Disease III Final
1/314
Earn XP
Description and Tags
Dr. Yacoub (Diabetic Ret, Retinal Vascular Occlusions)
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
315 Terms
____ is the leading cause of blindness in 18-64 y/o with incidence increasing as the pt ages
diabetic retinopathy
what population of people have the highest rate of diabetes?
hispanics, african americans, native americans (15%)
bc of genetics, socioeconomic factors, diet
____ measures the amount of blood sugar in the blood after fasting
fasting blood sugar (FBS)
fasting = no eating/drinking for at least 8 hrs, except water
____ measures the amount of sugar attached to hemoglobin over a 3-4 month window
glycated hemoglobin (HbA1c)
3-4 months bc the life cycle of a RBC is 3-4 months
what lab results are considered normal for diabetes?
HbA1c: 5.6% or lower
FBS: 99 mg/dl or lower
what lab results are considered prediabetic?
HbA1c: 5.7-6.4%
FBS: 100-125 mg/dl
what lab results are considered diabetic?
HbA1c: 6.5% or above
FBS: 126 mg/dl or more
7% HbA1c = ____ mg/dl
7% = 154 mg/dl
add or subtract 14 for every 0.5% up or down
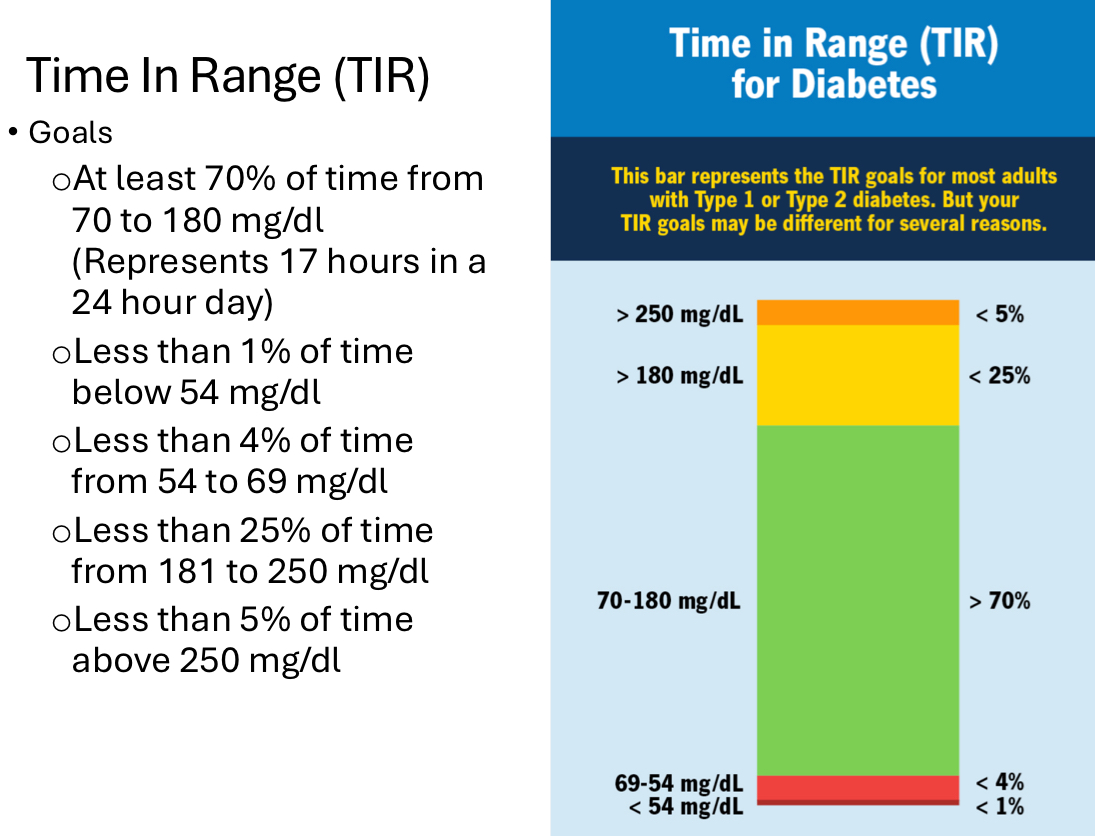
define time in range (TIR)
the amount of time pts with diabetes spend with their blood glucose levels in a recommended target range
a more complete picture of daily glucose fluctuations
helps identify trends in glucose levels
associated with better healthcare outcomes
typically done with continuous glucose monitor
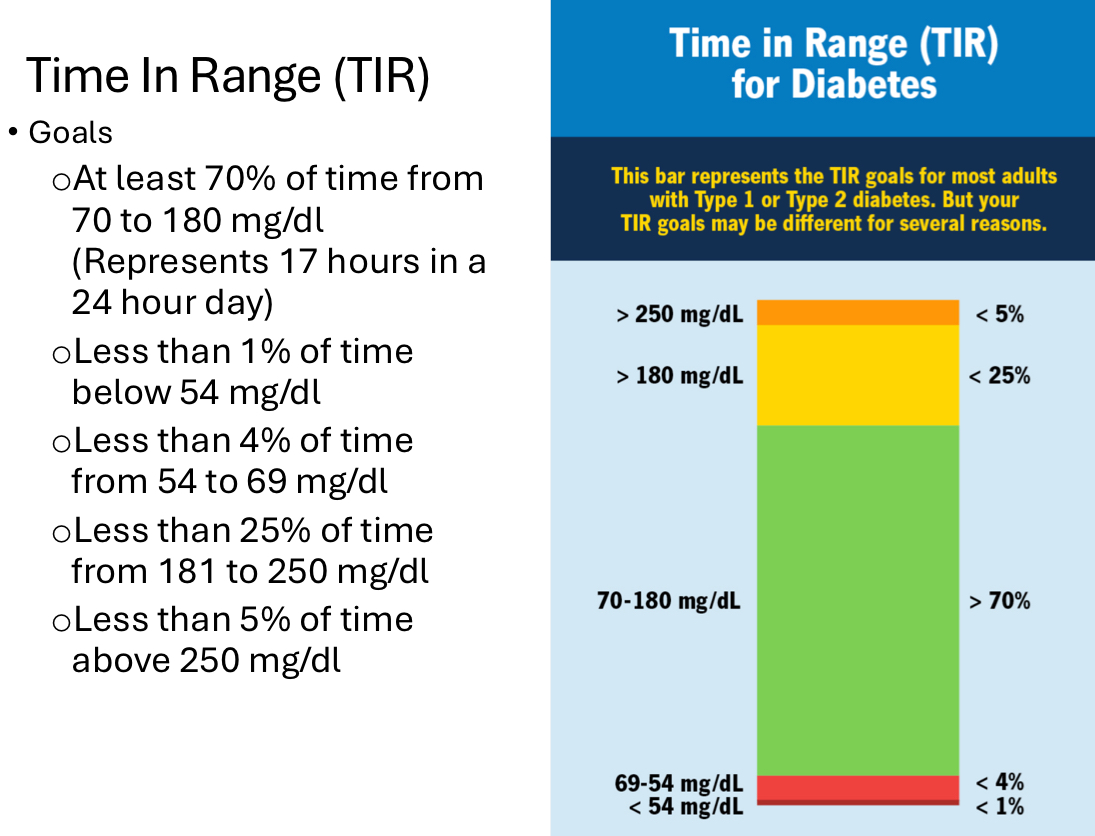
[importance of TIR]
studies have shown that large glucose fluctuations have been associated with the following:
oxidative stress
inflammation
increased risk of cardiovascular disease
decline in cognitive function
decreased quality of life
a lower time in range (TIR) is associated with
more advanced diabetic retinopathy
according to ADA guidelines, a pt with T1DM should have a dilated eye exam ____
T2DM pts should have a dilated eye exam ____
T1DM: DFE within 5 yrs of onset and then DFE every yr
T2DM: DFE at time of diagnosis and then DFE every yr
early diagnosis and treatment of diabetes can decrease severe vision loss (5/200) by
95%
what questions do we ask a diabetic pt?
type of dibetes?
how long have you been diabetic?
is the diabetes in control? seeing a PCP?
any fluctuation of vision?
last FBS/RBS? Hba1c? TIR?
the goal for TIR is to be _____ at least 70% of the time
70-180 mg/dl at least 70% of the time
testing done in DFE
BCVA (may need to refract)
pupils, EOMs, confrontations/VF screener
diabetic pts are prone to cranial nerve palsies, especially CN 6
SLE
look for iris neo at pupillary ruff
IOP
r/o POAG, neo glc
dilated fundus exam
OCT/OCT-A
ERG - shows function of cells too
Amsler grid
pertinent negatives for diabetes
(-) NVI
(-) NVD (neo of disc)
(-) NVE (neo elsewhere)
(-) CSME (clinically significant mac edema) or (-) DME (diabetic macular edema)
*always write assessment/plan regarding diabetic retinopathy even if there’s no sign of diabetic retinopathy
pathophysiology of diabetes
damaged retinal capillaries with increased permeability and occlusion with decreased perfusion → retinal capillary death
which leads to retinal hypoxia and retinal leakage (due to breakdown of inner blood-retina barrier)
diabetes causes an increase in what role players?
advanced glycation end products (AGEs)
sorbital
protein kinase C
VEGF
diabetes leads to an increase in advanced glycation end products (AGEs). why is this bad?
increase in AGEs causes:
apoptosis of endo cells that line retinal capillaries
increase in oxidative stress → retinal vascular damage
increase in inflammation
increase in VEGF
increase in damage to pericytes
disruption of proteins that make up walls of retinal vasculature
diabetes leads to increase in sorbital - why is this bad?
increase in sorbital causes:
increases basement membrane thickneing of retinal vasculature
increases damage to pericytes
increases cataract formation
diabetes leads to an increase in protein kinase C - why is this bad?
increase in protein kinase C causes:
increases damage to pericytes
increases VEGF
increase in platelet adherence/clotting → decrease in retinal blood flow
the ____ of retinal capillaries is typically a thin, fine structure that gives support to the capillary endo cells and pericytes
basement membrane of retinal capillaries
____ surround the retina capillary lumen, controls blood flow, synthesizes basement membrane
pericytes
what causes damaged retinal capillaries with increased permeability and decrease in perfusion in diabetes ?
