Lecture+13+Vector-borne+diseases+2024
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
definitive host
an organism that harbors the adult, sexually reproducing form of a parasite
intermediate host
an organism that harbors a sexually immature stage of a parasite
biological vector
an arthropod that actively transmits pathogens that complete part of their life cycle within the organism
mechanical vector
vector in which the pathogen does not complete any part of its life cycle during transit
vector-borne disease vectors
ticks, mosquitoes, biting flies, fleas, blood feeding bugs, mites, lice
require a blood meal for their eggs to mature: proteins and nutrients in blood essential for egg production
feed in different ways: - piercing-sucking, tearing-rasping - suggests blood feeding evolved multiple times
molecules used by blood-feeding parasite
Anticoagulants: These molecules prevent the host's blood from clotting, making it easier for the parasite to feed. Parasites need to stop coagulation to ensure the blood remains liquid for feeding.
Vasodilators: cause blood vessels to dilate (expand), making it easier for the parasite to access blood. By widening the vessels, they increase blood flow to the feeding area.
Anesthetics: Parasites release these to numb the host so they don't feel the bite as much. This helps the parasite feed undisturbed, as the host won't notice the bite right away.
Immunomodulators: help parasites evade the host's immune system, allowing them to feed without triggering an immune response. By modulating the host's immune system, parasites can avoid detection and continue feeding longer.
targets for vector-borne disease
Human Host Interventions:
Anti-parasite/pathogen therapies: target the parasite or pathogen after it has entered the human body to reduce or eliminate the infection.
Vaccines: boosting the human immune response to the parasite/pathogen before or after exposure.
Arthropod Vector
Genetically modified vectors incapable of reproduction or pathogen transmission
Attractants/repellants and behavioral modifiers: Chemicals or tools that either attract or repel the vectors, making it harder for them to transmit diseases to humans.
Novel insecticides:
Vector longevity curtailers: Methods to shorten the lifespan of the vector so that they don't live long enough to transmit pathogens effectively.
Parasite/Pathogen Interventions:
Vaccines blocking parasite acquisition or transmission by arthropods: Vaccines that target the parasites within the arthropod vector, Insect immune regulators (smart sprays): substances that regulate or enhance the insect's immune system, potentially stopping the parasite/pathogen from being transmitted to the next stage of the life cycle.
general strategies to interrupt transmission of vector borne disease
vectors
Kill vector or alter vector competence for microbe
Inhibit feeding on humansń
Pathogen
Block transmission
Inhibit uptake
Humans
Vaccinate
Diagnose & treat
Reservoir
Eliminate reservoir
Vaccinate or treat reservoir
types of viruses
dengue
zika
west nile
dengue virus
Family: Flaviviridae
Genus: Flavivirus
+ssRNA virus
uncontrolled spread of dengue
Increase in numbers of cases
Geographic dissemination
Co-circulation of multiple serotypes
dengue epidemiology
spread of multiple serotypes
global trade and travel
urbanization
clinical manifestations of dengue
dengue fever:
high fever, headache, retro-orbital pain, fatigue, nausea, vomiting, cutaneous rash
dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS)
increased vascular permeability, hemoconcentration, hypovelmic shock, hemorrhagic manifestations, thrombocytopenia, abdominal pain, cytoskin storn
sequential infection of dengue
while the body builds immunity to one dengue serotype after a primary infection, a secondary infection with a different serotype can lead to a more severe illness due to ADE, increasing the likelihood of complications like Dengue Hemorrhagic Fever (DHF) or Dengue Shock Syndrome (DSS).
Antibody dependent enhancement (ADE)
occurs when antibodies from a previous dengue infection worsen a secondary infection by helping the virus infect more cells, leading to more severe disease
integral hypothesis of dengue
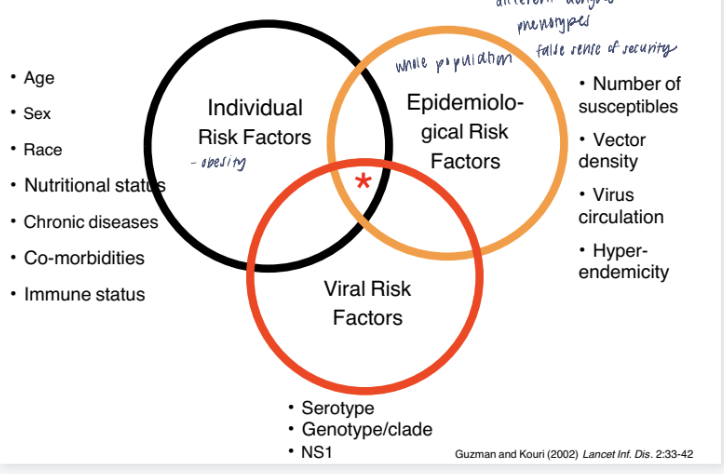
it’s not just one factor but the combination of personal characteristics, environmental conditions, and viral properties that determines the risk of dengue infection and its severity.
