climates) cause zoonotic cutaneous larva migrans locally. The image on the slide shows the typical serpiginous skin lesions seen with A. braziliense infections elsewhere
What are the characteristics of Trichuris vulpis infection in dogs, and who needs prevention?
Most infections are light and subclinical.
Clinical signs: large-bowel diarrhea, hematochezia, mucus, straining.
More common in older dogs and kennel environments.
Prepatent period: 10–12 weeks, so routine preventive treatment in dogs <6 months is questionable.
Mature outdoor dogs do require prevention
How are tapeworm infections usually diagnosed and what clinical signs occur?
Diagnosed by observing segments in feces or attached to fur.
Echinococcus multilocularis segments are too small to see.
Most infections cause no clinical signs, but some animals get perianal pruritus and may scoot
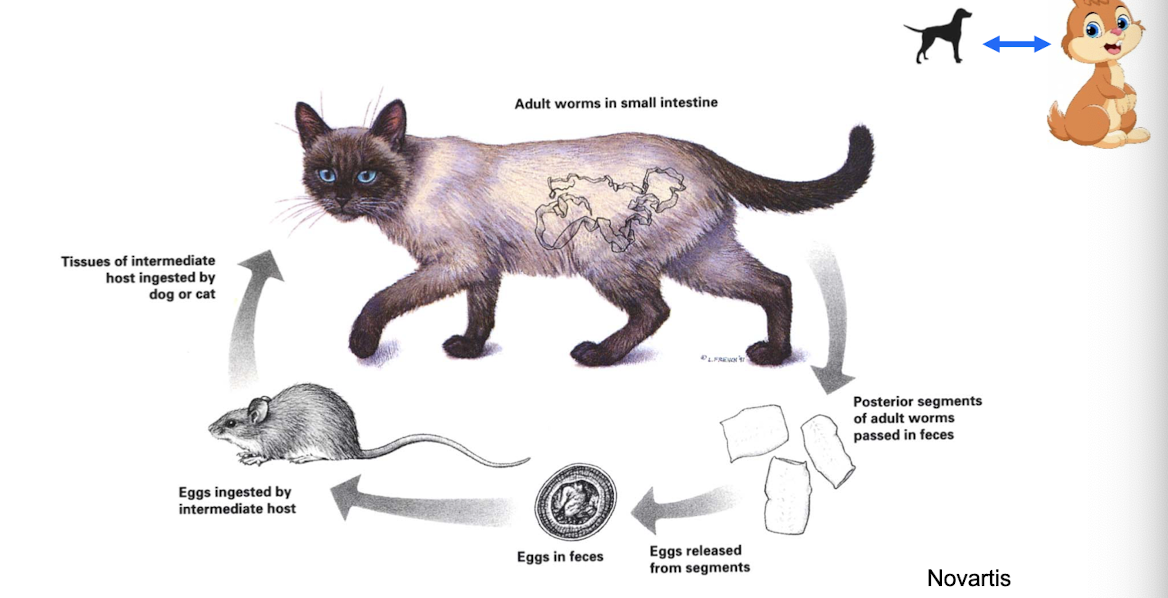
What tapeworms infect dogs and cats in Ontario, and what treatments are used?