increase in retinal vascular inflammation
+
damage to pericytes
+
apoptosis of endo cells that line retinal capillaries
+
basement membrane thickening
damaged retinal capillaries with increased permeability and decrease in perfusion will result in
proliferation of endo cells into lumen of capillaries (to fix capillary damage) → further thickening of basement membrane of capillaries
due to being overworked → burnout of endo and vascular repair
body tries to fix it
hypoperfusion vs. hyperperfusion
hypoperfusion: starts the process of diabetic retinopathy
hyperperfusion: leads to further vessel damage and progression
50% of pts with ____ will likely develop proliferative diabetic retinopathy after 20 yrs
type 1 DM
#1 risk factor for development of diabetic retinopathy
age of onset and duration = significant risk factor
the earlier pt is diagnosed, the more likely they will have diabetic retinopathy
____ is thought to increase risk of diabetic retinopathy due to changes in hormones and poor control that tends to occur during this age
puberty
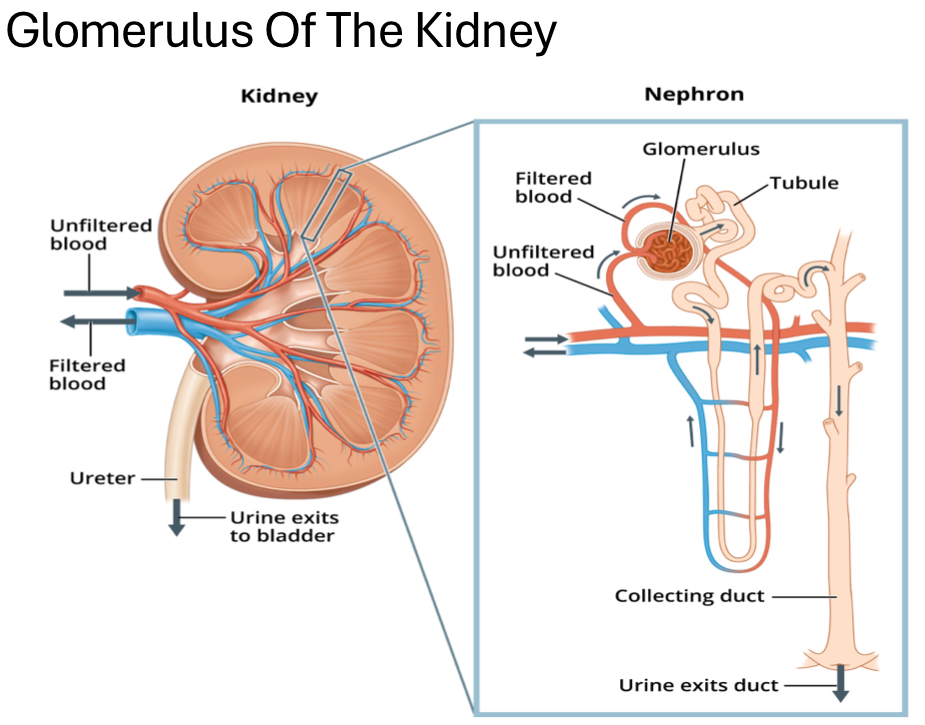
diabetes leads to progressive scarring and strain on the ____, which is found in the nephron, filters blood, and is highly vascular
glomerulus
diabetes leads to progressive scarring and strain on glomerulus → damaged glomerulus →
increase in proteinuria (albumin), blood urea nitrogen (BUN), serum creatine (waste build up in blood due to muscle activity) and decrease in GFR
kidney damage → increase in BP → hyperperfusion in retina
*proteinuria = protein in urine
T/F: HTN increases risk of diabetic retinopathy due to further damage of retinal vasculature and hyperperfusion
true
sleep apnea leads to ____ which in turn causes damage to nerves involved with baroreceptor activity
systemic hypoxia
sleep apnea → damage baroreceptor activity →
nocturnal HTN → further damage retinal vascular and increase in hyperperfusion
____ increases activation of platelets and leukocytes, leading to retinal vascular damage and decrease in perfusion
smoking
how does smoking increase BP?
nicotine causes severe vasoconstriction → increases BP
also increases risk of other CVD
high cholesterol is associated with increased accumulation of ____
retinal exudates (esp when looking at total cholesterol and LDLs)
T/F: high hematocrit was found to be significant risk factor for developing diabetic retinopathy due to increased hypoxia
false - low hematocrit (<40% in men, <34% in women)
hematocrit measures volume % of RBC in blood
T/F: metformin can exacerbate anemia in pts bc it’s been associated with decrease in vit B12 and folic acid (needed for health and development of RBC)
true
hematocrit measures the
volume % of RBC in blood
____ increases systemic glucocorticoids leads to increase in free fatty acids and further insulin resistance
stress
_____ increases risk of insulin resistance, increase in hunger, and increase in calorie intake
sleep deprivation
_____ increases the presence of cytokines, glycerol, and fatty acids, which leads to insulin resistance and a decrease in insulin production
obesity
also associated with CVD