dengue diagnosis
Clinical
Serology
RT-PCR
dengue prevention
Mosquito control
Wolbachia – common obligate intracellular endosymbiotic bacteria of insects
disrupt/alter symbiotic relationship to affect vector competence (shorten mosquito lifespan, reduce level of pathogen, etc.)
Vaccine: challenging
Must include all 4 serotypes
Only licensed vaccine has safety issuesh
zika virus
ss(+) RNA virus
Belongs to family Flaviviridae; genus Flavivirus
spread by the bite of an infected Aedes species mosquito
can be passed from a pregnant woman to her fetus; Infection during pregnancy can cause certain birth defects
Local mosquito-borne Zika virus transmission in the continental United States
clinical presentations of Zika
onset of symptoms by Day 1 post infection, last until day 5
most pateints feel better after day 3
maculopapular rash, conjuncivitis, fever, arthralgia, and myalgia
rarely: vomiting, edema, myalgia
guillain-barre syndrome
microcephaly and congenital zika syndrome
viral encephalitis
inflammation of the brain
variety of viruses (togavirus, flavivrus)
west nile virus (WNV): widespread in USA
mosquito: biological vector
west nile virus
flavivirus
ss + sense
enveloped
spread throughout USA< multiple species of mosquitos, 60+ species of birds, mammals, reptiles, and humans
asymptomatic, west nile fever, encephalities
illness primarily in elderly and very young
life cycle: mosquito-bird-mosquito
viral encephalitis: prevention and control
surveillance
Blood screening
Mosquito traps/pool testing for viruses
Sentinel chicken flock immuno-serological testing
Dead bird testing for virus (esp. WNV)
ArboNET
mosquito control
eliminate standing water, mosquito fish, standing water
public education
larvicides
avoid mosquito bites
lyme disease epidemiology
30,000 cases reported to CDC every year; may be ~300,000 (clinicians, commercial labs)
Most cases in New England and Great Lakes
Seasonality: Late spring and summer in United States
lyme disease transmission
Borrelia burgdorferi
vector:
ixodes scapularis: new england and midwest
ixodes pacificus: west coast
need 48-72 hours to disseminate from tick to human
seasonal temporaility
most transmission in late spring and summer by nymph stage ticks
lyme disease: clinical
incubation: 3-32 days
stage 1: 70-80% pateints
erythema migrans (EM) rash
malaise
fatigue
fever
myaglia
stage 2: 5% of untreated pateints
weeks to months folliwng EM
neuritis, carditis, meningitis
stage 3: 60% of untreated pateints
weeks to years following EM
arthiritis, joint pain, swelling
lyme disease virulence factor
one of few pathogenic bacteria that can survive without iorn
enzymes use manganese, avoiding the problem many pathogenic bacteria face in acquiring iron
endoflagella: motility in viscous environment (mucosal tissue)
hide flagella antigens
lyme disease diagnosis
clinical
challenging in stage 2/3
isolation of B.burgdorferi (from captured tick)
significant change in IgM and IgG antibody
lyme disease treatment and prevention
antibitoics: only early after infection
EM: doxycycline/amoxicillin
neurological: IV antibiotics
prevention:
repellent and barriers
immediate tick removal
malaria etiology
phylum: apicomplexa
5 species of plasmodium
P falciparum: worldwide, most serious
P. vivax: rare in reuatorial africa, common in ammericas
P. malariae
P. Ovale. P. knowlesi
vector: anopheles sp mosquito
malaria epidemiology
majority of cases in africa (95%)
infants protected form infection by transfer of maternal Abs
young children at greatest risk of infection
non immune hosts at highest risk for complications and death: travelers, young children
attempts at malaria control
WHO’s worldwide eradication of malaria program (1957)
Widespread use of antimalarial drugs (e.g., chloroquine) in humans
Use of insecticide DDT to control the mosquito vector
Program failed to eradicate or even control malaria
Rise of parasites resistant to chloroquine, pyrimethamine, etc
Anopheles resistant to DDT
Now improved control methods; in 2018, Gates Foundationlaunched Malaria Eradication Program
Insecticide-treated bednets