Species:
Dipylidium caninum (dogs + cats)
Taenia pisiformis (dogs)
Taenia taeniaeformis (cats)
Echinococcus multilocularis (dogs + cats)
Treatment for tapeworms
Praziquantel (effective against all 4; kills adult + immature stages)
Epsiprantel (effective against 1–3)
Usually one treatment is sufficient
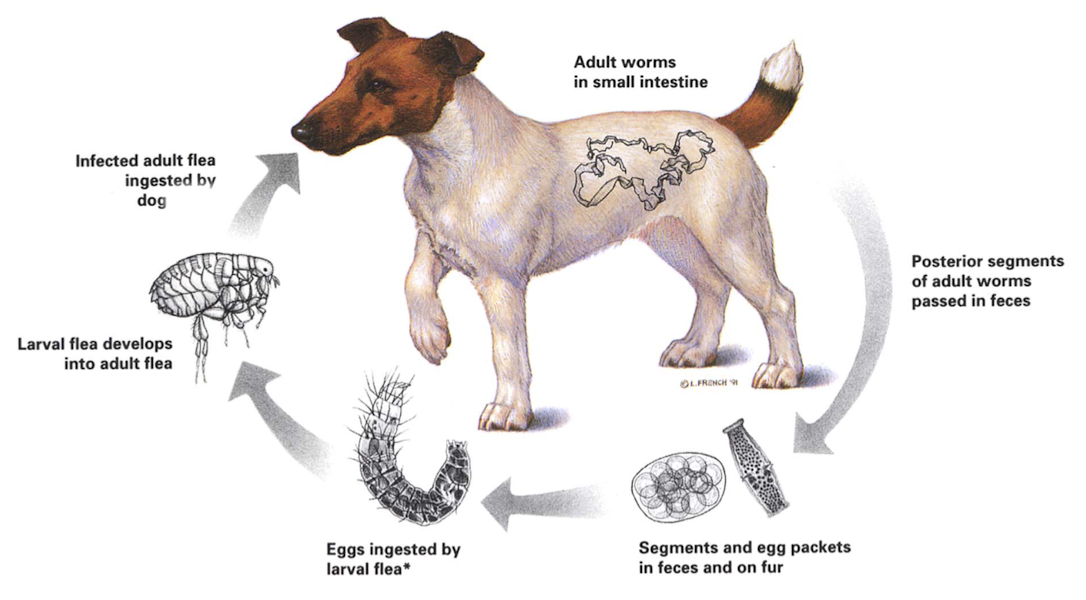
How is Dipylidium caninum transmitted, and what is the key to prevention?
Transmission requires ingestion of an infected adult flea containing cysticercoids. Therefore, flea control is essential for preventing Dipylidium infection. Praziquantel/eprinomectin treat infection, but prevention hinges on preventing fleas
How are Taenia infections acquired, and what is the primary method of prevention?
Dogs/cats acquire Taenia by ingesting infected intermediate hosts (rodents or rabbits). Prevention depends on limiting hunting/rodent exposure. Deworming treats adults but does not prevent reinfection if hunting continues
When is preventive tapeworm treatment considered justifiable in Ontario?
Cats that hunt rodents (Taenia taeniaeformis): treat with praziquantel/epsiprantel 1–4 times/year.
Dogs/cats at risk for E. multilocularis (rodent hunters in high-risk households): consider monthly praziquantel.
Preventive use depends on individual lifestyle risk
Which internal parasites require preventive programs in puppies/kittens and when should first treatment occur?
Puppies: Toxocara canis & Ancylostoma caninum.
Kittens: Toxocara cati + other nematodes depending on environment.
First treatment: 2 weeks of age, because T. canis eggs appear by 3 weeks and infections start in utero; T. cati by 4–5 weeks
What drug is recommended for first treatment in puppies and why are repeated doses needed?
Recommended drugs: pyrantel, fenbendazole, or milbemycin
Additional treatments are required because:
Reinfection is common.
Most drugs only kill adult nematodes, not migrating larvae
What are the recommended intestinal parasite control schedules for puppies and kittens?
Both puppies & kittens: Deworm at 2, 4, 6, 8, 10, 12 weeks.
Then: Monthly until 6 months old.
Ideally: fecal exam at 12 weeks and 6 months (NAVLE)
What parasite control should be recommended for puppies/kittens first seen at 7–8 weeks?
Begin (or continue) the recommended deworming schedule immediately (e.g., pyrantel/fenbendazole), and ensure follow-up treatments are scheduled at proper intervals through 12 weeks and monthly thereafter
Why are U.S. CAPC year-round broad-spectrum recommendations not considered appropriate for Canada?