fam hx plays a role too
____ increases risk of retinal vascular permeability, development of retinal neo, and increase in platelet adherence
ocular inflammation

goal for HbA1c in diabetes
7%
BP goal for diabetics
<130/80
or <120/75 if pt has renal damage
why does lisinopril reduce progression of diabetic retinopathy and progression of proliferative diabetic retinopathy ?
lisinopril lowers BP and protects kidney function
____ and ____ decreases overall metabolic demand of the retina
thinning of ganglion cell layer and NFL
T/F: chronic elevated IOP leads to vasoconstriction of retinal vasculature, which decreases risk of hyperperfusion
true
____ and ____ associated with myopia lead to a decreased risk of hyperperfusion
retinal vascular thinning and attenuation
T/F: PVDs tend to happen earlier in myopes, which is a good thing
true - it’s good bc the vitreous tends to have high conc. of VEGF
what are some things that decrease overall metabolic demand of the retina?
loss of retinal tissue
retinal thinning
thinning of GCL and NFL
_____ decreases risk of hyperperfusion and is considered protective of diabetes progression but can lead to asymmetric diabetic retinopathy
mild carotid artery stenosis (15-49% of carotid artery occluded)
the side without the occlusion is going to be worse
moderate-severe carotid artery stenosis also leads to asymmetric diabetic retinopathy, but too much hypoxia
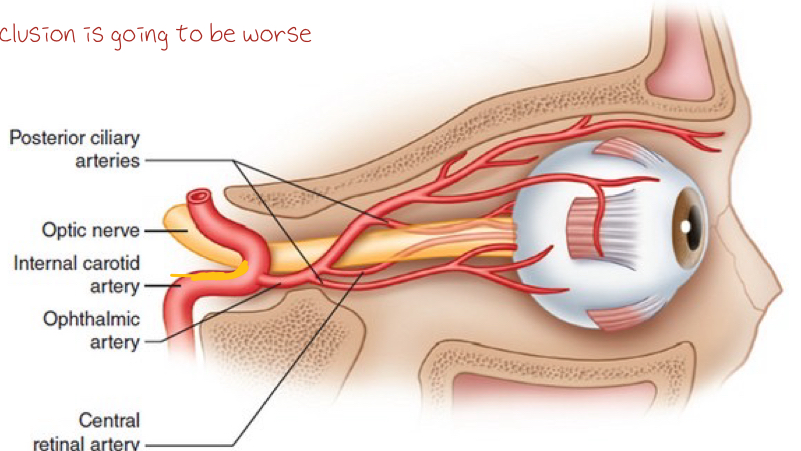
____ (too much hypoxia) increases progression of diabetes and is considered a risk factor and leads to asymmetric diabetic retinopathy
mod-severe carotid artery stenosis (50-100% of carotid artery occluded)
a pt presents with asymmetric dbe and 25% occlusion of right internal carotid artery. which eye will have the more severe diabetic retinopathy?
OS
a pt presents with asymmetric diabetic retinopathy and 75% occlusion of right internal carotid artery. which eye will have the more severe diabetic retinopathy ?
diabetic retinopathy more severe on same side - right eye
what’s the key sign that differentiates non-proliferative vs. proliferative diabetic retinopathy?
neovascularization
signs of non-proliferative diabetic retinopathy (NPDR)
microaneurysms (MA)
dot/blot hemorrhages
flame hemorrahges
roth spots
cotton wool spots (CWS)
venou beading
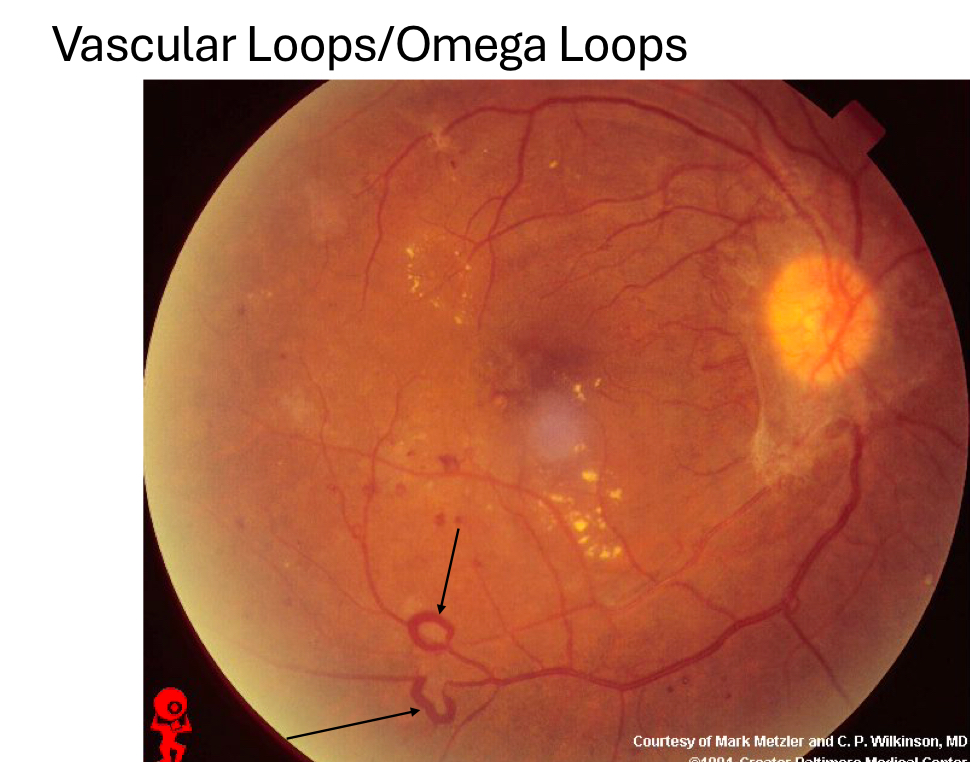
vascular loops/omega loops
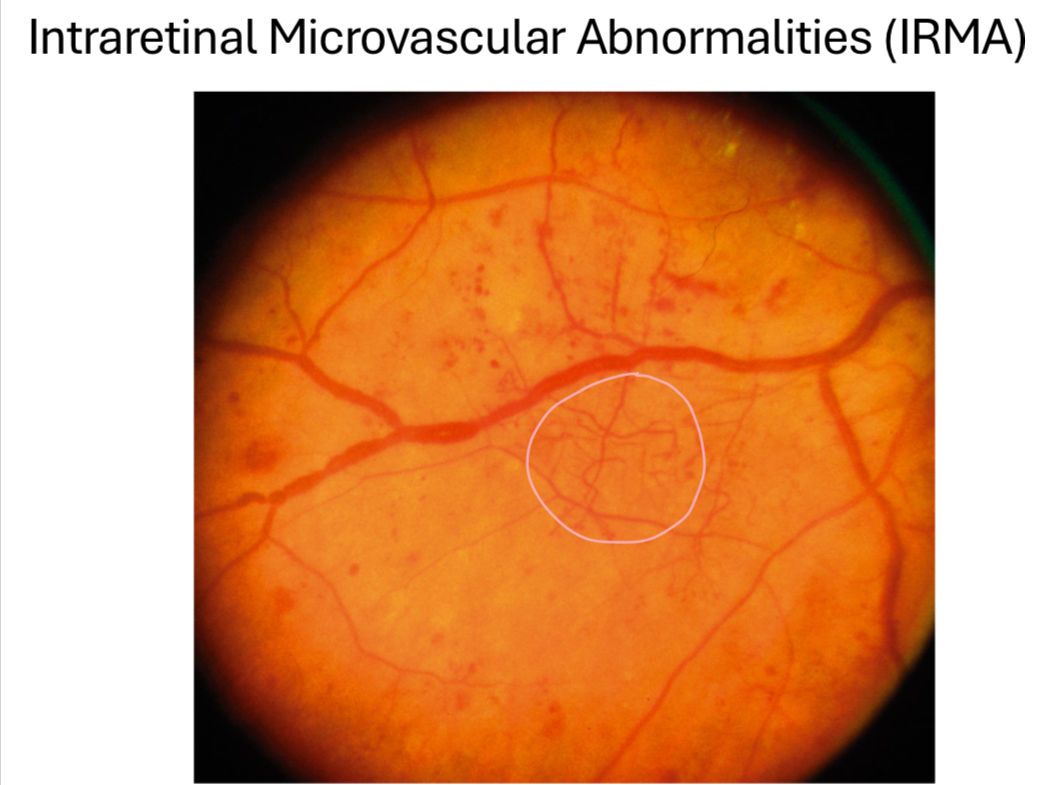
intraretinal microvascular abnormalities (IRMA)
capillary non-perfusion/dropout
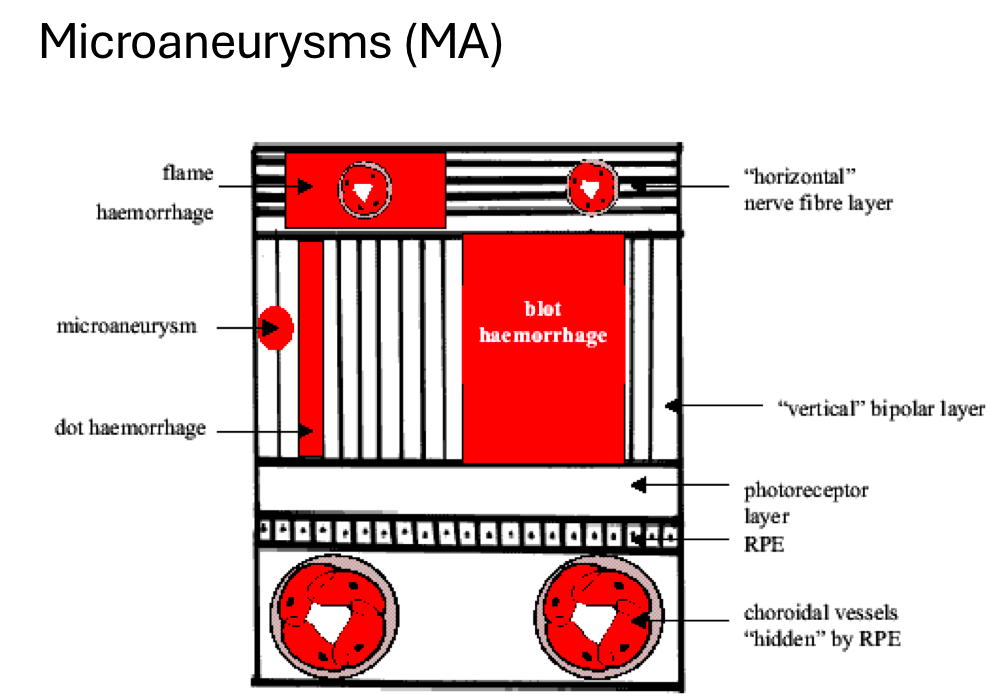
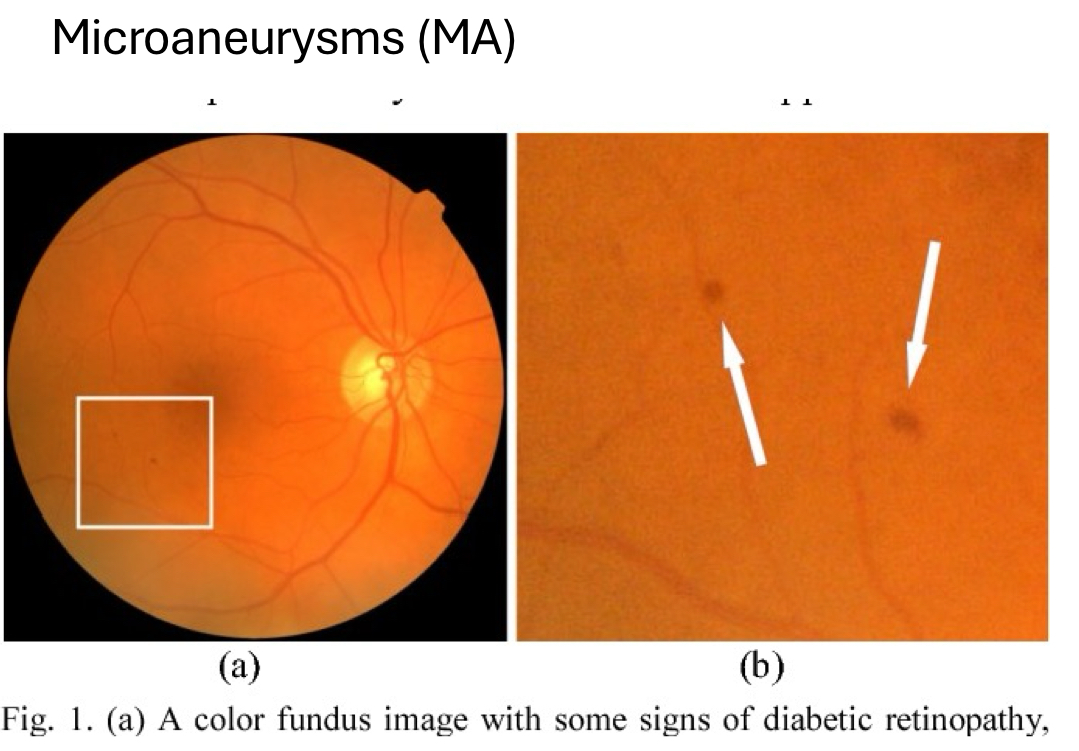
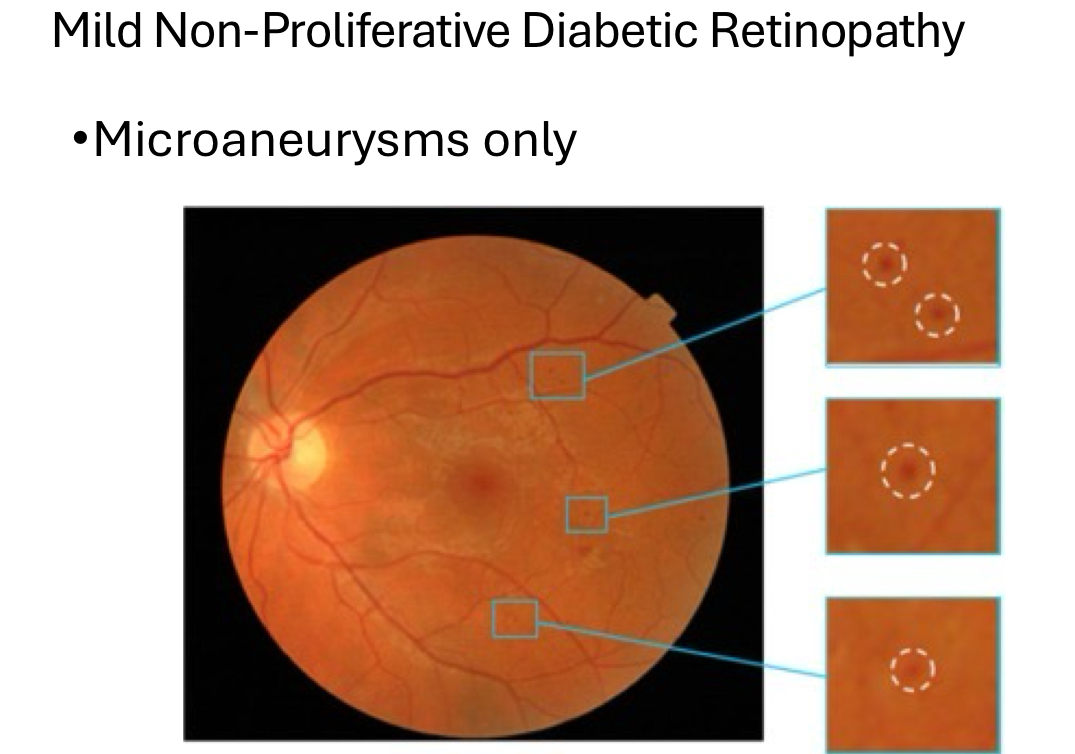
define microaneurysms (MA)
earliest sign of diabetic retinopathy
focal enlargement of capillary walls/outpouching due to weakening of capillary walls
INL (hyper-reflective ring, non-homo inner content on OCT)
temporal to fovea typically
potential to be a permanent finding in retina
best seen with FA, OCT-A
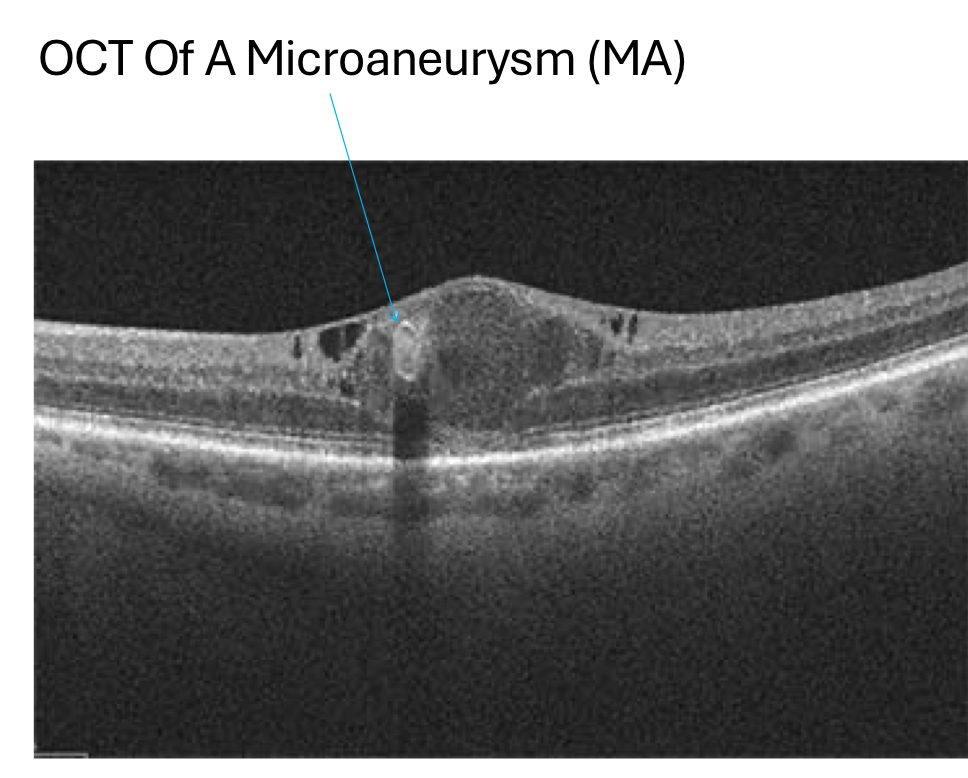
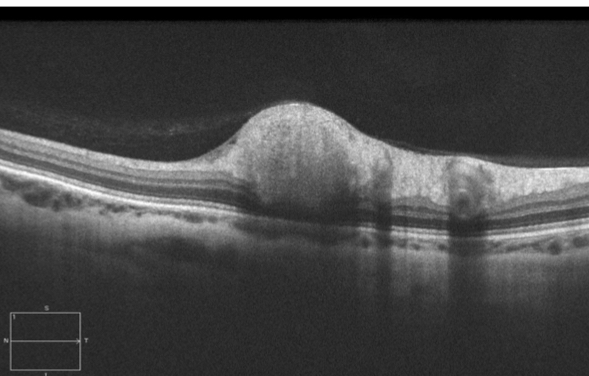
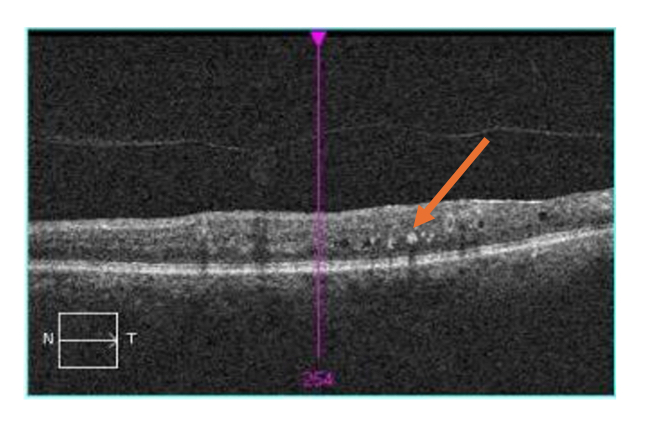
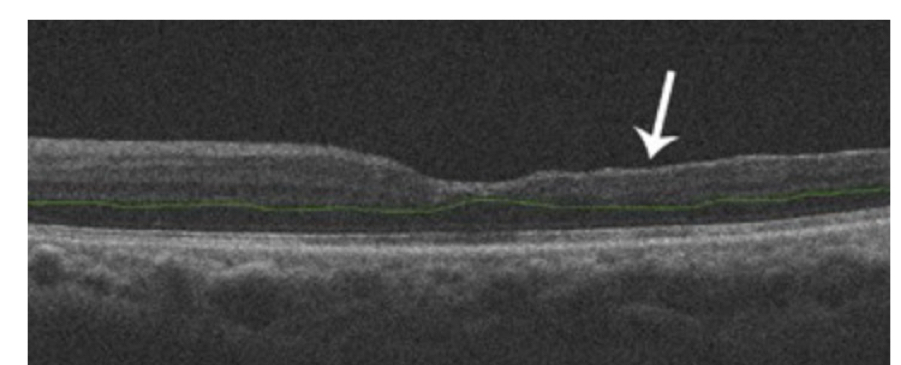
what does a MA look like on OCT?