ndoor residual spraying
Artemisinin combination therap
But, problems of resistance to insecticide and drugs
hypnozoites
in P. vivax and P. ovale a dormant stage [hypnozoites] can persist in the liver and cause relapses by invading the bloodstream weeks, or even years later
malaria clinical manifestation
High fever and chills (due to blood stage cycle)
Anemia (ruptured blood cells decrease oxygen transport)
Splenomegaly (spleen enlarges due to abundance of ruptured RBCs that needs clearing from circulation)
uniquely P. falciparum:
cerebral malaria: capillaries clog in the brain
renal failure: capillaries clog in kidney
pulmonary edema (fluid in lungs)
severe anemia
shock: excess antigen in bloodstream
why is p falciparum more virulent
can infect RBCs and erythropoetic (RBC) stem cels, exacerbating anemia
avoid clearance from spleen (survival strategy 1)
surface antigen in infected RBCs (pfEMP-1) binds adhesion molecules on endothelial cells in capillaries
PfEmp1 on RBC surface can bind platelets and other infected RBCs (rosetting)
by adhering to capillaries and rosetting, infected RBCs can clog blood flow to vital organs
where the capillaries are obstructed leads to particular clinical manifestations
p falciparum antigenic variation
survival strategy 2
P. falciparum evades the immune system by changing its surface antigens in a process called antigenic variation, leading to waves of immune responses.
parasite creates "waves" of antigen variation as each parasite clone switches its surface antigens, continuing this cycle until the parasite runs out of infected RBC surface antigens and matching endothelial cell receptors.
This strategy allows the parasite to persist in the host for a long time, even as the immune system gradually catches up to each variant.
Over time, after exposure to many variants, the host develops clinical immunity, allowing them to carry the parasite without experiencing symptoms, although the infection isn’t completely cleared.
treatment of malaria
chloroquine
resistance very common in P.falciparum infections
growing resistance in other plasmodium species
mefloquine
common chemoprophylaxis in travels
associated with weird dreams
antibiotics (doxycycline): used for chemoprophylaxis
arteminsins
used as herbal remedy in china for thousands of years
control & prevention of malaria
insecticide-treated bed nets
indoor residual spraying
chemoprophylaxis in travelers
repellents/long sleeved clothing
drain pools of standing water
vaccine: 3 doses + booster (1y)
low to moderate efficacy
relatively short-lived
onchocerciasis
etiology: enchocerca volvylus
filarial nematode
organism
adult worm
can live 15 years and release 700 microfiliare a day
vector
infected black of simulium sp
blackflies breed near fast-running water
onchocerciasis disease
microfilaria travel to subcutaneous tissue, mature into adults and reside in nodules
microfilaria in circulation travel to skin to be transmitted to biting fly
microfilaria migration causes extreme itching
lichenification
skin infections
sleep
microfilaria migration to eye causes blindess
immunopathogenesis of river blindness
4th leaving cause of blindness worldwide
microfilaria travel to corneal stroma and release wolbachia & wolbachia products when they die or release products
wolbachia LPS-like protein triggers macrophage and eosinophil chemotaxis to stroma and release cytokines
inflammation causes keratitis (corneal clouding) and blindess
wolbachia
Endosymbiotic bacteria in both adult worms and microfilaria
Required for embryogenesis
Can use drugs (e.g., doxycycline antibiotic) that target the Wolbachia and kill the adult worm)
onchocerciasis diagnosis
Skin snips for microfilaria
ID adult worms in nodules
onchocerciasis treatment
ivermectin: kills parasite larvae (microfilariae), relieves the severe skin itching and stops the damaging effects on the eye caused by the disease
does not affect adult worms so does not cure infection
doxycycline: kills wolbachia and adult worm
onchocerciasis prevention
mass ivermectin campaigns
repellents
insecticide