Because parasite epidemiology differs; Canadian veterinary parasitologists agree year-round broad-spectrum treatment is not justified for all animals in Canada. More targeted, risk-based approaches are appropriate
What is the recommended approach for dogs/cats over 6 months in Canada?
Perform a benefit/risk assessment based on lifestyle and household risk.
A reasonable plan includes:
Deworming 3–4×/year for high-risk animals not on heartworm prevention.
Animals on heartworm preventives receive ≈6 deworming treatments/year automatically.
Low-risk households: deworm based on fecal results
How is parasite control addressed in nursing bitches/queens?
Deworm dams at the same time as puppies/kittens.
No available treatment eliminates somatic larvae of Toxocara/Ancylostoma.
Ivermectin or fenbendazole before/after whelping may reduce transmission, but this is rarely used
Which fecal testing method is most sensitive for detecting intestinal parasites?
Centrifugal fecal flotation using ZnSO₄ is the most sensitive (22× more sensitive than standard smear).
Sensitivities:
Smear: 1×
Floatation: 6×
ZnSO₄: 6×
Centrifugation: 22×
Also consider antigen/PCR as supplemental tools
How often should fecal exams be performed in dogs/cats?
First year: 2–4 times
Adults:
If on year-round prevention: 1–2 times/year
If not on prevention or in high-risk homes: 2–4 times/year
How should you decide between flea-only vs flea + heartworm products?
If fleas are the only concern, a flea-only adulticide may be appropriate. If heartworm is also a concern, select a broad-spectrum preventive with flea activity or combine products for complete coverage
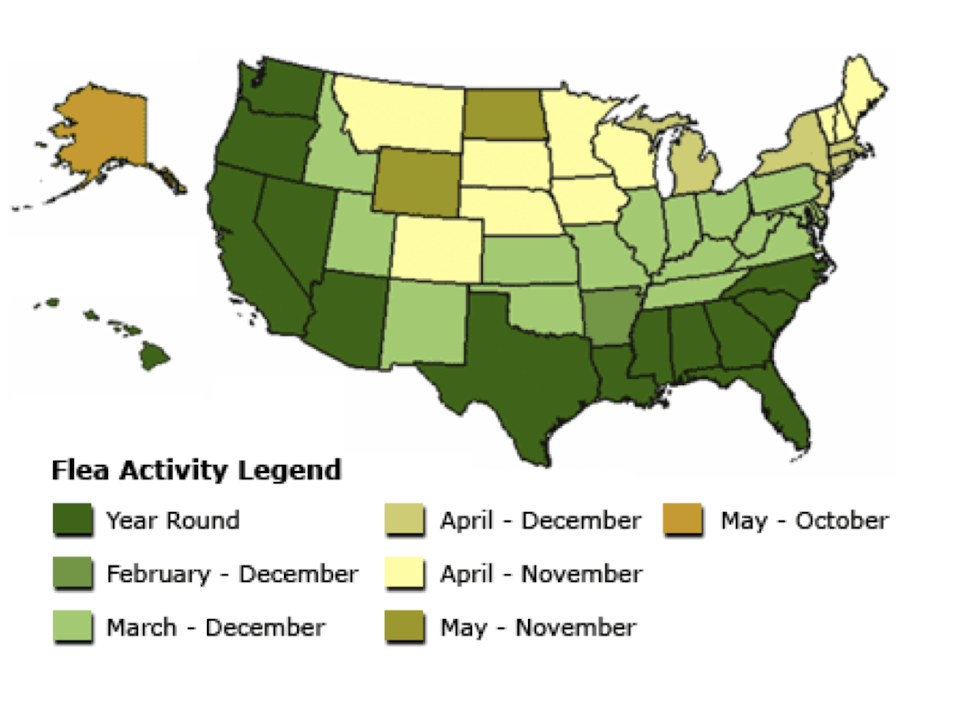
How long is flea season in different regions?
Depends on temperature and climate. Ontario generally has flea activity March–December, with year-round activity in warmer areas (see map on slide)
When does flea season occur in Guelph and when should preventives start?