located in INL
hyper-reflective ring with non-homogenous inner content
small
posterior shadowing
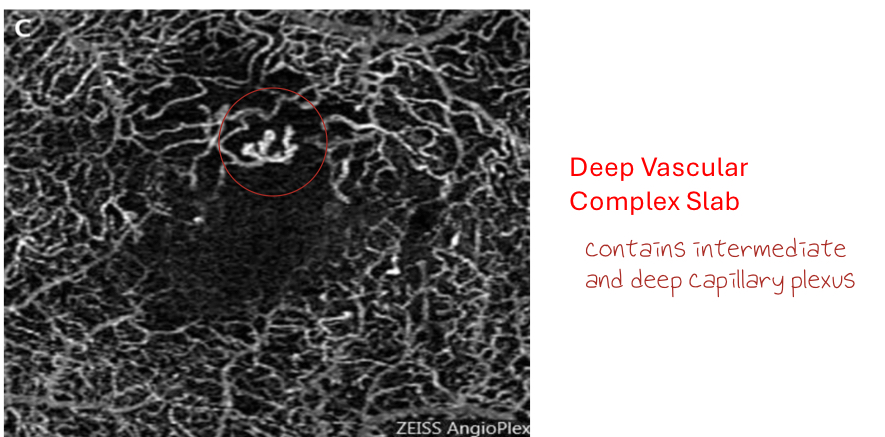
what does a MA look like on OCT-A?
disorganization of capillaries with focal areas of bulging seen in deep vascular complex slab
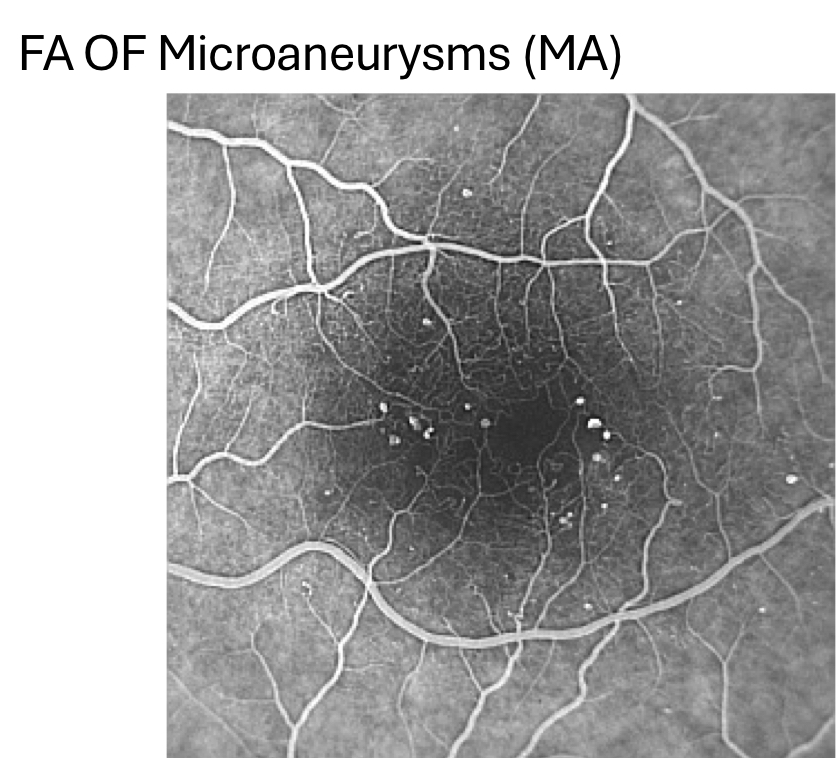
what does a MA look like on FA?
early bright hyperfluorescence, minimal leakage
walls of MA are weak and leak slightly around the outpouching
“christmas tree lights”
best way to view MA
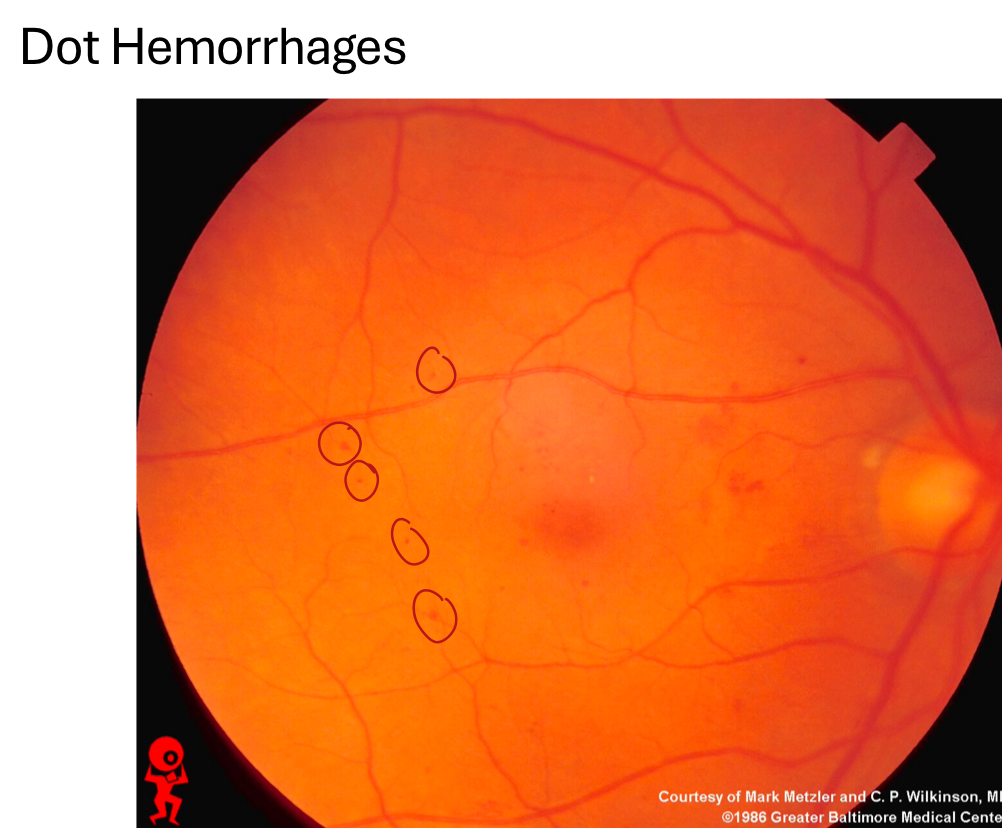
____ are small hemorrhages with distinct borders and form when MA or capillaries burst/leak
dot hemorrhages
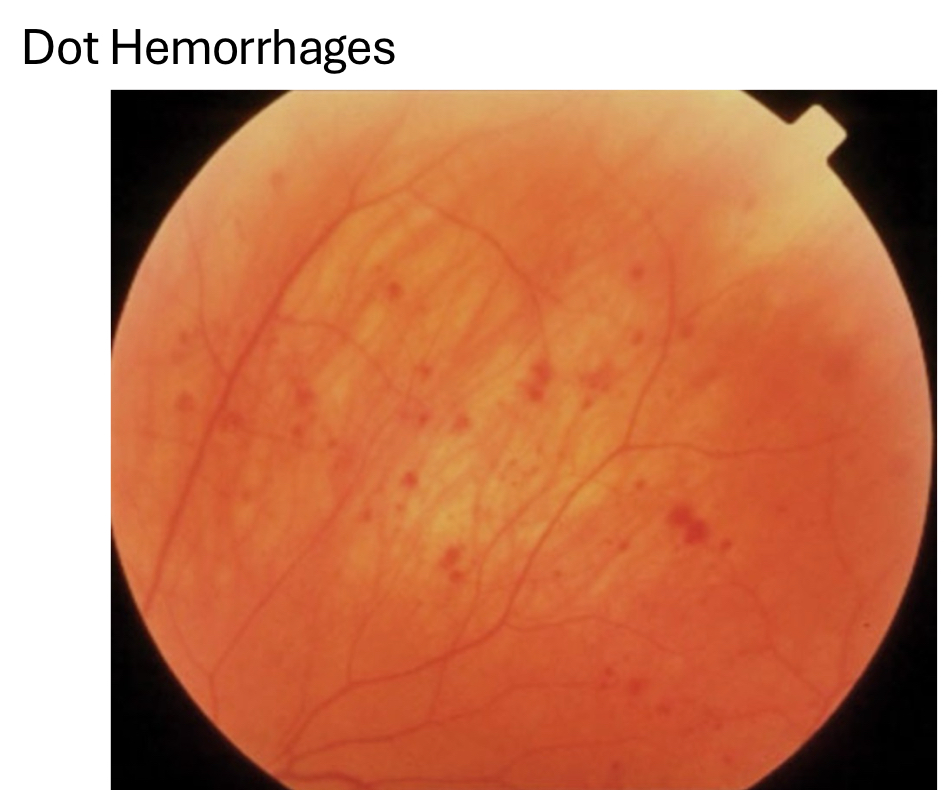
dot hemorrhages are located in ____ and resolve in _____
INL, OPL (intraretinal)
resolves in 3 months
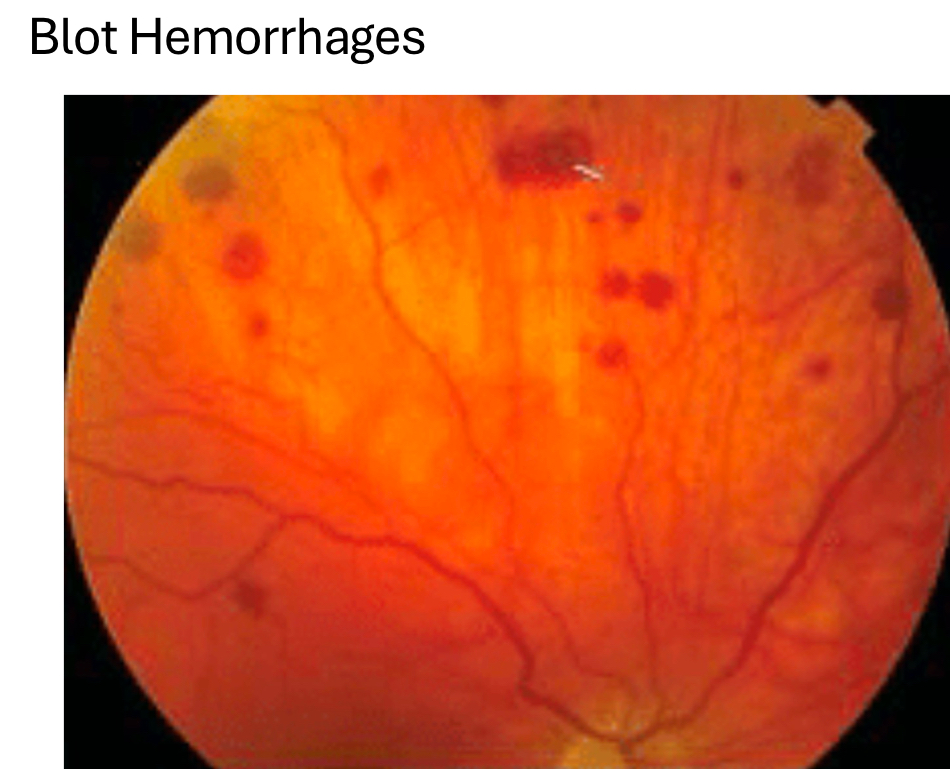
____ are large hemorrhages with indistinct/fuzzy borders and occur when MA or capillaries burst/leak
blot hemorrhages
_____ appear as linear, horizontal hemorrahges and occurs when larger pre-capillary arterioles burst/leak
flame hemorrhages

flame hemorrhages are located in ____ and resolve in ____
located in NFL (where axons of ganglion cells run horizontal/parallel to retina) - intraretinal
resolves in 6 weeks

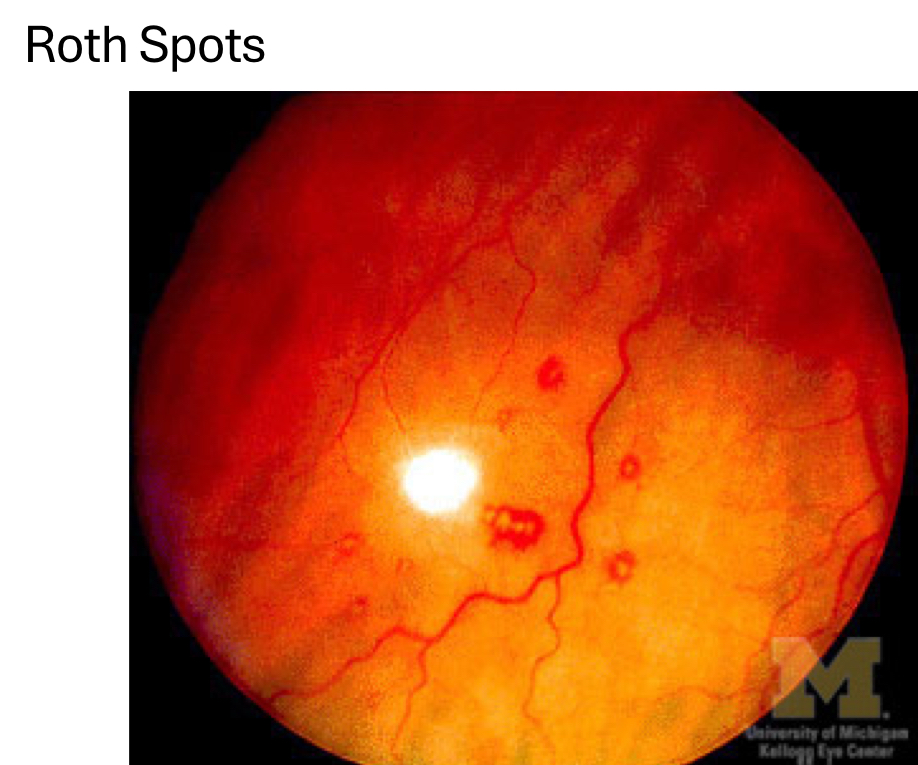
_____ are intraretinal hemorrhages with a white center and represents an acute systemic change (ex: rapidly increasing blood sugar)
roth spots
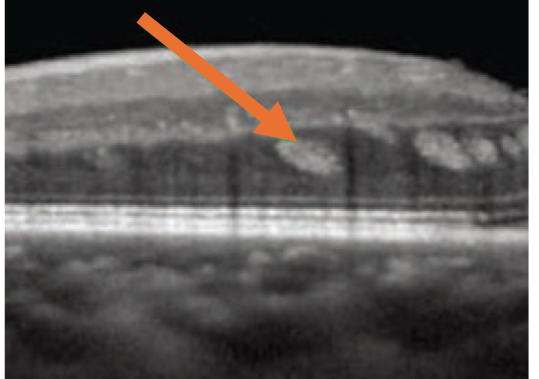
what do dot/blot/flame hemorrhages and roth spots look like on OCT?
uniform hyper-reflectivity
might not show up if small
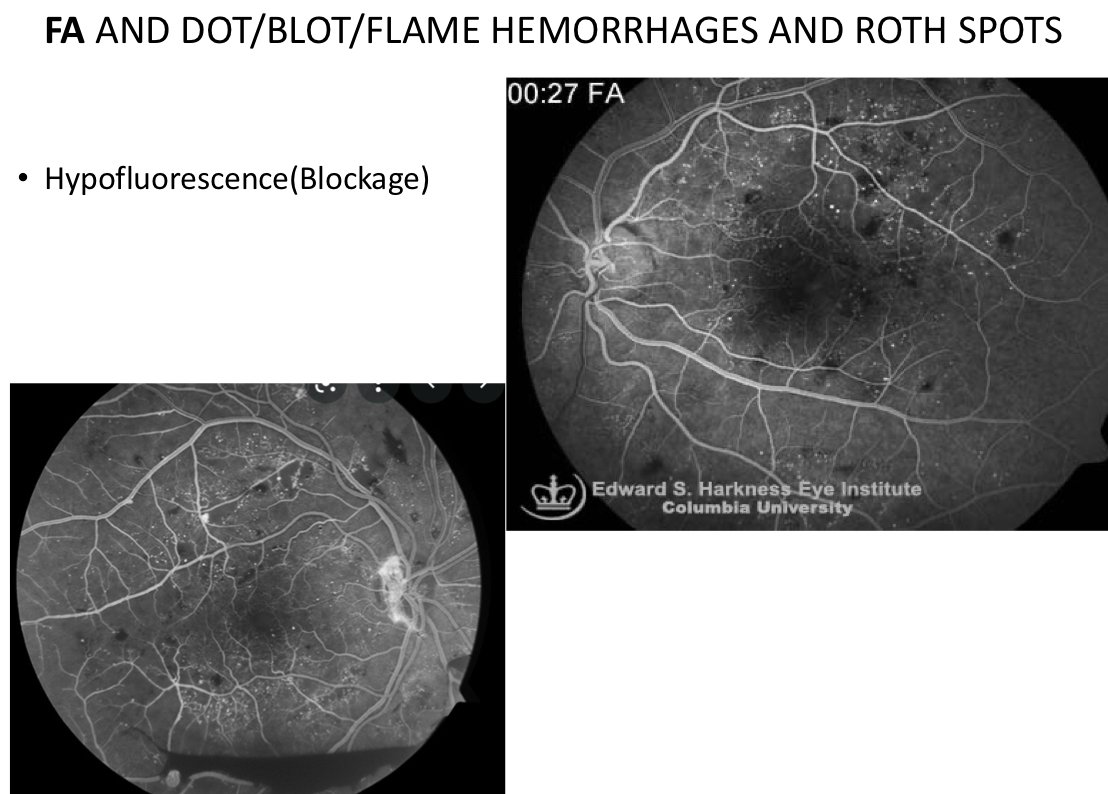
what do dot/blot/flame hemorrhages and roth spots look look like on FA?
hypofluorescence (blockage)
roth spots are intraretinal hemorrhages, typically a ___ or ____ hemorrhage
blot or flame hemorrhage
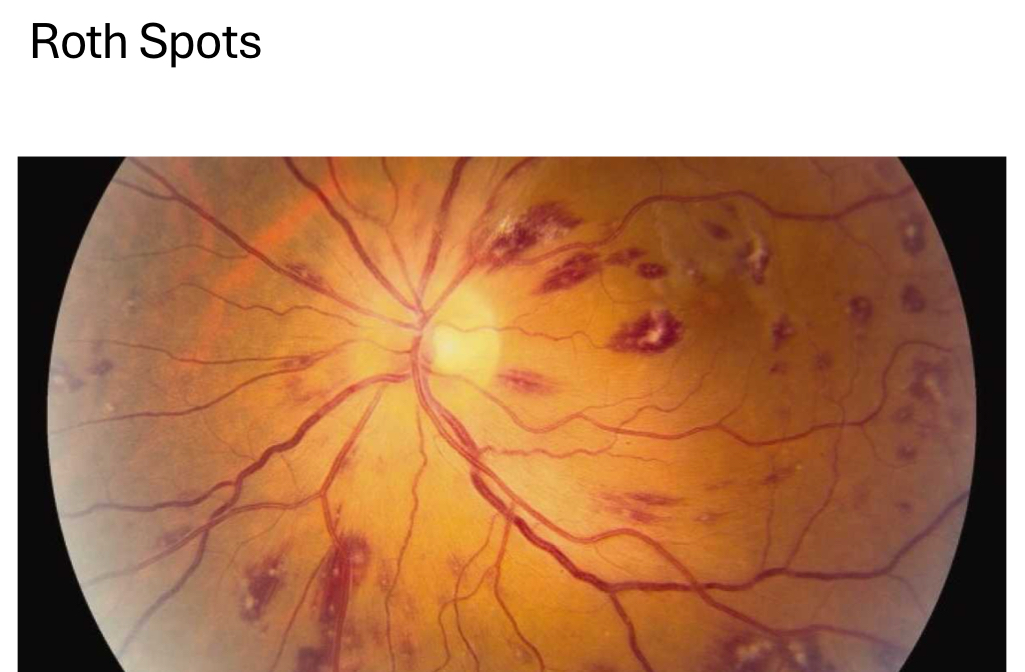
what do dot/blot/flame hemorrhages, roth spots, and CWS look like on FAF?