Flea season spans mainly spring through winter. First flea preventive should be given at the start of the season → June 1 if using monthly adulticides. Heartworm transmission overlaps seasonally
What flea-only adulticide is commonly used for dogs/cats?
Topical imidacloprid (Advantage II) — used when ticks are not a concern
Which ticks and tick-borne diseases are present in Ontario?
Dermacentor variabilis (American dog tick): Rickettsia rickettsii
Ixodes scapularis (black-legged tick):
Borrelia burgdorferi (Lyme disease)
Anaplasma phagocytophilum (canine granulocytic anaplasmosis)
Tick exposure assessment determines need for prevention
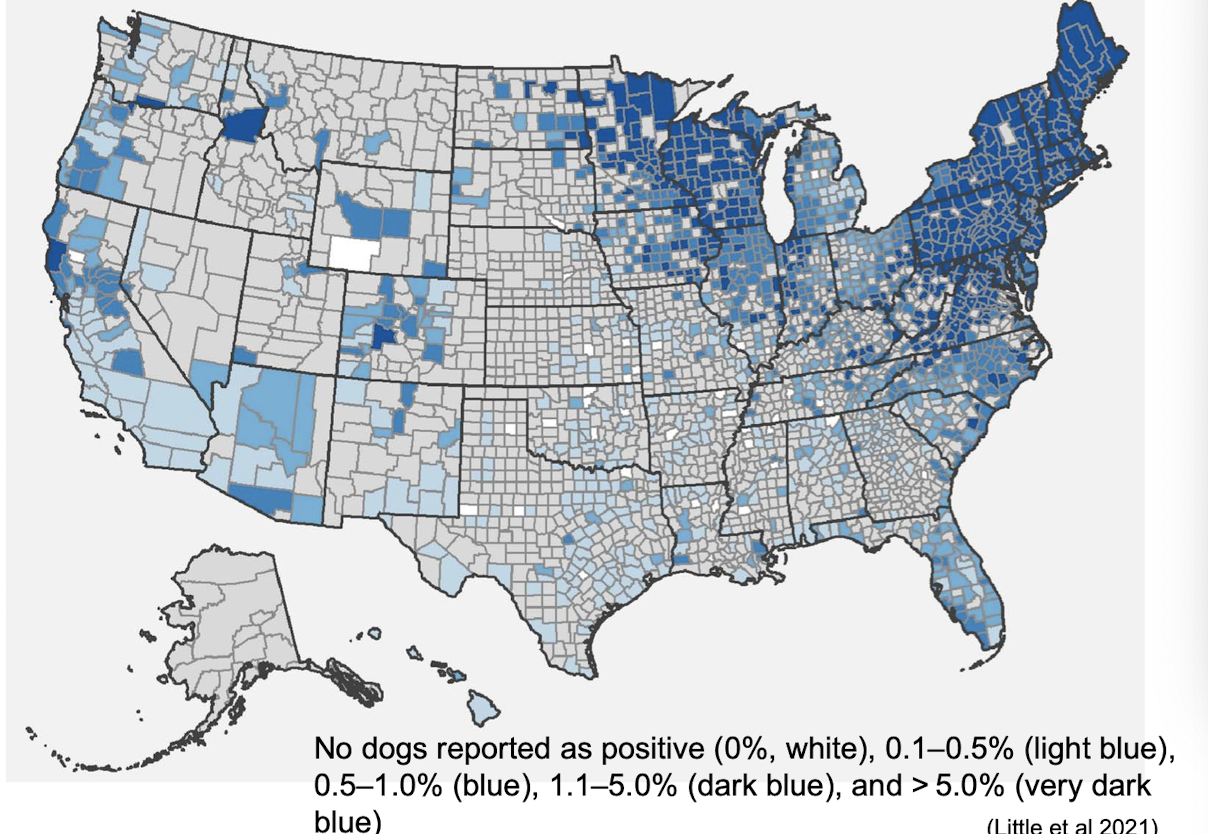
What factors determine whether a pet needs tick control?