decrease in AF
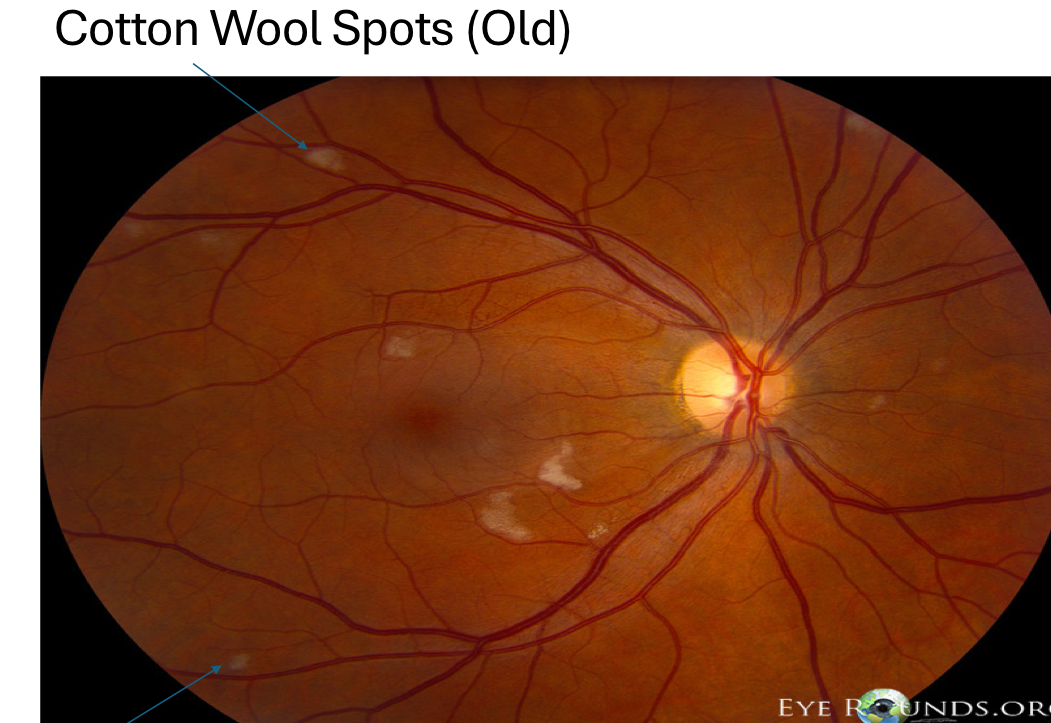
cotton wool spots (CWS) are a build up of ____ which occur due to blockage of axoplasmic flow associated with a RNFL infarct
buildup of axoplasmic debris

CWS appear as a superficial white fluffy deposit in the ____ layer
retinal nerve fiber layer (NFL)
resolution of CWS
resolves in 3-4 months
CWS will get smaller, waxy, more gray color
after resolution → localized atrophy of ganglion cells and nerve fibers → leads to “depression” sign
if a CWS or depression sign is large enough → lead to VF defect
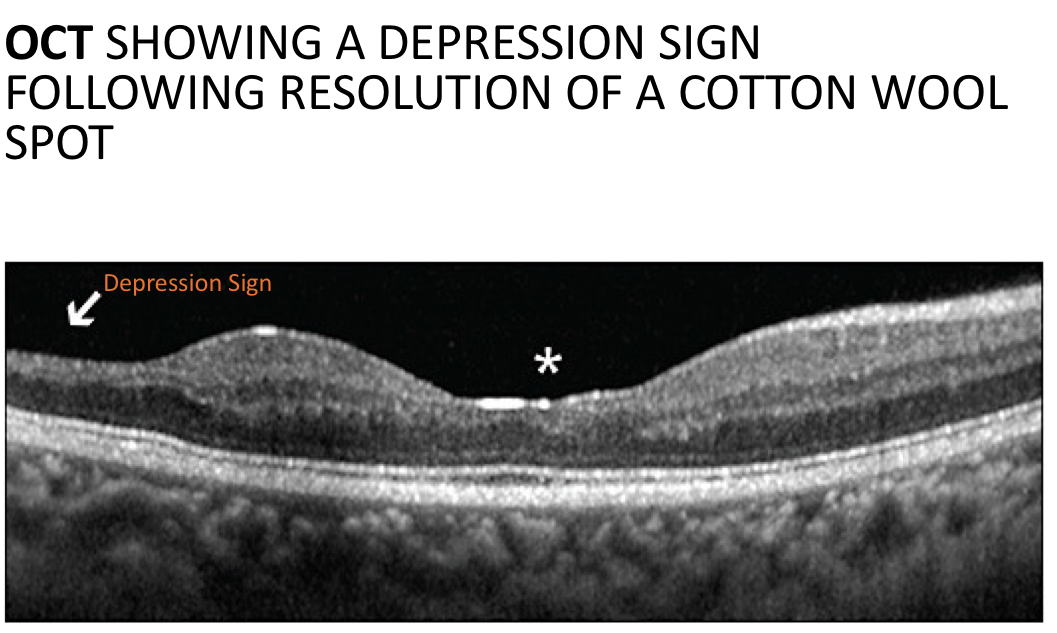
what do CWS look like on OCT?
superficial hyper-reflective nodule at RNFL
posterior shadowing
inner retinal thinning (“depression sign”) may be noted following resolution of CWS
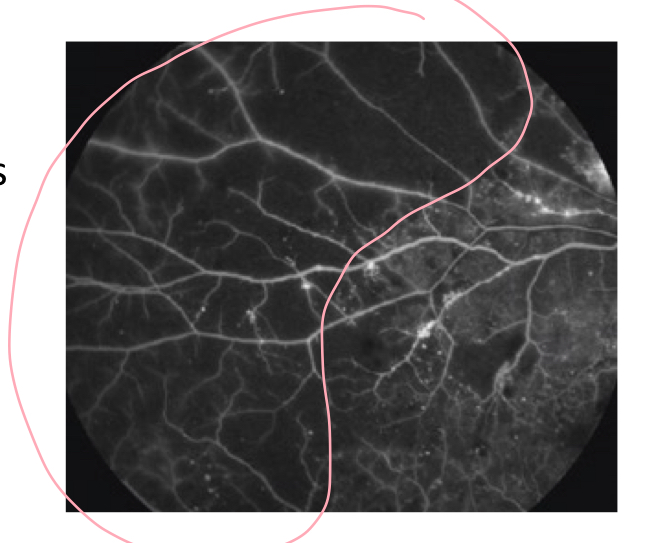
what do CWS look like on FA?
hypofluorescence (blockage) due to CWS itself with adjacent hypofluorescence (filling defect) due to non-perfusion

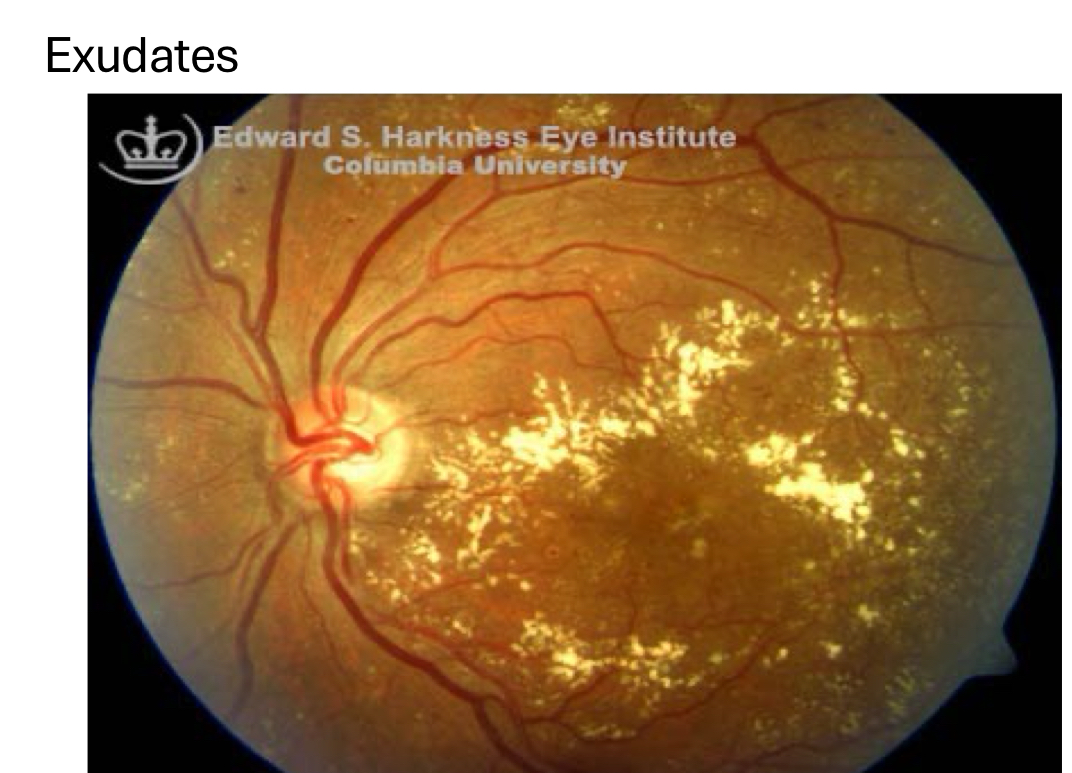
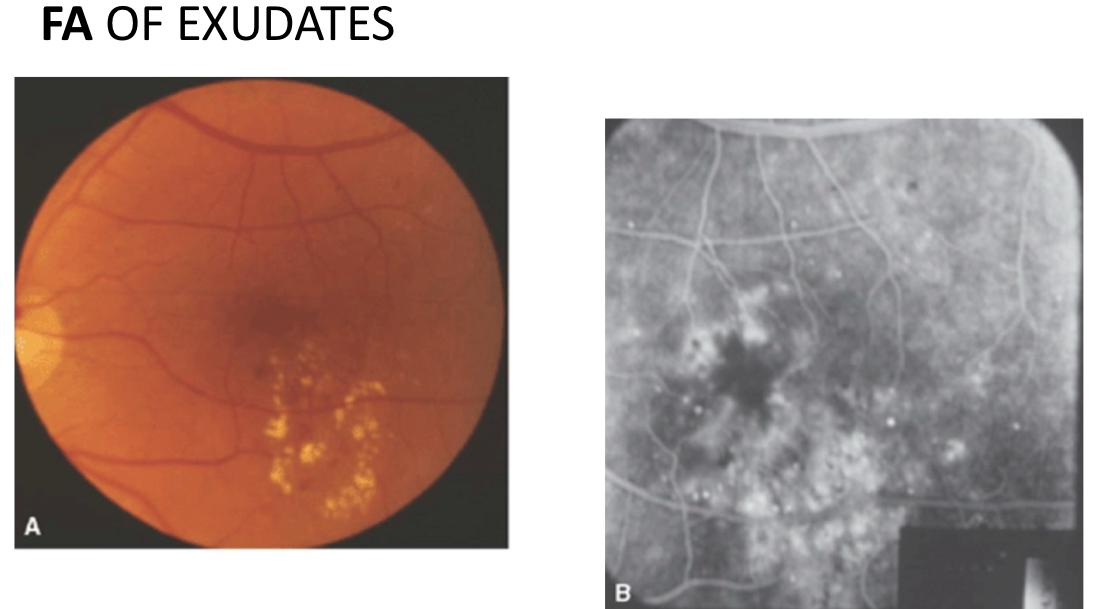
____ are composed of lipoproteins and appear as small, shiny yellow flecks typically associated with retinal fluid or edema
exudates
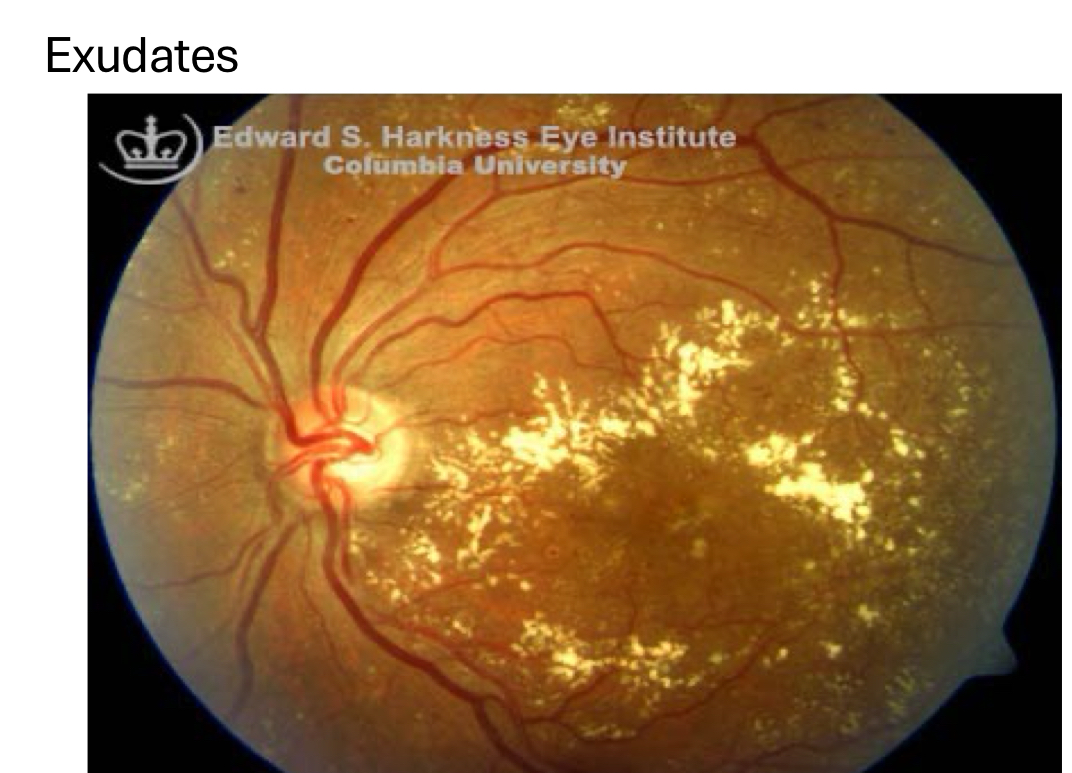
in diabetic retinopathy, exudates appear as
circinate rings with edema/fluid found in middle of the ring
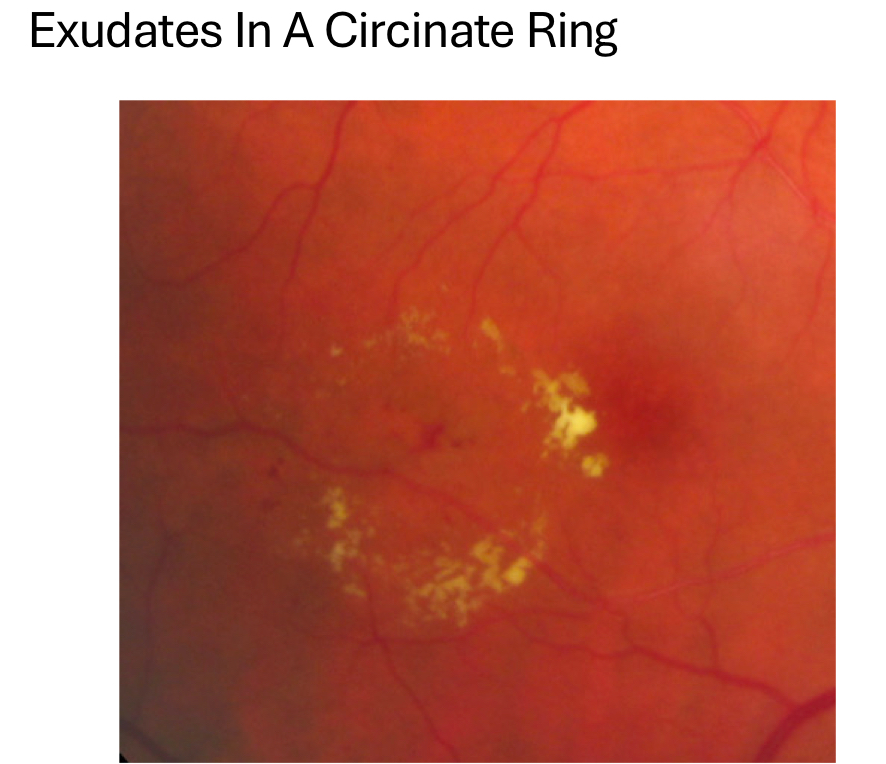
exudates are found at ____ and resolve in ____
found in OPL, ONL (can infiltrate other layers too)
take months-yrs to resolve
it’s visuallly devastating to have exudates in foveal region because
exudates can lead to fibrotic scarring and loss of retinal structures
photoreceptor damage
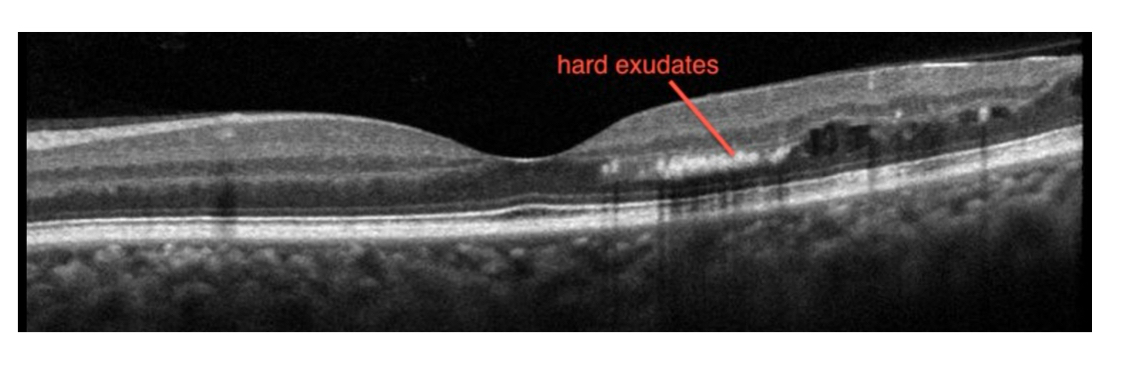
what do exudates look like on OCT?
hyper-reflective spot at ONL/OPL
can be associated with clear/hypo-reflective cystic spaces (fluid/edema)
posterior shadowing
lead to fibrotic scarring and loss of retinal structures
what do exudates look like on FA/FAF?
FA: hypofluorescence (blockage) due to exudates themselves with areas of adjacent hyper fluorescence (leakage)
aka exudates are dark, leakage is bright
FAF: decrease in AF
venous beading occurs due to
weakening of venous walls and sludging/thickening of blood
affects retinal veins/venules
appears as sausaing
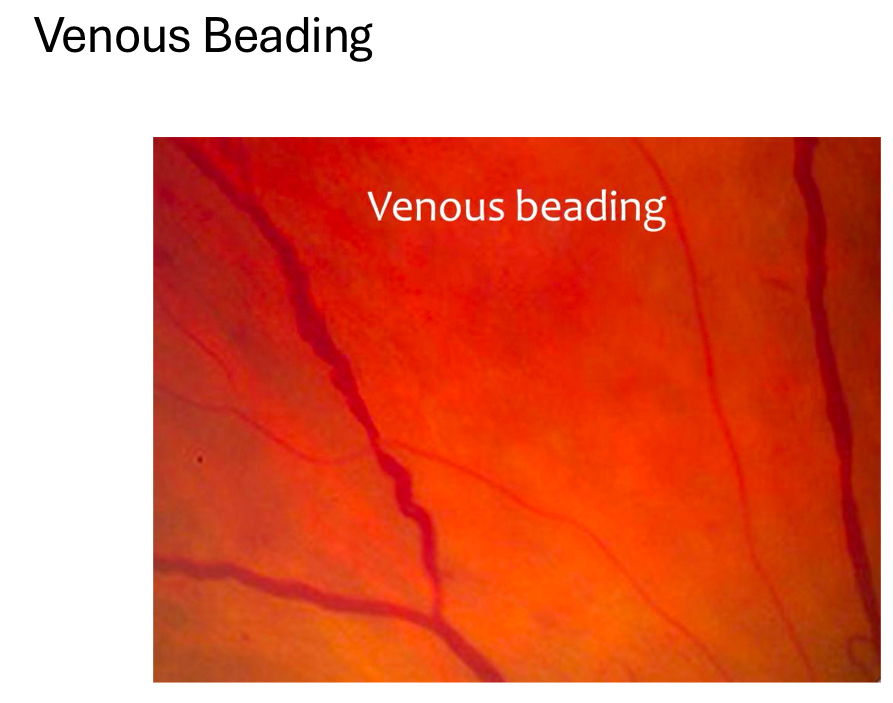
vascular loops and venous beading should show _____ on FA, OCT, OCT-A
no evidence of leakage, fibrotic tissue, or growth of vessels toward vessels
vascular loops/omega loops occur due to
extensive manipulation of vein/venule
formed to bypass an occlusive area in vein/venule
appears as loop
define intraretinal microvascular abnormalities (IRMA)
remodeling and dilation of pre-existing capillaries that occur to supply areas of capillary non-perfusion
these capillaries are “backup”
borders areas of capillary non-perfusion, in between arteries/arterioles and veins/venules
brings blood supply to areas of non-perfusion
looks almost identical to neo
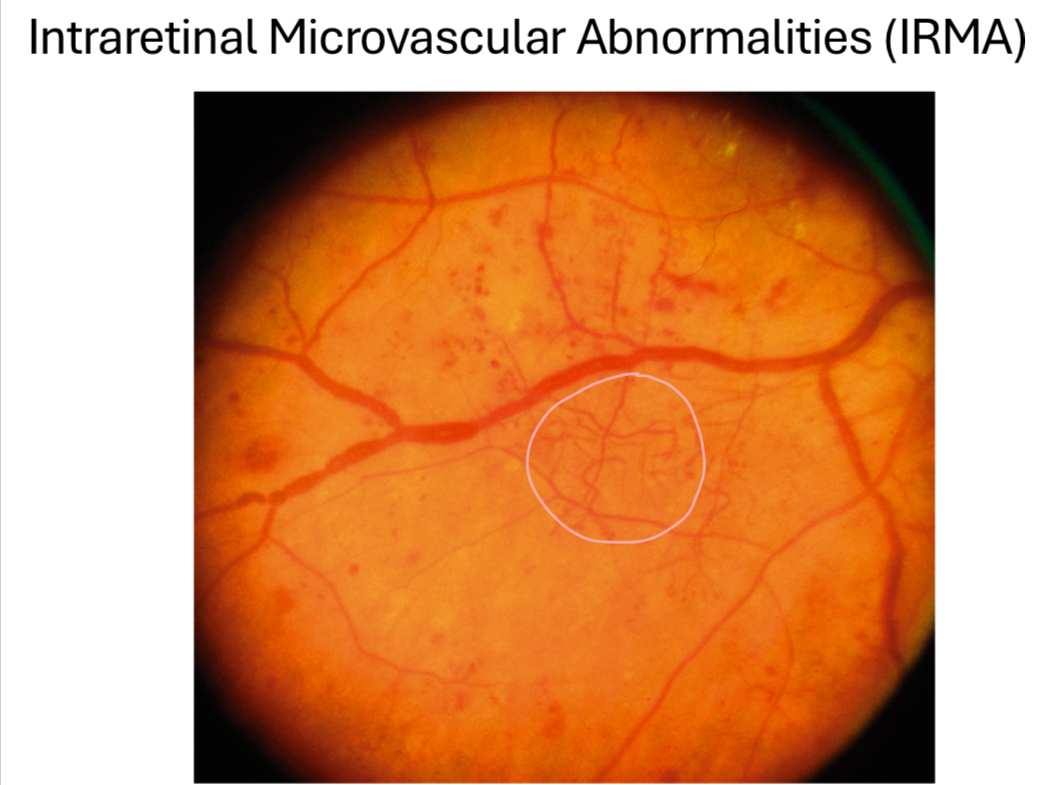
IRMAs are found
at the level of superficial or inner retina (stays w/in the retina)
unlike neo, which grows into vitreous
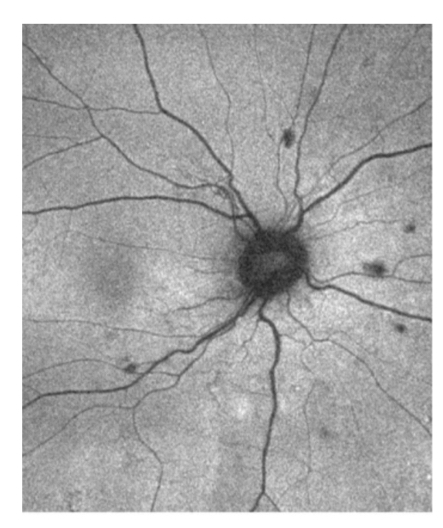
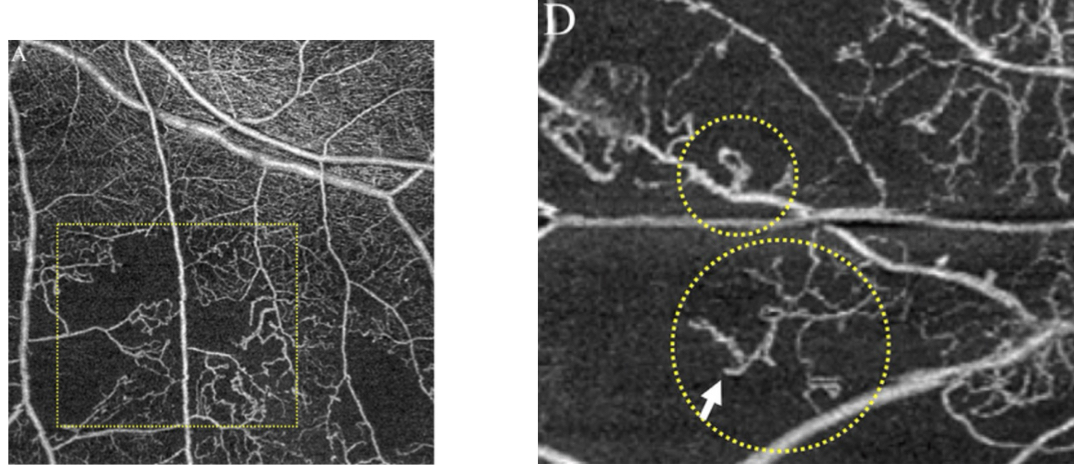
what does IRMA look like on OCT-A?