Does the pet go outdoors?
Do they live in or near a known risk area?
Do they travel to high-risk areas?
Risk maps help guide decision-making
What does the Ontario Blacklegged Tick Risk Map show?
The map highlights areas with established Ixodes scapularis populations across Ontario. Pets in yellow-highlighted zones have higher exposure risk and should receive tick prevention
What does the U.S. Lyme disease seroprevalence map indicate?
It shows county-level seropositivity of dogs for Borrelia burgdorferi from 2013–2019. Prevalence varies from 0% to >5%, highlighting the patchy nature of Lyme risk and the need for localized prevention decisions
When are adult ticks and nymphs active in Guelph?
Adult ticks: fall and spring
Nymphs: summer
Tick prevention should cover the months when vectors are active depending on lifestyle risk → base it on what ticks are seen and how many
Why must you use two products when prescribing narrow-spectrum heartworm preventives?
Because narrow-spectrum heartworm preventives do not control ticks. If full parasite coverage is needed, a separate tick product must be added. If using two topical products, they should be applied one week apart for safety
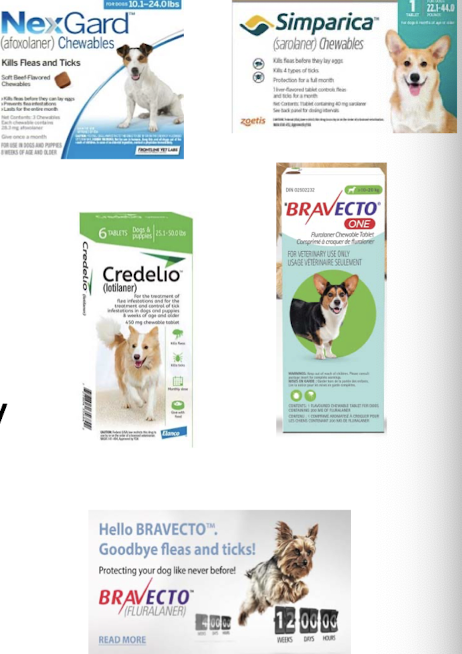
What oral tick/flea products are available and how often are they given?
Monthly: afoxolaner (NexGard), sarolaner (Simparica), lotilaner (Credelio), Bravecto One
3-month: fluralaner (Bravecto), dogs only
What topical and collar tick/flea products are available?
Topical (1 month): permethrin + imidacloprid (K9 Advantix II — dogs only, never give cats), fipronil (Frontline — USA only)
Topical (2 months): Bravecto for cats
Topical (3 months): Bravecto for dogs
Collar (8 months): Seresto (dogs & cats — USA only)
What are the advantages and disadvantages of all-in-one products for dogs?
Advantages:
One product for heartworm, intestinal parasites, fleas, ticks
Increased owner compliance
Disadvantages:
Cost
If the pet reacts to the product, all prevention must be changed
What all-in-one parasite prevention options exist for dogs?
Milbemycin + afoxolaner → NexGard Spectra

Moxidectin + pyrantel + sarolaner → Simparica Trio

Milbemycin + lotilaner → Credelio Plus
What all-in-one parasite prevention options exist for cats?
Moxidectin + Fluralaner → Vitrecto/Bravecto Plus
Selamectin + Sarolaner → Revolution Plus
Eprinomectin + Esafoxolaner + Praziquantel → NexGard Combo

Advantages/disadvantages similar to dogs
When is it appropriate to use “products for everything” in Ontario?
During periods when heartworm, fleas, and ticks overlap in activity — roughly June to November depending on climatic variation and pet lifestyle
What are wellness plans in veterinary practice?
They are packages of preventive and wellness services (vaccinations, exams, tests, antiparasitics, bloodwork) offered over one year, often with discounted pricing or payment plans
What types of services might be included in a veterinary wellness plan?
Exams, vaccines, fecal tests, nutritional consultation, parasite prevention, nail trims, bloodwork, and other diagnostic tests — typically bundled at a discounted rate