irregular vascular network in superficial vascular complex slab
shouldn’t see these vessels in vitreoretinal interface (IRMA doesn’t grow into vitreous)
on FA and OCT, IRMA should look like
no evidence of leakage, fibrotic tissue, or growth toward vitreous
some argue there’s slight leakage but much less than retinal neo
____ occurs due to capillary dropout/loss or lack of capillary blood flow, associated with retinal ischemia
capillary non-perfusion
on fundus, capillary non-perfusion looks like
an area in retina that’s mottled/irregular
difficult to see
what does capillary non-perfusion look like on OCT?
disorganization and thinning of inner retina
what does capillary non-perfusion look like on OCT-A?
best seen on OCT-A
areas of flow void in deep vascular complex slab
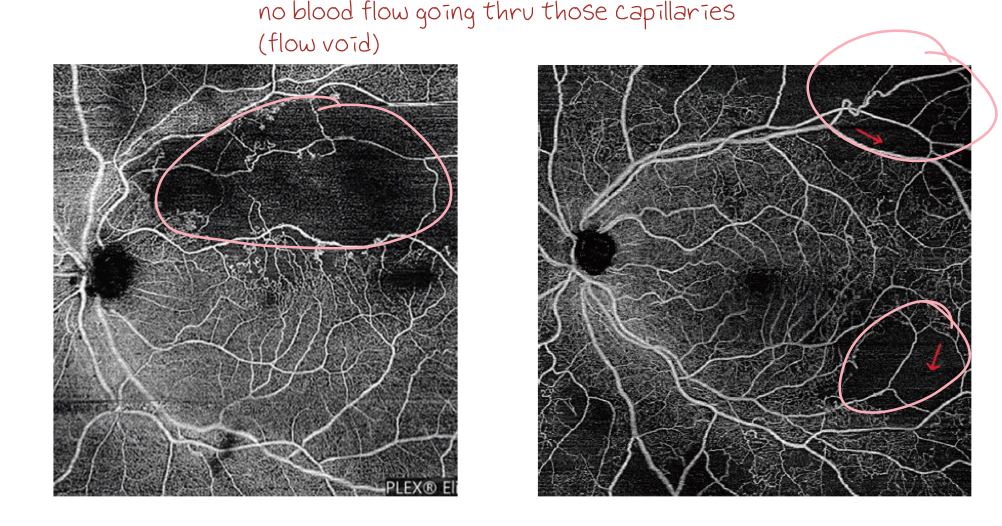
what does capillary non-perfusion look like on FA?
hypofluorescence (filling defect) due to loss of retinal capillaries
mild non-proliferative diabetic retinopathy is defined as ____
and should be treated as ____
microaneurysms only
treatment
monitor, give amsler grid
control BP, blood sugar, cholesterol + other potential risk factors
see pt back in 1 yr
5% risk of progression to proliferative diabetic retinopathy within 1 yr

____ risk of mild non-proliferative diabetic retinopathy progression to proliferative diabetic retinopathy within 1 yr
5% risk of progression
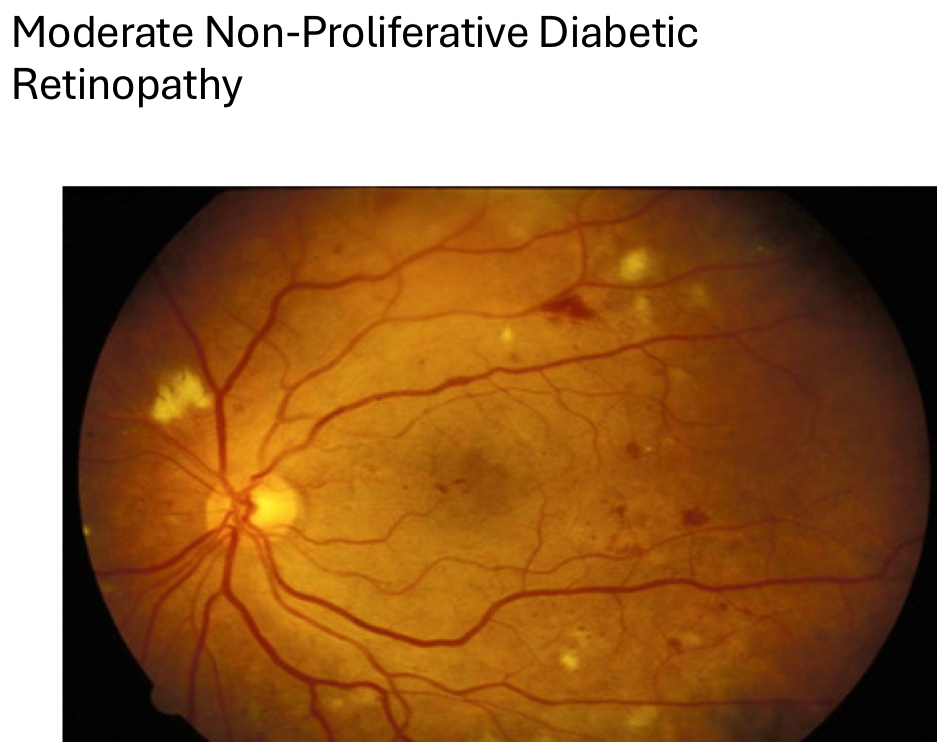
define moderate non-proliferative diabetic retinopathy
microaneurysms
dot/blot/flame hemes
dot/blot > flame and CWS
roth spots
capillary non-perfusion/dropout
cotton wool spots
exudates
venous beading
omega/vascular loops
IRMA
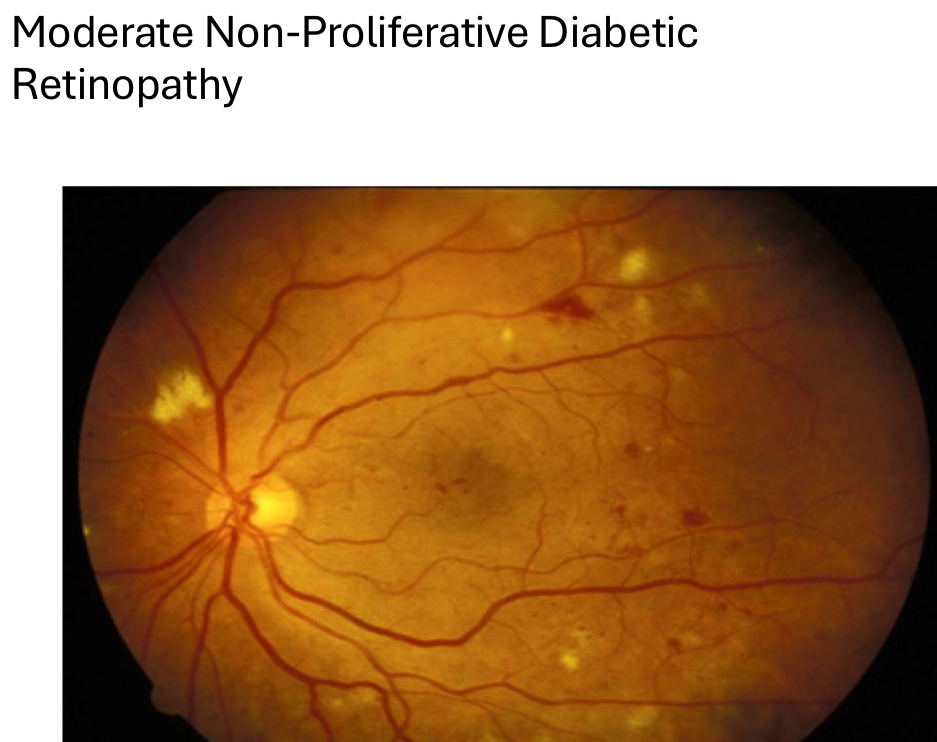
treatment of moderate non-proliferative diabetic retinopathy
monitor, give amsler grid
control BP, blood sugar, cholesterol + other potential risk factors
see pt back in 6-12 months depending on level of blood sugar control and other systemic conditions/risk factors
12% risk of progression to proliferative diabetic retinopathy diabetic retinopathy within 1 yr